Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7520
Peer-review started: February 15, 2021
First decision: March 11, 2021
Revised: March 29, 2021
Accepted: July 6, 2021
Article in press: July 6, 2021
Published online: September 6, 2021
Processing time: 197 Days and 5.2 Hours
Lung cancer with pulmonary tuberculosis (TB) refers to the occurrence of lesions simultaneously or sequentially in the lung(s) of the same patient, and the pathological examination and sputum TB examination diagnose them as lung cancer and TB, respectively. The occurrence of endobronchial TB (EBTB) with endobronchial tumor sequentially in the same bronchus lesion of the same patient is relatively rare.
A 62-year-old female patient was admitted to a local hospital on June 18, 2019 after a 3-mo history of dyspnea. She was a farmer and had no history of smoking and alcohol misuse. The patient had neither family nor work contact indicating exposure to TB. Emergency chest computed tomography (CT) examination showed that the right main bronchus was occupied and malignant tumor was possible. Histopathologic examination of a bronchial biopsy showed granulomatous inflammation with caseification and the presence of acid fast bacilli (AFB). However, after 6 mo of antitubercular treatment, repeat bronchoscopy and biopsy histological examination showed squamous cell carcinoma. The patient has started on systemic chemotherapy with carboplatin. After another two cycles of therapy, chest CT showed complete resolution of the lesions. Bronchoalveolar lavage and bronchial aspirate were negative for AFB and cancer cells.
It is not only more likely that a patient presenting with what appears to be TB will concurrently have a pulmonary malignancy than someone who does not have a TB infection, but also that it is of greater urgency to make an expedited diagnosis of the malignancy.
Core Tip: In the correct clinical setting, lesions such as those seen during bronchoscopy should alert the physician to the possibility of active tuberculosis (TB). With the advancement of diagnostic techniques, the screening of high-risk populations of patients with lung cancer, and the prolongation of postoperative survival rates, and the close follow-up of lung cancer patients with TB, it is expected that TB can be detected in an early stage with a good prognosis after treatment.
- Citation: Jiang H, Li YQ. Coexistence of tuberculosis and squamous cell carcinoma in the right main bronchus: A case report. World J Clin Cases 2021; 9(25): 7520-7526
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7520.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7520
Lung cancer with pulmonary tuberculosis (TB) refers to the occurrence of lesions simultaneously or sequentially in the lung(s) of the same patient, and the pathological examination and sputum TB examination diagnose them as lung cancer and TB, respectively. The pulmonary TB can be active or inactive.
The coexistence of lung cancer and TB has previously been reported and some studies suggest that TB lesion is an independent prognostic factor for lung cancer. The risk of lung cancer in TB patients was three times that in patients without TB. Paulin et al[1] demonstrated that malignancies intensify immune disorder, which may raise the probability of TB and latent TB recurrence.
Unlike other cases of TB, reports of the association between endobronchial TB (EBTB) and bronchial cancer are rare. Pulmonary TB together with bronchus squa
A 62-year-old female patient was admitted to a local hospital on June 18 2019 after a 3-mo history of dyspnea.
The patient was healthy.
The patient was a farmer and had no history of smoking and alcohol misuse. She had no history of tuberculosis or other previous chronic disease. The patient had neither family nor work contact indicating exposure to TB.
Physical examination disclosed no abnormalities. The patient had a body mass index of 29.6. She denied losing weight in the past 6 mo.
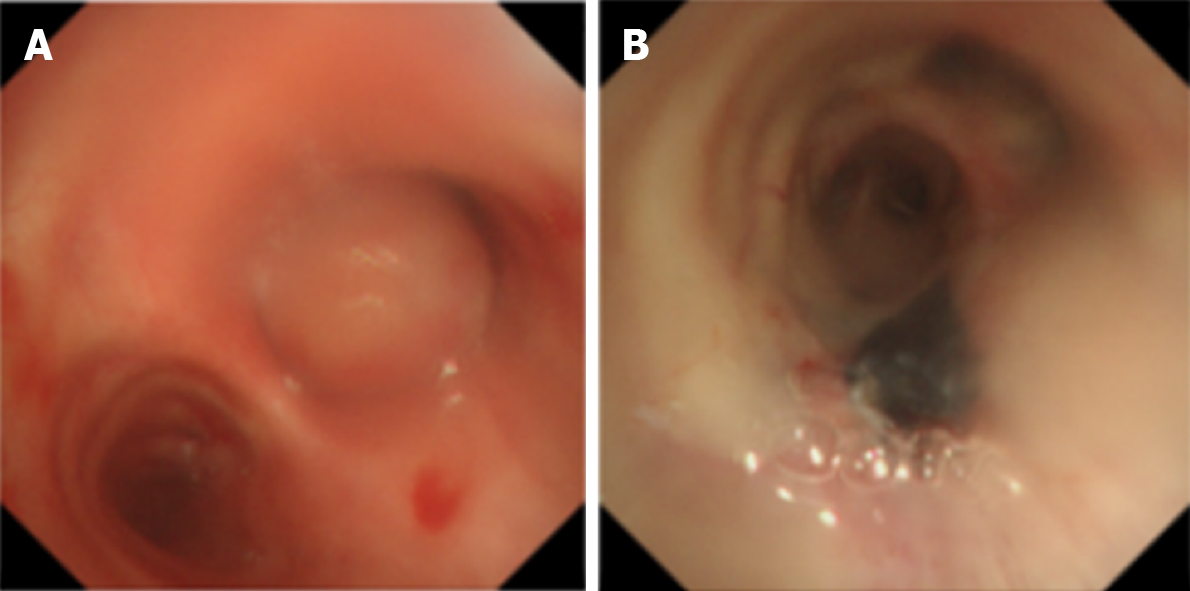
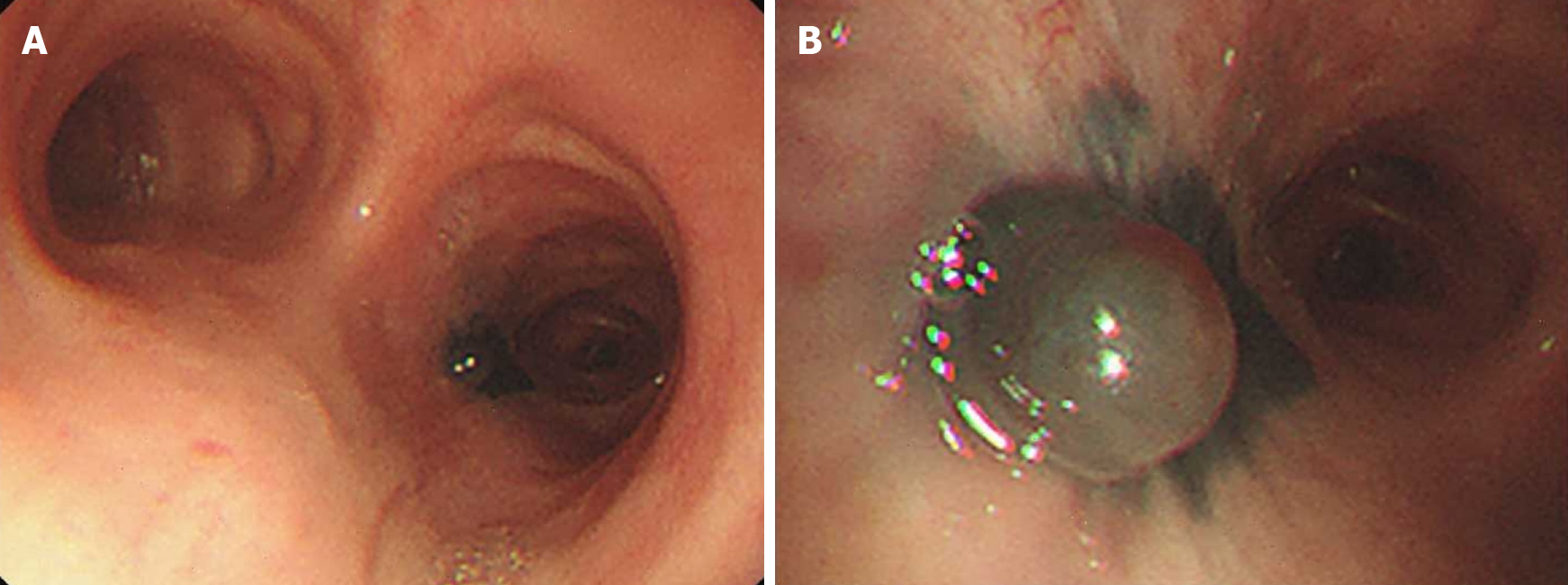
Tumor markers, TB antibody test, tuberculin skin test, and interferon gamma release assay were also negative. Sputum smear was negative for acid fast bacilli (AFB). Considering the possibility of bronchus cancer with lymph node metastasis, biopsy was suggested. On bronchoscopy, a tumorous growth obstructing around 90% of the right main bronchus was seen (Figure 1). The remaining bronchi were passable, without lesions. Reviewing the chest CT images, we found that the mass in the right main was easy to see, but the histology of mass was hard to identify on CT images. And this was also the reason why bronchoscopy was required.
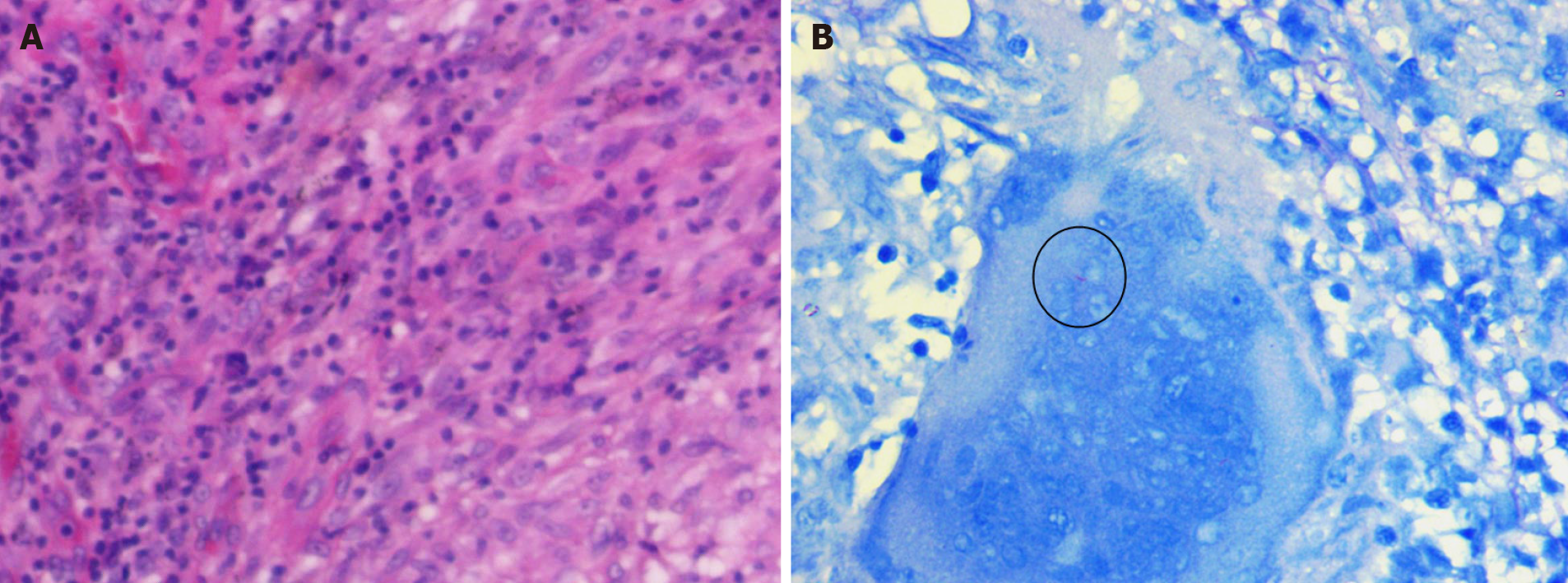
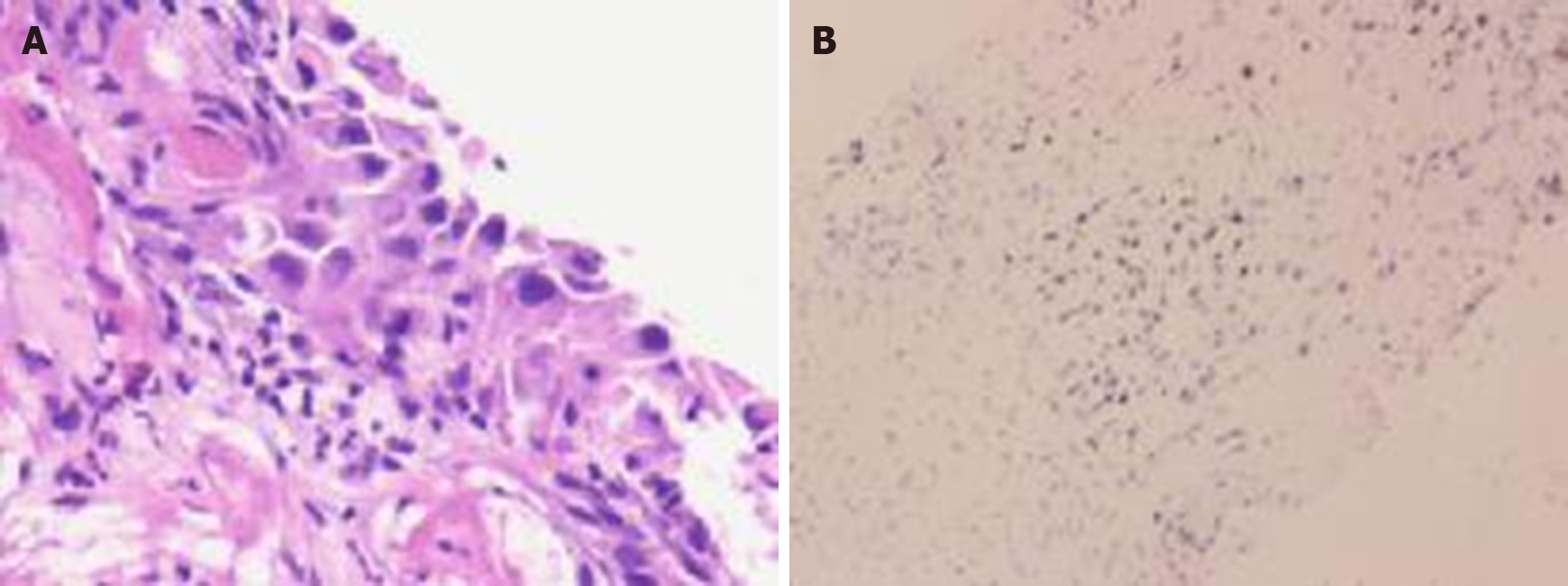
No distant metastasis or abdominal lymph node metastasis was found on CT examination. Tumorous mass resection via bronchoscopy under general anesthesia was performed, and the wound was ligated by use of a high frequency snare and cleaned up with an endotherm knife. Biopsy of the tumorous mass was performed for histological and cytological examinations. Histopathologic examination revealed well-defined caseating granuloma, and the biopsy was positive for AFB (Figure 2), and Xpert Mycobacterium tuberculosis (MTB)/rifampicin assay of the biopsy sample was weakly positive.
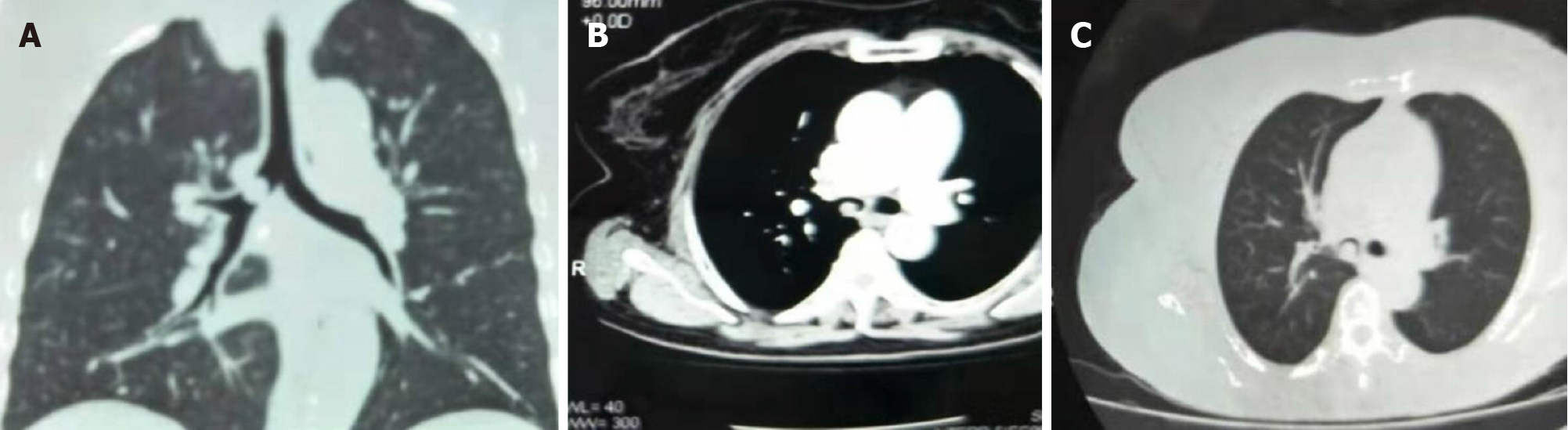
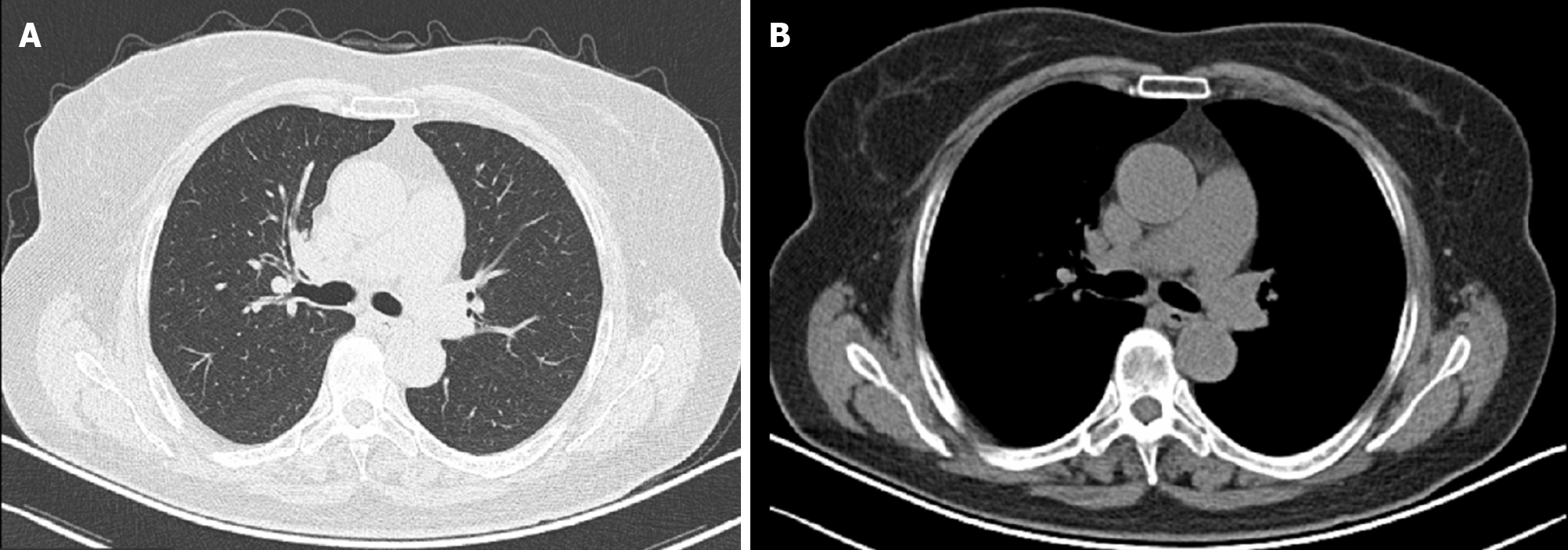
Emergency chest computed tomography (CT) examination showed that the right main bronchus was occupied (1.2 cm × 1.0 cm) and a malignant tumor was suspected (Figure 3).
Endobronchial MTB infection.
The patient was given standard anti-tuberculosis treatment with isoniazid, rifampicin, ethambutol, and pyrazinamide as per the national standard treatment guidelines.
Chest CT after 6 mo of therapy (December 23, 2019) showed that bronchial narrowing and airspace consolidation in the right main bronchus (5 mm × 4 mm) (Figure 4), but the size of mass was smaller than that at the first admission, without bronchial wall thickening, and lymphadenopathy in the mediastinal was considered to be mediastinal lymph node metastasis.
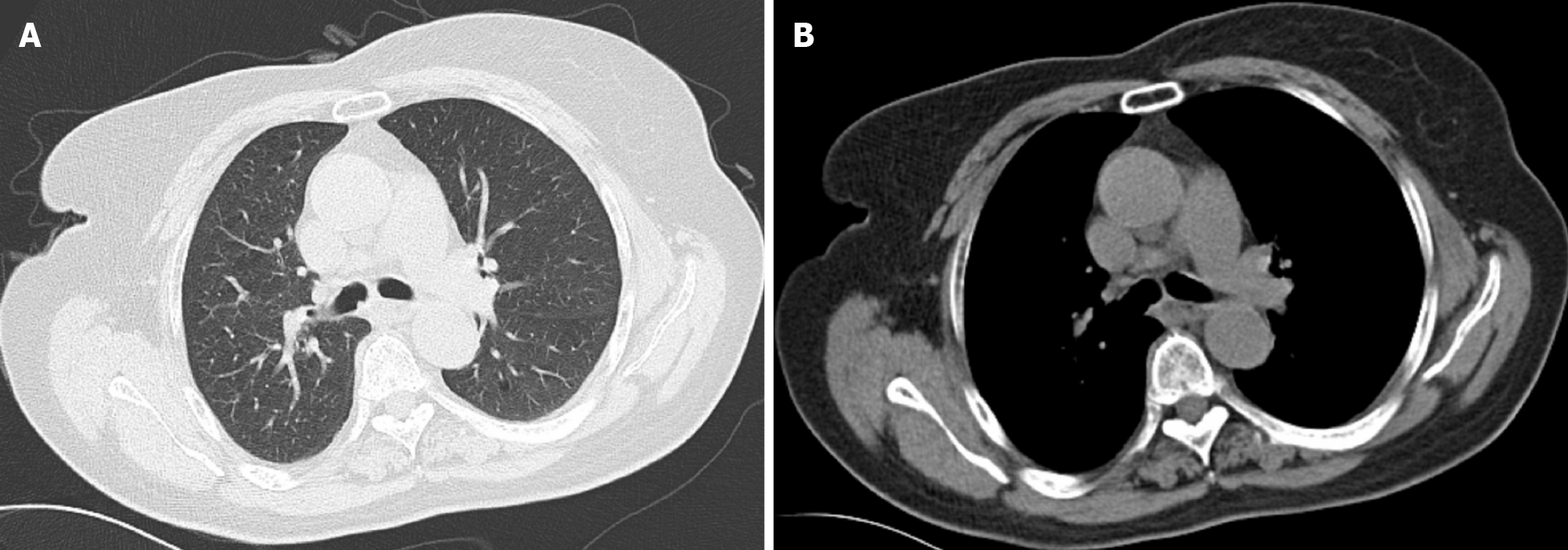
Laboratory examination revealed elevated tumor markers including CEA (4 ng/mL), CA125 (2 U/mL), NSE (3 ng/mL), SCC antigen (14 mg/L), CYFRA211 (41.2 ng/mL), and ProGRP (4 pg/mL). On bronchoscopy, a shiny black vesicular lesion was found in the right main bronchus (Figure 5). Mucosal punch biopsies were then obtained from the lesion. Poorly differentiated SCC was cytologically and histologically verified. Immunohistochemistry staining showed that the tumor cells were positive for P63, P40, CK7, CK(Pan), Ki67, and p53, but negative for TTF-1, NapsinA, SOX2, SALL4, and CD34 (Figure 6). Although the tumor was tiny, it invaded the main trachea, was very close to the carina, and was staged as IIIB (T4N2M0). Owing to the anatomic location of the tumor, surgical resection was not advised. Oncologists had suggested anticancer chemotherapy combined with anti-tuberculosis treatment so as not to increase the occurrence of complications or result in a negative outcome. On the basis of clinical studies, the NCCN guidelines recommend that cisplatin combined with gemcitabine be preferred for squamous cell NSCLC. The patient had started on systemic chemotherapy with cisplatin combined with gemcitabine. After 3 mo of therapy (March 20, 2020), chest CT showed complete resolution of the lesion (Figure 7). Bronchoalveolar lavage and bronchial aspirate were negative for AFB and cancer cells. The patient has been followed for 9 mo so far. She is currently on anti-tuberculosis medication combined with anticancer chemotherapy.
In 1810, the coexistence of pulmonary TB and lung cancer was first described, which poses significant challenges for their diagnosis and treatment[2]. Among the exposures associated with the risk for lung cancer, a history of chronic pulmonary disease, especially tuberculosis, is one potentially important factor[3].
Several case series and case-control studies on this association have been well-documented, but the association between lung TB and lung carcinoma is still controversial[4]. Studies have proposed that chronic inflammation in the lungs due to TB could cause clastogenic activity in the DNA of bronchial epithelium. Another hypothesis is lateral gene transfer. Since MTB is an intracellular organism, bacterial DNA could integrate into bronchial epithelial cells to induce neoplastic transformation[5,6]. In addition, lung carcinogenesis (LC) during the course of chronic TB was more pronounced in animals with severe lung tissue damage mediated by TB susceptibility locus[7].
Several studies have shown a significantly increased lung cancer risk associated with preexisting TB, and the association of preexisting TB with adenocarcinoma was significant. In a case series of LC in Ankara, SCC was the most common cancer, and LC had a more peripheral origin and was squamous cell carcinoma histopathologically[8]. In this patient, it is significant that EBTB was diagnosed before SCC, and the main cancer lesion was tiny; however, the lesions of SCC and EBTB were located in the same bronchial region. Therefore, we should not exclude the possibility that the histological type of LC depends on the anatomical location.
Considering that the immune suppression caused by cyclic anticancer chemo
In the correct clinical setting, lesions such as those seen during bronchoscopy should alert the physician to the possibility of an active MTB infection[10]. With the advancement of diagnostic techniques, the screening of high-risk populations for lung cancer, and the prolongation of postoperative survival and close follow-up of lung cancer patients with tuberculosis, it is expected that TB can be detected in an early stage with a good prognosis after treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velikova T S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Paulin LM, West NE, Akulian JA, Garibaldi BT. Endobronchial tuberculosis with anthracofibrosis. Am J Respir Crit Care Med. 2014;190:226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Hanaoka J, Ohuchi M, Kaku R, Okamoto K, Ohshio Y. Bronchoscopic balloon dilatation combined with laser cauterization of high and long segmental tracheal stenosis secondary to endobronchial tuberculosis: A case report. Respir Med Case Rep. 2019;28:100917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Parker CS, Siracuse CG, Litle VR. Identifying lung cancer in patients with active pulmonary tuberculosis. J Thorac Dis. 2018;10:S3392-S3397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Cevizci MN, Kara SS, Dokucu Aİ. Endobronchial Tuberculosis Mimicking Foreign Body Aspiration. Pediatr Neonatol. 2016;57:158-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Chan ED. Are there common threads in the susceptibility to cancer and tuberculosis? J Thorac Dis. 2020;12:1776-1780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Liang HY, Li XL, Yu XS, Guan P, Yin ZH, He QC, Zhou BS. Facts and fiction of the relationship between preexisting tuberculosis and lung cancer risk: a systematic review. Int J Cancer. 2009;125:2936-2944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 180] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Çakar B, Çiledağ A. Evaluation of coexistence of cancer and active tuberculosis; 16 case series. Respir Med Case Rep. 2018;23:33-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Molina-Romero C, Arrieta O, Hernández-Pando R. Tuberculosis and lung cancer. Salud Publica Mex. 2019;61:286-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Cukic V. The Association Between Lung Carcinoma and Tuberculosis. Med Arch. 2017;71:212-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Levin E, Bowling MR. Malignancy in the tracheal bronchus: A case series and review of the literature. Clin Respir J. 2018;12:2441-2445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |