Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7261
Peer-review started: April 29, 2021
First decision: June 3, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 26, 2021
Processing time: 117 Days and 0.2 Hours
Alimentary tract duplication is a rare congenital disease that may occur in any part of the alimentary tract, whereas thoracoabdominal duplications only account for approximately 2% of all alimentary tract duplication cases. Many symptoms, including abdominal pain, abdominal distension, vomiting, gastrointestinal bleeding, chest discomfort, chest pain, and shortness of breath, may be present in patients with abdominal or thoracic duplication.
A 10-mo-old infant, with a free previous medical history, was admitted to our hospital with melena three times in 6 d. Enhanced magnetic resonance imaging of the thoracic vertebrae revealed multiple cervicothoracic vertebral deformities, spina bifida, meningomyelocele towards the posterior mediastinum, and possible concurrent infection. Upper gastroenterography indicated intestinal malrotation. A laparoscopic abdominal examination was performed, and the operation was intraoperatively converted to laparotomy. This case was diagnosed intraoperatively as thoracoabdominal intestinal duplication. The intestinal duplications in the abdomen and large part of the thorax were excised. The results of postoperative pathological examination confirmed that this case was alimentary tract duplication and that part of the duplication contained gastric mucosa. The infant recovered well and was discharged 1 wk after the surgery. A follow-up computed tomography scan 3 mo after operation showed myelomeningocele while the posterior mediastinal cyst was significantly reduced.
Thoracoabdominal duplication should be considered if a child has suspected abdominal intestinal duplication with hematochezia as an onset symptom.
Core Tip: Small intestine duplication is the most common type of alimentary tract duplication, whereas thoracoabdominal duplications only account for approximately 2% of all alimentary tract duplication cases. Many symptoms, including abdominal pain, abdominal distension, vomiting, gastrointestinal bleeding, chest discomfort, chest pain, and shortness of breath, may be present in patients with abdominal or thoracic duplication. If a child has suspected abdominal intestinal duplication with hema
- Citation: Yang SB, Yang H, Zheng S, Chen G. Thoracoabdominal duplication with hematochezia as an onset symptom in a baby: A case report. World J Clin Cases 2021; 9(24): 7261-7268
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7261.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7261
Alimentary tract duplication is a rare congenital disease that may occur in any part of the alimentary tract. Small intestine duplication is the most common type, whereas thoracoabdominal duplications only account for approximately 2% of all alimentary tract duplication cases. Thoracoabdominal duplication is intrathoracic extension of duplication that originates from the gastrointestinal system, which passes through the diaphragmatic fissure and enters the posterior mediastinum. Approximately 60%-70% of thoracoabdominal duplications originate from the jejunum and duodenum[1]. Many symptoms, including abdominal pain, abdominal distension, vomiting, gastrointestinal bleeding, chest discomfort, chest pain, and shortness of breath, may be present in patients with abdominal or thoracic duplication. Here, we report the case of a 10-mo-old infant with thoracoabdominal duplication who was admitted to our hospital for hematochezia.
A 10-mo-old infant was admitted to our hospital with melena three times in 6 d.
Six days prior to admission to our hospital, the infant passed dark stools once and had no symptoms such as fever, abdominal pain, diarrhea, and vomiting. On the next day, the infant defecated dark stools twice, and his face became cyanotic when he cried. He was sent to a local hospital for treatment. Routine blood examination showed a white blood cell count of 13.17 × 109 and hemoglobin level of 60 g/L. According to the chest X-ray, the left 5th and 6th ribs displayed fusion-like changes, and the lower posterior mediastinum showed patchy shadows. Abdominal ultrasound indicated that the liver was enlarged and irregularly shaped, and the mesenteric lymph nodes were swollen. The infant was admitted to the pediatric intensive care unit and was given symp
The patient had a free previous medical history.
The patient had no family history that was related to the present illness.
Physical examination showed that the infant’s abdomen was flat and soft. There was no significant tenderness or muscle guarding or obvious lumps.
Emergency complete blood cell counting showed a white blood cell count of 11.1 × 109 and hemoglobin level of 113 g/L.
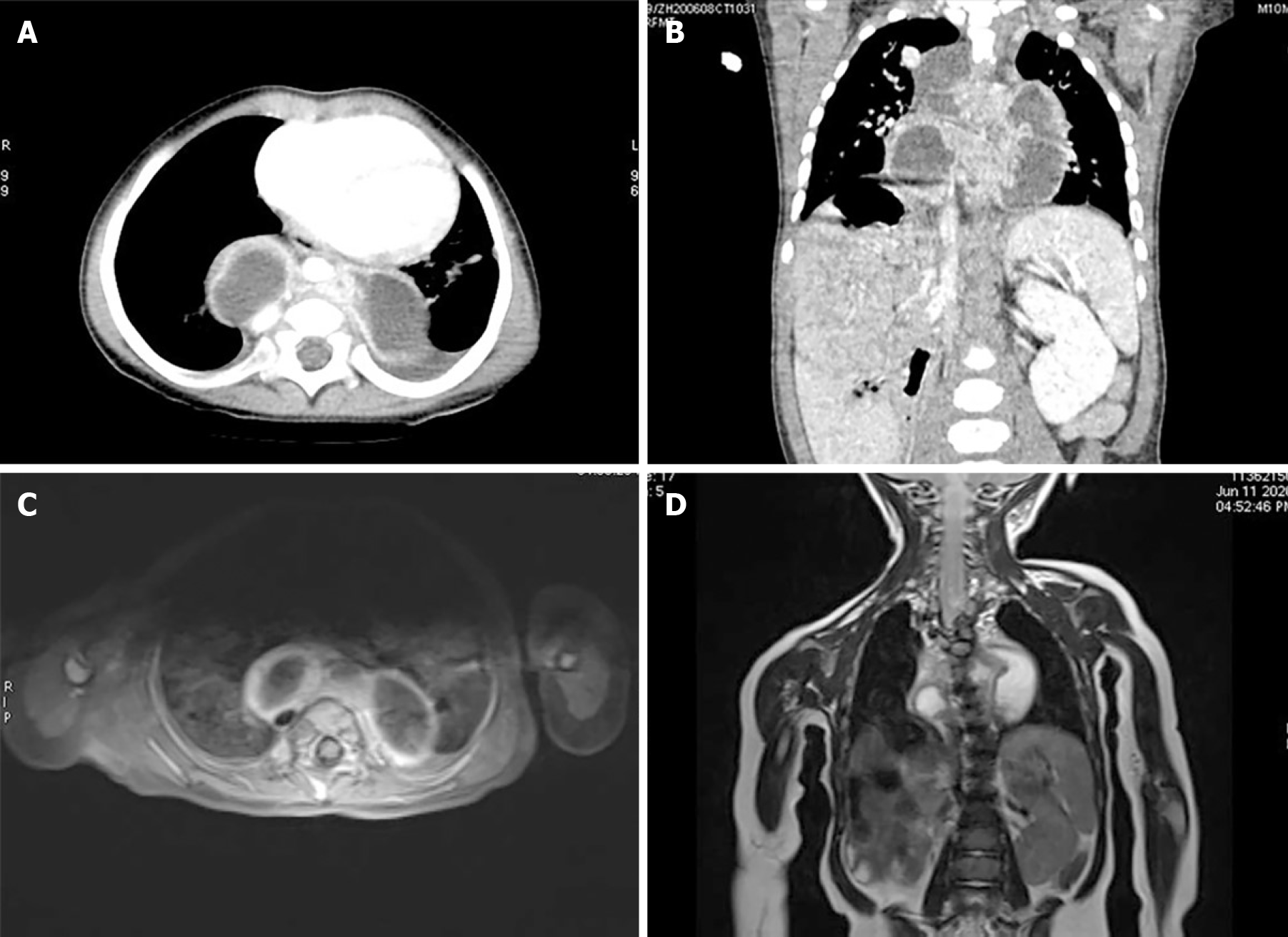
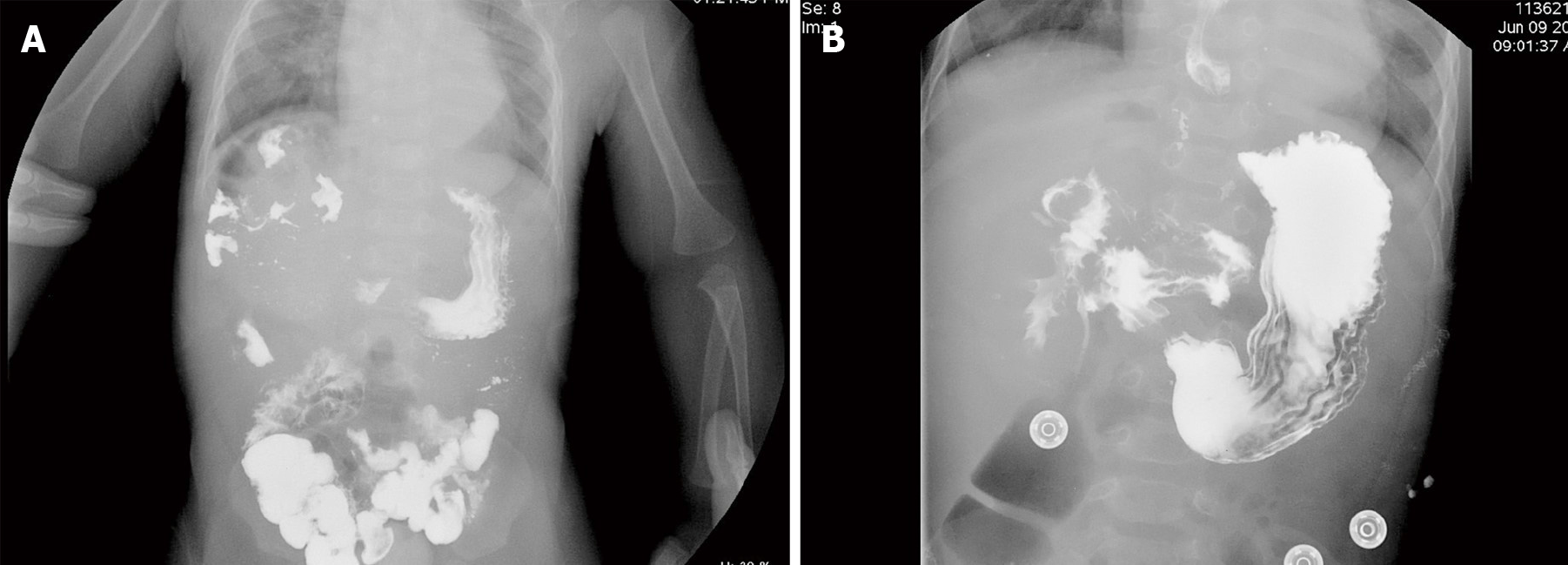
Ultrasound indicated that the superior mesenteric vein and superior mesenteric artery were in an abnormal position. In addition, there was intestine tube-like tissue between the liver and kidney and posterosuperior to the right liver lobe, which extended upward. An enhanced CT examination of the upper abdomen indicated the distention and elevation of the right diaphragm (bowel interposition) and an irregular liver, with the position shifted downward. An enhanced chest CT scan showed slight subsegmental consolidation and atelectasis in the lower lobe of the left lung, a small amount of bilateral pleural effusion, rib malformation, eventration of the right diaphragm (bowel interposition), and multiple thoracic deformities with posterior mediastinal cystic lesions (possible meningocele) (Figure 1A and B). In addition, there was local thickening and abnormal enhancement of the spinal meninges, indicating possible infection. The infant was then examined by enhanced magnetic resonance imaging (MRI) of the thoracic vertebrae, which revealed multiple cervicothoracic vertebral deformities, spina bifida, meningomyelocele towards the posterior mediastinum, and possible concurrent infection (Figure 1C and D). Upper gastroenterography indicated intestinal malrotation (Figure 2).
Tc-99m pertechnetate scintigraphy showed no obvious abnormality. A multidisciplinary team discussion was held among representatives of the general surgery, neurosurgery, and thoracic surgery departments. The neurosurgeons and thoracic surgeons suggested that the posterior mediastinal cyst might be myelomeningocele, and surgery should not be performed, instead observation and follow-up should be conducted. The general surgeons believed that gastroscopy and colonoscopy should be performed first in case of hematochezia, and if the cause of hematochezia was still unclear, laparoscopic abdominal examination should be performed. Gastroscopy and colonoscopy were performed later and revealed no abnormalities.
The final diagnosis of the present case was thoracoabdominal intestinal duplication.
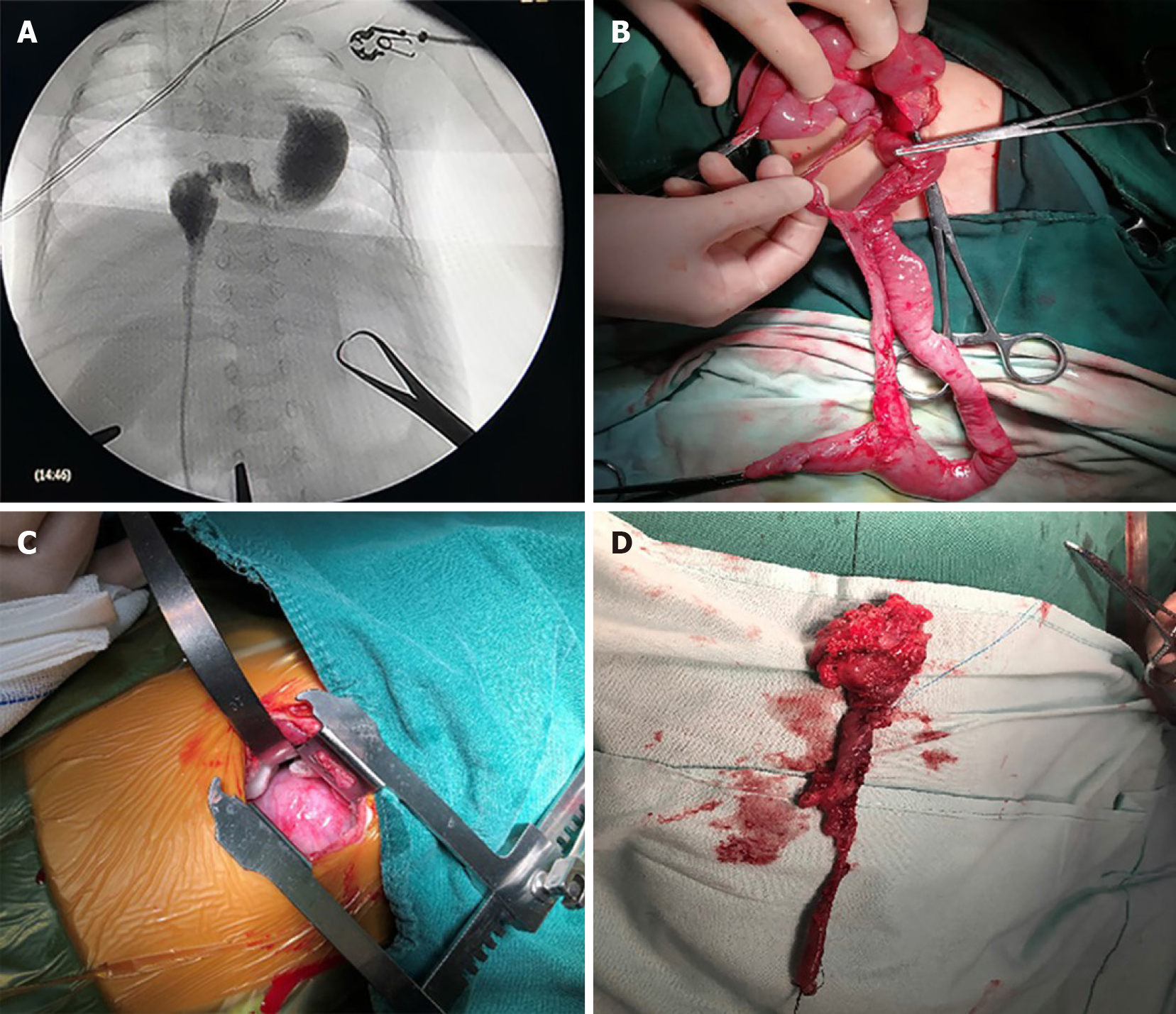
A laparoscopic abdominal examination was performed. During the operation, we found that the duodenum was to the right of the midline, and the cecum was in the right lower quadrant, but the colon did not fix to the hepatic flexure, predisposing to Ladd bands formation (Type 3B). In addition, tubular duplication of the intestine was found at the junction of the jejunum and the ileum, which shared the mesentery with the normal intestinal canal. The proximal end of the duplication extended upward behind the liver to the diaphragm. Therefore, the operation was intraoperatively converted to laparotomy. After the abdomen was opened, a long intestinal duplication was observed. The distal end of the duplication was communicating with the normal intestinal canal, while the proximal end extended toward the back of the liver. To deliver the contrast agent, a catheter was inserted upward (in the direction of diaphragm) into the duplicated intestine. After the contrast agent was injected, it could be observed that the intestinal tube passed through the diaphragm and extended upward to the posterior mediastinum, and crossed the midline right to left behind the oesophagus and aorta (Figure 3A). Approximately 30 cm of the duplicated intestine and parallel intestinal tube were excised, and end-to-end anastomosis was performed on the normal intestine between the proximal and distal end (Figure 3B). Thoracic surgeons were consulted during the operation. It was decided to remove the duplication in the posterior mediastinum by transthoracic resection. An incision was made on the lateral posterior side of the left chest. The lung was pushed in an anterosuperior direction, which revealed a large amount of intestinal tissue in the posterior mediastinum (Figure 3C). This case was diagnosed intraoperatively as thoracoabdominal intestinal duplication. The mediastinal pleura was opened upward along the intestinal tissue to the back of the thoracic aorta. It was observed that the intestinal tube extended horizontally to the right mediastinum below the tracheal bifurcation. The intestinal tube was excised. Along the intestinal tube towards the diaphragmatic surface, a part of the intestine crossed the midline from back of the aorta to the right mediastinum and then entered the abdominal cavity from the esophageal hiatus. The intestinal tissue was completely freed and removed from the esophageal hiatus. The esophageal hiatus was then sutured continuously at the site of the intestinal tube penetration. Approximately 20 cm of the thoracic intestine was excised (Figure 3D).
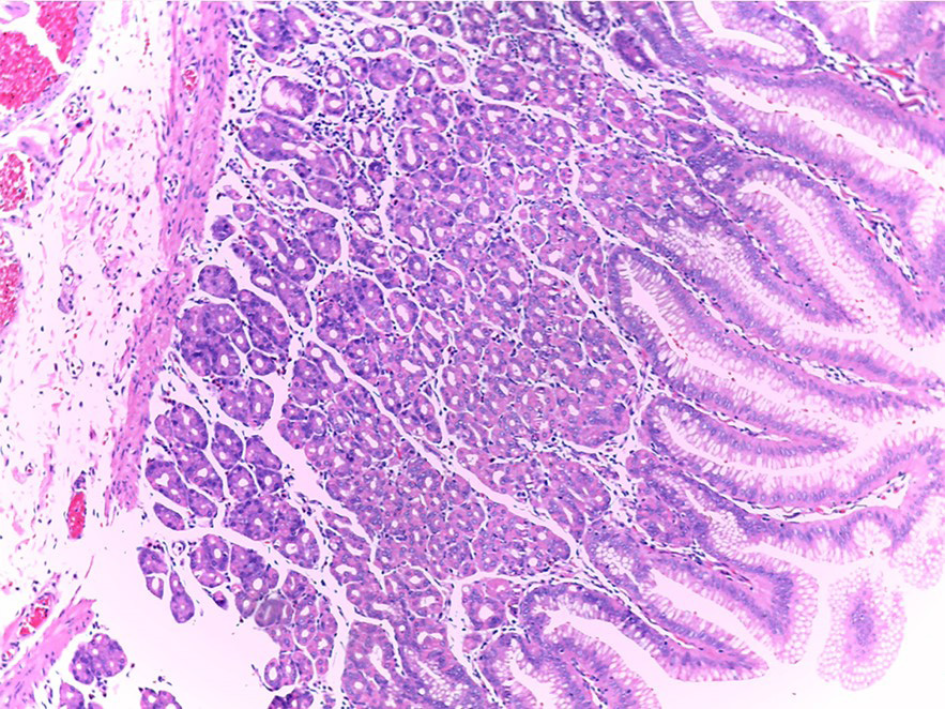
The infant recovered well and was discharged 1 wk after the surgery. The results of postoperative pathological examination confirmed that this case was indeed alimentary tract duplication and that part of the duplication contained gastric mucosa (Figure 4). Chest CT showed myelomeningocele while the posterior mediastinal cyst was significantly reduced during outpatient follow-up 3 mo after the surgery (Figure 5). After neurosurgery consultation, it was decided that regular follow-ups should be conducted for the meningocele.
Alimentary tract duplication is a rare congenital malformation that may occur anywhere in the alimentary tract. The incidence of alimentary tract duplication is approximately 1/4500 and is slightly higher in men[2,3]. Thoracoabdominal intestinal duplication is a rare type of alimentary tract duplication. It originates in the abdomen, passes through the diaphragm, and reaches the thoracic cavity. The duplicated intestinal tube is usually longer than normal, and larger tubes often occur in the right posterior mediastinum. Approximately 60% of the intestinal duplications communicate with the intestinal canal in the abdominal cavity, usually connecting with the normal duodenum or jejunum. In our patient, the duplication connected to the abdominal intestine and became a blind end structure in the thoracic cavity.
The clinical symptoms and signs are related to age, the range of extension and the type of duplication in the chest or abdomen, the presence/absence of communication with intestinal lumen, and the presence/absence of ectopic gastric mucosa. Approximately 80% of the children with thoracoabdominal intestinal duplication experience onset within 1 year of age[4]. Newborns usually have respiratory symptoms such as dyspnea. Older children often show symptoms such as chest and abdominal pain, gastrointestinal bleeding, and anemia. Although the existing auxiliary examinations (such as X-ray, B-ultrasound, CT, and MRI) can provide important clues regarding the location and size of certain lesions and their relationship with the adjacent anatomical structures, a definitive diagnosis should depend on the pathological results. Since some intestinal duplications contain ectopic gastric mucosa, pancreatic tissue, and even respiratory tract mucosa, diagnosis can be improved with Tc-99m pertechnetate scintigraphy. However, this test still has a notable rate of false positive and false negative results. In some cases, prenatal ultrasound can be used to assist diagnosis[5,6]. Clinically, it is difficult to distinguish intestinal duplication from mesenteric cyst and Meckel’s diverticulum when the symptoms are mainly acute intestinal obstruction or bleeding. Duplications in the mediastinum often present as respiratory symptoms. Such duplication usually occurs in the right mediastinum and is often accompanied by spinal deformities such as spina bifida, hemivertebra, and myelomeningocele[7]. It often needs to be differentiated from mediastinal tumors, mediastinal bronchogenic cysts, lymphangiomas, pericardial cysts, and cystic teratomas, which are generally not accompanied by spinal deformities.
The infant reported in the present study had melena as the main symptom, and there were no clinical manifestations of intestinal obstruction, such as abdominal pain and vomiting. Upper gastrointestinal angiography conducted at our hospital and other hospitals indicated the possibility of intestinal malrotation. In addition, to clarify the cause of the blood in the stool, gastroscopy and colonoscopy were performed to rule out esophageal varices, ulcers, inflammatory bowel disease, intussusception, polyps, and other causes of gastrointestinal bleeding. Taking the existing clinical data into account, we considered a high possibility of intestinal malrotation. Therefore, a laparoscopic abdominal examination was performed. During the operation, intestinal duplication that passed through the diaphragm into the mediastinum was discovered. Intraoperative angiography determined that the deformity was thoracoabdominal duplication. A retrospective analysis of the clinical characteristics of this case found the following factors that led to the missed diagnosis: (1) In addition to black stool, the infant also presented the clinical manifestation of cyanosis when crying. Therefore, there should have been high suspicion of concurrent chest diseases, and relevant chest examinations should have been performed; (2) The ultrasound performed at our hospital indicated the presence of intestine tube-like tissue between the liver and kidney and posterosuperior to the right liver lobe, which extended upward. Subsequent CT and MRI examinations of the chest showed that the spinal cord and spinal meninges bulged towards the posterior mediastinum, but the possibility of enterogenous cysts was ignored in favor of intrathoracic cysts. In fact, this infant was eventually diagnosed with both intestinal duplication and meningocele in the thoracic cavity; and (3) The results of preoperative Tc-99m pertechnetate scintigraphy were negative. However, the postoperative pathological results confirmed the local presence of gastric mucosa in the intestine, indicating that the imaging result was a false negative.
In the case of concurrent deformities with thoracic duplication, children generally have a narrowed thoracic cavity, and thus, cysts can easily exert pressure on the respiratory system. Affected children may experience chest pain, chest tightness, and cough. In addition, children may develop symptoms such as fever and cough due to cyst rupture or self-infection. In severe cases, dyspnea and cyanosis occur even when children are calm. When symptoms are mild, children develop cyanosis only when they are crying or engaging in light activities. Thoracic duplication is often accompanied by spinal deformities (such as spina bifida, hemivertebrae, or myelomeningocele), while intrathoracic meningocele can also be complicated by spinal deformities[8]. The infant reported here had concurrent spinal deformity. He had both enterogenous cysts and meningocele in the thoracic cavity, which added difficulty to the preoperative diagnosis. Zhang et al[8] suggested that attention should be paid to intestinal duplication in the abdominal cavity when mediastinal enterogenous cysts are noted, and vice versa. Khanna et al[9] also proposed that when a case of intestinal duplication is diagnosed, attention should be paid to whether there are concurrent duplications of other parts. Nazem et al[10] mentioned that there could be concurrent esophageal duplication cysts and small intestine duplication.
Surgical resection is the only treatment for thoracoabdominal duplication. Surgery should be performed as soon as possible to avoid complications such as infection, compression of surrounding tissues and organs, cyst bleeding or rupture, and cancer. Moreover, treatment of thoracoabdominal duplication is often more difficult than the treatment of isolated thoracic duplication or abdominal duplication. The specific surgical method, open or endoscopic, is selected based on the location and shape of the lesion and the experience of the surgeon. The postoperative prognosis is generally good, with few postoperative complications and a low recurrence rate. Khanna et al[9] reported that a neonate with total midgut duplication underwent staged surgery due to a poor general condition and long tubular duplication. The proximal cyst was excised in stage I. Postoperative reexamination revealed the presence of an enterogenous cyst in the mediastinum. In stage II, the mucosal lining of the duplicated bowel was stripped off. In stage III, the enterogenous cyst in the mediastinum was excised. However, unlike our case, the mediastinal cyst in this case was not connected with the abdominal duplication. Moralioglu et al[3] reported a case in which an enterogenous cyst in the right posterior mediastinum extended through the diaphragm and communicated with the alimentary tract duplication in the abdominal cavity. This case was similar to the one we reported here, and the lesion was eventually removed by combined thoracic-abdominal surgery. However, the lesion passed through the diaphragm and extended upward to the posterior mediastinum, and crossed the midline right to left in our case. Therefore, thoracic incision was made on the lateral posterior side of the left chest. It is worth noting that our case was complicated with meningocele. However, there were no neurological symptoms, and neurosurgery suggested regular follow-ups should be conducted. Moralioglu et al[3] suggested that cases with spinal involvement can be treated by combined surgery by an experienced neurosurgical team.
In summary, thoracoabdominal duplication is a rare disease with diverse clinical manifestations. When a child is admitted to the hospital with acute abdominal disease or gastrointestinal bleeding, clinicians focus mainly on the abdominal symptoms, and the thoracic clinical manifestations are often neglected. Therefore, if a child with suspected abdominal intestinal duplication has concurrent respiratory symptoms, the possibility of thoracoabdominal duplication should be considered, and enhanced chest-related examinations should be performed. Resection of the thoracoabdominal duplications in one-stage surgery appears to be an appropriate and safe treatment option.
The authors appreciate Dr. Ma YY for providing the pathological data.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Moralioglu S S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Sharma S, Yadav AK, Mandal AK, Zaheer S, Yadav DK, Samie A. Enteric Duplication Cysts in Children: A Clinicopathological Dilemma. J Clin Diagn Res. 2015;9:EC08-EC11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Okur MH, Arslan MS, Arslan S, Aydogdu B, Türkçü G, Goya C, Uygun I, Cigdem MK, Önen A, Otcu S. Gastrointestinal tract duplications in children. Eur Rev Med Pharmacol Sci. 2014;18:1507-1512. [PubMed] |
| 3. | Moralioglu S, Pektas OZ, Celayir AC, Bosnali O, Kaygusuz E. Thoracoabdominal duplication symptomatic on both sides: a case report. West Indian Med J. 2014;63:192-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Pokorny WJ, Goldstein IR. Enteric thoracoabdominal duplications in children. J Thorac Cardiovasc Surg. 1984;87:821-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Jan IA, Al Nuaimi A, Al Hamoudi B, Al Naqbi K, Bilal M. Distal Esophageal Duplication Cyst with Gastro-Esophageal Reflux Disease: A Rare Association and a Management Challenge. J Coll Physicians Surg Pak. 2016;26:148-150. [PubMed] |
| 6. | Cuch B, Nachulewicz P, Wieczorek AP, Wozniak M, Pac-Kozuchowska E. Esophageal Duplication Cyst Treated Thoracoscopically During the Neonatal Period: Clinical Case Report. Medicine (Baltimore). 2015;94:e2270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Patiño Mayer J, Bettolli M. Alimentary tract duplications in newborns and children: diagnostic aspects and the role of laparoscopic treatment. World J Gastroenterol. 2014;20:14263-14271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 8. | Zhang KR, Jia HM, Pan EY, Wang LY. Diagnosis and treatment of mediastinal enterogenous cysts in children. Chin Med Sci J. 2006;21:201-203. [PubMed] |
| 9. | Khanna V, Khanna K, Srinivas M. Total midgut duplication: a ticking time bomb. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Nazem M, Amouee AB, Eidy M, Khan IA, Javed HA. Duplication of cervical oesophagus: a case report and review of literatures. Afr J Paediatr Surg. 2010;7:203-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |