Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7504
Peer-review started: March 8, 2021
First decision: March 25, 2021
Revised: April 5, 2021
Accepted: July 14, 2021
Article in press: July 14, 2021
Published online: September 6, 2021
Processing time: 175 Days and 22.4 Hours
Polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes (POEMS) syndrome is a rare paraneoplastic syndrome caused by a plasma cell proliferative disorder. The syndrome is characterized by elevated plasma cells, platelets, and vascular endothelial growth factor levels. Although heart disease rarely occurs in POEMS syndrome, the death rate increases sharply after heart failure. We report a patient who initially presented with an endocrine disease and developed congestive heart failure related to POEMS syndrome 9 years later.
A 23-year-old woman with no history of menstruation and a 9-year history of type I diabetes reported feeling breathless after activities. She could not lie down and rest at night. Three months prior, she experienced pain and increased tension in her left thigh accompanied by tenderness and edema in both lower extremities. The chief complaint upon hospital admission was that blood sugar has increased for more than 9 years, pain in the left thigh, and edema in both legs for more than 2 mo. After a multisystem evaluation, she was diagnosed with POEMS syndrome. Her echocardiogram showed left ventricular dilation with systolic dysfunction, and the left ventricular ejection fraction was only 38% with severely elevated brain natriuretic peptide. She received a combination of dexamethasone and thalidomide for 1 mo, but her symptoms did not improve. Therefore, we added a two-per-week bortezomib injection. After 2 wk, the patient’s heart function had improved significantly.
This case provides information about the treatment of POEMS syndrome with complications and highlights the challenges of developing a standardized treatment.
Core Tip: The standardized treatment for multiple myeloma may become the first reference for the treatment of polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes (POEMS) syndrome. We believe that the treatment effect for POEMS syndrome is poor once heart failure occurs. Therefore, early identification of heart disease and its cause along with timely follow-up treatment are critical to the treatment of POEMS syndrome. Whether this patient continues to undergo peripheral blood stem cell transplantation treatment after drug treatment remains to be evaluated. To date, the surgical indications and results have not been well defined, and a method for preventing heart disease has not been established for POEMS patients without heart failure.
- Citation: Fu LY, Zhang HB. Effective treatment of polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes syndrome with congestive heart failure: A case report. World J Clin Cases 2021; 9(25): 7504-7511
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7504.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7504
Polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes (POEMS) syndrome is a rare paraneoplastic syndrome caused by a plasma cell proliferative disorder that is most commonly lambda restricted. This complex multisystem disease may involve angiogenesis and proinflammatory cytokines. For example, upregulation of various proinflammatory cytokines and growth factors [tumor necrosis factor-alpha, interleukin (IL)-1, IL-6, and above all, vascular endothelial growth factor (VEGF)] plays a crucial role in the pathogenesis of POEMS syndrome, contributing to vascular leakage and polyneuropathy. Cases of POEMS syndrome with heart failure are rare. Given the limited experiences with early diagnoses and follow-up treatments, no clinically standardized treatment is available. However, reports have described effective treatment methods[1] as well as methods of observing heart disease in patients with POEMS syndrome[2]. This case report describes a patient with POEMS syndrome and heart failure who has not yet received high-dose chemotherapy with peripheral blood stem cell transplantation (PBSCT), dexamethasone, or thalidomide.
A 23-year-old Chinese woman with overall poor physical development was admitted to the hospital because her blood sugar had increased over 9 years. In addition, her left thigh was swollen and painful, and her lower extremities showed edema.
The patient had been diagnosed with type I diabetes 9 years before she came to the hospital. However, she was not treated with regular insulin injections outside the hospital, and her blood sugar was not well controlled. One year ago, she felt tired after exercise and could not lie down at night; she also felt squeezing in her chest area during defecation. She felt pain in her left thigh pain and increased tension that had occurred more than 3 mo earlier accompanied by tenderness, edema in both lower extremities, paleness, swelling, and ulceration. Initially, she could walk autonomously but gradually became unstable while standing, even finding it difficult to squat during bowel movements.
“Cataractectomy” was performed 1 year ago.
Menarche had not occurred to date, and she was diagnosed with a naive uterus outside our hospital. The family history was unremarkable.
The parameters of vital signs were as follows: Heart rate, 107 beats/min; BP 110/78 mmHg; height, 145 cm; and weight, 45 kg. The skin and mucous membranes of the whole body were pale. There was no pubic or axillary hair, and multiple areas of the skin were damaged and crusted. On auscultation, the breath sounds in both upper lungs were thick and weak, and moist rales were heard in both lower lungs. The abdomen was distended. The liver and spleen were unaffected and moved upon respiration. There was positive dullness and pitting edema of both lower limbs. There were no other obvious abnormalities.
The patient’s laboratory results are listed in Table 1. Endocrine examination revealed hypothyroidism and hypogonadotropic hypogonadism. The patient’s brain natriuretic peptide (BNP) was severely elevated.
| Hematology | Serum chemistry | Endocrinology |
| WBC (7.71 × 109/L) | α1 (8.5%) | LH (0.02 mIU/mL) |
| Neu (65.4%) | γ (30.9%) | FSH (0.95 mIU/mL) |
| RBC (2.88 × 1012 /L) | Alb (22 g/L) | GH (11.69 ng/mL) |
| HB (85 g/dL) | cTnT (0.188 μg/L) | T3 (0.54 nmol/L) |
| Hct (28%) | Mb (272.8 ng/mL) | T4 (5.26 nmol/L) |
| PLT (360 × 109/L) | CK-MB (12.7 U/L) | TSH (17.634 mU/L) |
| BNP (5487 pg/mL) | PTH (51.6 ng/L) | |
| Urinalysis | PT (16.5 s) | IGF-1 (< 25.0 ng/mL) |
| PTR (1.43) | VEGF (9800 pg/mL) | |
| Protein (1921 μmol/dL) | INR (1.45) | IgG (23.90 g/L) |
| M protein (0.27 g/L) | Fbg (3.95 g/L) | IgA (5.04 g/L) |
| KET (++) | ALB (26 g/L) | HbA1c (8.10%) |
| AST (30 U/L) | ||
| ALT (25 U/L) | ||
| BUN (7.4 mmol/L) | ||
| CRE (50 μmol/L) | ||
| UA (408 μmol/L) | ||
| Na (135 mmol/L) | ||
| K (4.8 mmol/L) | ||
| Cl (104 mmol/L) |
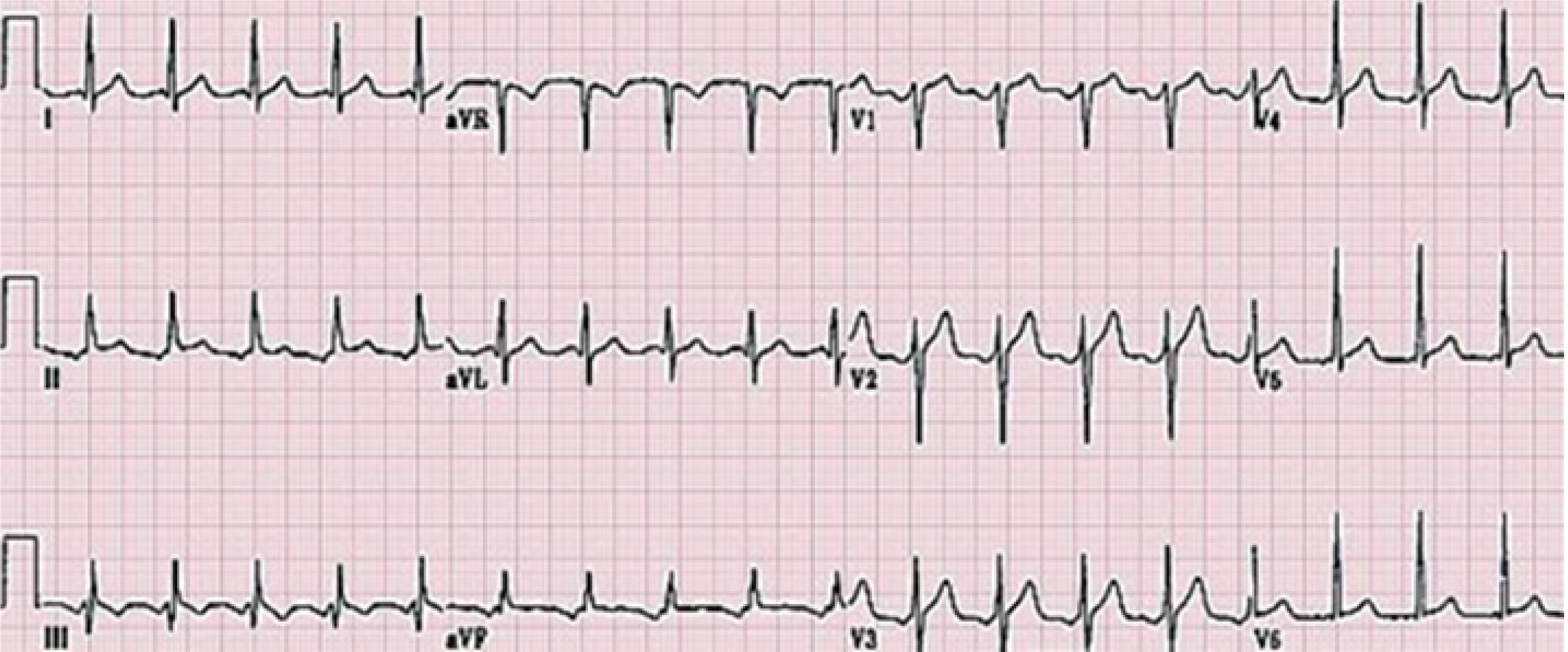
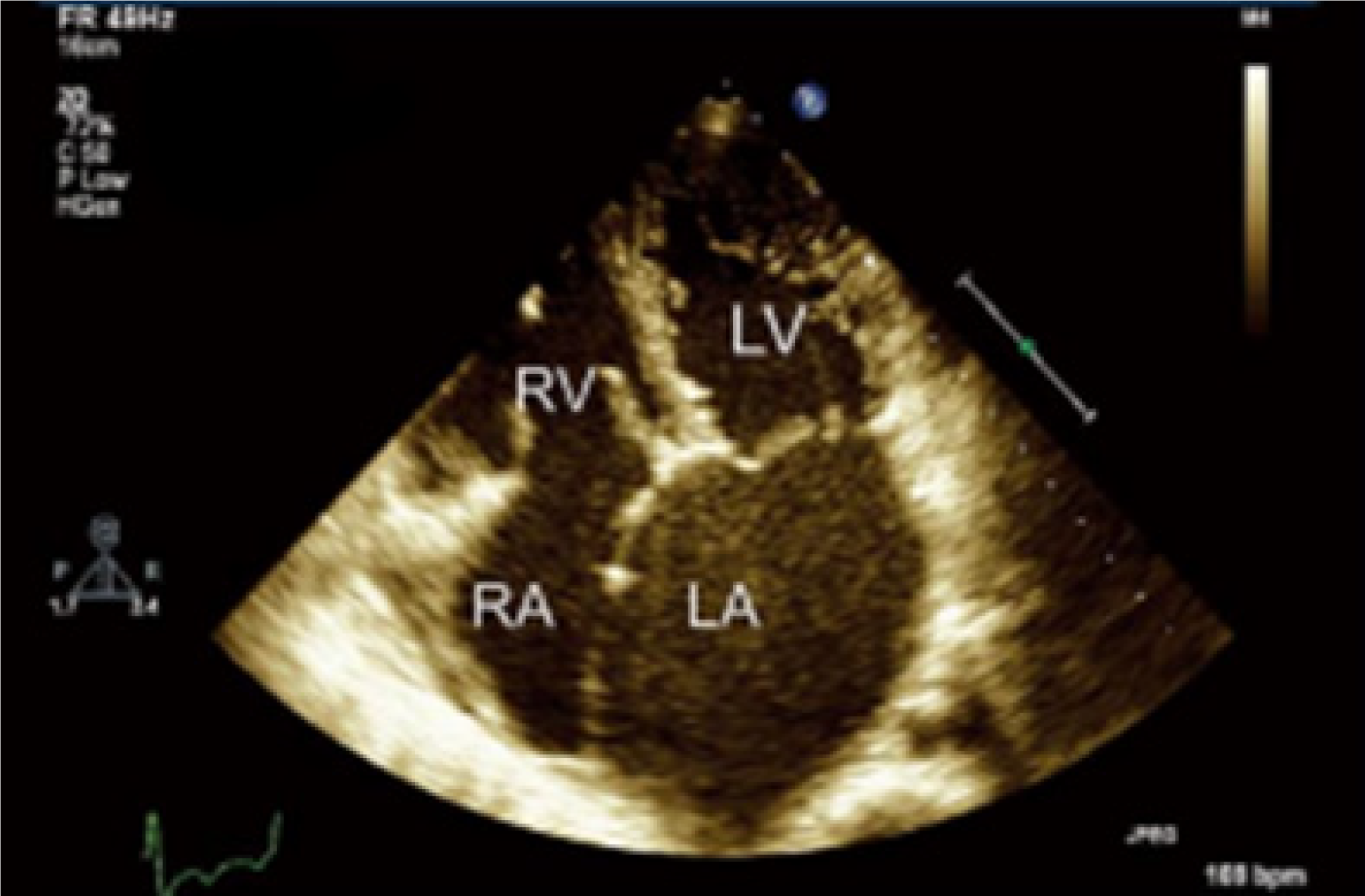
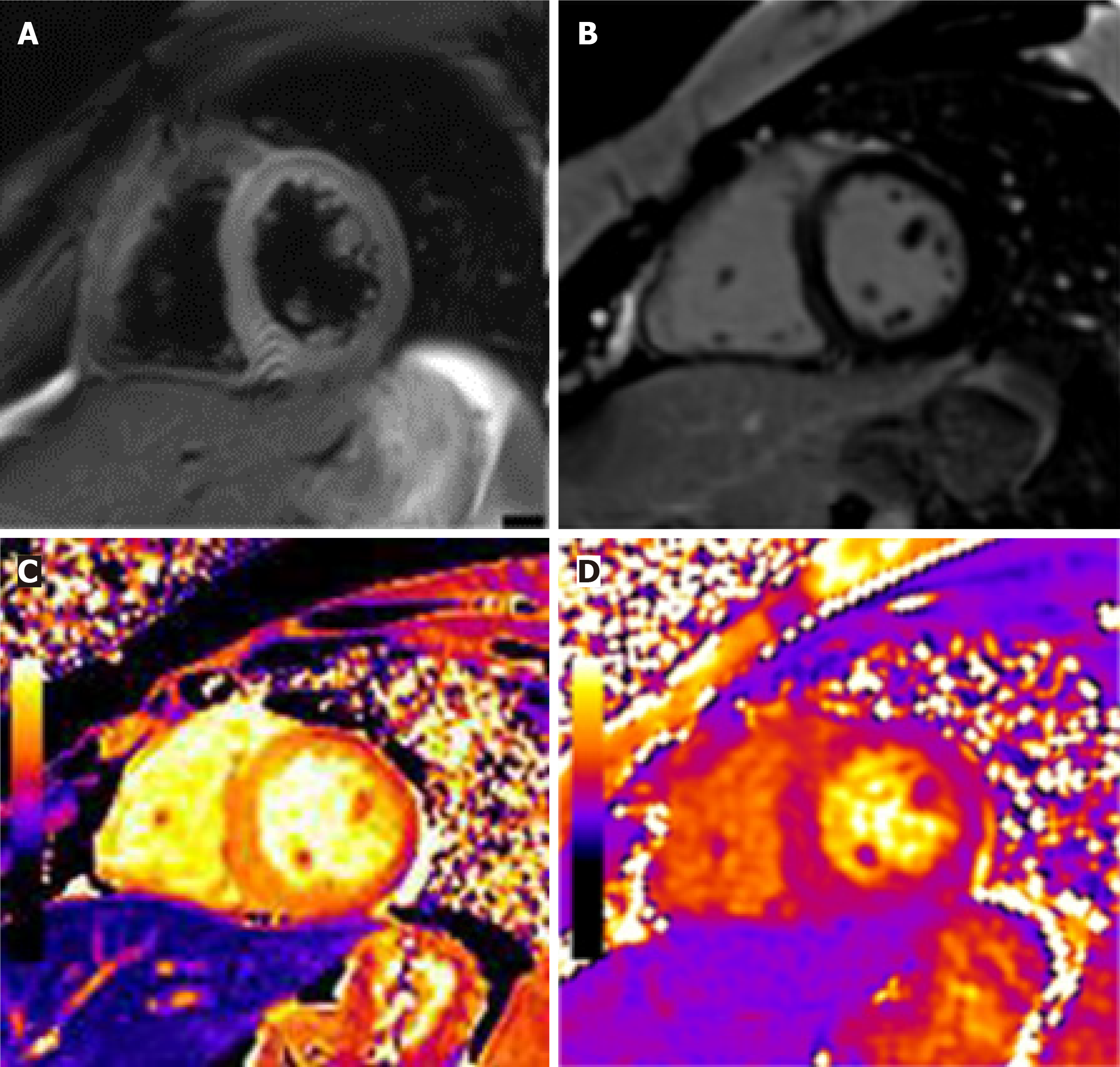
Electromyography showed that the conduction velocity of both upper limbs was slowed and accompanied by low amplitude M and F waves; edema of both lower limbs could not be detected. Computed tomography (CT) showed enlarged liver, spleen, and multiple lymph nodes with pleural effusion and ascites. We did not find monoclonal plasma cell proliferation by lymph node biopsy, bone biopsy, or flow cytometry. A 12-lead electrocardiogram showed sinus tachycardia (Figure 1). It is worth noting that echocardiography showed left ventricular dilation with systolic dysfunction, and the left ventricular ejection fraction (LVEF) was only 38% (Figure 2). Cardiac magnetic resonance imaging (MRI) showed interstitial edema of the myocardium, myocardial native T1 values globally increased, and late gadolinium enhancement could represent definite myocardial necrosis (Figure 3).
The patient had multiple neuropathy, organ enlargement, endocrine diseases, skin changes, and other manifestations, coupled with an increase of VEGF. She was finally diagnosed as having POEMS syndrome with congestive heart failure.
We started her on an insulin pump (continuously adjusting the dose) with some oral medicines that were targeted to improve heart function. These drugs were digoxin (0.125 mg/d), sacubitril valsartan sodium tablets (50 mg/d), and furosemide (60 mg/d). To actively control blood sugar and improve heart function symptoms, 50 mg/d oral dexamethasone (4 consecutive days, repeated every 14 d) combined with 100 mg/d thalidomide (increased to 200 mg after 14 d) was administered. One month later, the patient's weight, cardiac ejection fraction, BNP, LVEF, and other indicators suggested that the patient’s lower limb edema and cardiac function had not significantly improved. Therefore, we changed the treatment plan based on the 1 mo of treatment, and the patient was administered intravenously with 20 mg/d dexamethasone (for 4 consecutive days/2 wk) and 50 mg/d oral thalidomide combined with 1.3 mg/m2 bortezomib (injected twice a week for 2 consecutive weeks).
The patient showed significant improvement in cardiac function at the 6th week after all treatments. For example, the LVEF increased to 45%, and a 5-kg weight loss was observed. A CT scan showed reduced hepatosplenomegaly, and serum VEGF levels decreased rapidly. In the process of continuing the treatment plan, we recommended that the patient undergo autologous stem cell transplantation to obtain a better prognosis and informed the patient of the adverse consequences of the treatment. The patient refused this treatment. In the current treatment plan, thalidomide was well tolerated, and there was no neurotoxicity with bortezomib. If oral medication is necessary, we can only give long-term medication as far as possible without affecting the patient’s future stem cell collection.
In most patients diagnosed with POEMS syndrome, neuropathy is the first clinical feature and may even be the only feature at the initial diagnosis[3]. However, based on all the examination results, this patient was diagnosed with multiple serous effusions with multisystem damage and multiple endocrine diseases; the cause of the heart function decline was unknown. There were no abnormally relevant immunological indicators of systemic lupus erythematosus and dermatomyositis during diagnosis and treatment; thus, rheumatic immune disease could not explain the patient's polyneuropathy. Studies have shown that monoclonal lambda sclerosing plasma
In this case, the response to treatment with dexamethasone and thalidomide was poor. Given the lack of standardized treatment, the poor response may have been related to the dosage, method, and individual differences. However, the patient's heart function improved significantly after the addition of bortezomib. Current research on proteasome inhibitors for the treatment of MM has been relatively in-depth. We believe that these two diseases are both caused by abnormal plasma cells. The standardized treatment for MM should serve as the first reference for the treatment of POEMS syndrome-related complications.
We thank Hong-Bin Zhang, MD for his expert clinical consultation and assistance in preparing this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Barison A, Naswhan AJ S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Li JH
| 1. | Inoue D, Kato A, Tabata S, Kitai T, Takiuchi Y, Kimura T, Shimoji S, Mori M, Nagai Y, Togami K, Matsushita A, Nagai K, Maruoka H, Imai Y, Beppu M, Kawamoto M, Takahashi T. Successful treatment of POEMS syndrome complicated by severe congestive heart failure with thalidomide. Intern Med. 2010;49:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Takahashi Y, Iwano H, Nakano I, Fukushima A, Naya M, Shimizu A, Matsuno Y, Oyama-Manabe N, Anzai T. POEMS Syndrome Showing Left Ventricular Dysfunction and Extracellular Edema Assessed by Cardiac Magnetic Resonance Imaging. Intern Med. 2019;58:2539-2543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Takahashi W, Ichikawa M, Okazaki A, Nakamura F, Arai H, Handa T, Nakamura Y, Seo S, Sasaki K, Mitani K. [Effective treatment of POEMS syndrome accompanied by plasmacytoma with lenalidomide, dexamethasone, and local irradiation]. Rinsho Ketsueki. 2020;61:262-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, Marino P, Smiseth OA, De Keulenaer G, Leite-Moreira AF, Borbély A, Edes I, Handoko ML, Heymans S, Pezzali N, Pieske B, Dickstein K, Fraser AG, Brutsaert DL. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539-2550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1826] [Cited by in RCA: 1845] [Article Influence: 102.5] [Reference Citation Analysis (0)] |
| 5. | Dispenzieri A. How I treat POEMS syndrome. Blood. 2012;119:5650-5658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Sinisalo M, Hietaharju A, Sauranen J, Wirta O. Thalidomide in POEMS syndrome: case report. Am J Hematol. 2004;76:66-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Kuwabara S, Misawa S, Kanai K, Sawai S, Hattori T, Nishimura M, Nakaseko C. Thalidomide reduces serum VEGF levels and improves peripheral neuropathy in POEMS syndrome. J Neurol Neurosurg Psychiatry. 2008;79:1255-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Kim SY, Lee SA, Ryoo HM, Lee KH, Hyun MS, Bae SH. Thalidomide for POEMS syndrome. Ann Hematol. 2006;85:545-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Samaras P, Bauer S, Stenner-Liewen F, Steiner R, Zweifel M, Renner C, Knuth A. Treatment of POEMS syndrome with bevacizumab. Haematologica. 2007;92:1438-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Dispenzieri A, Klein CJ, Mauermann ML. Lenalidomide therapy in a patient with POEMS syndrome. Blood. 2007;110:1075-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Weber D, Rankin K, Gavino M, Delasalle K, Alexanian R. Thalidomide alone or with dexamethasone for previously untreated multiple myeloma. J Clin Oncol. 2003;21:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 416] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 12. | Dispenzieri A. POEMS Syndrome: 2019 Update on diagnosis, risk-stratification, and management. Am J Hematol. 2019;94:812-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 13. | Cerri F, Falzone YM, Riva N, Quattrini A. An update on the diagnosis and management of the polyneuropathy of POEMS syndrome. J Neurol. 2019;266:258-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Chandrashekaran S, Dispenzieri A, Cha SS, Kennedy CC. Pulmonary morbidity improves after autologous stem cell transplantation in POEMS syndrome. Respir Med. 2015;109:122-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Li J, Tian Z, Zheng HY, Zhang W, Duan MH, Liu YT, Cao XX, Zhou DB. Pulmonary hypertension in POEMS syndrome. Haematologica. 2013;98:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Tanus T, Miller HJ. POEMS syndrome presenting with cardiomegaly and cardiomyopathy. J Intern Med. 1992;231:445-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Yokokawa T, Nakazato K, Kanno Y, Mizukami H, Kobayashi A, Yoshihisa A, Takahashi H, Shichishima-Nakamura A, Ohkawara H, Noji H, Suzuki H, Saitoh S, Ogawa K, Hisa S, Takeishi Y. Pulmonary hypertension and refractory heart failure in a patient with Crow-Fukase (POEMS) syndrome. Intern Med. 2013;52:1061-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Shimizu N, Goya M, Akimoto H, Koike A, Nogami A, Ito H, Marumo F, Hiroe M. Cardiomyopathy in a case of Crow-Fukase syndrome. Jpn Heart J. 1997;38:877-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Iwasaki H, Ogawa K, Yoshida H, Takashima F, Shimizu K, Lee JD, Ueda T, Nakamura T. Crow-Fukase syndrome associated with pulmonary hypertension. Intern Med. 1993;32:556-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Reitan JB, Pape E, Fosså SD, Julsrud OJ, Slettnes ON, Solheim OP. Osteosclerotic myeloma with polyneuropathy. Acta Med Scand. 1980;208:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Ishii Y, Yamazaki E, Ishiyama Y, Yamamoto E, Hattori Y, Hagihara M, Tomita N, Ishigatsubo Y. Successful treatment of POEMS syndrome with bortezomib and dexamethasone, combined with radiotherapy, and followed by autologous stem cell transplantation. Int J Hematol. 2013;98:723-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Leuchte HH, Holzapfel M, Baumgartner RA, Neurohr C, Vogeser M, Behr J. Characterization of brain natriuretic peptide in long-term follow-up of pulmonary arterial hypertension. Chest. 2005;128:2368-2374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |