Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7285
Peer-review started: May 12, 2021
First decision: June 15, 2021
Revised: June 16, 2021
Accepted: July 6, 2021
Article in press: July 6, 2021
Published online: August 26, 2021
Processing time: 103 Days and 21.8 Hours
Intervertebral disc calcification (IDC) combined with ossification of the posterior longitudinal ligament (OPLL) in cervical discs is rarely reported. This case study presents a rare case of IDC combined with OPLL in the C2-C3 segment.
Here, we present a case of a 6-year-old Asian boy with severe neck pain and stiffness. Physical examination showed no neurological or other abnormalities. Digital radiography and computed tomography (CT) revealed a calcified intervertebral disc and OPLL at the C2-C3 vertebrae. The spinal canal compromise at C2-C3 was approximately 50% on magnetic resonance imaging. The final diagnosis was IDC combined with OPLL. We applied a neck brace for the patient to protect the neck. The patient's neck pain and stiffness recovered significantly within approximately 3 wk. At the 3 mo follow-up, the follow-up CT showed resolution of the ossified intervertebral disc herniation, and a small amount of calcification and slight OPLL remained at the involved segment.
IDC combined with OPLL is a relatively rare condition in children. However, the majority of patients could have a favorable outcome, and the ossified mass in the canal would be spontaneously resolved with conservative therapy.
Core Tip: Intervertebral disc calcification (IDC) with ossification of the posterior longitudinal ligament (OPLL) is rare. At present, there is no consensus on the diagnosis and treatment of the disease. If the disease is not recognized, it is easily misdiagnosed and leads to unnecessary treatment. In addition, there are few reports of upper cervical IDC with OPLL, which may limit doctors’ awareness of the disease. This case study presents a rare case of IDC combined with OPLL in the C2-C3 segment to help diagnose and treat the disease.
- Citation: Wang XD, Su XJ, Chen YK, Wang WG. Regression of intervertebral disc calcification combined with ossification of the posterior longitudinal ligament: A case report. World J Clin Cases 2021; 9(24): 7285-7291
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7285.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7285
Intervertebral disc calcification (IDC) with ossification of the posterior longitudinal ligament (OPLL) is rare. To date, only 8 cases of IDC with OPLL in children have been reported[1-7]. Of the 8 reported cases, 6 were in the cervical spine and 2 were in the thoracic spine. Finally, the clinical symptoms of all patients disappeared after conservative treatment. However, according to imaging evaluation, 4 patients recovered completely[2,4,6,7], 1 patient had persistent mild OPLL[3], 2 patients had persistent mild IDC[4,5], and 1 patient had progressive IDC1. All reported patients had neck pain or back pain to varying degrees due to the IDC and OPLL extending into the spinal canal, compressing the spinal cord or nerve root, and all went to the hospital with or without neurological defects. This does not exclude the possibility that some patients with IDC with OPLL have not been identified and reported due to their absence of symptoms. At present, there is no accepted treatment standard for this disease and conservative treatment is usually the first choice this kind of patient[3,6]. According to the results of a literature search, there are few reports of upper cervical IDC with OPLL, which may limit doctors’ awareness of the disease.
This case study presents a rare case of IDC combined with OPLL in the C2-C3 segment to help diagnose and treat the disease.
A 6-year-old Asian boy complained of severe neck pain and limited neck movement for 3 d.
During a handstand performed while hip-hop dancing 3 d ago, the patient accidentally landed on the ground on his neck. He subsequently presented with severe neck pain and stiffness. The symptoms continued to worsen without improvement, so his parents took him to the spine department.
The patient had no significant medical history.
The patient had no remarkable personal and family history.
Physical examination showed no neurological or other abnormalities.
Laboratory examinations showed no significant abnormalities.
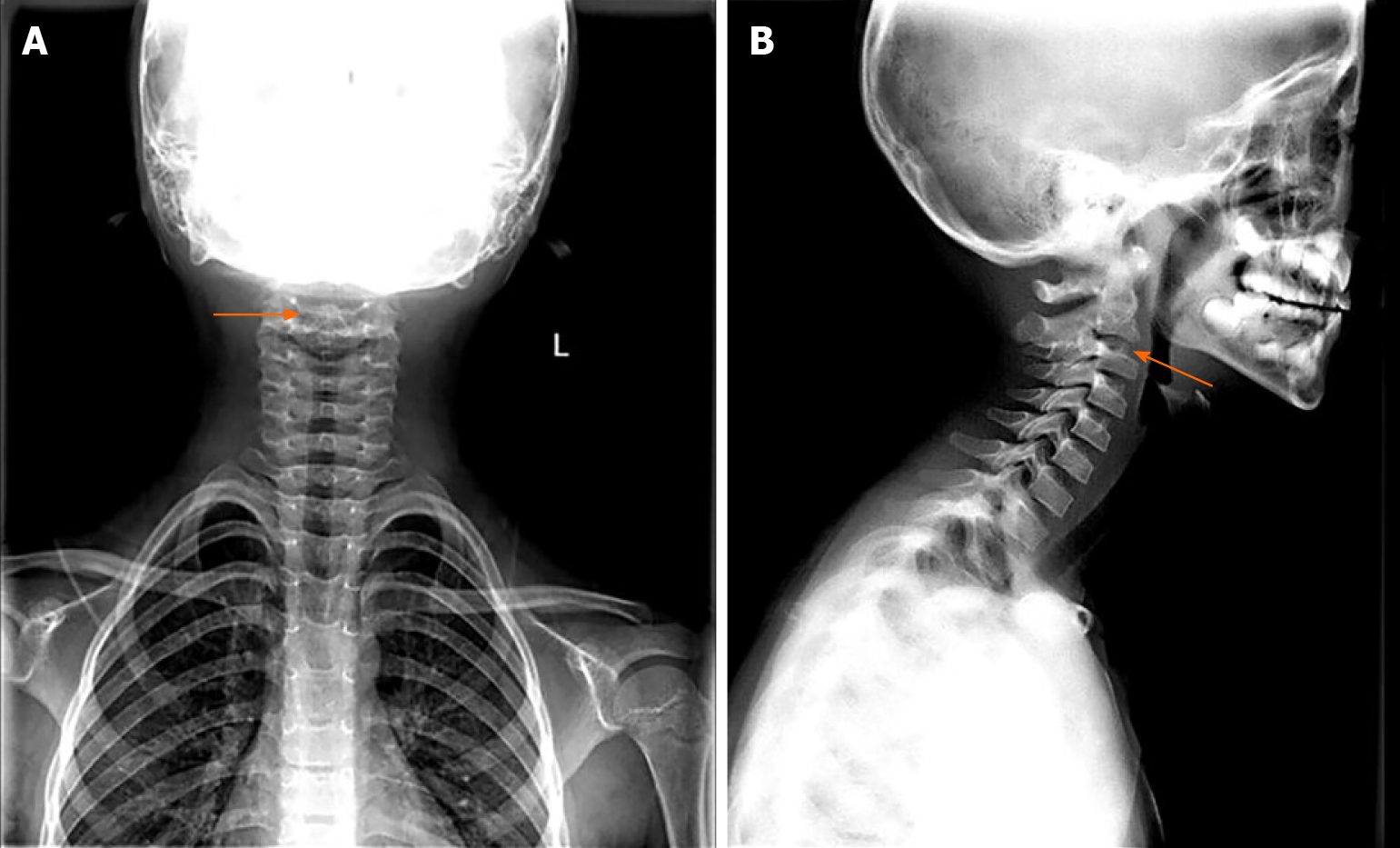
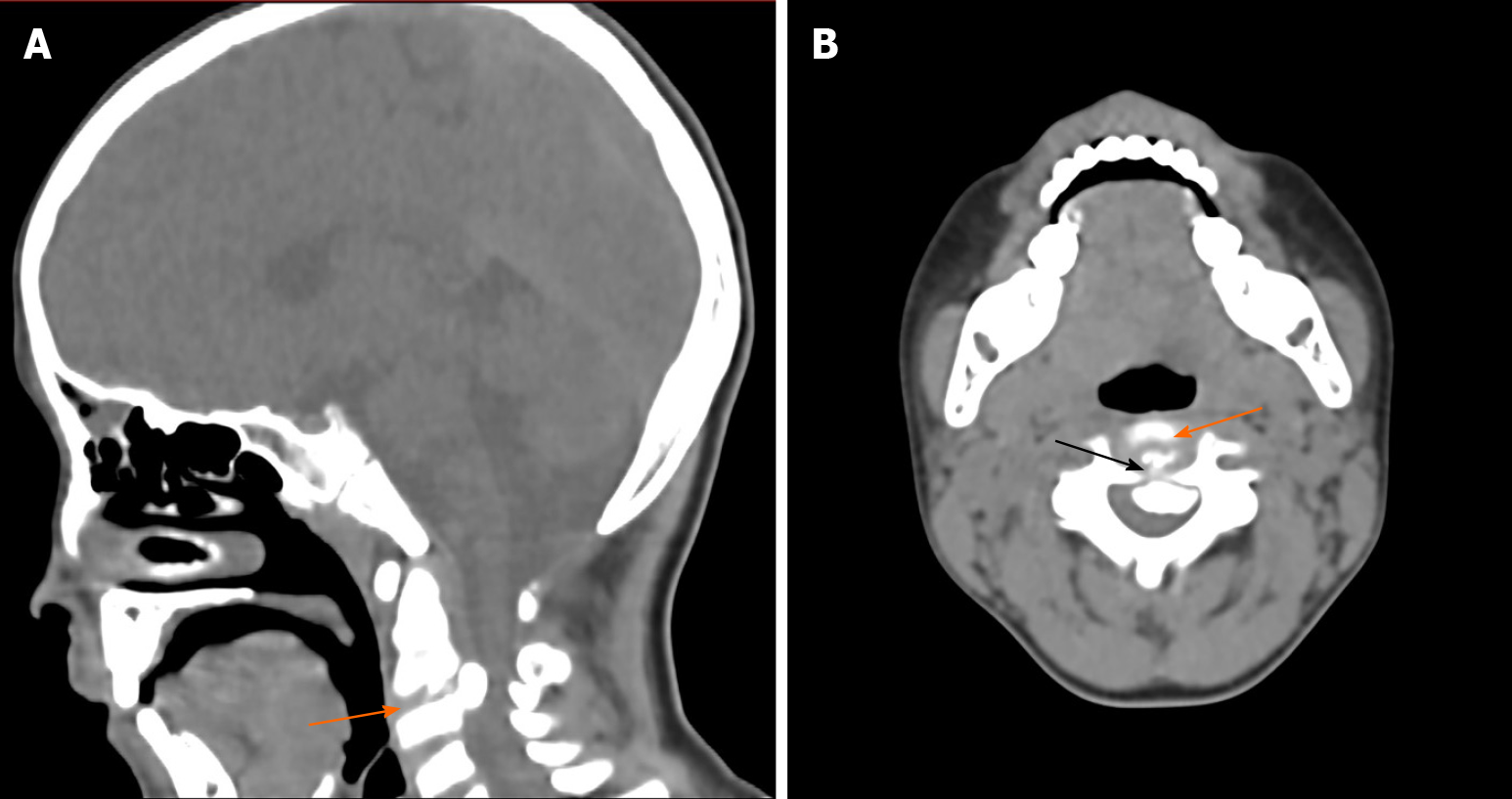
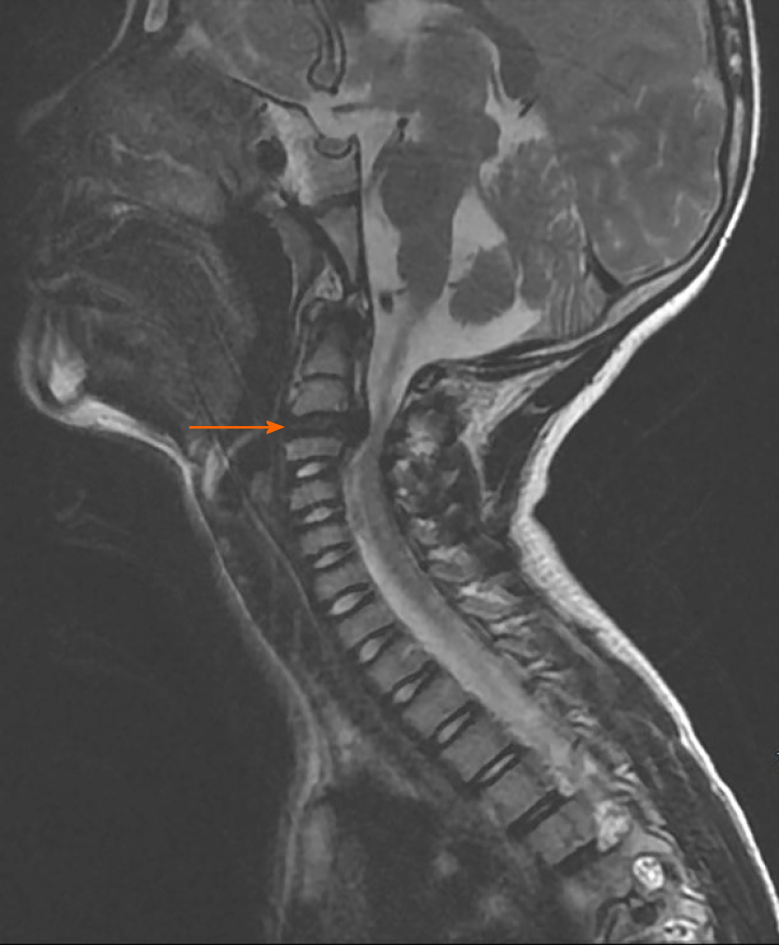
Digital radiography (DR) showed a dense projection of the intervertebral disc between the second and third cervical vertebrae (Figure 1). Then computed tomography (CT) further demonstrated cervical disc calcification and partial OPLL in the C2-C3 segment (Figure 2). Magnetic resonance imaging (MRI) of the cervical spine revealed cervical disc herniation, resulting in a certain degree of spinal cord compression (Figure 3). The degree of spinal canal compromise was defined as a percentage that was calculated by dividing the smallest sagittal diameter of the spinal canal at the level of the disc herniation by the mean sagittal diameter at adjacent levels cephalad and caudad to the herniated disc as seen on CT or MRI[8]. According to the rough estimation by MRI, the spinal canal compromise at C2-C3 was approximately 50%.
According to the above findings, IDC combined with OPLL was diagnosed.
Considering that his symptoms were not very serious and that this disease was benign and self-limited, the patient was treated with a neck brace for protection.
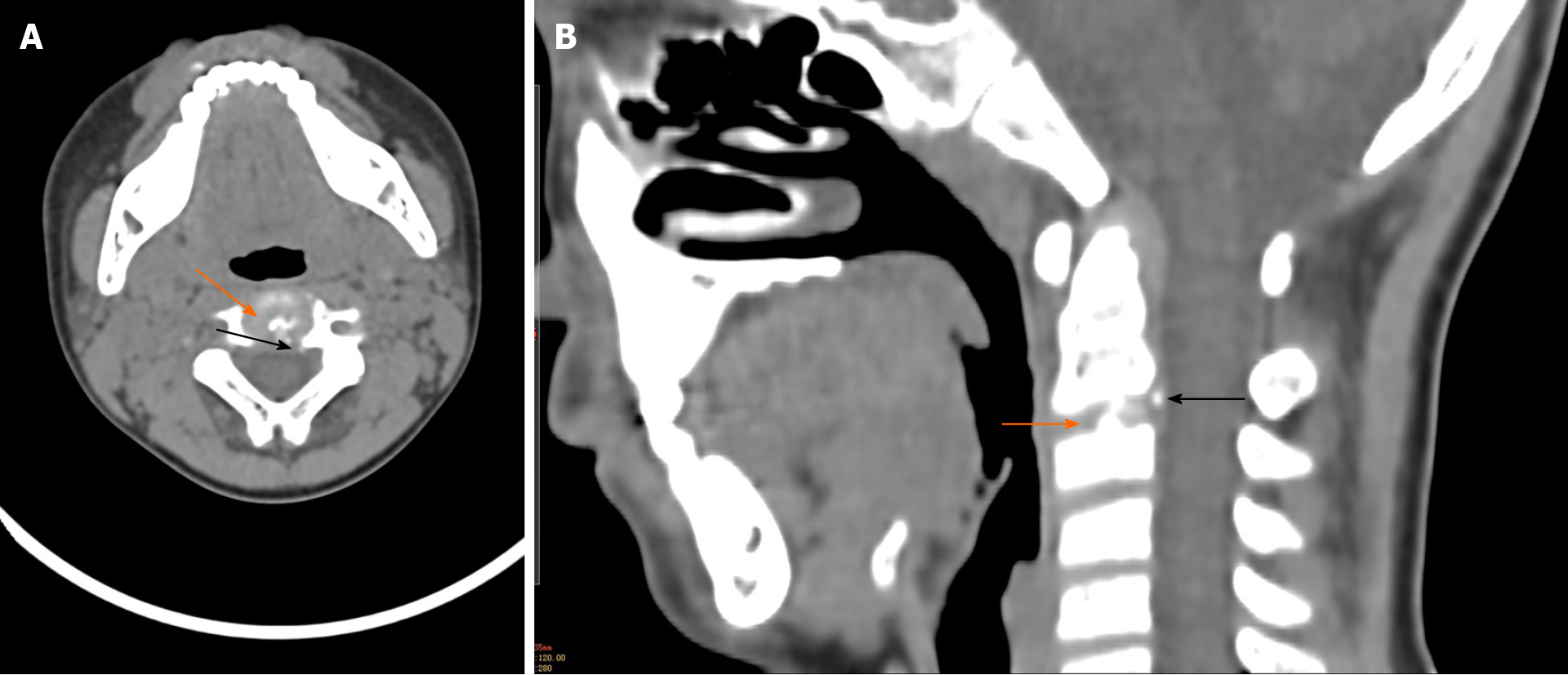
The patient reported significant relief in his neck pain after the cervical spine was immobilized. Then the patient was discharged from the hospital, and his parents were instructed to take good care of him to avoid new accidental falls and any other injuries. The patient's neck pain and stiffness recovered significantly within approximately 3 wk. At the 3 mo follow-up, the patient felt no discomfort. Follow-up CT showed resolution of the ossified intervertebral disc herniation, and only a small amount of calcification and slight OPLL remained (Figure 4). The patient and his parents expressed satisfaction with the treatment and expressed their sincere gratitude to the doctors.
IDC in children is a rare spinal disorder that was first reported in 1924[9]. OPLL is usually considered a degenerative cervical or thoracic pathology in adults and was first reported in 1838[10]. IDC combined with OPLL in pediatric patients is much less frequent, and to date only 8 cases have been published[1-7].
The patients in the previously reported cases were two men and six women, aged 6-years-old to 11-years-old. In general, the injury occurs in a single segment of the disc, and a few cases have also involved two parts of the disc[1,4,6,7]. In the imaging examinations of the reported cases, abnormal signs of intervertebral discs were seen, and the masses penetrated into the spinal canal and compressed the spinal cord. However, masses in the spinal canal are not easily identified as a calcified disc herniation or OPLL. In addition, rarely herniated calcified discs protrude laterally into the transverse foramen[11]. Therefore, if the disease is not recognized, it is easily misdiagnosed and leads to unnecessary treatment.
The exact cause of IDC accompanied by OPLL is still unclear. However, trauma is often considered an inducer because some children’s disc calcifications occur before trauma[12,13]. Beluffi et al[9] suggested that there are two types of IDC: Symptomatic and asymptomatic. Matsunaga et al[10] studied the natural course of OPLL and found that 90% of OPLL patients had clinical symptoms; 23% of OPLL patients had a history of neck trauma. Therefore, we presume that IDC may be in a stable period with no clinical symptoms, and due to the presence of asymptomatic IDC, OPLL can be induced by herniated IDC in an accidental cervical trauma. Disc calcification leads to a decrease in T2-weighted signal strength on MRI, which is considered an imaging manifestation of disc degeneration[14]. In children, calcification mainly affects the nucleus pulposus[15]. The presence of a calcified nucleus pulposus may affect the stress balance of the affected intervertebral disc, which leads to the nucleus pulposus protruding and compressing, stimulating and causing an inflammatory reaction within the posterior longitudinal ligament. Chronic inflammatory stimulation leads to ossification and further aggravation of the compression. Any trauma to the area is an important inducer that leads to further backward penetration of the intervertebral disc into the spinal canal, compression of the spinal cord or nerve root, and corresponding clinical symptoms. The increase in erythrocyte sedimentation rate indicates that the disease is related to inflammation[16]. During conservative treatment, due to the inflammatory reaction, the blood supply to the lesion increases, which provides a basis for the spontaneous disappearance of the calcification in the herniated disc and the ossification in posterior longitudinal ligament. Simple IDC disappears in 3 to 60 mo, with an average of 15 mo[8]. However, after 9 years of follow-up, Du et al[4,12] found that residual IDC persisted and the height of the affected intervertebral space had become narrow, indicating that residual IDC may not subside spontaneously with time.
The main symptoms of IDC accompanied by OPLL are neck pain, stiffness, torticollis, and neck movement limitation. Physical examination can often reveal neck muscle spasms, tenderness at the lesion site, and limited neck movement. If there is nerve root or spinal cord compression, there may be corresponding signs of nervous system defects[12,15]. In the reported cases, the most frequently reported symptoms were neck pain. Similarly, neck pain was the main symptom in this case. Ninety-five percent of OPLL in adults is clinically symptomatic, with different degrees of myelopathy and radiculopathy[10]. However, child OPLL is different from adult OPLL. Although the imaging manifestations are very serious, the spinal canal compromise at C2-C3 could be approximately 50% but the clinical symptoms are not serious, and few children have neurological defects[2,4].
At present, there is no consensus on the diagnosis of the disease. We suggest that the following characteristics may be helpful for a preliminary diagnosis: local pain in the cervical or thoracic region, full or limited cervical motion, and high-density areas and ossified mass on DR and CT. MRI can be recommended to identify compression of the spinal cord. Generally, imaging findings are the main basis for diagnosis[15]. However, for this disease, there exists a possibility that the imaging performance and clinical symptoms are inconsistent[1,2,5-7,12].
At present, it is believed that conservative treatment including bed rest, brace braking, traction, and drugs should be prioritized[1-7]. However, traction has an uncertain outcome in patients with compressed cervical spinal cord because it has the possibility of aggravating the spinal cord compression[17]. If the calcification protrudes into the spinal canal, traction is contraindicated given the possibility of aggravating the spinal cord compression. For patients with no or mild neurological dysfunction, even without intervention, recovery is still possible within several weeks[2]. Patients receiving conservative treatment should focus on avoiding injury and must be closely followed up and return to the hospital immediately in case of aggravation of nerve compression symptoms. The symptoms could be totally relieved with conservative therapy, and the ossified mass can automatically regress in 3-6 mo[1-3,5,6], but in some cases, as much as 1-2 years may be needed[4,7]. When the patient has severe neurologic deficits and the disease continuously progresses, surgical intervention should be considered[18].
IDC combined with OPLL is rare, but we must be aware of its presence. The exact etiology is still unclear. Conservative treatment is usually effective. Clinical symptoms may subside in weeks to months without recurrence. The majority of patients may have a favorable outcome, and the ossified mass in the canal would be spontaneously resolved with conservative therapy in 3 mo to 2 years. However, slight IDC or OPLL may remain for a long time.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaur M S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Liu JH
| 1. | Fu Z, Shi J, Jia L Jr, Yuan W Jr, Guan Z. Intervertebral thoracic disc calcification associated with ossification of posterior longitudinal ligament in an eleven-year-old child. Spine (Phila Pa 1976). 2011;36:E808-E810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Zhu J, Sun K, Xu X, Sun J, Kong Q, Wang S, Shi J. A Preliminary Attempt of Nonintervention in the Treatment of Patients with Intervertebral Disc Calcification Combined with Ossification of the Posterior Longitudinal Ligament. World Neurosurg. 2019;129:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | O'Dell MC, Flores M, Murray JV Jr. Pediatric Idiopathic Intervertebral Disc Calcification. Pediatr Neurol. 2016;61:115-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Du JJ, Meng H, Cao YJ, Li FQ, Luo ZJ. Calcification of the intervertebral disc and posterior longitudinal ligament in children. J Spinal Disord Tech. 2012;25:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Wang G, Kang Y, Chen F, Wang B. Cervical intervertebral disc calcification combined with ossification of posterior longitudinal ligament in an-11-year old girl: case report and review of literature. Childs Nerv Syst. 2016;32:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Mizukawa K, Kobayashi T, Yamada N, Hirota T. Intervertebral disc calcification with ossification of the posterior longitudinal ligament. Pediatr Int. 2017;59:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Li CH, Lui TH, Ngai WK. Acute calcification of intervertebral disc and posterior longitudinal ligament in a 7-year-old girl: a case report. J Orthop Surg (Hong Kong). 2016;24:424-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Dai LY, Ye H, Qian QR. The natural history of cervical disc calcification in children. J Bone Joint Surg Am. 2004;86:1467-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Beluffi G, Fiori P, Sileo C. Intervertebral disc calcifications in children. Radiol Med. 2009;114:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976). 2012;37:E309-E314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 11. | Mac-Thiong JM, Leduc S, Marton D, Duhaime M, Morin B. Herniation of a calcified cervical disc into the foramen transversarium in an 8-year-old child. Spine (Phila Pa 1976). 2004;29:E349-E352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Du JJ, Chen YF, Peng Y, Li XJ, Ma W. Calcification of the intervertebral disc and ossification of posterior longitudinal ligament in children. BMC Musculoskelet Disord. 2018;19:316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Boody BS, Lendner M, Vaccaro AR. Ossification of the posterior longitudinal ligament in the cervical spine: a review. Int Orthop. 2019;43:797-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 14. | Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26:1873-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2447] [Cited by in RCA: 2853] [Article Influence: 118.9] [Reference Citation Analysis (0)] |
| 15. | Coppa V, Marinelli M, Martiniani M, Giacchetta AM, Gigante AP, Specchia N. Pediatric intervertebral disc calcification: case series and systematic review of the literature. J Pediatr Orthop B. 2020;29:590-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Tsutsumi S, Yasumoto Y, Ito M. Idiopathic intervertebral disk calcification in childhood: a case report and review of literature. Childs Nerv Syst. 2011;27:1045-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Sumi M, Miyamoto H, Suzuki T, Kaneyama S, Kanatani T, Uno K. Prospective cohort study of mild cervical spondylotic myelopathy without surgical treatment. J Neurosurg Spine. 2012;16:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Schaser KD, Stover JF, Kaeaeb MJ, Haas NP, Mittlmeier T. Mild cervical spine trauma showing symptomatic calcified cervical disc herniation in a child: a case report. Spine (Phila Pa 1976). 2003;28:E93-E94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |