Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7490
Peer-review started: January 30, 2021
First decision: April 25, 2021
Revised: May 4, 2021
Accepted: July 15, 2021
Article in press: July 15, 2021
Published online: September 6, 2021
Processing time: 213 Days and 3.9 Hours
Deep venous thrombosis (DVT) is a serious complication of lumbar spine surgery. Current guidelines recommend pharmacomechanical prophylaxis for patients at high risk of DVT after spine surgery. May-Thurner syndrome (MTS), a venous anatomical variation that may require invasive intervention, is an often overlooked cause of DVT. To date, no case reports of symptomatic MTS caused by isthmic spondylolisthesis or subsequent acute DVT after posterior lumbar surgery have been published.
We here present a case of a patient who developed acute DVT 4 h after spon
In conclusion, clinicians should consider MTS in the presence of a dangerous triad: spondylolisthesis, elevated D-dimer levels, and sonographically indicated unilateral deep vein dilation. Consultation with a vascular surgeon is also essential to MTS management.
Core Tip: The overall prevalence of May-Thurner syndrome (MTS) and its contribution to deep venous thrombosis (DVT) are currently underestimated. We here present a case of acute DVT induced by MTS after lumbar surgery. MTS should be considered in the presence of a dangerous triad (spondylolisthesis, elevated D-dimer levels, and sonographically indicated unilateral deep vein dilation). Consultation with a vascular surgeon is essential to MTS management. A literature review of MTS in spinal settings was also performed.
- Citation: Yue L, Fu HY, Sun HL. Acute deep venous thrombosis induced by May-Thurner syndrome after spondylolisthesis surgery: A case report and review of literature. World J Clin Cases 2021; 9(25): 7490-7497
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7490.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7490
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is one of the most serious complications of spine surgery, with an incidence of 0.1% to 2.09%[1-3]. There are multiple quantitative VTE risk assessment models (RAMs) available for use in clinical practice. The one that is most widely validated in surgery populations is the Caprini score (version 2005). Despite their comprehensiveness, the RAMs used might not account for additional VTE risk factors such as potential anatomical variations[4]. May-Thurner syndrome (MTS), also known as iliac vein compression syndrome, is a rare vascular condition in which the left common iliac vein (LCIV) is mechanically compressed by the overriding right common iliac artery (RCIA), leading to venous congestion. MTS can be asymptomatic with partial venous obstruction, but progression with symptoms related to chronic venous hypertension or acute DVT can occur[5]. Although MTS accounts for only 2% to 5% of all DVT patients, multiple cadaveric and radiographic studies have shown that the actual prevalence in the general population is as high as 14% to 32%[6,7]. The present study reports a patient with MTS induced by isthmic spondylolisthesis who developed subsequent acute DVT after posterior spine surgery.
A 40-year-old Chinese woman was hospitalized with a chief complaint of severe back pain without neurological symptoms for 3 mo. She had exhausted conservative measures and elected to proceed with surgery. Her baseline pain severity was 90 mm on a 100-mm visual analogue scale (VAS).
The patient had a past history of cervical squamous cell carcinoma with metastasis to T10 vertebrae and the lung. She had undergone chemoradiation but not surgery, and her most recent radiotherapy and chemotherapy were 6 mo and 5 mo prior to admission, respectively. She denied any recent travel, surgeries, or immobilization. Her body mass index was 27.3 kg/m2.
There was no other obvious abnormality or any past illness other than cervical cancer.
There was no special history or personal history. The patient had no known family history of DVT.
No abnormality other than low-back tenderness were noticed on physical exam
The routine blood and blood biochemical parameters of the patient were within normal limits. Her D-dimer level was 0.55 mg/mL, and her fibrinogen degradation product (FDP) level was 4.5 mg/mL.
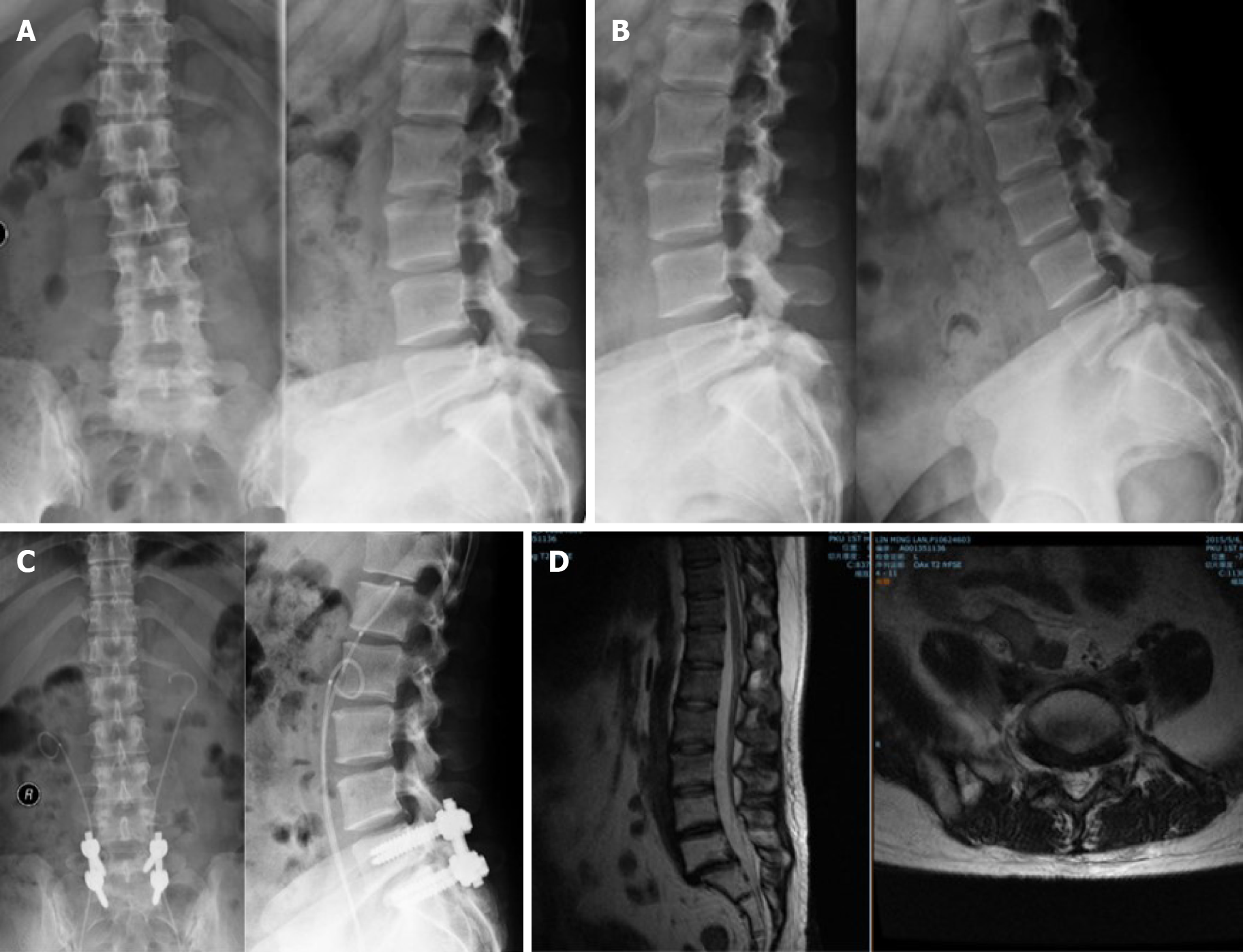
X-ray and computed tomography (CT) showed grade 1 bilateral isthmic L5 spon
Preoperative thrombosis risk factor assessment indicated a high risk of DVT with a Caprini score of 6 because of obesity, history of chemoradiation, malignancy, and major surgery)[8]. The thromboembolic prophylaxis plan was thrombosis prophylaxis hosiery immediately after the surgery and application of low-molecular-weight heparin (LMWH) as soon as the bleeding risk became low enough for that to be acceptable.
The procedure included L5-S1 decompression, lumbar spondylolisthesis reset, L5-S1 pedicle screw fixation, and posterior-lateral lumbar fusion. The entire surgery lasted 135 min, and the estimated blood loss was only 50 mL.
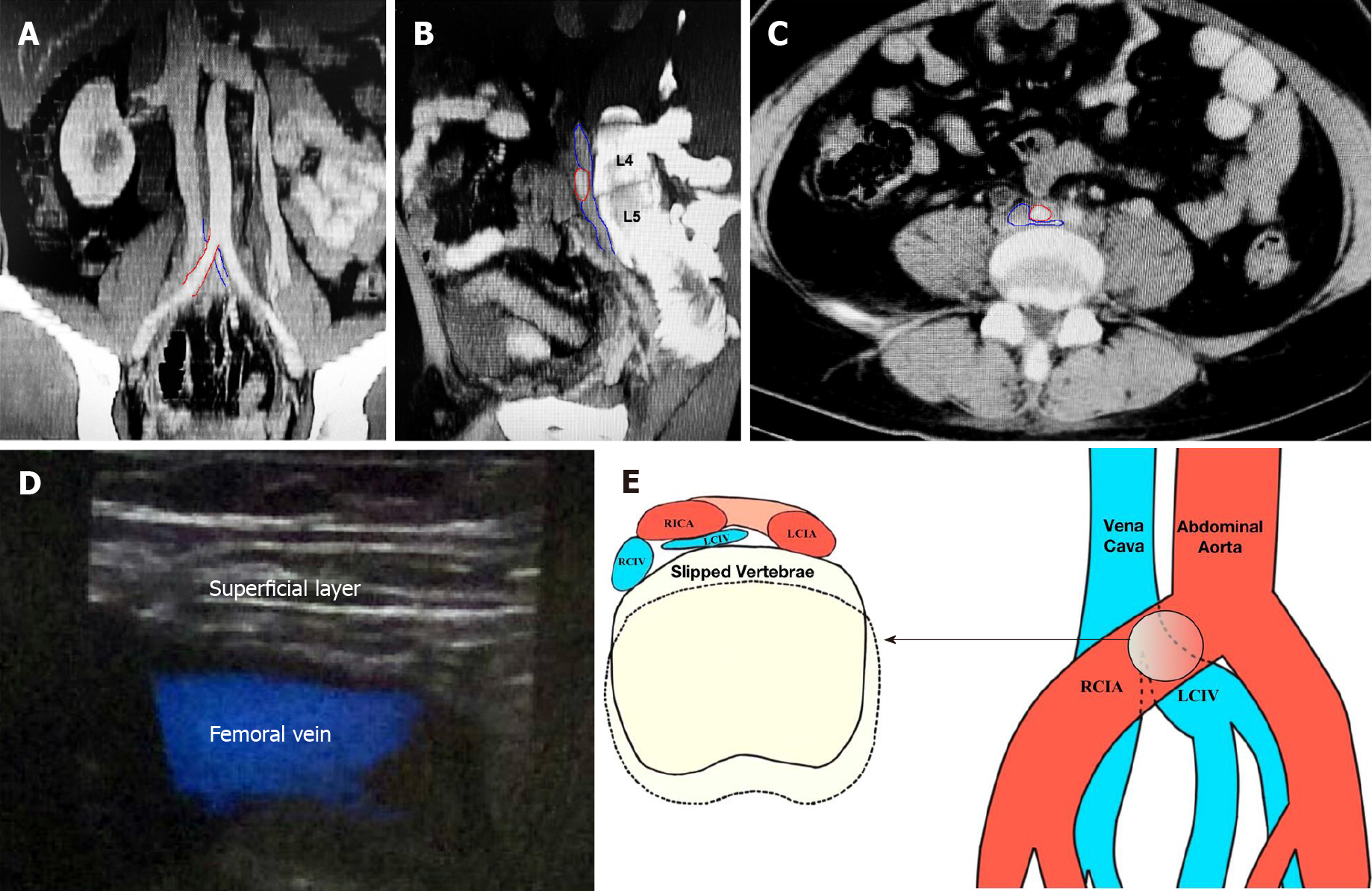
Compression stockings were applied as planned. However, swelling and pain were noted in her left lower limb 4 h after the surgery. Laboratory tests and Doppler ultrasound were performed, and results showed elevated D-dimer level (2.15 mg/L), elevated FDP (12.5 mg/L) level, and left common femoral and deep femoral venous thrombosis. DVT was confirmed; the patient was immobilized and antithrombotic and thrombolytic therapy (LMWH and warfarin) were immediately administered. On review of preoperative examinations, an enhanced pelvis CT scan taken 2 wk before the operation for tumor follow-up showed that the LCIV was sandwiched between the RCIA and slipped vertebrae. MTS was therefore considered (Figure 2A-C).
The diagnosis was left common femoral and deep femoral venous thrombosis, MTS, isthmic spondylolisthesis, and metastatic cervical cancer.
After a 2-wk immobilization and systemic anticoagulation, the left leg swelling gradually subsided, and embolism was undetectable on ultrasonography.
At the 1 mo postoperative follow-up, her VAS score of back pain decreased to 20 mm without further complications (Figure 1C). Neither DVT nor PE occurred during 1-year of follow-up. It should be noted that the patient also manifested acute progressive renal failure postoperatively because of bilateral radiotherapy-induced urethral stricture. The symptoms were relieved after percutaneous nephrostomy and insertion of two double-J tubes.
MTS is described as venous compression by the iliac artery against the spine that may or may not present with symptoms of venous obstruction. This syndrome was first described in 1908 when McMurrich[9] noted that the incidence of congenital adhesions in the common iliac veins contributed to DVTs. In 1957, May and Thurner[10] reported that the presence of intraluminal fibrous bands, caused by external compression by the RCIA, directly led to extensive DVT of the left lower extremity in 22% of 430 cadavers, and they named the condition MTS. Although most cases of MTS follow the classic left-sided description (Figure 2E), right-sided MTS has also been reported[11,12]. Risk factors for MTS include female gender, scoliosis, dehydration, hypercoagulable disorders, and radiation exposure[5].
To the best of our knowledge, this is the first case report of MTS secondary to isthmic spondylolisthesis, and it highlights the need to suspect this variant of MTS under certain conditions. MTS is mostly asymptomatic for partial venous obstruction, but progression may present acutely as DVT/PE or chronically as varicose veins, venous ulcerations, or recurrent superficial venous thrombophlebitis[13,14]. Awareness of MTS should be raised especially among neurosurgeons, because spinal diseases or procedures can be responsible for MTS, while MTS can also manifest as sciatic neuralgia or cauda equina syndrome[15-19] (Table 1).
| Ref. | Country | Study type | Number of patients | Gender/age in yr | Length of onset | Means of diagnosis | Cause of MTS/MTS consequences | Treatment |
| Delera et al[30], 2021 | United States | Case report | 1 | Female/60 | 8 mo | CT, Venogram and IVUS | Spondylolisthesis | Wait and see strategy |
| Kim et al[15], 2020 | Korea | Case report | 1 | Female/28 | 15 d | CT | Spinal heterotopic ossification | Wait and see strategy |
| Díaz et al[31], 2019 | Spain | Case report | 1 | Female/40 | 6 h | MRI, venography | MTS induced back pain and radicular pain | Catheter-directed thrombolysis, cava venal filter and stenting |
| Khalid et al[32], 2019 | United States | Case report | 1 | Female/66 | 3 mo | CT, Venogram, IVUS | Degenerative disc | Ballooning and stenting |
| Xu et al[16], 2019 | China | Case report | 1 | Female/59 | 1 mo | CT, MRI and venography | lumbar disc anterior herniation | Disc radiofrequency thermocoagulation |
| Yamamooto et al[18], 2018 | Japan | Case report | 1 | Male/53 | 3 mo | CT, MRI and venography | MTS induced sciatic neuralgia | Stenting |
| McKean et al[33], 2017 | UK | Case report | 1 | Female/64 | Several wk | CT | Degenerative spondylolisthesis | Anticoagulation therapy |
| Rachaiah et al[17], 2016 | India | Case report | 1 | Female/63 | 3 d | Venogram | Vertebral transpedicular screw | Catheter-directed thrombolysis and oral anticoagulation therapy |
| Ou-Yang and Lu[34], 2016 | China | Cross-sectional study | 33 | NM/61.5 ± 10.6 | 22.5 ± 7.6 d | CT | Intervertebral discs (17/33), osteophytes (16/33), and degenerative lumbar spondylolisthesis (8/33) | Catheter-directed thrombosis, thromb-broken aspiration, ballooning and stenting |
| Woo et al[35], 2016 | United States | Case report | 1 | Female/65 | NM | MRA, venography | Pedicle screw perforation | Ballooning and stenting |
| Reddy et al[36], 2015 | United States | Case report | 1 | Female/33 | 8 d after spine surgery | CT, venography | NM | Catheter-directed thrombolysis, stenting and oral anticoagulation therapy |
| Oteros et al[37], 2008 | Spain | Case report | 1 | Female/13 | During scoliosis surgery | CT, venography | Scoliosis | Wait and see strategy |
The overall prevalence of MTS and its contribution to DVT have been underestimated, as cadaveric studies have shown that venous spurs on the LCIV were present in 50% to 66.7% patients with left-sided iliofemoral DVT[20,21]. MTS typically progresses in three stages, asymptomatic iliac vein compression, development of venous spurs, and thrombus formation[15,22]. Timely diagnosis of MTS is challenging because MTS is usually overshadowed by other more easily recognized risk factors of DVT[7]. Despite its superior accuracy in diagnosing MTS, the use of contrast venography is usually limited in disease screening by its invasive nature. Although CT, magnetic resonance venography, and intravascular ultrasound (IVUS) have also been proven to be effective, they cannot be used for routine preoperative examinations in practice[23]. Doppler ultrasound is convenient and is useful in the detection of lower limb DVT but not MTS because of technological challenges. In our case, although preoperative ultrasound of the lower limb showed mild dilation of the left femoral vein, MTS was only confirmed by enhanced pelvic CT. As suggested by Harbin and Lutsey[7], the patient’s preoperative elevation of D-dimer could have indicated hypercoagulability and possible MTS. Therefore, based on this case, we conclude that MTS should be suspected when the following dangerous triad is observable: spondylolisthesis, elevated D-dimer levels, and unilateral deep vein dilation on sonography. The specific risks of thrombosis in this patient were obesity, history of chemoradiation, malignancy, and major surgery. All the factors could have been responsible for the thrombosis event, and MTS would have gone undetected if not for the review of the patient’s gynecological CT imaging.
Several RAMs have been developed for postoperative VTE estimation and prevention, and the Caprini risk score is the one that has been the most extensively used and validated[8,24-26]. However, the commonly used RAMs do not take such variant factors as MTS into account and may cause clinicians to underestimate the risk of venous thrombosis complications. Bartlett et al[4] recommended exercising caution in relying on RAMs to determine the optimal prophylaxis strategy. The Caprini score of this patient was 6 with recommended prevention of pharmacological and mechanical prophylaxis, which is clearly inappropriate in the setting of MTS because it does not address the underlying pathology. Standard care for MTS is endovascular treatment, which involves catheter-directed pharmacological thrombolysis, mechanical thrombectomy, and stenting of the iliac vein with or without a caval filter. Recanalization in difficult cases can be performed under IVUS guidance[27]. Surgery, including vein repair with thrombus removal, relocation of the artery, and placement of a venous bypass graft, are only indicated when endovascular approaches have failed[28]. However, invasive intervention is not always necessary when MTS is asymptomatic[29]. For this patient, endovascular intervention was not suitable because of the accompanying acute progressive renal failure and hyperkalemia. Antithrombotic and thrombolytic therapy were effective for her. We here further presume the repair of the spondylolisthesis anatomically addressed the compression of left common femoral vein and indirectly relieved MTS.
In summary, our case showed that MTS may occur in patients with isthmic spondylolisthesis. MTS should be suspected if the patient shows a dangerous triad. Besides, consultation with a vascular surgeon is essential to MTS management in patients undergoing spine surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berra LV, Kumar P S-Editor: Liu M L-Editor: Filipodia P-Editor: Liu JH
| 1. | Park JH, Lee KE, Yu YM, Park YH, Choi SA. Incidence and Risk Factors for Venous Thromboembolism After Spine Surgery in Korean Patients. World Neurosurg. 2019;128:e289-e307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Wang T, Yang SD, Huang WZ, Liu FY, Wang H, Ding WY. Factors predicting venous thromboembolism after spine surgery. Medicine (Baltimore). 2016;95:e5776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Wang TY, Sakamoto JT, Nayar G, Suresh V, Loriaux DB, Desai R, Martin JR, Adogwa O, Moreno J, Bagley CA, Karikari IO, Gottfried ON. Independent Predictors of 30-Day Perioperative Deep Vein Thrombosis in 1346 Consecutive Patients After Spine Surgery. World Neurosurg. 2015;84:1605-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Bartlett MA, Mauck KF, Stephenson CR, Ganesh R, Daniels PR. Perioperative Venous Thromboembolism Prophylaxis. Mayo Clin Proc. 2020;95:2775-2798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 5. | Albeir YM, Kathryn AC, Waltham MA. May-Thurner syndrome. [cited 23 April 2021]. In: UpToDate [Internet]. Available from: https://www.uptodate.com/contents/may-thurner-syndrome#!. |
| 6. | Mangla A, Hamad H. May-Thurner Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. [PubMed] |
| 7. | Harbin MM, Lutsey PL. May-Thurner syndrome: History of understanding and need for defining population prevalence. J Thromb Haemost. 2020;18:534-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 8. | Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 581] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 9. | McMurrich JP. The occurrence of congenital adhesions in the common iliac veins, and their relation to thrombosis of the femoral and iliac veins. Am J Med Sci. 1908;135:342. |
| 10. | May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8:419-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 498] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Burke RM, Rayan SS, Kasirajan K, Chaikof EL, Milner R. Unusual case of right-sided May-Thurner syndrome and review of its management. Vascular. 2006;14:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Abboud G, Midulla M, Lions C, El Ngheoui Z, Gengler L, Martinelli T, Beregi JP. "Right-sided" May-Thurner syndrome. Cardiovasc Intervent Radiol. 2010;33:1056-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Butros SR, Liu R, Oliveira GR, Ganguli S, Kalva S. Venous compression syndromes: clinical features, imaging findings and management. Br J Radiol. 2013;86:20130284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 14. | Suwanabol PA, Tefera G, Schwarze ML. Syndromes associated with the deep veins: phlegmasia cerulea dolens, May-Thurner syndrome, and nutcracker syndrome. Perspect Vasc Surg Endovasc Ther. 2010;22:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Kim DH, Boudier-Revéret M, Sung DH, Chang MC. Deep vein thrombosis of the common iliac vein caused by neurogenic heterotopic ossification in the anterior lower lumbar spine of a patient with complete paraplegia due to radiation-induced myelopathy. J Spinal Cord Med. 2020;1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Xu F, Tian Z, Huang X, Xiang Y, Yao L, Zou C, Fu C, Wang Y. A case report of May-Thurner syndrome induced by anterior lumbar disc herniation: Novel treatment with radiofrequency thermocoagulation. Medicine (Baltimore). 2019;98:e17706. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Rachaiah JM, Goyal V, Nagesh C, Reddy B, Srinivas BC. An interesting case of iatrogenic may-thurner like syndrome. Int J Med Res Health Sci. 2016;5:83-86. |
| 18. | Yamamoto K, Gondo G, Ogino H, Watanabe T, Tanaka M, Tanaka S, Kawasaki T. Sciatic Neuralgia Caused by May-Thurner Syndrome. World Neurosurg. 2018;116:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Tello Díaz C, Allegue Allegue N, Gil Sala D, Gonçalves Martins G, Boqué Torremorell M, Bellmunt Montoya S. Cauda Equina Syndrome Caused by Epidural Venous Plexus Engorgement in a Patient with May-Thurner Syndrome. Ann Vasc Surg. 2019;60:480.e7-480.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Ibrahim W, Al Safran Z, Hasan H, Zeid WA. Endovascular management of may-thurner syndrome. Ann Vasc Dis. 2012;5:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Chung JW, Yoon CJ, Jung SI, Kim HC, Lee W, Kim YI, Jae HJ, Park JH. Acute iliofemoral deep vein thrombosis: evaluation of underlying anatomic abnormalities by spiral CT venography. J Vasc Interv Radiol. 2004;15:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 128] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Lugo-Fagundo C, Nance JW, Johnson PT, Fishman EK. May-Thurner syndrome: MDCT findings and clinical correlates. Abdom Radiol (NY). 2016;41:2026-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Mako K, Puskas A. May-Thurner syndrome - Are we aware enough? Vasa. 2019;48:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Sharafuddin MJ, Kresowik TF. Commentary. Pawaskar M, Satiani B, Balkrishnan R, Starr JE. Economic evaluation of carotid artery stenting versus carotid endarterectomy for the treatment of carotid artery stenosis. J Am Coll Surg. 2007;205:413-419. Perspect Vasc Surg Endovasc Ther. 2008;20:385-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Aminian A, Andalib A, Khorgami Z, Cetin D, Burguera B, Bartholomew J, Brethauer SA, Schauer PR. Who Should Get Extended Thromboprophylaxis After Bariatric Surgery? Ann Surg. 2017;265:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 26. | Shah DR, Wang H, Bold RJ, Yang X, Martinez SR, Yang AD, Khatri VP, Wisner DH, Canter RJ. Nomograms to predict risk of in-hospital and post-discharge venous thromboembolism after abdominal and thoracic surgery: an American College of Surgeons National Surgical Quality Improvement Program analysis. J Surg Res. 2013;183:462-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Fereydooni A, Stern JR. Contemporary treatment of May-Thurner Syndrome. J Cardiovasc Surg (Torino). 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Jost CJ, Gloviczki P, Cherry KJ Jr, McKusick MA, Harmsen WS, Jenkins GD, Bower TC. Surgical reconstruction of iliofemoral veins and the inferior vena cava for nonmalignant occlusive disease. J Vasc Surg. 2001;33:320-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 102] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Carroll S, Moll S. Inferior Vena Cava Filters, May-Thurner Syndrome, and Vein Stents. Circulation. 2016;133:e383-e387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Delara R, Cornella J, Knuttinen MG. May-Thurner Syndrome from Spinal Anterolisthesis. J Minim Invasive Gynecol. 2021;28:160-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 31. | Díaz de Santiago I, Insausti Gorbea I, De Miguel Gaztelu M, Albás Sorrosal S, Poblet Florentín J, Rubio Vela T. [May-Thurner syndrome, diagnosis and treatment: a case report]. An Sist Sanit Navar. 2019;42:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Khalid S, Youn YJ, Azrin M, Lee J. Late-Onset Nonthrombotic Left Common Iliac Vein Compression Secondary to Degenerative Lumbar Disc: A Case Report of May-Thurner Variant. Vasc Endovascular Surg. 2019;53:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | McKean D, Allman Sutcliffe J, El Hassan H, Parvizi N, Wali A, Warakaulle D, Teh J, Seel E, Blagg S, Hughes RJ. May-Thurner variant secondary to degenerative lumbar spondylolisthesis: a case report. BJR Case Rep. 2017;3:20170011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 34. | Ou-Yang L, Lu GM. Underlying Anatomy and Typing Diagnosis of May-Thurner Syndrome and Clinical Significance: An Observation Based on CT. Spine (Phila Pa 1976). 2016;41:E1284-E1291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Woo EJ, Ogilvie RA, Krueger VS, Lundin M, Williams DM. Iliac vein compression syndrome from anterior perforation of a pedicle screw. J Surg Case Rep. 2016;2016:rjw003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Reddy D, Mikhael MM, Shapiro GS, Farrell T. Extensive Deep Venous Thrombosis Resulting from Anterior Lumbar Spine Surgery in a Patient with Iliac Vein Compression Syndrome: A Case Report and Literature Review. Global Spine J. 2015;5:e22-e27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Oteros Fernández R, Bravo Rodríguez F, Delgado Acosta F, González Barrios I. [May-Thurner syndrome and surgery for scoliosis]. Radiologia. 2008;50:245-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |