Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7391
Peer-review started: April 21, 2021
First decision: May 24, 2021
Revised: June 1, 2021
Accepted: July 27, 2021
Article in press: July 27, 2021
Published online: September 6, 2021
Processing time: 131 Days and 23.1 Hours
Burnout, musculoskeletal pain, and sharps injuries (SIs) affect medical workers.
To establish a model between SIs, burnout, and the risk factors to assess the extent to which burnout affects SIs.
This questionnaire was used for an observational and cross-sectional study, which was based on members at a hospital affiliated with a medical university in Taichung, Taiwan, in 2020. The valid responses constituted 68.5% (1734 of 2531). The items were drawn from the Nordic Musculoskeletal Questionnaire and Copenhagen burnout inventory and concerned work experience, occupational category, presence of chronic diseases, sleep duration, overtime work, and work schedule. Factor analysis, chi-square test, Fisher exact test, Multiple linear, logistic regression and Sobel test were conducted. The present analyses were performed using SAS Enterprise Guide 6.1 software (SAS Institute Inc., Cary, NC, United States), and significance was set at P < 0.05.
Personal and work-related burnout ranks, sex, work experience ranks, occupational groups, drinking in the past month, sleep duration per day, presence of chronic diseases, overtime work ranks, and work schedule were associated with SIs. Frequent upper limb and lower limb pain (pain occurring every day or once a week) determined to be related to SIs. High personal burnout (> Q3) and high work-related burnout (> Q3) mediated the relationship between SIs and frequent lower limb pain. Similarly, frequent lower limb pain mediated the relationship of SIs with high personal and high work-related burnout. High personal and high work-related burnout mediated the relationships of SIs with overtime work and irregular shift work. The mediating model provides strong evidence of an association between mental health and SIs.
Burnout was determined to contribute to SIs occurrence; specifically, it mediated the relationships of SIs with frequent musculoskeletal pain, overtime work, and irregular shift work.
Core Tip: Burnout affects approximately half of all nurses, physicians, and other clinicians. Sharps injuries, which frequently occur among health care workers, constitute a critical problem. Our study found burnout was determined to contribute to sharps injuries occurrence; specifically, it mediated the relationships of sharps injuries with frequent musculoskeletal pain, overtime work, and irregular shift work. Results from the present study suggest that if the problem of burnout is ignored, training or safe operation may not be sufficient to effectively prevent work-related injuries. To the best of our knowledge, this finding has never been reported.
- Citation: Chen YH, Tsai CF, Yeh CJ, Jong GP. Is burnout a mediating factor between sharps injury and work-related factors or musculoskeletal pain? World J Clin Cases 2021; 9(25): 7391-7404
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7391.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7391
In May 2018, burnout was recognized as an “occupational phenomenon” in the International Classification of Diseases, 11th Revision (ICD-11) of the World Health Organization. Burnout is a state of physical, emotional, and mental exhaustion that results from long-term involvement in work situations that are emotionally demanding[1]. The specific definition of burnout in the ICD-11 is “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.”
Burnout is responsible for high physician turnover and reduced clinical hours, which cause total losses of approximately 4.6 billion dollars in the United States each year[2]. Moreover, burnout affects approximately half of all nurses, physicians, and other clinicians[3]. Studies on resident physicians and nurses have indicated that most cases of burnout are personal or work-related. Studies have noted that work-related burnout (WB) and personal burnout (PB) occur in 30% and 50% of individuals with burnout, respectively[4]. Notably, burnout also affects the patient-related quality of care[5]. The numerous reasons for the development of burnout include basic demographic characteristics such as sex[4,6] and age[7]; occupational factors such as work experience (WE)[8], overtime (OT) work[9], and shift work[10]; lifestyle habits such as sleep duration (SLD)[10,11] and exercise[11]; and health status (e.g., the presence of chronic diseases)[12].
In the United States, 13% of the workforce experience losses in productivity stemming from a painful physical condition, amounting to an estimated US$61.2 billion in pain-related lost productive time each year[13]. Musculoskeletal (MS) in the lower back, shoulders, and neck are most commonly reported[14]. In addition, myofascial pain syndromes from trigger points are among the main causes of MS pain due to traumatic/micro traumatic events (often secondary to occupational postu
The United States Centers for Disease Control and Prevention defines sharp injuries (SI) as an exposure event (blood/body fluid exposure) that occurs when a needle or other sharp object penetrates the skin. SI frequently occurs among health care workers and constitutes a critical infective problem upon contamination of the sharp object. As one study noted, 0.42 hepatitis B infections, 0.05 to 1.30 hepatitis C infections, and 0.04 to 0.32 human immunodeficiency virus (HIV) infections develop per 100 cases of SI per year. The literature review conducted in that study revealed that SIs led to mean costs of €1966 if the source patient was HIV positive and had coinfections of hepatitis B and hepatitis C[16]. SI occurrence has been reported to be associated with occupational factors such as WE[17], work hours[18], and shift work schedules[19] as well as demographic characteristics such as sex[20] and age[21]. Moreover, one article asserted that the experience of SIs was related to the mental health of health care workers[22]. Therefore, the relationship between burnout level (as measured using a routine questionnaire) and SI deserves scholarly attention with regard to the prevention of work-related injuries among medical personnel. In the present study, a model of causal relationships between SI, burnout, and work-related risk factors was established to assess the extent to which burnout affects SI. This investigation serves as a basis on which the impact of mental health on occupational injuries can be further explored in the future. Specifically, the present study examined the relationship between mental health and occupational injuries, with burnout and SI as agent variables.
This questionnaire was used for an observational and cross-sectional study, which was based on members at a hospital affiliated with a medical university in Taichung, Taiwan, in 2020. Of the 2531 individuals to whom the questionnaire was sent, 1838 (72.6%) completed the questionnaire. After exclusion for missing data, 1734 questionnaires (68.5%) were determined to be valid.
The participants’ WE (years) and occupational category were provided by the occupational safety department of the hospital. On the questionnaire, the participants were asked whether they had a listed chronic disease (CD), with the selection of one or more diseases classified as a “yes” response. The participants were also asked whether they had experienced a SI in the past year. In response to the question on smoking in the past month, “never” or “have quit smoking” were classified as “no.” As for drinking in the preceding month, answers of “seldom” or “every day” were classified as “yes,” whereas “never” was classified as “no.” SLD was classified as < 5, 5–6, 6–7, 7–8, or > 8 h. The participants were asked whether they exercised at least once a day, at least once a week, at least once a month, less than once a month, or never. Possible responses to the question on OT work were the following: seldom, fewer than 45 h per month, 45–80 h per month, and more than 80 h per month. The responses were classified as seldom, < 45 h per month, and > 45 h per month accordingly. As for work schedule, the options given were day shift work, night shift work, irregular shift work, and regular shift work.
This study adopted the Nordic MS Questionnaire (NMQ) modified and translated by the Taiwan Institute of Occupational Safety and Health[23]. The NMQ, which is used in the investigation of the site and frequency of MS pain, was developed in a project funded by the Nordic Council of Ministers. The NMQ has acceptable reliability[23] and has been applied in a wide range of occupational groups, including nurses[24]. Items on the NMQ include questions on the presence of pain attributable to work-related factors in the preceding year and on the pain sites, the options for which were the neck (N1), left shoulder (N2), right shoulder (N3), upper back (N4), waist or lower back (N5), left elbow (N6), right elbow (N7), left wrist (N8), right wrist (N9), left hip/thigh/buttock (N10), right hip/thigh/buttock (N11), left knee (N12), right knee (N13), left ankle (N14), and right ankle (N15). If a participant answered “yes” to the question on the experience of work-related pain over the past year, they were instructed to indicate its frequency: every day, once a week, once a month, or once every half year. Pain occurring every day or once a week was defined as frequent MS (FMS) pain and was scored as 1. Pain occurring once a month or once every half year was scored as 0.
In the present study, factor analysis was conducted on the NMQ results to determine the underlying variables that explained most of the questionnaire. According to the principle proposed by Hair et al[25], factors that should be retained have feature vector values exceeding 1. Through varimax rotation, the standardized scoring coefficients constituted new factor loadings and were defined as new factors according to the corresponding significance of the factor loadings.
The Copenhagen burnout inventory (CBI), which comprises three scales assessing PB, WB, and client-related burnout, has extremely high internal reliability and low nonresponse rate[26]. The present study used the Chinese version of CBI, which has proven to be a reliable and valid tool for assessment of burnout problems[27]; thus, it was used to evaluate burnout in the present study, with a focus on PB and WB. The first six items, which concern PB, are as follows: C1: “How often do you feel tired?” C2: “How often are you physically exhausted?” C3: “How often are you emotionally exhausted?” C4: “How often do you think ‘I can’t take it anymore’?” C5: “How often do you feel worn out?” C6: “How often do you feel weak and susceptible to illness?”
Items 7–13, which concern WB, are as follows: C7: “Is your work emotionally exhausting?” C8: “Do you feel burnt out because of your work?” C9: “Does your work frustrate you?” C10: “Do you feel worn out at the end of the working day?” C11: “Are you exhausted in the morning at the thought of another day at work?” C12: “Do you feel that every working hour is tiring for you?” C13: “Do you have enough energy for family and friends during leisure time?”
The response options-“always”, “often”, “sometimes”, “seldom”, and “never/almost never”-are scored as 100, 75, 50, 25, and 0 points, respectively, except for item C13, which is inverse scored (i.e., the responses are scored as 0, 25, 50, 75, and 100 points, respectively). Levels of PB and WB are represented by the mean of the total PB and WB scores (the sum of scores on items C1–C6 and items C7–C13), respectively.
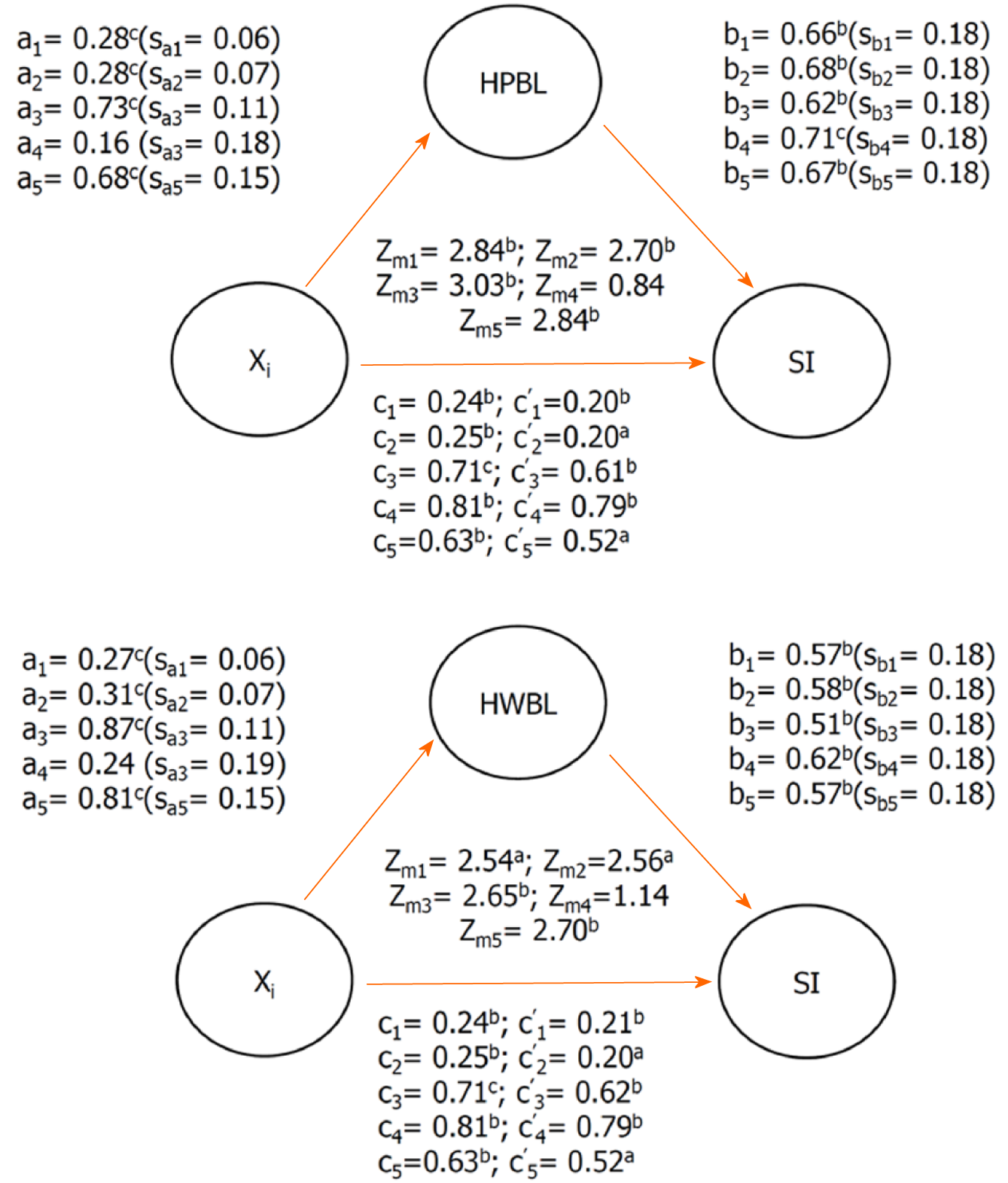
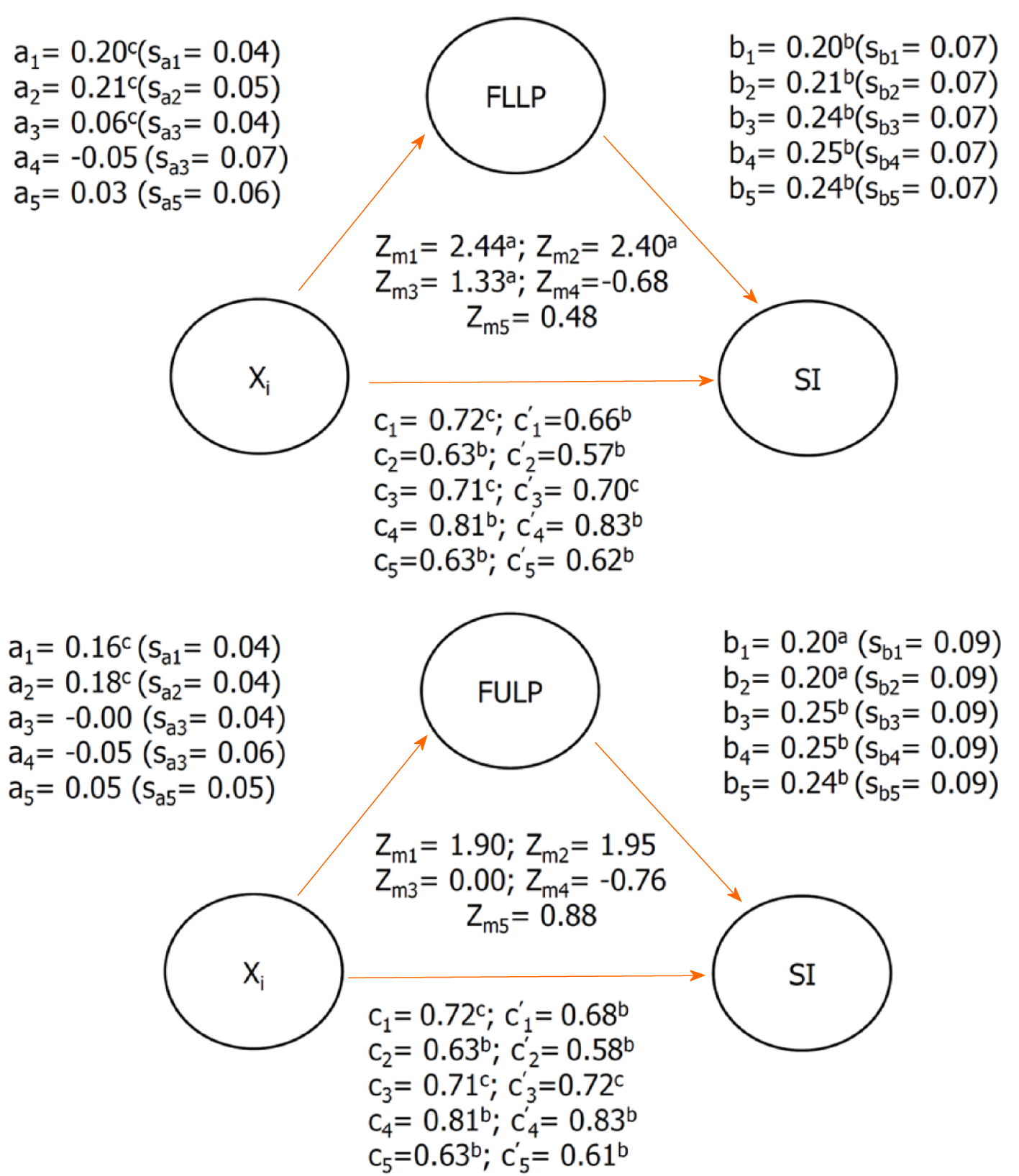
The categorical variables were subjected to the chi-square test or Fisher exact test. Significance in the differences among the means of continuous variables was determined using the t test or one-way ANOVA. Multiple linear or logistic regression was conducted to control the interference of potential risk factors in the association between the independent variables (IVs) and the dependent variable (DV)-specifically, to determine whether adjustments to variables significantly affected IV–DV associations. Mediation effects were analyzed on the basis of the strategy proposed by Baron and Kenny[28] in which: (1) The IV significantly affects the mediator (first-stage effect); (2) The IV significantly affects the DV in the absence of the mediator; (3) The mediator has a significant unique effect on the DV (second-stage effect); and (4) The effect of the IV on the DV weakens upon addition of the mediator to the model. A method for mediation suitable for a combination of categorical and continuous variables, developed by Iacobucci[29], was used; the (formula 1) are as follows.

Where X is an IV; Y is a DV; M is the adjusted variable (i.e., the mediating factor) in a simple mediation model; a is a logistic/Linear regression coefficient of X against M when M and X are a DV and IV, respectively; b is the logistic/Linear regression coefficient of M against Y in a simple mediation model; c is the logistic/Linear regression coefficient of X against Y; and c' is the logistic/Linear regression coefficient of X against Y with M as the adjusting variable. The standard errors of a and b are represented by sa and sb, respectively.
The original formula of the Sobel test was rederived into formula 2.
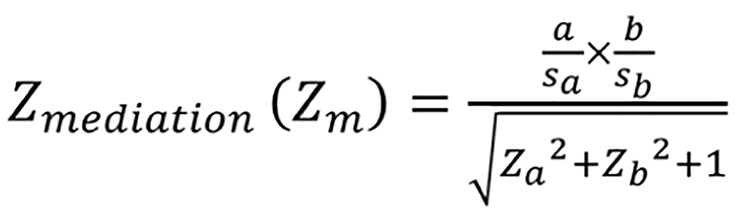
Results exceeding |1.96| and |2.57| (for a two-tailed test) are significant at α = 0.05 and α = 0.01, respectively. The present analyses were performed using SAS Enterprise Guide 6.1 software (SAS Institute Inc., Cary, NC, United States), and significance was set at P < 0.05.
As shown in Table 1, the mean PB and WB scores were 36.69 ± 17.59 and 34.19 ± 16.29, respectively. SI incidence was 8.42%. Q1, Q2, and Q3 represented the lower quartile, median, and upper quartile, respectively. The highest proportions of SIs (12.55% and 12.42%) corresponded to PB and WB (rank > Q3 for both), respectively. Differences in SI occurrence were significant among the PB or WB ranks. Women reported higher PB and WB than men (37.39 vs 33.64 and 34.89 vs 31.13, respectively; P < 0.01 for both), but SIs were more common in men (13.85% vs 7.17%; P < 0.01). Regarding WE, ranks > Q2 and ≤ Q3 corresponded to the highest PB level (mean = 38.94 ± 17.60), whereas a rank > Q3 corresponded to the lowest WB level (mean = 31.36 ± 15.46). Moreover, ranks > Q1 and ≤ Q2 with regard to WE corresponded to the highest proportion of SI occurrence (12.21%). Significant differences in the proportion of SI occurrence and in the levels of PB and WB were noted among occupational groups, with nurses experiencing the highest PB and WB (41.22 and 39.33). Notably, SIs occurred most commonly among physicians (15.86%). Levels of PB (mean = 39.51) and WB (mean = 36.17) were significantly higher in participants who reported drinking during the preceding month, as was SI occurrence (11.41%). SLD was significantly associated with PB level, WB level, and SI occurrence. The highest PB and WB (mean scores = 48.52 and 41.82, respectively) were observed in the participants who reported sleeping ≤ 5 h per night, as was the highest SI occurrence (14.52%). The participants who exercised daily reported significantly lower PB and WB (mean scores = 31.27 and 28.84, respectively) than those who exercised less frequently, but no significant difference in SI occurrence was noted. Compared with those without such conditions, the participants with CD had significantly higher levels of PB and WB (mean scores = 38.69 and 35.43, respectively) and were more likely to have sustained an SI (10.53%). Burnout levels and SI occurrence differed significantly according to the monthly number of OT hours. Specifically, the participants who worked > 45 h per month had the highest PB and WB (mean scores = 48.51 and 43.73, respectively). These individuals were also the most likely to have sustained an SI (16.98%). Burnout levels and SI occurrence also differed significantly with work schedule. Specifically, the participants who worked irregular shifts reported the highest PB and WB (mean scores = 43.54 and 40.90, respectively) as well as the highest SI occurrence (13.45%).
| Characters | n | PB score | WB score | SI |
| mean ± SD | mean ± SD | Subject (%) | ||
| SI in past one year | 1734 | 36.69 ± 17.59 | 34.19 ± 16.29 | 146 (8.42) |
| PB ranks | 1,b | |||
| > Q3 | 542 | 56.93 ± 12.20 | - | 68 (12.55) |
| > Q2 and ≤ Q3 | 482 | 37.22 ± 3.31 | - | 30 (6.22) |
| > Q1 and ≤ Q2 | 394 | 27.08 ± 2.09 | - | 29 (7.36) |
| ≤ Q1 | 316 | 13.12 ± 6.79 | - | 19 (6.01) |
| WB ranks | 1,b | |||
| > Q3 | 451 | - | 54.66 ± 9.45 | 56 (12.42) |
| > Q2 and ≤ Q3 | 572 | - | 36.70 ± 4.03 | 39 (6.82) |
| > Q1 and ≤ Q2 | 344 | - | 26.61 ± 1.78 | 25 (7.27) |
| ≤ Q1 | 367 | - | 12.20 ± 7.27 | 26 (7.08) |
| Sex | b | b | 2,b | |
| Male | 325 | 33.64 ± 16.48 | 31.13 ± 15.28 | 45 (13.85) |
| Female | 1409 | 37.39 ± 17.77 | 34.89 ± 16.44 | 101 (7.17) |
| WE ranks | b | b | 1,b | |
| ≤ Q1 | 375 | 36.23 ± 17.73 | 34.72 ± 17.37 | 34 (9.07) |
| > Q1 and ≤ Q2 | 434 | 37.29 ± 17.98 | 35.12 ± 16.10 | 53 (12.21) |
| > Q2 and ≤ Q3 | 487 | 38.94 ± 17.60 | 35.48 ± 16.06 | 38 (7.80) |
| > Q3 | 438 | 34.07 ± 16.73c | 31.36 ± 15.46 | 21 (4.79) |
| Occupation groups | c | c | 1,b | |
| Doctors | 145 | 37.10 ± 17.37 | 34.11 ± 16.78 | 23 (15.86) |
| Nurses | 627 | 41.22 ± 17.27 | 39.33 ± 15.55 | 55 (8.77) |
| Others | 962 | 33.67 ± 17.20 | 30.84 ± 15.82c | 68 (7.07) |
| Right-handed | ||||
| Yes | 1663 | 36.89 ± 17.64 | 34.31 ± 16.31 | 142 (8.54) |
| No | 71 | 31.87 ± 15.62 | 31.34 ± 15.48 | 4 (5.63) |
| Drinking in past month | c | b | 2,b | |
| Yes | 561 | 39.51 ± 17.05 | 36.17 ± 16.03 | 64 (11.41) |
| No | 1173 | 35.34 ± 17.69 | 33.24 ± 16.33 | 82 (6.99) |
| Smoking in past month | ||||
| Yes | 12 | 31.60 ± 16.80 | 25.89 ± 17.04 | 2 (16.67) |
| No | 1722 | 36.72 ± 17.60 | 34.24 ± 16.27 | 144 (8.36) |
| SLD (per day) ranks | c | c | 1,a | |
| ≤ 5 h | 62 | 48.52 ± 20.62 | 41.82 ± 17.57 | 9 (14.52) |
| > 5 and ≤ 6 h | 566 | 41.04 ± 17.91 | 38.26 ± 16.47 | 54 (9.54) |
| > 6 and ≤ 7 h | 771 | 34.91 ± 16.38 | 32.35 ± 15.40 | 66 (8.56) |
| > 7 h | 335 | 31.23 ± 16.47 | 29.89 ± 15.80 | 17 (5.07) |
| Exercise per day | b | c | ||
| Yes | 133 | 31.27 ± 18.88 | 28.84 ± 17.87 | 11 (8.27) |
| No | 1601 | 37.14 ± 17.41 | 34.63 ± 16.08 | 135 (8.43) |
| Suffering chronic disease | b | a | 2,a | |
| Yes | 608 | 38.69 ± 17.95 | 35.43 ± 16.70 | 64 (10.53) |
| No | 1126 | 35.61 ± 17.31 | 33.51 ± 16.02 | 82 (7.28) |
| OT work ranks | c | c | 1,b | |
| > 45 h / mo | 53 | 48.51 ± 19.78 | 43.73 ± 18.34 | 9 (16.98) |
| < 45 h / m | 481 | 41.32 ± 17.21 | 39.27 ± 15.82 | 58 (12.06) |
| Seldom | 1200 | 34.31 ± 17.07c | 31.73 ± 15.75 | 79 (6.58) |
| Work schedule classes | c | c | 1,b | |
| Irregular shift | 223 | 43.54 ± 18.63 | 40.90 ± 16.91 | 30 (13.45) |
| Regular shift | 204 | 37.89 ± 17.15 | 35.19 ± 15.19 | 25 (12.25) |
| Night | 204 | 37.77 ± 18.14 | 37.45 ± 16.26 | 17 (8.33) |
| Day | 1103 | 34.88 ± 16.99 | 32.04 ± 15.89 | 74 (6.71) |
Table 2 presents information on the sites and occurrence of MS pain experienced over the 12 mo as well as the sites and proportion of MS pain that occurred at least once a week (i.e., FMS pain). Because the eigenvalues of factors 1 and 2 exceeded 1, these factors were retained. Although the eigenvalue of factor 3 was lower than 1, it was retained for the maximum explaining questionnaire. The factor loadings were converted into standardized scoring coefficients through varimax rotation. The relatively large factor loading values in bold for factors 1, 2, and 3 correspond to pain in the upper trunk, lower limbs, and upper limbs, respectively. Frequent upper torso pain (FUTP) occurred in the neck, both shoulders, and upper back, and its standardized coefficient was defined as FUTP. As for frequent lower limb pain (FLLP), sites included both hip/thigh/buttocks, both knees, and both ankles, and its standardized coefficient was defined as FLLP. Frequent upper limb pain (FULP) occurred in both elbows and both wrists, and its standardized coefficient was defined as FULP. The explained variation in FUTP, FLLP, and FULP was 73.86%, 23.11%, and 8.67%, respectively. This indicated that the participants experienced upper trunk pain most frequently, followed by lower limb and upper limb pain. Although FULP had the smallest explained variation of the three, it was retained because the present study was focused on the relationship between SI and upper limb pain.
| Pain site | Pain past 12 months | FMS pain | Factor loadings | ||
| Subjects | Subjects | Factor 1: Upper torso | Factor 2: Lower limb | Factor 3: Upper limb | |
| Neck | 636 (36.68) | 405 (23.36) | 0.29 | -0.04 | -0.05 |
| Left shoulder | 370 (21.34) | 234 (13.49) | 0.27 | -0.06 | -0.03 |
| Right shoulder | 444 (25.61) | 283 (16.32) | 0.29 | -0.05 | -0.02 |
| Upper back | 327 (18.86) | 210 (12.11) | 0.19 | 0 | 0.01 |
| Waist or lower back | 529 (35.01) | 300 (17.30) | 0.12 | 0.02 | 0 |
| Left elbow | 65 (3.75) | 35 (2.02) | -0.03 | -0.02 | 0.25 |
| Right elbow | 126 (7.27) | 81 (4.67) | -0.01 | -0.04 | 0.27 |
| Left wrist | 103 (5.94) | 67 (3.86) | -0.03 | 0 | 0.24 |
| Right wrist | 205 (11.82) | 110 (6.34) | -0.02 | -0.04 | 0.31 |
| Left hip/thigh/buttock | 70 (4.04) | 48 (2.77) | -0.04 | 0.19 | 0.04 |
| Right hip/thigh/buttock | 70 (4.04) | 45 (2.60) | -0.04 | 0.19 | 0.05 |
| Left knee | 95 (5.48) | 51 (2.94) | 0.04 | 0.2 | -0.09 |
| Right knee | 88 (5.08) | 51 (2.94) | 0.02 | 0.29 | -0.11 |
| Left ankle | 42 (2.42) | 31 (1.79) | -0.06 | 0.23 | 0 |
| Right ankle | 51(2.94) | 39 (2.25) | -0.05 | 0.21 | 0 |
| Eigenvalues | 4.02 | 1.26 | 0.47 | ||
| Explained variation (%) | 73.86 | 23.11 | 8.67 | ||
Table 3 shows that the participants who had experienced an SI in the preceding year had significantly higher FLLP and FULP scores than those who had not, but no significant differences were noted for the FUTP score. In short, FLLP and FULP were identified as risk factors for SIs.
Because of the extremely high proportion of SIs corresponding to PB or WB ranks > Q3 (Table 1), PB rank was reclassified as PB > Q3 and PB ≤ Q3, and WB rank was reclassified as WB > Q3 and WB ≤ Q3. PB > Q3 and WB > Q3 corresponded to high PB level (HPBL) and high WB level (HWBL), respectively. Similarly, the participants who worked irregular shifts had significantly higher PB and WB scores; therefore, the work schedule was reclassified as irregular work shifts (IRWS) and other work schedules. Moreover, because SIs were only reported by nine participants who worked > 45 h of OT per month, OT work was reclassified as an experience of OT (EOT) work and seldom worked OT.
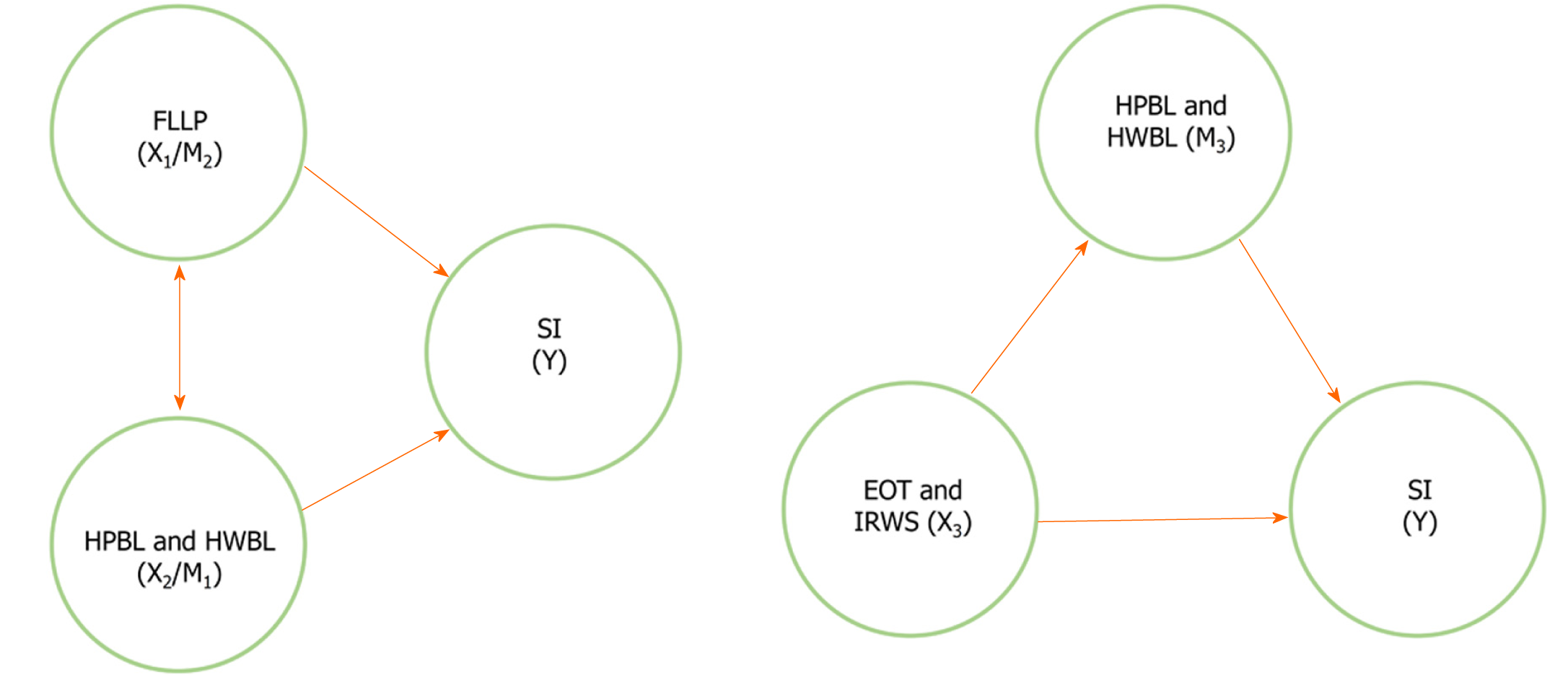
Figure 1 shows the mediation effect of burnout in the association between SIs and the risk factors. The value of c must be statistically significant and greater than that of
From the analytical results (Table 1-3, Figure 1 and 2), the following inferences can be made: an increase in the frequency of limb pain was closely correlated with an increase in SI incidence, and an increase in burnout level caused by an increase in the frequency of limb pain increased SI occurrence. The participants with HPBL accounted for a higher proportion of the SIs that occurred, and the increase in FLLP caused by HPBL also raised the proportion of SI occurrence. The participants with EOT work were more likely to sustain an SI, as were the participants experiencing serious burnout caused by OT work, which would increase the rate of SI occurrence. Similarly, the participants with IRWS were also more likely to sustain an SI, as were the participants experiencing serious burnout caused by IRWS, which would increase the rate of SI occurrence.
Constructed on the basis of the results presented in Figure 1 and 2 is a simple mediation model that indicates the existence of direct or mediating relationships between SI and FLLP, HPBL/HWBL, and EOT work or IRWS. HPBL and HWBL mediated the SI–FLLP relationship. Similarly, FLLP was a mediating factor in the relationships of SI with HPBL and HWBL. Furthermore, HPBL and HWBL mediated the relationships of SI with EOT work and IRWS.
In line with reports that both PB and WB levels are significantly higher among female resident physicians[4] and that male nurses experience burnout syndrome less commonly than female nurses[6], the women in the present sample reported significantly higher PB and WB than the men (Table 1). Regarding SIs, a study indicated that male health workers were 10 times more likely to sustain an SI than were female health workers[30]. The men in the present study were more likely to sustain SIs than the women (13.85% vs 7.17%).
Studies have reported that nurses and clinicians working OT are more likely to experience burnout[9]. In one study, an increase in weekly work hours increased the occurrence of SIs among nurses[31]. As shown in Table 1, a dose–response relationship between SI and OT work (> 45, < 45 h, or seldom) was observed. Similar results were noted for relationships of PB and WB with OT. Specifically, more OT work hours increased SI occurrence and the mean levels of PB and WB, and PB and WB was positively associated with SIs. These results suggest that OT work was related to PB and WB level as well as to SI occurrence. PB and WB may contribute critically to the relationship between SI and OT work; this possibility warrants further investigation. As shown in Figure 1, PB and WB partially mediated the relationship between SI and EOT work; the effects were significant. These results suggest that EOT work affected SI directly or indirectly (through an unknown path). Studies have noted that increased OT was significantly associated with impairments in attention, executive function[32], and stress response[33]. Whether OT work affects SI incidence through these factors remains to be determined.
One study noted that burnout syndrome was more common among nurses working irregular shifts than among those working regular shifts[6]. In the same vein, studies have observed that working regular shifts exerted protective effects against Sis[19,21]. Consistent with results from other studies, in the present study, the highest mean PB and WB was reported by participants working irregular shifts (Table 1). As shown in Figure 1, PB and WB also partially mediated the relationship between SI and irregular shifts, indicating that irregular shifts may have affected SI through burnout in some participants; in others, irregular shifts may have exerted direct effects on SI through other routes.
A large study conducted in the Netherlands on MS pain occurring over 12 mo reported that lower back pain occurred the most frequently (43.9%), followed by shoulder pain (30.3%) and neck pain (31.4%)[14]. In line with these results, the corresponding occurrence of low back pain, shoulder pain, and neck pain in the present study was 35.01%, 46.95%, and 36.68%, respectively (Table 2). A study on seven occupational groups in Norway reported a significant association between burnout and MS pain[34]. In the present study, the frequency of limb pain (lower or upper) was positively associated with HPBL and HWBL (a = 0.28, P < 0.0001; a = 0.28, P < 0.0001; Figure 1). A cross-sectional study on burnout and occupational accidents in which the Maslach Burnout Inventory (MBI) questionnaire was administered to employees in the occupational medicine department of a hospital reported that each one-unit increase in the burnout score corresponded to a 9% increase in the risk of injury[35]. In a study on Chinese nurses in which the MBI questionnaire was again used, emotional exhaustion was positively associated with SI occurrence[36]. Regarding the present results obtained from the CBI, SI occurrence differed significantly in PB (P < 0.01) and WB ranks (P < 0.01) (Table 1). As shown in Figure 2, HPBL (c = 0.72, P < 0.001) and HWBL (c = 0.63, P < 0.01) were positively associated with SI occurrence. The present results are consistent with those from other studies that used the MBI. However, in an extension of the literature, we further explored the causal relationships between SI, work-related risk factors, and burnout through the analysis of mediating effects. As shown in Figure 2, FLLP also mediated the relationships of SI with HPBL and HWBL, indicating that FLLP and HPBL or HWBL form a vicious circle with SI (Figure 3). These findings serve as a valuable reference for SI prevention. To test for significance, we used the Zm formula developed by Iacobucci[29], which can effectively test for mediating effects in samples exceeding 300 when X, Y, and M are categorical variables. The present sample size of 1734 more than meets this requirement. Therefore, the Zm formula was suitable.
WE, drinking in the preceding year, SLD, exercise, and CD, variables adjusted in the model, were identified as risk factors for SI and burnout. The significant association of these variables with SI and burnout is supported by results from other studies. For example, studies have indicated that individuals with less WE are at a higher risk of sustaining SIs[17], and the report of burnout was significantly positively associated with higher alcohol consumption[37]. Moreover, PB has been demonstrated to be significantly associated with impaired sleep quality[11], and reductions in SLD increase the risk of occupational injury[38]. University students or nurses who engage in physical activity or exercise have been noted to report significantly lower levels of PB and fatigue[11], and individuals with burnout appear to be more susceptible to physical illness than those without burnout[39]. Therefore, the adjustment of these variables was both necessary and appropriate for reducing the impacts of possible confounders on the SI model.
The burnout mediation model regarding SI and occupational risk factors (e.g., OT work, irregular shift, and MS pain) provides strong evidence of an association between mental health and SIs. The literature mostly examines the relationship between SI and the work process or the use of protective equipment; deeper psychological factors are seldom explored. The relationship between SIs and work-related injuries not induced by burnout warrants further investigation. A study on 112 workers in metal melting industries reported no significant association between occupational burnout and unsafe actions[40]. Despite the small sample size in that study, results from both that study and the present study suggest that if the problem of burnout is ignored, training or safe operation may not be sufficient to effectively prevent work-related injuries. Therefore, to mitigate the problem of work-related injuries, institutions should take effective countermeasures to alleviate burnout among medical personnel.
This study was performed in the context of the coronavirus disease 2019 pandemic, which may have been more demanding on medical personnel than the non-pandemic period. Therefore, a similar study that assesses the regular work conditions and exposure of health care workers during the non-pandemic period should be replicated and compared with the result of the pandemic period.
Burnout was determined to contribute to SI occurrence; specifically, it mediated the relationships of SI with FUTP, FLLP, EOT, and IRWS. FLLP also mediated the relationship between SI and burnout, forming a vicious circle of burnout and FLLP that further increased the frequency of SIs. To the best of our knowledge, this finding has never been reported. The present findings serve as a reference for the management of mental health and the prevention of SIs among medical personnel worldwide.
Burnout affects approximately half of all nurses, physicians, and other clinicians. Sharps injuries, which frequently occur among health care workers, constitute a critical problem in the hospital.
Studies conducted in many countries revealed the relationship between burnout level (as measured using a routine questionnaire) and sharps injury deserves scholarly attention with regard to the prevention of work-related injuries among medical personnel. However, studies assessing the extent to which burnout affects sharps injuries are scarce.
To be established a model between sharps injuries, burnout, and the risk factors to assess the extent to which burnout affects sharps injuries.
A questionnaire was used for an observational and cross-sectional study, which was based on members at a hospital affiliated with a medical university in Taichung, Taiwan, in 2020. The valid responses constituted 68.5% (1734 of 2531). The items were drawn from the Nordic Musculoskeletal Questionnaire and Copenhagen burnout inventory and concerning work experience, occupational category, presence of chronic diseases, sleep duration, overtime work, and work schedule. Factor analysis, chi-square test, Fisher exact test, multiple linear, logistic regression, and Sobel test were conducted.
Our study found burnout was determined to contribute to sharps injuries occurrence; specifically, it mediated the relationships of sharps injuries with frequent musculoskeletal pain, overtime work, and irregular shift work.
Burnout was determined to contribute to SIs occurrence; specifically, it mediated the relationships of sharps injuries with frequent musculoskeletal pain, overtime work, and irregular shift work.
A similar study that assesses the regular work conditions and exposure of health care workers during the non-pandemic period should be replicated and compared with the result of the pandemic period.
Manuscript source: Unsolicited manuscript
Specialty type: Health care sciences and services
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Costantini R, Labusca L S-Editor: Liu M L-Editor: A P-Editor: Zhang YL
| 1. | Schaufeli WB, Greenglass ER. Introduction to special issue on burnout and health. Psychol Health. 2001;16:501-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 204] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 2. | Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, Trockel M, Goh J. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. 2019;170:784-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 516] [Article Influence: 86.0] [Reference Citation Analysis (0)] |
| 3. | Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, West CP. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1478] [Cited by in RCA: 1584] [Article Influence: 158.4] [Reference Citation Analysis (0)] |
| 4. | Thrush CR, Guise JB, Gathright MM, Messias E, Flynn V, Belknap T, Thapa PB, Williams DK, Nada EM, Clardy JA. A One-Year Institutional View of Resident Physician Burnout. Acad Psychiatry. 2019;43:361-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Klein J, Grosse Frie K, Blum K, von dem Knesebeck O. Burnout and perceived quality of care among German clinicians in surgery. Int J Qual Health Care. 2010;22:525-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Bagheri Hosseinabadi M, Ebrahimi MH, Khanjani N, Biganeh J, Mohammadi S, Abdolahfard M. The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. J Clin Nurs. 2019;28:1868-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 7. | Perumalswami CR, Griffith KA, Jones RD, Stewart A, Ubel PA, Jagsi R. Patterns of Work-Related Burnout in Physician-Scientists Receiving Career Development Awards From the National Institutes of Health. JAMA Intern Med. 2020;180:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Bogiatzaki V, Frengidou E, Savakis E, Trigoni M, Galanis P, Anagnostopoulos F. Empathy and burnout of healthcare professionals in public hospitals of Greece. Int J Car Sci. 2019;12:611-626. |
| 9. | Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood). 2012;31:2501-2509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 254] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 10. | Gander P, O'Keeffe K, Santos-Fernandez E, Huntington A, Walker L, Willis J. Fatigue and nurses' work patterns: An online questionnaire survey. Int J Nurs Stud. 2019;98:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Cai S, Lin H, Hu X, Cai YX, Chen K, Cai WZ. High fatigue and its associations with health and work related factors among female medical personnel at 54 hospitals in Zhuhai, China. Psychol Health Med. 2018;23:304-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS One. 2017;12:e0185781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 392] [Cited by in RCA: 635] [Article Influence: 79.4] [Reference Citation Analysis (0)] |
| 13. | Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443-2454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1042] [Cited by in RCA: 994] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 14. | Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003;102:167-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 810] [Cited by in RCA: 762] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 15. | Vecchiet L, Giamberardino MA, Saggini R. Myofascial pain syndromes: clinical and pathophysiological aspects. Clin J Pain. 1991;7 Suppl 1:S16-S22. [PubMed] |
| 16. | Elseviers MM, Arias-Guillén M, Gorke A, Arens HJ. Sharps injuries amongst healthcare workers: review of incidence, transmissions and costs. J Ren Care. 2014;40:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 17. | Cho E, Lee H, Choi M, Park SH, Yoo IY, Aiken LH. Factors associated with needlestick and sharp injuries among hospital nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. 2013;50:1025-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Nsubuga FM, Jaakkola MS. Needle stick injuries among nurses in sub-Saharan Africa. Trop Med Int Health. 2005;10:773-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | d'Ettorre G. Needlestick and Sharp Injuries Among Registered Nurses: A Case-Control Study. Ann Work Expo Health. 2017;61:596-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Yang AD, Quinn CM, Hewitt DB, Chung JW, Zembower TR, Jones A, Buyske J, Hoyt DB, Nasca TJ, Bilimoria KY. National Evaluation of Needlestick Events and Reporting Among Surgical Residents. J Am Coll Surg. 2019;229:609-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Smith DR, Choe MA, Jeong JS, Jeon MY, Chae YR, An GJ. Epidemiology of needlestick and sharps injuries among professional Korean nurses. J Prof Nurs. 2006;22:359-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Sohn JW, Kim BG, Kim SH, Han C. Mental health of healthcare workers who experience needlestick and sharps injuries. J Occup Health. 2006;48:474-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, Jørgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2798] [Cited by in RCA: 2615] [Article Influence: 68.8] [Reference Citation Analysis (0)] |
| 24. | Reardon M, Abrahams R, Thyer L, Simpson P. Review article: Prevalence of burnout in paramedics: A systematic review of prevalence studies. Emerg Med Australas. 2020;32:182-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 25. | Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate data analysis: With Readings. 4th ed. NJ: Prentice-Hall, 1995. |
| 26. | Kristensen TS, Borritz M, Villadsen E, Christensen KBJW. The Copenhagen burnout inventory: A new tool for the assessment of burnout. Work Stress. 2005;19:192-207. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1187] [Cited by in RCA: 1347] [Article Influence: 67.4] [Reference Citation Analysis (0)] |
| 27. | Chalghaf N, Guelmami N, Slimani M, Del Puente G, Re TS, Zerbetto R, Maldonado Briegas JJ, Guglielmi O, Garbarino S, Azaiez F, Bragazzi NL. Development and Preliminary Validation of the "Teacher of Physical Education Burnout Inventory" (TPEBI) in Arabic Language: Insights for Sports and Occupational Psychology. Front Psychol. 2019;10:456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1966] [Cited by in RCA: 3077] [Article Influence: 78.9] [Reference Citation Analysis (0)] |
| 29. | Mackinnon DP, Cox MC. Commentary on "Mediation Analysis and Categorical Variables: The Final Frontier" by Dawn Iacobucci. J Consum Psychol. 2012;22:600-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 30. | Dilie A, Amare D, Gualu T. Occupational Exposure to Needle Stick and Sharp Injuries and Associated Factors among Health Care Workers in Awi Zone, Amhara Regional State, Northwest Ethiopia, 2016. J Environ Public Health. 2017;2017:2438713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Lo WY, Chiou ST, Huang N, Chien LY. Long work hours and chronic insomnia are associated with needlestick and sharps injuries among hospital nurses in Taiwan: A national survey. Int J Nurs Stud. 2016;64:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Proctor SP, White RF, Robins TG, Echeverria D, Rocskay AZ. Effect of overtime work on cognitive function in automotive workers. Scand J Work Environ Health. 1996;22:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 33. | Kikuchi H, Odagiri Y, Ohya Y, Nakanishi Y, Shimomitsu T, Theorell T, Inoue S. Association of overtime work hours with various stress responses in 59,021 Japanese workers: Retrospective cross-sectional study. PLoS One. 2020;15:e0229506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 34. | Langballe EM, Innstrand ST, Hagtvet KA, Falkum E, Gjerløw Aasland O. The relationship between burnout and musculoskeletal pain in seven Norwegian occupational groups. Work. 2009;32:179-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Kotti N, Hajjaji M, Kchaou A, Sellami I, Masmoudi ML, Masmoudi J, Jmal KH. Burnout and occupational accident. Eur Psych. 2017;41:S324-S325. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Wang S, Yao L, Li S, Liu Y, Wang H, Sun Y. Sharps injuries and job burnout: a cross-sectional study among nurses in China. Nurs Health Sci. 2012;14:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Alexandrova-Karamanova A, Todorova I, Montgomery A, Panagopoulou E, Costa P, Baban A, Davas A, Milosevic M, Mijakoski D. Burnout and health behaviors in health professionals from seven European countries. Int Arch Occup Environ Health. 2016;89:1059-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 38. | Arlinghaus A, Lombardi DA, Willetts JL, Folkard S, Christiani DC. A structural equation modeling approach to fatigue-related risk factors for occupational injury. Am J Epidemiol. 2012;176:597-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 39. | Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, Aromaa A, Lönnqvist J. The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 168] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 40. | Akbari H, Kashani M, Asadi Z, Kaveh M, Hannani M. The correlation between occupational unsafe acts and job burnout among workers in Kashan metal melting industries 2017. Int Arch Health Sci. 2019;6:148-153. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |