Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7588
Peer-review started: April 6, 2021
First decision: May 11, 2021
Revised: May 14, 2021
Accepted: July 22, 2021
Article in press: July 22, 2021
Published online: September 6, 2021
Processing time: 147 Days and 3.3 Hours
Zoster sine herpete (ZSH) can be misdiagnosed because there are no typical vesicular eruptions characterized by a dermatomal distribution. However, incorrect treatment due to a misdiagnosis can lead to severe pain and fatal complications.
A 75-year-old woman complained of sudden onset right shoulder pain and atypical headache. After 18 d, sudden hearing loss occurred in the left ear. In serology tests conducted after the onset of hearing loss, varicella-zoster virus IgM was positive. She had no history of a rash or trauma. Under the suspicion of ZSH, antiviral treatment and stellate ganglion block were administered four times, and the pain was effectively controlled.
Early diagnosis and treatment of ZSH can help not only by reducing pain but also by preventing fatal complications.
Core Tip: If the development of shingles does not occur in patients with complex underlying diseases, treatment and diagnosis of zoster sine herpete (ZSH) may be delayed. Clinical symptoms are well evaluated when the patient complains of pain. Serological tests should be conducted to provide a basis for the diagnosis of ZSH. It is possible to effectively treat the disease without causing serious complications.
- Citation: Yun G, Kim E, Baik J, Do W, Jung YH, You CM. Diagnosis and management of ophthalmic zoster sine herpete accompanied by cervical spine disc protrusion: A case report. World J Clin Cases 2021; 9(25): 7588-7592
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7588.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7588
The causes of atypical facial pain and headache are variable, and one of them is herpes zoster (HZ)[1]. Zoster sine herpete (ZSH) is an atypical clinical manifestation of HZ. ZSH has been defined as pain in a dermatomal distribution without a rash and is more difficult to diagnose than typical HZ because there is no vesicular eruption. Misdiagnosis of ZSH can lead to prolonged severe neuropathic pain, nerve palsy, myelitis, pneumonitis, otitis externa, ophthalmic complications, and fatal complications, such as encephalitis or stroke[2].
Ophthalmic ZSH was first described by Ross in 1949. When ZSH involves the ophthalmic division of the trigeminal nerve, it causes symptoms such as trigeminal neuralgia and headache[3,4]. As ZSH is uncommon, it is usually not suspected, especially when accompanied by other problems, until other common causes for the symptoms are ruled out. Herein, we report a case of ZSH that occurred in a patient with sudden hearing loss and cervical spine abnormalities. The patient was diagnosed based on serologic examination findings and clinical manifestations and treated successfully with antiviral management and stellate ganglion blocks.
A 75-year-old woman complained of sharp and shooting pain in the right frontal region for one month.
The patient had received a cervical epidural block twice at an orthopedic clinic because of sudden shoulder pain in the C4/5 dermatome and atypical headache. However, she still had sharp and shooting pain in the right frontal region. The pain was so severe that she could not sleep at night and touch her hair. Eighteen days after the symptoms occurred, she collapsed due to dizziness. One month after initial onset of symptoms, the patient was admitted to the otolaryngology department of our hospital and received steroid pulse therapy for sudden left hearing loss. In addition, the patient was referred to a pain clinic. When the pain physician asked the patient about her symptoms, she said that the right forehead hurt the most. No typical rash was observed in the patient's ear or the area of pain. There was no history of a rash or trauma (Figure 1).
The patient had no previous diagnosis.
The patient had no significant family history.
No neurological abnormalities were observed. The patient’s symptoms were not provoked by neck movement or pressure over tender points in the neck and did not worsen with the Spurling’s test.
The result for varicella-zoster virus (VZV)-IgM (titer 2.7) was positive in a test conducted to determine the cause of sudden hearing loss. The test was performed 23 days after the onset of pain. When she was referred to the pain clinic one month after the occurrence of symptoms, VZV-IgG and polymerase chain reaction (PCR) tests were performed to precisely determine the patient’s condition. Serum VZV-IgG (titer, 4.26) finding was positive. However, DNA in the serum was not detected by PCR testing.
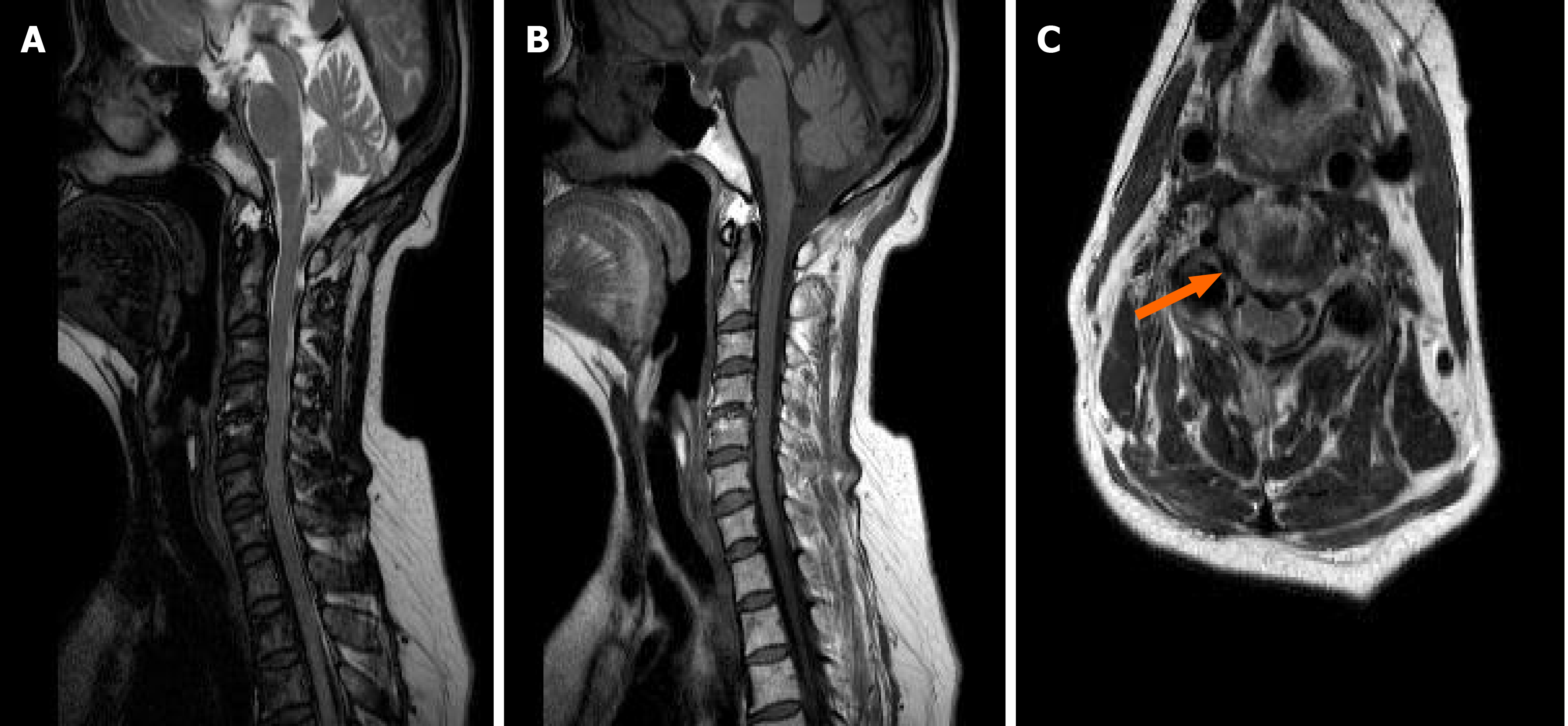
Brain computed tomography and magnetic resonance imaging (MRI) were performed to diagnose central origin lesions, but no abnormalities were observed. MRI of the cervical spine was performed under the suspicion of cervicogenic headache and cervical radiculopathy, and C3/4 central disc protrusion, C4/5 disc protrusion, right neural foramina stenosis at C4/5, focal compression of the spinal cord at C4/5, and C5/6 disc protrusion were observed (Figure 2).
The final diagnosis of the case was ophthalmic ZSH.
First, a stellate ganglion block was planned for rapid control of severe pain. Stellate ganglion blocks were administered four times, once every two days. At the same time, antiviral management (valacyclovir 1 g, three times per day for 7 d) was performed.
After the first stellate ganglion block using 6 mL of 0.375% ropivacaine was administered, the patient reported that she could wash her hair. Stellate ganglion block was performed three more times, after which the numeral rating scale score reduced from 10 to 0. The pain was effectively controlled. The patient was discharged without pain.
In this case, the patient experienced continuous pain in a specific area innervated by the ophthalmic branch of the trigeminal nerve. She also experienced pain in the shoulder and neck because of an abnormal cervical spine. She had previously received a cervical epidural block two times, and her neck and shoulder pain were alleviated, but the headache worsened within one month. Concurrently, the patient collapsed due to sudden hearing loss in the left ear and was hospitalized. The pattern of pain corresponded to neuropathic pain, and both VZV-IgG and VZV-IgM were observed in the serum. We initiated antiviral management and administered ultrasound-guided stellate ganglion block under the suspicion of ZSH, and her headache was completely resolved in a week.
The most important aspect in diagnosing HZ is vesicle history[1]. The diagnosis of ZSH is difficult because there are no vesicles in the area associated with pain. Owing to its rarity, it is generally not considered as the cause.
In this case, the patient had an abnormal cervical spine (C3/4, C4/5, C5/6) with C4/5 right neural foramina stenosis. She experienced not only a headache but also shoulder and neck pain. She had restricted range of motion in the neck. Usually a cervicogenic headache worsens due to provocation maneuvers and is diminished following diagnostic cervical epidural blockade, which were not observed in our case[5]. Therefore, cervicogenic headache could be excluded. Headache can be caused by a tumor or cranial nerve problem, but there was no abnormality on brain MRI and neurologic examination conducted by a neurologist. As the area associated with the pain was innervated by the ophthalmic branch of the trigeminal nerve, trigeminal neuralgia was considered. However, trigeminal neuralgia is characterized by touch-evoked paroxysmal attacks, unlike the pain in this patient.
Diagnosis is usually based on clinical manifestations; however, serological examinations can be used for diagnosis. When a patient has a primary infection with VZV, VZV-IgM will be positive, but VZV-IgG will not be detected[6]. Both VZV-IgM and VZV-IgG are detected in case of reactivation of VZV[6]. VZV-IgM can be detected in a narrow time window during the early VZV reactivation period[7]. VZV DNA findings are usually negative when a VZV-specific antibody response occurs[7]. The most valuable tests are the detection of VZV DNA or VZV-IgG in cerebrospinal fluid (CSF)[8]. However, immunoglobulin tests and PCR test using CSF were not performed because the patient refused CSF tapping. Some studies have reported that serum VZV-IgG has no diagnostic value because such antibodies can be detected in nearly all adults throughout life[8]. In this case, acute zoster pain was suspected because positive laboratory findings of VZV-IgM was observed 24 d after the onset of symptoms. Since VZV-IgG and PCR tests were not performed at the same time, it is difficult to diagnose based on serology alone. The possibility that the virus had been lost due to the activation of the immune response was considered. In conclusion, a diagnosis with only serological examination was not possible in this case. Diagnosis would have been easier if VZV DNA detection in the CSF or saliva was performed.
The patient was female and elderly. Therefore, delayed antiviral therapy could cause serious complications. Antiviral therapy and stellate ganglion blocks were administered based on serological findings and clinical symptoms, which were indicative of ZSH. Consequently, severe neuropathic pain on her right face disapp
ZSH of the trigeminal nerve should be considered as a cause of severe headache associated with the area this nerve innervates. Early diagnosis and treatment of ZSH can help not only reduce pain but also prevent fatal complications.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, general and internal
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He CY S-Editor: Wang JL L-Editor: A P-Editor: Xing YX
| 1. | Dayan RR, Peleg R. Herpes zoster - typical and atypical presentations. Postgrad Med. 2017;129:567-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Weitzman D, Shavit O, Stein M, Cohen R, Chodick G, Shalev V. A population based study of the epidemiology of Herpes Zoster and its complications. J Infect. 2013;67:463-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Marumoto T, Hiratsuka Y, Murakami A. The significance of the determination of lymphocytes with clinical manifestation of ophthalmic zoster sine herpete. Clin Ophthalmol. 2010;4:817-822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Sigireddi RR, Lyons LJ, Beaver HA, Lee AG. Herpes zoster ophthalmicus: Pre-eruption phase sine herpete. Am J Ophthalmol Case Rep. 2018;10:201-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Blumenfeld A, Siavoshi S. The Challenges of Cervicogenic Headache. Curr Pain Headache Rep. 2018;22:47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Kasahara M, Ichinohe T, Sano T, Fukuda K, Kaneko Y. A case of zoster sine herpete of the trigeminal nerve. Bull Tokyo Dent Coll. 2011;52:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Zhou J, Li J, Ma L, Cao S. Zoster sine herpete: a review. Korean J Pain. 2020;33:208-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 8. | Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Neurological disease produced by varicella zoster virus reactivation without rash. Curr Top Microbiol Immunol. 2010;342:243-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |