Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7564
Peer-review started: March 7, 2021
First decision: May 24, 2021
Revised: May 30, 2021
Accepted: July 19, 2021
Article in press: July 19, 2021
Published online: September 6, 2021
Processing time: 176 Days and 21.7 Hours
Trigger finger at the wrist, which occurs with finger movement, is an uncommon presentation. Few reports describing cases of trigger finger at the wrist have been published. Thus, we present a case of an intramuscular lipoma arising from an anomalous flexor digitorum muscle belly in a 48-year-old female patient causing painful finger triggering at the wrist and carpal tunnel syndrome (CTS).
A 48-year-old woman with complaints of a catching sensation during wrist motion and a progressive tingling sensation on the palmar aspect of the right hand for approximately 2 years was referred to our hospital. Triggering of the index to middle finger was evident with a palpable and audible clunk over the carpal tunnel during passive motion. Tinel’s sign was positive over the carpal tunnel of the right wrist with a positive Phalen’s test. Nerve conduction studies of the median nerve demonstrated a right CTS. Ultrasound examination revealed a 2.5 cm × 2.0 cm subcutaneous hyperechoic mass with no obvious blood flow at the wrist of the right arm. Surgical excision of the tumor and muscle mass led to a resolution of the patient’s symptoms, and any triggering or discomfort disappeared. The patient has had no evidence of recurrence at more than 1 year of follow-up.
Triggering of the fingers at the wrist is rare. It must be noted that there are many possible causes and types of triggering or clicking around the wrist. Accurate diagnosis is mandatory to avoid inaccurate treatment of patients with trigger wrist. During the diagnosis and treatment of CTS, attention should be paid to the variation of tendon tissue in the carpal tunnel, to avoid only focusing on the release of transverse carpal ligament and ignoring the removal of anomalous muscle belly.
Core Tip: Our manuscript presents a case of an intramuscular lipoma arising from an anomalous flexor digitorum muscle belly in a 48-year-old female patient causing painful finger triggering at the wrist and carpal tunnel syndrome. Moreover, we reviewed the literature and discuss its etiology. Our findings revealed that there are many possible causes and types of triggering or clicking around the wrist. The accurate examination and proper diagnosis are mandatory to avoided improper and time-wasting treatment for patients with trigger finger at the wrist. During the diagnosis and treatment of carpal tunnel syndrome, attention should be paid to the variation of tendon tissue in the carpal tunnel to avoid focusing only on the release of transverse carpal ligament and ignoring the removal of anomalous muscle belly.
- Citation: Huang C, Jin HJ, Song DB, Zhu Z, Tian H, Li ZH, Qu WR, Li R. Trigger finger at the wrist caused by an intramuscular lipoma within the carpal tunnel: A case report. World J Clin Cases 2021; 9(25): 7564-7571
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7564.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7564
Trigger finger at the wrist is a relatively uncommon condition compared to trigger finger, which is the most common cause of pain and disability of the hands[1]. Triggering at the wrist occurs with finger or wrist motion[2]. Few reports describing trigger finger at the wrist have been published. The possible etiologies of the condition include an anomalous muscle belly in the carpal tunnel, tumor, or a rheumatoid nodule in the flexor tendons inside the carpal tunnel[3]. We present a case of trigger finger at the wrist caused by a combination of both tumor and anomalous muscle belly in the carpal tunnel. We report such a case of an intramuscular lipoma (IML) arising from anomalous flexor digitorum muscle belly in a 48-year-old female patient, causing painful finger triggering at the wrist and carpal tunnel syndrome (CTS). Moreover, to date, few reports describing cases of trigger finger at the wrist caused by IML arising from the anomalous flexor digitorum muscle (FDS) have been reported in the literature. Thus, we have reviewed the literature and discuss its etiology.
A 48-year-old woman complained of a catching sensation during wrist motion and a progressive tingling sensation on the palmar aspect of the right hand.
Patient’s symptoms started approximately 2 years ago with a catching sensation during wrist motion and a progressive tingling sensation on the palmar aspect of the right hand, which had been worsened the last 3 mo.
The patient was in good health and had no history of other diseases.
The patient and her family had no history of other diseases.
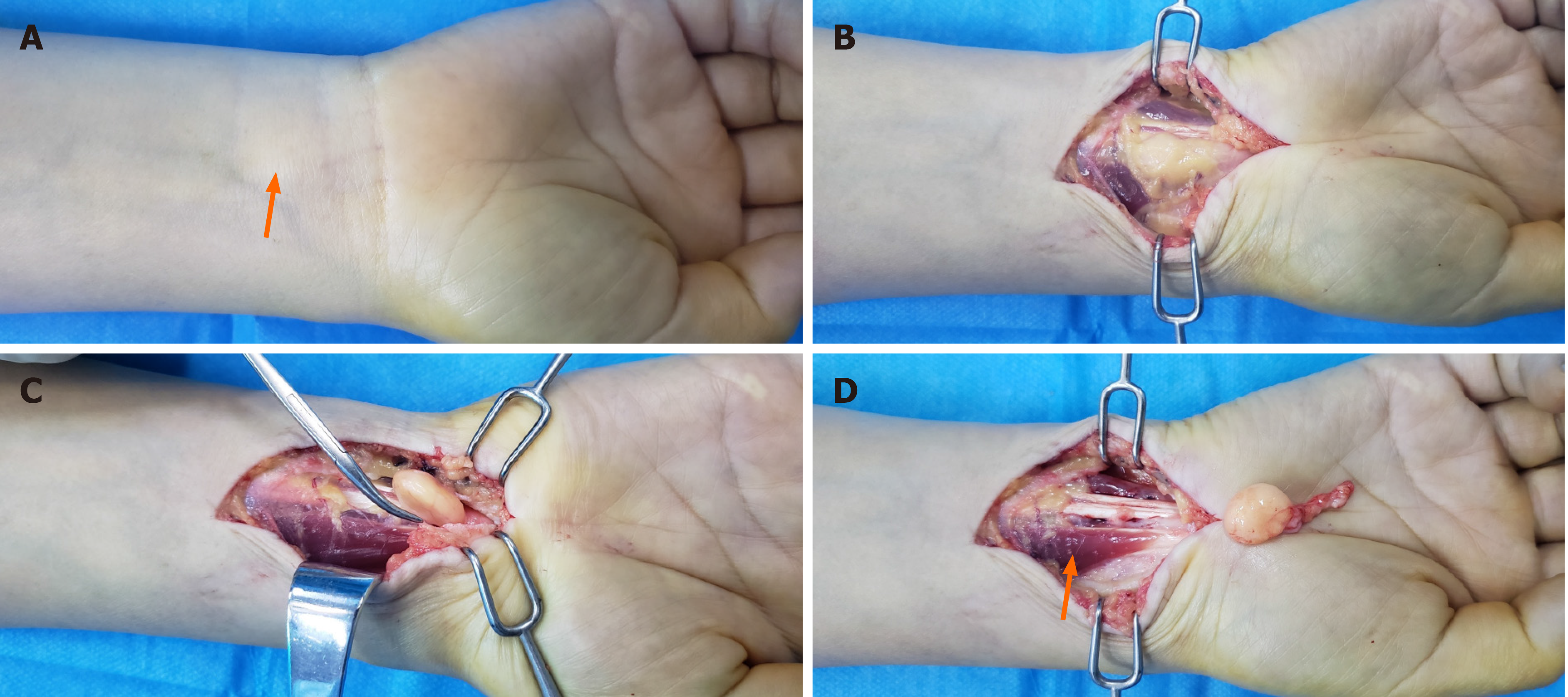
There was a moderate palpable mass (3 cm × 2 cm) on the palmar side of her right wrist (Figure 1A). The mass was not tender and moved simultaneously up and down during flexor tendon movement. Paraesthesia, distributed over the palmar radial three and a half digits of the hand, developed after the onset of wrist triggering, suggesting CTS. The paraesthesia progressively worsened when performing manual tasks and when sleeping. During the physical examination, triggering of the index to middle finger was evident with a palpable and audible clunk over the carpal tunnel during passive motion. Tinel’s sign was positive over the carpal tunnel of the right wrist with a positive Phalen’s test. Active and passive ranges of motion as well as grip strength were normal, except for the right index finger, which became limited during flexion. Nerve conduction studies of the median nerve demonstrated a right CTS.
X-ray examinations revealed no abnormal findings. Ultrasound examination revealed a 2.5 cm × 2.0 cm subcutaneous hyperechoic mass with no obvious blood flow at the wrist of the right arm.
The clinical diagnosis was trigger finger at the wrist and CTS.
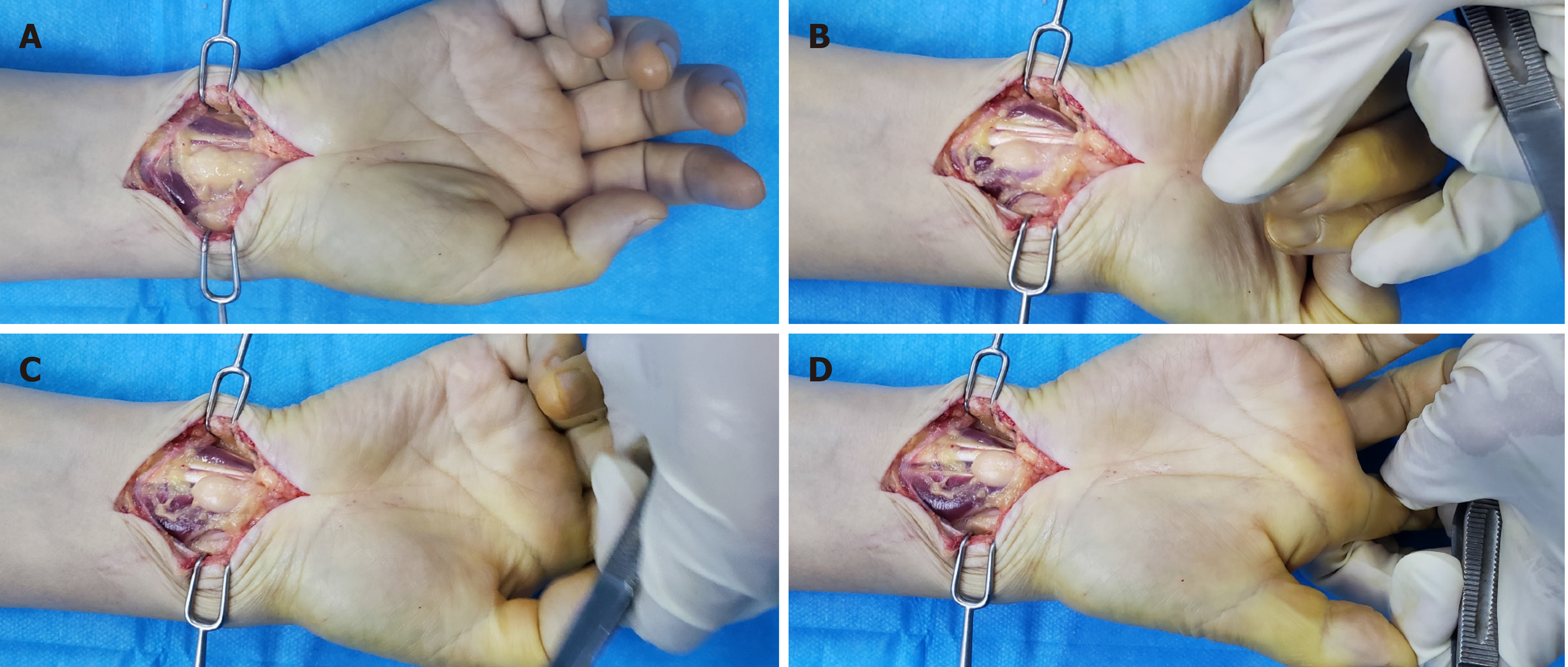
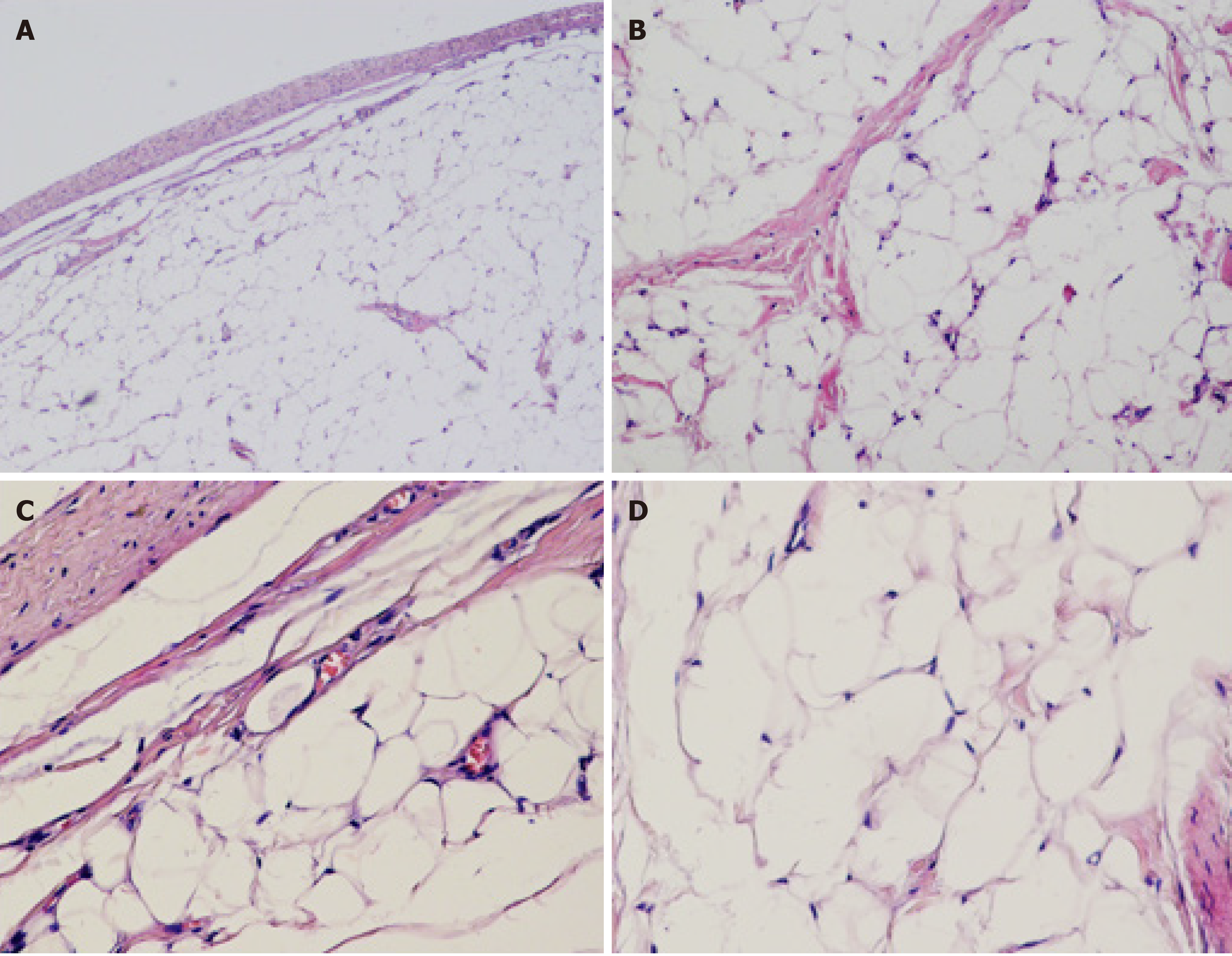
Surgical exploration was performed through a longitudinal carpal tunnel incision (Figure 1B-D). After peeling back the skin and subcutaneous tissues, no subcutaneous edema was observed, and there was no obvious inflammation in the deep fascia. After removal of the deep fascia, the anomalous flexor digitorum muscle belly was shifted down abnormally, and a yellowish-white cable-like mass was observed at the distal end of the FDS of the index finger. The muscle fibers were bluntly peeled, and a 2.5 cm × 2.0 cm × 2.0 cm oval, yellow, soft mass with an intact capsule was visible. The mass arose from the anomalous muscle belly of the FDS, growing longitudinally and extending into the carpal tunnel. The mass was shifted synchronously with the tendon during passive flexion of the index finger. The mass was positioned outside the carpal tunnel during flexion and entered into the carpal tunnel at a depth of approximately 2.5 cm during overextension, extruding the flexor tendon and median nerve (Figure 2A and B). After careful separation, the mass outside the capsule was completely resected. Continuous exploration indicated the abnormal muscle belly shift of the FDS. During hyperextension, the mass extended into the carpal tunnel and slightly extruded the median nerve and the flexor tendon (Figure 2C and D). After the removal of the muscle bundles and muscle membranes that were abnormally shifted down, the entrapment on the wrist disappeared during passive movements. The median nerve was released to eliminate local compression. After fully controlling bleeding, the incision was rinsed and closed layer-by-layer. Postoperatively, the mass was dissected, and the section was composed of homogenous, yellow fine adipose tissues, with no obvious lesions, such as fibrosis or necrosis of the muscle bundles. Pathological findings indicated an IML due to the presentation of mature adipose tissue and fibrous tissue (Figure 3). The morphology was IML.
Postoperative 1-year follow-up showed no recurrence of the tumor, no abnormalities in movement and sensation of the index and middle fingers, and negative signs of Tinel and Phalen signs of the median nerve of the wrist.
Trigger finger at wrist is a rare condition and was first reported by Eibel[4] in 1961. Most hand surgeons have no direct experience with trigger fingers at the wrist[1]. Suematsu et al[3] have classified the phenomenon of trigger finger into the following three categories: Class A trigger finger at the wrist is due to a tumor or a rheumatoid nodule occurring on the flexor tendon or tendon sheath, which enters and exits from the carpal tunnel; class B trigger finger at the wrist is due to an anomalous muscle belly (including an abnormal lumbrical muscle or abnormal muscle belly of the FDS); and class C trigger finger at the wrist is a combination of classes A and B[3]. Few cases of the above mentioned presentation caused by tumors, such as fibroma, rheumatoid nodule, and giant cell tumor, have been reported. However, IML has rarely been reported. In the present case, the trigger finger at the wrist was caused by the IML arising from the anomalous flexor digitorum muscle belly. Thus, our case was considered a class C trigger finger according to Suematsu’s classification[3]. In our case, intermittent median nerve compression was also associated with the trigger finger. This was probably due to the intermittent compression effect of the tumor movement while passing through the carpal tunnel.
Lipomas are common benign tumors of different sizes that usually occur under the skin or in the large muscles of the thigh, shoulder, or upper arm[5]. Some lipomas that occur in the muscle are called IMLs, and the first case of IML in the trapezius muscle was reported in 1853[6,7]. Most of the IMLs occur in the trunk and proximal limbs, and tumors located in the wrist and fingers are rarely reported[8,9]. In 1988, Brand and Gelberman[10] reported the first case of lipoma in FDS causing triggering at the carpal tunnel and median nerve compression. An IML is a histologically benign, painless, and slow-growing mass. The clinical manifestations are mainly determined by the tumor location. When the mass is too large and invades the muscle, its movement may be restricted. When the mass compresses the nerve and vessel, corresponding paresthesia will appear and may affect the joint function[11,12]. In this case, the IML of the FDS shifted synchronously with the index finger and its distal end entered into the carpal tunnel. Therefore, the increased contents of the carpal tunnel extruded the median nerve, resulting in the CTS.
Imaging examination is the most important auxiliary method for IML diagnosis[13]. Warwick et al[14] believed that ultrasound examination is the first choice for the diagnosis of soft tissue tumors, by dynamically observing the relationship between the location and depth of the tumor and adjacent tissues[14]. Under ultrasound, IML mostly manifests as a clear mass with echo intensity equivalent to that of the subcutaneous fat but higher than that of the muscle and often without blood flow signals[14]. When it is difficult to assess the complete anatomical relationship between lipomas and adjacent structures by ultrasound, or when lipomas are suspected of malignant tumors, further magnetic resonance imaging (MRI) or computed tomography (CT) examinations are required. IML shows high signals on T1 and T2-weighted images of MRI, and low signal on fat-suppressed T2-weighted images. CT images show a low-density intramuscular mass with a negative Hounsfield value, and the attenuation is similar to that of adipose tissue. Several soft-tissue density bands of varying thicknesses that are occasionally interrupted and represent the muscle fibers therein[14]. Accompanied ossification can be better depicted on CT images[15].
In this case, the lipoma located specially should be distinguished from malignant tumors, such as highly differentiated liposarcoma, clear cell sarcoma, and fibrosarcoma in addition to intramuscular hemangiomas, ganglion cysts, and giant cell tumors of the tendon sheath. Intramuscular hemangiomas are characterized by abnormal proliferation of blood vessels in the muscle tissue; ultrasound can detect and enrich venous blood flow signals. Ganglion cysts that occur in the flexor tendon of the hand can also cause symptoms similar to CTS, and they can be identified by ultrasound images[16]. Histopathological examination of a giant cell tumor of the tendon sheath indicates that the tumor is rich in multinucleated giant cells and hemosiderin deposits. IMLs differ in tissue type and degree of differentiation and vary in sonographic appearance. The identification of IMLs mainly depends on the histopathological examination. Microscopically, there are atypical cells or mixture of vacuolated lipoblasts and fibroblast-like spindles, which are often in the intermuscular septa with increased number and thickness. Moreover, there are some vascular components of different sizes, and inflammatory cells and mucus-like areas are often observed around the intermuscular septa[17-19].
Treatment of IML depends on tumor location, size, and clinical symptoms related to the lesion. Observation without treatment is applicable for a small lipoma that does not cause functional restrictions[20]. For patients with obvious signs and discomforts, the tumor can be removed by surgery. Currently, the recurrence rate of IML is believed to be very low. However, the recurrence rate after treatment has been historically reported to be between 3% and 62.5%[21-23]. The follow-up period ranges from several months to decades, and the specific period is determined by the investigators[21-23]. Relapses are thought to be due to the incomplete clearance of lipomas during surgery, which is most likely due to the tumors being adjacent to important anatomical structures or fear of limited functions resulting from complete removal of the affected muscles[7]. Therefore, tumor cytoreduction is also an acceptable option for tumors not suitable for complete resection or in the case of complete resection that can cause severe functional impairment[24]. Generally, chemotherapy and radiation therapy are generally not recommended due to the benign nature of IMLs[7].
In this case, the IML originated from the anomalous muscle belly of FDS and grew longitudinally along the tendon and shifted with the index finger during flexion and extension. The tumor was located outside the carpal tunnel during flexion and extension and entered into the carpal tunnel at a depth of 2.5 cm during overextension. There was slight numbness on the radial side of the thumb, index finger, and middle finger, which is defined as typical CTS caused by median nerve entrapment. The tumor and surrounding tissues were completely removed intraoperatively and showed that the muscle belly of the FDS was abnormally shifted down. The distal end of the muscle belly of the FDS moved with the index finger and partially entered into the carpal tunnel. Christensen[25] had proposed three types of anomalous muscle belly of the FDS: (1) The flexor digiti “superficialis” derived from the carpal ligament and the fascia palmaris or the tendon itself; (2) The elongated muscle bellies continuing through the carpal tunnel before becoming tendinous; and (3) A digastric type in which the palmar muscle belly replaces the tendon. This case belongs to the second type among them. As previously reported, the muscle belly of the FDS that is excessively shifted down is also the cause of CTS[1,26]. Particularly, when the symptoms of CTS are significantly related to physical activities, the presence of muscles with abnormal structures needs to be considered. Generally, MRI contributes to improving the accuracy of preoperative diagnosis[26]. For CTS caused by the anomalous muscle belly, location, size, and symptoms of the muscle belly determine whether a surgical treatment is required. Javed and Woodruff[27] believed that when the mass is unable to touch, only the release of the transverse carpal ligament is sufficient to eliminate completely the symptoms[27]. Beyond that, the removal of the abnormal muscle belly is necessary if the abnormal muscle belly can be reached and extended distally. Resection of the abnormal muscle belly can reduce the risk of recurrence or results in only partial remission after surgery, avoiding the need for secondary surgery[27]. In addition, resection of the muscle is recommended if a normal flexor digitorum profundus tendon is present, which warrants a normal range of motion of the finger[26]. In the present case, the symptoms of CTS were mild and considered to originate from the IML. Apart from tumor resection, resection of the anomalous muscle belly of the FDS was concurrently performed to relieve these symptoms. The patient had no recurrence and CTS symptoms during follow-up.
Triggering of the fingers at the wrist is rare. It must be noted that there are many possible causes and types of triggering or clicking around the wrist. Accurate diagnosis is mandatory to avoided inaccurate treatment of patients with trigger finger at the wrist. During the diagnosis and treatment of CTS, attention should be paid to the variation of tendon tissue in the carpal tunnel, to avoid focusing only on the release of transverse carpal ligament and ignoring the removal of anomalous muscle belly.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Diab RA, Papadakis M, Tawonsawatruk T, Yiğit Ş S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
| 1. | Bou-Merhi JS, Harris PG, Brutus JP. "Trigger finger at the wrist" due to anomalous flexor digitorum superficialis muscle belly within the carpal tunnel. Chir Main. 2007;26:238-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Berlund P, Kalamaras M. A case report of trigger wrist associated with carpal tunnel syndrome caused by an intramuscular lipoma. Hand Surg. 2014;19:237-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Suematsu N, Hirayama T, Takemitsu Y. Trigger wrist caused by a giant cell tumour of tendon sheath. J Hand Surg Br. 1985;10:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Eibel P. Trigger Wrist with Intermittent Carpal Tunnel Syndrome: A Hitherto Undescribed Entity with Report of a Case. Can Med Assoc J. 1961;84:602-605. [PubMed] |
| 5. | Kind M, Stock N, Coindre JM. Histology and imaging of soft tissue sarcomas. Eur J Radiol. 2009;72:6-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Regan JM, Bickel WH, Broders AC. Infiltrating benign lipomas of the extremities. West J Surg Obstet Gynecol. 1946;54:87-93. [PubMed] |
| 7. | McTighe S, Chernev I. Intramuscular lipoma: a review of the literature. Orthop Rev (Pavia). 2014;6:5618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 8. | Kalmar G, Doobay N. Intramuscular Lipoma of the Flexor Hallucis Brevis MuscleA Case Report. J Am Podiatr Med Assoc. 2017;107:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Rispoli L, Singh JR, Piesco J. Unusual Location of Intramuscular Lipoma Presenting as an Extensor Tendon Tear: A Diagnostic Dilemma. Am J Phys Med Rehabil. 2017;96:e162-e163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Brand MG, Gelberman RH. Lipoma of the flexor digitorum superficialis causing triggering at the carpal canal and median nerve compression. J Hand Surg Am. 1988;13:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Warner JJ, Madsen N, Gerber C. Intramuscular lipoma of the deltoid causing shoulder pain. Report of two cases. Clin Orthop Relat Res. 1990;110-112. [PubMed] |
| 12. | Dubyk F, Maqbool B, Gill AA, Fine S. Intramuscular lipoma originating in pectoralis major: A rare presentation of a large breast mass. Breast J. 2019;25:145-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Amirthalingam U. Atypical Imaging Features of a Simple Intramuscular Lipoma. J Clin Diagn Res. 2017;11:TD01-TD02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Warwick D, Kar S, Harris M. Ultrasound case report of a palmar lipoma causing carpal tunnel syndrome. Ultrasound. 2013;21:224-227. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Heffernan EJ, Lefaivre K, Munk PL, Nielsen TO, Masri BA. Ossifying lipoma of the thigh. Br J Radiol. 2008;81:e207-e210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Fletcher CD, Martin-Bates E. Intramuscular and intermuscular lipoma: neglected diagnoses. Histopathology. 1988;12:275-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 88] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Evans HL, Soule EH, Winkelmann RK. Atypical lipoma, atypical intramuscular lipoma, and well differentiated retroperitoneal liposarcoma: a reappraisal of 30 cases formerly classified as well differentiated liposarcoma. Cancer. 1979;43:574-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Ohguri T, Aoki T, Hisaoka M, Watanabe H, Nakamura K, Hashimoto H, Nakamura T, Nakata H. Differential diagnosis of benign peripheral lipoma from well-differentiated liposarcoma on MR imaging: is comparison of margins and internal characteristics useful? AJR Am J Roentgenol. 2003;180:1689-1694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Billing V, Mertens F, Domanski HA, Rydholm A. Deep-seated ordinary and atypical lipomas: histopathology, cytogenetics, clinical features, and outcome in 215 tumours of the extremity and trunk wall. J Bone Joint Surg Br. 2008;90:929-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Presman B, Jauffred SF, Kornø MR, Petersen MM. Low Recurrence Rate and Risk of Distant Metastases following Marginal Surgery of Intramuscular Lipoma and Atypical Lipomatous Tumors of the Extremities and Trunk Wall. Med Princ Pract. 2020;29:203-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Ramos-Pascua LR, Guerra-Álvarez OA, Sánchez-Herráez S, Izquierdo-García FM, Maderuelo-Fernández JÁ. [Intramuscular lipomas: Large and deep benign lumps not to underestimated. Review of a series of 51 cases]. Rev Esp Cir Ortop Traumatol. 2013;57:391-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Garavaglia J, Gnepp DR. Intramuscular (infiltrating) lipoma of the tongue. Oral Surg Oral Med Oral Pathol. 1987;63:348-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Song HJ, Hong WK, Lee HS, Shin JH, Choi GS. Intramuscular lipoma of the sternocleidomastoid muscle. J Eur Acad Dermatol Venereol. 2008;22:363-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Su CH, Hung JK, Chang IL. Surgical treatment of intramuscular, infiltrating lipoma. Int Surg. 2011;96:56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Christensen S. Anomalous muscle belly of the flexor digitorum superficialis in two generations. Hand. 1977;9:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Honing ML, Ritt MJ, Bos KE. An anomalous flexor digitorum superficialis to the index finger. Surg Radiol Anat. 1995;17:339-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Javed S, Woodruff M. Carpal tunnel syndrome secondary to an accessory flexor digitorum superficialis muscle belly: case report and review of the literature. Hand (N Y). 2014;9:554-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |