Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7231
Peer-review started: April 8, 2021
First decision: May 11, 2021
Revised: May 24, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 26, 2021
Processing time: 137 Days and 10.7 Hours
Splenic hamartoma (SH) is a rare, benign vascular proliferation that is often found incidentally. It may be misdiagnosed as a splenic aneurysm or splenic malignancy.
A 21-year-old male patient was admitted to our hospital with a complaint of an incidentally discovered asymptomatic splenic space-occupying lesion for 2 wk. Abdominal computed tomography (CT) scan showed a circular low-density shadow in the hilum of the spleen. Contrast-enhanced CT revealed an aneurysm located in the hilum of the spleen before operation. Laparoscopic splenectomy was performed and postoperative pathology revealed the presence of SH.
Imaging studies are insufficient for the differential diagnosis of SH from other diseases, and laparoscopic splenectomy is a less invasive procedure and useful for the diagnostic purpose as well.
Core Tip: Splenic hamartoma (SH) is a rare, benign vascular proliferation that is found incidentally and often misdiagnosed. We present a case of incidentally discovered asymptomatic splenic space-occupying lesion, which was misdiagnosed as a splenic aneurysm. Laparoscopic splenectomy was performed and postoperative pathology revealed the presence of SH. The findings of this case study emphasize that imaging studies are insufficient for the differential diagnosis of SH from other diseases, and laparoscopic splenectomy is a less invasive procedure that is useful for diagnostic purposes as well.
- Citation: Cao XF, Yang LP, Fan SS, Wei Q, Lin XT, Zhang XY, Kong LQ. Incidentally discovered asymptomatic splenic hamartoma misdiagnosed as an aneurysm: A case report. World J Clin Cases 2021; 9(24): 7231-7236
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7231.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7231
Splenic hamartoma (SH) is a very rare benign vascular lesion[1], with an incidence of three cases in 200000 splenectomies and an incidence of 0.024% to 0.13%[2]. It was first described in 1861 by Rokitansky[3], and was originally called splenoma, spleen within a spleen, fibrotic nodules, hemangioma, hyperplastic nodules, and tumor-like congenital malformations[4]. Most patients with SH are asymptomatic, with no specific imaging findings, making it difficult to distinguish from other benign and malignant splenic diseases.
Herein, we report a 21-year-old male patient with an asymptomatic SH, which was misdiagnosed as an aneurysm.
A 21-year-old male was admitted to our hospital with abnormal nodules in the spleen on abdominal ultrasonography during a routine health check-up.
No remarkable medical history and weight loss were reported.
The patient had a free previous medical history.
The patient had no related family and psychosocial history.
On physical examination, there was no palpable mass in the abdomen.
Laboratory tests did not show any significant abnormalities.
Abdominal computed tomography (CT) showed a round low-density shadow at the hilum of the spleen with a clear boundary, measuring 3.5 cm × 3.6 cm × 3.7 cm. Contrast-enhanced CT revealed that in the arterial phase, the lesion presented heterogeneous enhancement, while in venous phase and delayed phase the enhancement was slightly higher than the density of the spleen, similar to those of aortic three-phase enhancement (Figure 1A-E).
A diagnosis of a benign lesion of the spleen was made and a splenic aneurysm was considered initially.
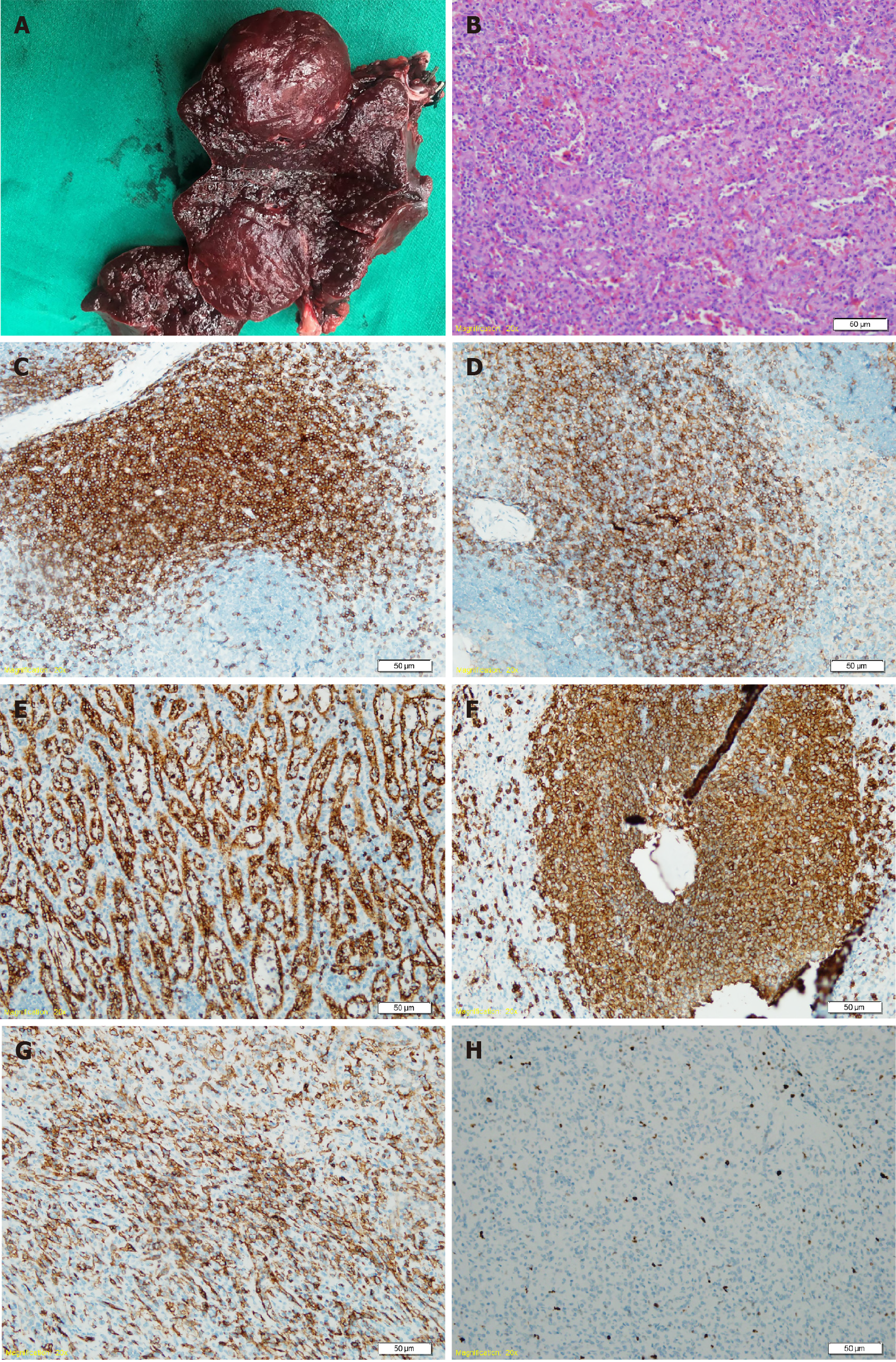
Morphopathological analyses of the spleen revealed that the lesion was soft, red and gray, measuring 3.0 cm, adjacent to the hilum of spleen (Figure 2A). Microscopic examination showed that the tumor had no definite capsule, which was mainly formed by the disordered arrangement of sinusoid lacunae with fissures. Similar to the red pulp with a disordered structure, dilated sinuses, endothelial cell proliferation and obesity, connective tissue, lymphocytes, plasma cells and granulocytes could be seen between the fissures, while white pulp and trabeculae were not seen. Immunohistochemical staining showed that the peripheral lymphoid follicles were positive for cluster of differentiation 20 (CD20), and the splenosomes were positive for CD3, CD4, and CD8. The follicular dendritic cells were positive for CD21, and the endothelial cells in the tuberous sinus expressed CD8 and CD34, and partially expressed CD31 and CD68, and Ki-67 was about 2% (Figure 2B-H). The final diagnosis was isolated SH.
Due to the risk of spontaneous rupture in the case of misdiagnosed splenic aneurysm, the patient underwent laparoscopic splenectomy. The operation went smoothly. It was confirmed that the lesion originated from the spleen parenchyma near the splenic hilum rather than the splenic artery; thus, the diagnosis of splenic aneurysm was excluded.
The patient recovered uneventfully and was discharged on postoperative day 5 with adequate oral intake, and normal vital signs.
SH is a rare benign tumor that occurs at any age, with a mean age of 27 years for men and 37 years for women, and has equal incidence in males and females[5,6]. The tumor is usually detected incidentally as a singular lesion with a diameter ranging from a few millimeters up to 20 cm[7], but women seem to have larger lesions, probably due to hormonal influence on tumor growth[8]. Most patients with SH are asymptomatic while symptomatic patients account for only 15% of cases[9]. Signs and symptoms can be associated with the size of lesion. Common clinical manifestations include pain, palpable mass or spontaneous rupture[7,9,10]. Thrombocytopenia, anemia, pancy
SH should be differentiated from other vascular tumors of the spleen including hemangioma, lymphangioma, hemangioendothelioma, and angiosarcoma. Solid mass-forming lesions of the spleen such as lymphoma, metastatic disease, inflammatory pseudotumor and sarcoidosis are also included in the differential diagnosis[2,7,9,14-16]. Although imaging findings of SH are nonspecific, there are useful clues, such as on CT, SH appears as an isodense or hypodense solid mass, and heterogeneous contrast enhancement relative to adjacent normal spleen parenchyma was present in the arterial phase, venous phase or delayed phase[17]. On magnetic resonance imaging (MRI), SH appears isointense in the T1-weighted image, but heterogeneously hyperintense in the T2-weighted image compared to normal parenchyma[18].
Fine needle aspiration biopsy may be useful in establishing a definitive diagnosis preoperatively[4]. However, this technique is associated with some serious complications including bleeding and abdominal seeding; thus, it has been only performed in a limited number of cases[4,11]. Pathologically, SH shows unique histological features; the key immunohistochemical feature is CD8 positivity of the lining cells of the vascular channels. The cells are also positive for CD31, factor VIII–related antigen, and vimentin[1,11], all of which are helpful in differentiating SH from capillary heman
When an SH is suspected and malignancy cannot be ruled out, splenectomy should be considered. Laparoscopic splenectomy is the standard procedure for most of benign hematologic diseases and solid splenic tumors, and there is no exception for SH[19]. Additionally, partial splenectomy is an alternative procedure according to the age of the patient, size of the mass and findings of preoperative imaging studies[3,20].
The present case is the first SH that we encountered in clinical practice, due to the lack of experience and the non-specific features of the lesion, we misdiagnosed it as a splenic aneurysm initially. Fortunately, the subsequent operation and postoperative pathology corrected the diagnosis.
SH is a rare benign vascular proliferation characterized by CD8-positive immu
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gurala D, Matowicka-Karna J S-Editor: Gao CC L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Cheng N, Chen J, Pan Y, Jiang Y, Zhou J, Shao C. Splenic hamartoma with bizarre stromal cells: a case report and literature review. Diagn Pathol. 2018;13:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 2. | Lam KY, Yip KH, Peh WC. Splenic vascular lesions: unusual features and a review of the literature. Aust N Z J Surg. 1999;69:422-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Basso SM, Sulfaro S, Marzano B, Fanti G, Chiara GB, Lumachi F. Incidentally discovered asymptomatic splenic hamartoma with rapidly expansive growth: a case report. In Vivo. 2012;26:1049-1052. [PubMed] |
| 4. | Lee H, Maeda K. Hamartoma of the spleen. Arch Pathol Lab Med. 2009;133:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Dolcet C, Kornprat P, Lindenmann J, Beham-Schmid C, Mischinger HJ. Incidental finding of a splenic hamartoma with tumour-like extramedullary erythropoiesis. Wien Med Wochenschr. 2011;161:394-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Gonzalez Urquijo M, Rodarte-Shade M, Rangel-Rangel R, Castillo-Meraz JA, Rodriguez-Tejeda JR, Gil-Galindo G. A giant splenic hamartoma associated with hematologic disorders: A case report. Ann Med Surg (Lond). 2018;36:199-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Eker T, Kocaay AF, Sevim Y, Çakmak A. Splenic hamartoma is a rare cause of abdominal pain: Case report and literature review. Turk J Surg. 2017;33:294-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Komo T, Hihara J, Kanou M, Kohashi T, Ohmori I, Yoshimitsu M, Ikeda T, Nakashima A, Miguchi M, Yamakita I, Mukaida H, Hirabayashi N, Kaneko M. Splenic hamartoma associated with thrombocytopenia: A case report. Int J Surg Case Rep. 2017;39:172-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Sim J, Ahn HI, Han H, Jun YJ, Rehman A, Jang SM, Jang K, Paik SS. Splenic hamartoma: A case report and review of the literature. World J Clin Cases. 2013;1:217-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 10. | Bartels A, Brock C, Nelson C, Denney J, Barnes S. Spontaneous rupture of a splenic hamartoma. Am Surg. 2013;79:E331-E332. [PubMed] |
| 11. | Wang RT, Xu XS, Hou HL, Qu K, Bai JG. Symptomatic multinodular splenic hamartoma preoperatively suspected as metastatic tumor: a case report. World J Gastroenterol. 2014;20:10637-10641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Colović N, Cemerikić V, Colović R, Zogović S, Stojković M. [Hamartoma of the spleen]. Srp Arh Celok Lek. 2000;128:331-334. [PubMed] |
| 13. | Serra F, Sorrentino L, Cabry F, Biondini D, Ceccarelli PL, Campanelli M, Gelmini R. First case of laparoscopic partial splenectomy in a child with hamartoma: Case report and review of the literature. Int J Surg Case Rep. 2018;53:140-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Tajima S, Koda K. A case of cord capillary hemangioma of the spleen: a recently proven true neoplasm. Pathol Int. 2015;65:254-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Kwon H. Inflammatory pseudotumor-like follicular dendritic cell tumor of the spleen. Turk J Gastroenterol. 2018;29:128-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Mikamori M, Tanemura M, Furukawa K, Saito T, Ohtsuka M, Suzuki Y, Imasato M, Kishi K, Akamatsu H. Laparoscopic splenectomy for isolated splenic sarcoidosis: A case report. Int J Surg Case Rep. 2019;60:79-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Dong A, Wang Y, Lu J, Zuo C. Enhanced CT and FDG PET/CT findings of splenic hamartoma. Clin Nucl Med. 2014;39:968-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Van de Wiele C, Verstraete K, Bourgeois S, Maes A. Negative 18F-FDG PET and positive CT and MRI findings in multifocal splenic hamartoma. Hell J Nucl Med. 2017;20:182-183. [PubMed] |
| 19. | Piccolo G, Cavallaro A, Antonacci V, Nicosia A, Iozzia C, Cavallaro V, Minutolo V. Laparoscopic splenectomy for splenic hamartoma in elderly patien Case report and review of the literature. Ann Ital Chir. 2012;2012. [PubMed] |
| 20. | Uranues S, Grossman D, Ludwig L, Bergamaschi R. Laparoscopic partial splenectomy. Surg Endosc. 2007;21:57-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |