Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7558
Peer-review started: March 2, 2021
First decision: April 29, 2021
Revised: May 9, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: September 6, 2021
Processing time: 181 Days and 11.7 Hours
Based on the location and size of the fracture block, open reduction and internal fixation can be employed or assisted for shoulder arthroscopy in the treatment of glenoid fractures. However, the treatment of lower part of glenoid fractures through a novel axillary approach has not been reported so far.
A 22-year-old right-handed man was transferred to our outpatient clinic because of right shoulder injury during a traffic accident. X-ray examination after admission suggested the fracture of the lower part of the right glenoid and an ipiselial proximal humeral fracture. Three-dimensional (3D) computed tomography (CT) further suggested that the size of the fracture block of the lower part of the right glenoid was 3.4 mm × 16.2 mm. The patient was diagnosed as the fracture of the lower part of the glenoid, also known as bony Bankart lesion without shoulder dislocation. After general anesthesia, the patient was surgically treated with the open reduction internal fixation through a novel axillary approach. 3D CT and shoulder joint function were reexamined at 12 mo of follow-up, showing acceptable recovery.
This case report describes a novel axillary approach adopted in an open reduction with cannulated screw and wire anchor internal fixation. After a follow-up for more than 12 mo, 3D CT and shoulder joint function examinations display a good recovery.
Core Tip: Based on the location and size of the fracture block, open reduction and internal fixation can be employed or assisted for shoulder arthroscopy in the treatment of glenoid fractures. However, the treatment of lower part of glenoid fractures through a novel axillary approach has not been reported so far. This study reports a case with lower part of glenoid fracture and treated with open reduction with cannulated screw and wire anchor internal fixation through a novel axillary approach. After a follow-up for more than 12 mo, reexaminations of three-dimensional computed tomography and shoulder joint function display a good recovery.
- Citation: Jia X, Zhou FL, Zhu YH, Jin DJ, Liu WX, Yang ZC, Liu RP. Treatment of lower part of glenoid fractures through a novel axillary approach: A case report. World J Clin Cases 2021; 9(25): 7558-7563
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7558.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7558
Generally speaking, scapular fractures are often caused by high-energy trauma in traffic accidents[1]. Intra-articular fractures account for 1% of scapular fractures[2]. Glenoid fractures take up nearly 0.1% of total body fractures and 10% of scapular fractures[3]. The treatment of glenoid fracture depends on the size and displacement of the fracture fragments, including non-surgical treatment, open surgery, or open surgery with arthroscopy[4]. Schofer et al[5] suggested that the functional effects are significant after the conservative treatment of scapular fractures. However, Rollo et al[6] considered that non-surgical treatment of scapular fractures may cause pain, vascular problems, delayed union, malunion, persistent shoulder symptoms, or loss of arm function. Most of the Bankart lesions in the anterior and posterior glenoid fractures and superior labrum anterior and posterior lesions to the glenoid can be treated by surgery under arthroscopy[7-9]. However, the lower part of the glenoid fractures, especially large fracture masses, are difficult to be surgically treated with arthroscopic reduction and fixation, and open reduction internal fixation (ORIF) is recognized as a better choice for these specific cases[1,8]. It is generally known that the axillary has a relatively complex anatomical structure, and there are considerably important blood vessels and nerves passing through the axillary.
Accordingly, a novel axillary approach should be adopted during surgical treatment of the lower part of glenoid fractures, which can prevent the damage to the axillary vessels and nerves as much as possible, but clearly expose the fracture area of the subaxillary glenoid. Thus, a novel axillary approach from the muscle space was desig
A 22-year-old right-handed man suffered from right shoulder pain for 24 h because of the traffic accident.
The patient had right shoulder pain with limited movement, and could not raise the right arm. No abnormal sensation in the right upper limb was examined.
The patient denied the history of right shoulder disease and operation.
Physical examinations showed right shoulder tenderness, limited movement of the right shoulder, no numbness, limited finger movement, and vascular injury.
The results of preoperative laboratory examinations were normal.
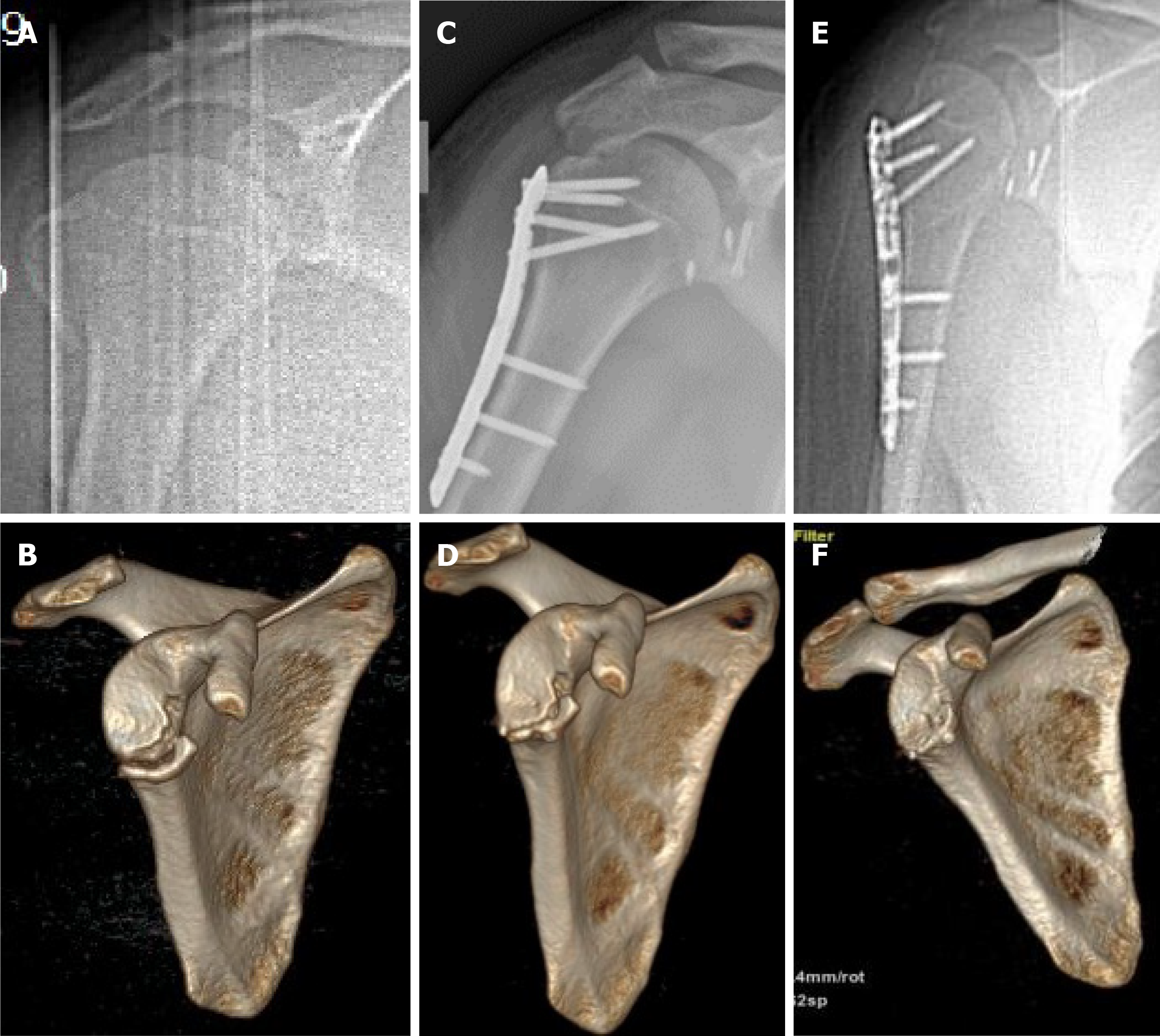
X-ray examination after admission suggested the lower part of the right glenoid fracture with an ipiselial proximal humeral fracture (Figure 1A). Three-dimensional (3D) computed tomography (CT) further suggested that the size of the fracture block was 3.4 mm × 16.2 mm (Figure 1B).
According to the history and preoperative imaging examination, the patient was finally diagnosis as the lower part of the right glenoid fracture with an ipiselial proximal humeral fracture.
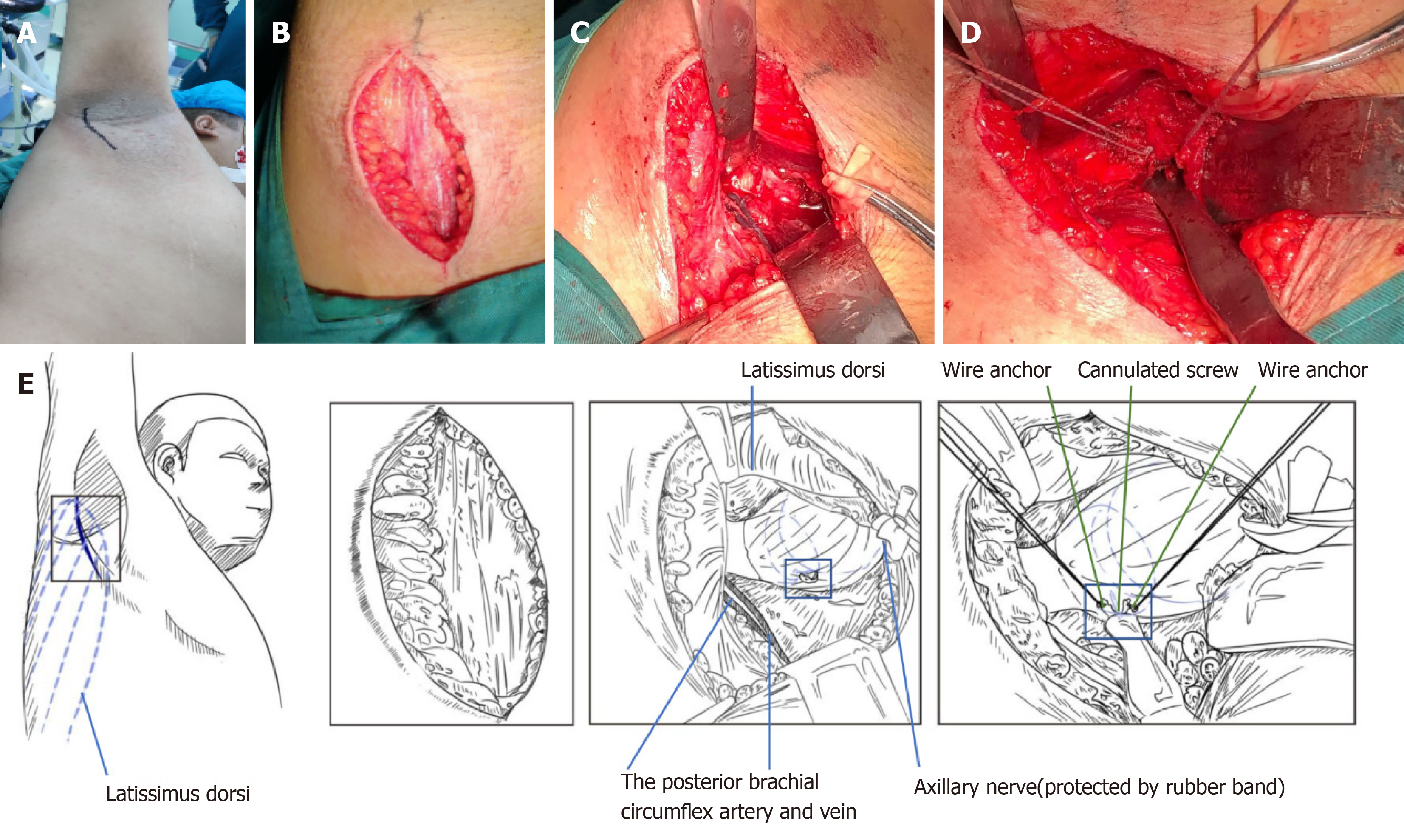
On day 5 after the injury, the patient was surgically treated by ORIF through a novel axillary approach following general anesthesia. The patient was placed on a fluoroscopic operating table in a lateral position. A longitudinal incision was made in the armpit, followed by exposure of the anterior edge of the latissimus dorsi by separating subcutaneous tissues (Figure 2A and B). The axillary nerve under the latissimus dorsi was exposed and separated, which was traversed from the medial side of the armpit to the lateral side. Subsequently, the posterior brachial circumflex artery and vein, under the axillary nerve, were exposed. The blood vessels and nerves were protected by a tender traction. Next, the joint capsule of lower part of the glenoid was exposed between the gap of axillary nerve and circumflex blood vessel (Figure 2C and D). Moreover, the joint capsule was cut transversely to expose the fracture block, fracture end and articular surface of the glenoid. Anatomic reduction was achieved under a direct vision. After the fracture reduction, two 1.5 mm fine Kirschner wires were used for temporary fixation, and then the fracture block was fixed with one cannulated screw (3 mm in diameter, 18 mm in length), and then two 2.7 mm wire anchors were used to strengthen the fixation (Figure 2E). After removal of the glenohumeral joint under a direct vision, the fracture block was exposed and fixed stably. The gauze equipment was counted, and the wound was washed and sutured layer by layer.
Another anteromedial approach of the shoulder joint under the same body position was adopted for surgical treatment of the ipsilateral proximal humeral fracture. After open reduction, the proximal humeral locking plate was used for fixation.
The patient’s forearm was suspended for 3 wk postoperatively. Postoperative exercises of the elbow, wrist and hand were encouraged during the first 3 wk. A passive range of motion exercises were initiated at the third wk. At the sixth wk, patients were instructed to start active auxiliary exercises. During the follow-up period for more than 12 mo, imaging (including facture of subaxillary glenoid and ipsilateral proximal humeral) (Figure 1) and functional examinations were conducted (Table 1).
| Case number | Sex | Age (yr) | Mechanism of Injury | Ideberg fracture classification | Follow-up time (mo) | Postoperative constant score | Postoperative bone healing |
| 1 | Male | 22 | Traffic accident | Type II | 12 | 95 | Bony union |
Ideberg classification of scapular fractures is the most common classification of intra-articular glenoid fractures. The classification system is modified by Goss, involving 6 types of fractures[10]. Among them, type II fractures are those of the lower part of the glenoid, which induce the instability and dislocation of the shoulder joint[11]. If surgical treatment is required, reduction and wire anchor fixation for small fractures can be performed under the shoulder arthroscopy. However, arthroscopic reduction and fixation are difficult to be performed in cases with large fracture masses or those with the scapular neck involved. van Oostveen et al[12] believed that appropriate surgical methods according to different types of fractures can achieve satisfactory results.
In this study, a novel axillary approach in the lateral decubitus position was designed. It is generally known that the axillary has a relatively complex anatomical structure, and there are considerable important blood vessels and nerves passing through the axillary. Vascular and nerve damage can be easily caused because of the complicated anatomical structure. The axillary approach proposed in this study was a novel approach initiated from the anterior edge of the latissimus dorsi and passed through the space between the axillary nerve and the circumflex scapular vessel (Figure 2). This approach can avoid the main blood vessels and nerves in the armpit, which also directly enters to the subscapular fracture area. Moreover, the proposed approach had multiple advantages like an easy exposure of the operation area, a direct access to the surgical site, achievement of fracture reduction and fixation under a direct vision, and prevention of the axillary nerve and vessel damages.
In the present study, the Constant score of shoulder joint reached 95 in the patient with inferior rim fractures of the glenoid after surgical treatment, which was better than the average Constant score of 82 reported by Bartoníček et al[13].
Shoulder arthroscopy has great advantages in the treatment of Bankart lesions[14,15]. Generally speaking, surgery is preferred to displaced glenoid fossa fractures[16]. However, when the shoulder arthroscopy fails to reduce and fix scapular glenoid fractures with other parts of the scapula, ORIF is a good choice[17,18]. Besides, ORIF is also suitable for fractures of the lower part of glenoid. Thus, the axillary approach was developed here. Besides the reduction and internal fixation of fresh fractures, the novel axillary approach was also proven to be a very good choice for patients with bone lesions, cysts, old fracture nonunion and subluxation of shoulder joint around the lower part of glenoid.
This case report describes a novel axillary approach adopted in the open reduction with cannulated screw and wire anchor internal fixation. The patient was surgically treated by ORIF through the novel axillary approach following general anesthesia. After a follow-up for more than 12 mo, 3D CT and shoulder joint function reexaminations showed a good recovery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand P S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Cole PA, Gauger EM, Schroder LK. Management of scapular fractures. J Am Acad Orthop Surg. 2012;20:130-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Gilbert F, Eden L, Meffert R, Konietschke F, Lotz J, Bauer L, Staab W. Intra- and interobserver reliability of glenoid fracture classifications by Ideberg, Euler and AO. BMC Musculoskelet Disord. 2018;19:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Sen RK, Sud S, Saini G, Rangdal S, Sament R, Bachhal V. Glenoid fossa fractures: Outcome of operative and nonoperative treatment. Indian J Orthop. 2014;48:14-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Seidl AJ, Joyce CD. Acute Fractures of the Glenoid. J Am Acad Orthop Surg. 2020;28:e978-e987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Schofer MD, Sehrt AC, Timmesfeld N, Störmer S, Kortmann HR. Fractures of the scapula: long-term results after conservative treatment. Arch Orthop Trauma Surg. 2009;129:1511-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Rollo G, Huri G, Meccariello L, Familiari F, Çetik RM, Cataldi C, Conteduca J, Giaracuni M, Bisaccia M, Longo D, Giannotti PS. Scapular body fractures: Short-term results of surgical management with extended indications. Injury. 2021;52:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Corradini A, Campochiaro G, Gialdini M, Rebuzzi M, Baudi P. Arthroscopic repair of glenoid rim fractures: a ligamentotaxis surgical technique. Musculoskelet Surg. 2018;102:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Noguchi T, Mautner JF, Duncan SFM. Dorsal Plate Fixation of Scapular Fracture. J Hand Surg Am. 2017;42:843.e1-843.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Park JY, Lee JH, Oh KS, Chung SW, Park H, Park JY. Does anchor insertion angle or placement of the suture anchor affect glenoid rim fracture occurrence after arthroscopic Bankart repair? J Shoulder Elbow Surg. 2020;29:e124-e129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am. 1992;74:299-305. [PubMed] |
| 11. | Griesser MJ, Harris JD, McCoy BW, Hussain WM, Jones MH, Bishop JY, Miniaci A. Glenoid fracture after Bristow-Latarjet shoulder stabilization: a case report and review of the literature. J Shoulder Elbow Surg. 2013;22:e17-e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | van Oostveen DP, Temmerman OP, Burger BJ, van Noort A, Robinson M. Glenoid fractures: a review of pathology, classification, treatment and results. Acta Orthop Belg. 2014;80:88-98. [PubMed] |
| 13. | Bartoníček J, Tuček M, Klika D. Inferior glenoid fossa fractures: patho-anatomy and results of operative treatment. Int Orthop. 2017;41:1741-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Park JY, Lee JH, Chung SW, Oh KS, Noh YM, Kim SJ. Does Anchor Placement on the Glenoid Affect Functional Outcome After Arthroscopic Bankart Repair? Am J Sports Med. 2018;46:2466-2471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Tauber M, Moursy M, Eppel M, Koller H, Resch H. Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc. 2008;16:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Kannan S, Singh HP, Pandey R. A systematic review of management of scapular fractures. Acta Orthop Belg. 2018;84:497-508. [PubMed] |
| 17. | Plachel F, Schanda JE, Ortmaier R, Auffarth A, Resch H, Bogner R. The "triple dislocation fracture": anterior shoulder dislocation with concomitant fracture of the glenoid rim, greater tuberosity and coracoid process-a series of six cases. J Shoulder Elbow Surg. 2017;26:e278-e285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Uzel AP, Laflamme GY. [Fracture of the glenoid cavity Goss-Ideberg type II with inferior dislocation of the shoulder]. Chir Main. 2009;28:260-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |