Published online Sep 6, 2021. doi: 10.12998/wjcc.v9.i25.7292
Peer-review started: March 17, 2021
First decision: May 5, 2021
Revised: May 12, 2021
Accepted: August 5, 2021
Article in press: August 5, 2021
Published online: September 6, 2021
Processing time: 166 Days and 14.3 Hours
Radiation therapy (RT) is considered one of the cornerstone modalities of treatment for different cancer types. The preparation and delivery of RT requires a number of staff members from different disciplines within the radiation oncology department. Since the emergence of the corona virus disease 2019 (COVID-19) pandemic, RT, similar to other cancer care modalities, has been adapted to minimize patient and staff exposure without compromising the oncological outcomes. This was reflected in the dramatic practice changes that occurred in the past year to address the lockdown restrictions and fulfill the infection control requirements. RT practices differ across regions based on financial and training levels, and developing countries with limited resources have struggled to maintain radiation treatment services at a level equivalent to that in developed countries while following pandemic control guidelines. The response during the COVID-19 pandemic varied between developing countries according to the infection rate and RT technological capabilities. In this editorial, we review recently published articles addressing radiotherapy practice reports during the COVID-19 pandemic in developing countries.
Core Tip: This editorial discusses the impact of corona virus disease 2019 (COVID-19) pandemic on radiation oncology practice in developing countries. The challenges and measures taken to mitigate COVID19 and its ramifications.
- Citation: Abuhijla F, Abuhijlih R, Mohamad I. Radiation oncology practice during COVID-19 pandemic in developing countries. World J Clin Cases 2021; 9(25): 7292-7296
- URL: https://www.wjgnet.com/2307-8960/full/v9/i25/7292.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i25.7292
The estimated increase in new cancer cases will be more than 24 million in 2030, and this problem is a growing challenge for healthcare systems, especially in low- and middle-income countries[1]. Radiation therapy (RT) is an integral part of multidisciplinary cancer care, and approximately half of all cancer patients will receive radioth
In early 2020, severe acute respiratory syndrome coronavirus 2 infections started to spread uncontrollably. In March 2020, the World Health Organization announced that the corona virus disease 2019 (COVID-19) outbreak was a pandemic; since then, many countries in the world have been forced to implement partial and complete lockdowns that have lasted for months. Variations in the status of the pandemic and governmental actions coupled with insufficient resources could result in a greater impact and worse poorer outcomes, leading to a higher risk to the safety of health care providers in developing countries that could aggravate the crisis[5].
During this time, hospitals worldwide were experiencing an increased number of patients and a lack of medical supplies. Elective surgeries and interventions were postponed due to hospital crowding and the fear of infection. Elective cancer procedures were cancelled or postponed as well, which resulted in delays in cancer diagnosis and treatment and psychological distress on the part of the patients and their families.
RT has changed dramatically during the past year, and these changes were implemented to cope with lockdown restrictions and to fulfill infection control requirements[6]. Developing countries have struggled to maintain radiation treatment services at a level equivalent to that in developed countries while following pandemic control guidelines[7]. In China, during COVID-19 pandemic outbreak; lock down resulted in treatment interruptions in more than 50% of patients who were on active chemoradiation[8].
Changes to RT practices depended on regional factors such as financial and training levels. The implemented modifications included postponing elective radiation treatment, utilizing hypofractionated regimens and encouraging online (remote) access to radiotherapy planning and quality control systems to decrease direct physical contact[9].
The financial burden of cancer care has always been a main concern in low- and middle-income countries, as their healthcare systems already face diverse problems due to the poor infrastructure, lack of funding and absence of effective administrative and strategic planning. The consequences of the COVID-19 pandemic exacerbated these financial problems[10].
The response to the COVID-19 pandemic varied among developing countries according to the infection rate in the region and the RT technological capabilities in the country. The presence of a strong information technology (IT) infrastructure enabled the developed world to switch smoothly to online and remote workflows. In developing countries, the situation was the opposite: a lack of financial and IT support led to a poor response to the pandemic and a failure to quickly adapt practices to the current situation. Developing countries are facing multiple financial and social complications as a result of the pandemic, and prioritizing COVID-19 patients has led to the cancelation and postponement of treatment for many cancer patients. Some countries are affected by war and lack health care systems. All these challenges should be addressed in developing countries. Future planning and international support will be crucial to help developing countries overcome this pandemic.
During the COVID-19 pandemic, most cancer centers around the world have adopted alternative oncological guidelines to adapt to the circumstances, including using a hypofractionated RT regimen or shifting the RT start date. However, hypofractionated regimens usually require careful planning and delivery, as they involve giving a higher dose with a lower number of fractions, which means that the impact of target inaccuracy could have a worse effect on tumor control and increase the risk of damage to adjacent organs. In addition, a delay in RT can sometimes result in poor outcomes. This leads us to question prior to implementing a new practice whether a delay or change is oncologically justifiable[11].
One major change that has occurred in response to the pandemic is the shift towards telemedicine and the development of a virtual clinic workflow for RT. Reducing hospital visits and minimizing contact were not the only advantages of virtual clinics; virtual clinics also provide more flexibility during discussions with patient and family members and eliminate the need for waiting rooms. However, for exams and investigations, the patient still has to present to the clinic in person. Proper planning to make the clinical visit worthwhile should be performed[12,13].
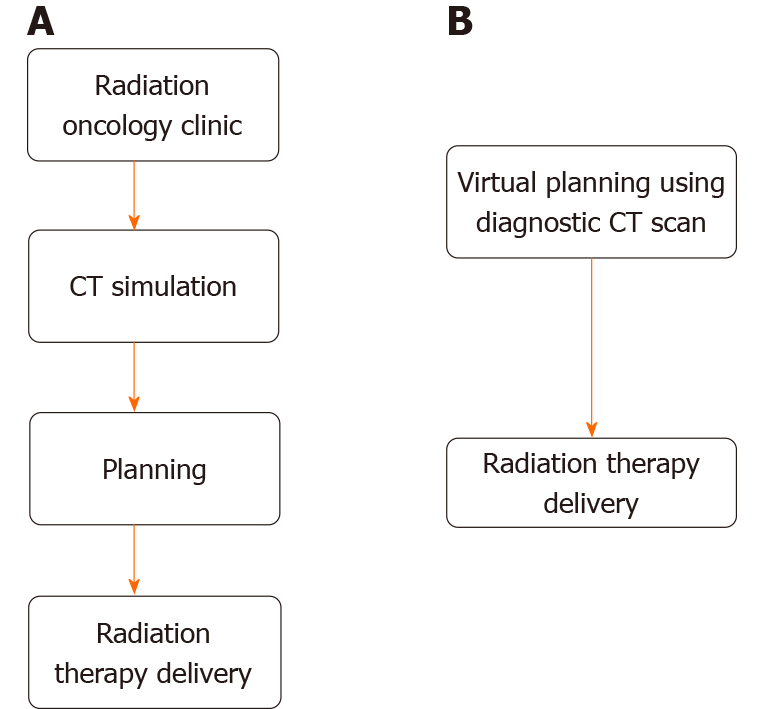
In life-threatening situations such as those involving bleeding and spinal cord compression, in which RT needs to be delivered urgently, the use of a hypofractionated regimen is preferable to achieve a more rapid response; the use of these regimens also adheres to the protocols in place during the COVID-19 pandemic[14]. It may also be possible to omit computed tomography (CT) simulations and to use diagnostic CT as an alternative fast track to RT during emergencies[15], this will help to minimize exposure and short preparation time as shown in Figure 1.
A recent systematic review published by Donkor et al[16] addressed the approaches used to mitigate the impact of COVID-19 on radiotherapy centers in low- and middle-income countries. Eleven studies were included in review, and the methods used to cope with COVID-19 in RT departments were as follows: forming COVID-19 response multidisciplinary teams; increasing the use of telemedicine; modifying the layout of waiting areas; reducing staff; isolating patients suspected of having COVID-19; and adopting triage systems.
COVID-19 vaccines are now available, and the number of infections is expected to decrease; as a result, quarantine measures are expected to be eased. Regardless of whether the general public is willing to be vaccinated, cancer patients should be prioritized for vaccination once it becomes available due higher morbidity and mortality among COVID-19 patients with cancer[17,18]. Unfortunately, access to the vaccine is not equal, and wealthy, developed countries are currently receiving the vaccines that are being produced. Unequal access will slow recovery in developing countries and add to the current challenges.
Adapted guidelines and protocols should be implemented at the national and institutional levels in RT units in developing countries to cope with the rapid changes in RT practices and to enable them to continue to serve patients. Collecting and sharing data is crucial to building a better understanding. More vaccination campaigns should be implemented in developing countries to minimize the burden of the pandemic on cancer care in general and more specifically on RT.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: Jordan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kawabata H, Sun Y S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Jaffray DA, Knaul FM, Atun R, Adams C, Barton MB, Baumann M, Lievens Y, Lui TY, Rodin DL, Rosenblatt E, Torode J, Van Dyk J, Vikram B, Gospodarowicz M. Global Task Force on Radiotherapy for Cancer Control. Lancet Oncol. 2015;16:1144-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Atun R, Jaffray DA, Barton MB, Bray F, Baumann M, Vikram B, Hanna TP, Knaul FM, Lievens Y, Lui TY, Milosevic M, O'Sullivan B, Rodin DL, Rosenblatt E, Van Dyk J, Yap ML, Zubizarreta E, Gospodarowicz M. Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 664] [Cited by in RCA: 726] [Article Influence: 72.6] [Reference Citation Analysis (0)] |
| 3. | Hanna TP, Shafiq J. Estimating the population benefit of radiotherapy: using demand models to estimate achievable cancer outcomes. Clin Oncol (R Coll Radiol). 2015;27:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Zubizarreta EH, Fidarova E, Healy B, Rosenblatt E. Need for radiotherapy in low and middle income countries – the silent crisis continues. Clin Oncol (R Coll Radiol). 2015;27:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 217] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 5. | Abu Hammad O, Alnazzawi A, Borzangy SS, Abu-Hammad A, Fayad M, Saadaledin S, Abu-Hammad S, Dar Odeh N. Factors Influencing Global Variations in COVID-19 Cases and Fatalities; A Review. Healthcare (Basel). 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Gostin LO, Wiley LF. Governmental Public Health Powers During the COVID-19 Pandemic: Stay-at-home Orders, Business Closures, and Travel Restrictions. JAMA. 2020;323:2137-2138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 257] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 7. | Baskar R, Itahana K. Radiation therapy and cancer control in developing countries: Can we save more lives? Int J Med Sci. 2017;14:13-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Xie C, Wang X, Liu H, Bao Z, Yu J, Zhong Y, Chua MLK. Outcomes in Radiotherapy-Treated Patients With Cancer During the COVID-19 Outbreak in Wuhan, China. JAMA Oncol. 2020;6:1457-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Mohindra P, Buckey CR, Chen S, Sio TT, Rong Y. Radiation therapy considerations during the COVID-19 Pandemic: Literature review and expert opinions. J Appl Clin Med Phys. 2020;21:6-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Kugbey N, Ohene-Oti N, Vanderpuye V. COVID-19 and its ramifications for cancer patients in low-resource settings: Ghana as a case study. Ecancermedicalscience. 2020;14:ed99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Nagar H, Formenti SC. Cancer and COVID-19 - potentially deleterious effects of delaying radiotherapy. Nat Rev Clin Oncol. 2020;17:332-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 12. | Gutkin PM, Prionas ND, Minneci MO, Allen E 3rd, Balazy KE, Rahimy E, Chang DT, Horst KC. Telemedicine in Radiation Oncology: Is It Here to Stay? Int J Radiat Oncol Biol Phys. 2020;108:416-420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Maroongroge S, Smith B, Bloom ES, Ning MS, Wang C, Das P, Koong AC, McAleer MF, Woodhouse KD. Telemedicine for Radiation Oncology in a Post-COVID World. Int J Radiat Oncol Biol Phys. 2020;108:407-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Yerramilli D, Xu AJ, Gillespie EF, Shepherd AF, Beal K, Gomez D, Yamada J, Tsai CJ, Yang TJ. Palliative Radiation Therapy for Oncologic Emergencies in the Setting of COVID-19: Approaches to Balancing Risks and Benefits. Adv Radiat Oncol. 2020;5:589-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Nierer L, Walter F, Niyazi M, Shpani R, Landry G, Marschner S, von Bestenbostel R, Dinkel D, Essenbach G, Reiner M, Belka C, Corradini S. Radiotherapy in oncological emergencies: fast-track treatment planning. Radiat Oncol. 2020;15:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Donkor A, Atuwo-Ampoh VD, Opie C, Yakanu F, Lombe D, Khader J. Novel coronavirus mitigation measures implemented by radiotherapy centres in low and middle-income countries: a systematic review. Rep Pract Oncol Radiother. 2021;26:303-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Ribas A, Sengupta R, Locke T, Zaidi SK, Campbell KM, Carethers JM, Jaffee EM, Wherry EJ, Soria JC, D'Souza G; AACR COVID-19 and Cancer Task Force. Priority COVID-19 Vaccination for Patients with Cancer while Vaccine Supply Is Limited. Cancer Discov. 2021;11:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 153] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 18. | Zhang H, Wang L, Chen Y, Wu Q, Chen G, Shen X, Wang Q, Yan Y, Yu Y, Zhong Y, Wang X, Chua MLK, Xie C. Outcomes of novel coronavirus disease 2019 (COVID-19) infection in 107 patients with cancer from Wuhan, China. Cancer. 2020;126:4023-4031. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (1)] |