Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7224
Peer-review started: April 6, 2021
First decision: April 13, 2021
Revised: April 14, 2021
Accepted: July 14, 2021
Article in press: July 14, 2021
Published online: August 26, 2021
Processing time: 140 Days and 0.6 Hours
Chronic pancreatitis occasionally requires surgical treatment that can be performed with various techniques. Often, this type of surgery presents with postoperative complications. We report a case of a successful retrograde pancreatojejunostomy for chronic pancreatitis and infected pancreatic cysts.
A 62-year-old male with a 10-year history of chronic pancreatitis presented with epigastric pain for one week and a 20 kg weight loss over one year. Computed tomography showed stones in the pancreas (mainly the head), expansion of the main pancreatic duct, and thinning of the pancreatic parenchyma. Magnetic resonance imaging showed infected pancreatic cysts connected to the stomach with a fistula from the splenic hilum to the caudal portion of the liver’s lateral segment. An endoscopic retrograde pancreatography was performed; the guide wires could not pass through the stones in the pancreas and therefore, drainage of the main pancreatic duct was not achieved. Next, a distal pancreatomy and splenectomy were performed; however, the pancreatic juice in the remaining parenchyma was blocked by the stones. Hence, we performed a retrograde pancreatojejunostomy and Roux-en-Y anastomosis. The patient had no postoperative complications and was discharged from the hospital on postoperative day 14.
A distal pancreatomy, retrograde pancreatojejunostomy, and Roux-en-Y anastomosis could be an effective surgical procedure for intractable chronic pancreatitis.
Core Tip: Surgical treatment for chronic pancreatitis often presents with postoperative complications. We present the case of a successful retrograde pancreatojejunostomy for chronic pancreatitis and infected pancreatic cysts. This surgical procedure might be a valid option for surgeons faced with similar cases.
- Citation: Kimura K, Adachi E, Toyohara A, Omori S, Ezaki K, Ihara R, Higashi T, Ohgaki K, Ito S, Maehara SI, Nakamura T, Maehara Y. Successful outcome of retrograde pancreatojejunostomy for chronic pancreatitis and infected pancreatic cysts: A case report. World J Clin Cases 2021; 9(24): 7224-7230
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7224.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7224
Chronic pancreatitis is caused by alcoholic or inheritable factors, and the basic treatment is medication[1]. Currently, treatment methods for chronic pancreatitis focus on the management of pain, complications (i.e., duodenal, biliary, and pancreatic obstruction and pancreatic pseudocysts), and pancreatic insufficiency[2]. Endoscopic therapy is often performed on patients who are refractory to medication, and the development of endoscopic retrograde cholangiopancreatography and endoscopic ultrasound have obtained satisfactory results[3].
On the other hand, surgery is occasionally considered for the treatment of chronic pancreatitis. Surgery is indicated in cases in which endoscopic treatments fail and in cases with contenious abdominal pain[4]. Various surgical procedures, in addition to pancreatoduodenectomy or distal pancreatomy, have been developed but are not always facile and often present with postoperative complications[5]. In particular, cases with an infected pancreatic pseudocyst are difficult due to the risk of severe adhesion and hemorrhage.
Herein, we present a review of the literature and a novel case of chronic pancreatitis with pancreatic stones in the pancreas head and an infected pancreatic pseudocyst in the pancreas tail. A good outcome was achieved after a distal pancreatomy, splene
A 62-year-old male presented with exacerbated epigastric pain for one week and a 20 kg weight loss over one year.
He had an internal pancreatic duct stent insertion 10 years ago.
He had no medical follow-up for the past 10 years and no other history of illness.
He was a heavy drinker until 10 years ago. He would drink shochu 1000 mL daily.
The clinical examination revealed tenderness in his epigastric region. His general condition was otherwise good.
Laboratory examinations findings are showed in Table 1.
| Factor | Value | Reference range | Unit |
| White blood cell | 10200 | 3500-8400 | /μL |
| Hemoglobin | 11.1 | 11.3-15.2 | g/dL |
| Platelet count | 600000 | 158000-348000 | /μL |
| Neutrophils | 81.60% | 40-70 | % |
| Albumin | 26 | 4.0-5.0 | g/dL |
| Aspartate aminotransferase | 36 | 13-33 | U/L |
| Alanine aminotransferase | 29 | 6-30 | U/L |
| Alkaline phosphatase | 363 | 115-359 | U/L |
| Gamma-glutamyl transpeptidase | 58 | 10-47 | U/L |
| Amylase | 30 | 44-132 | U/L |
| Lipase | 14 | 13-55 | U/L |
| C-reactive protein | 12.32 | < 0.2 | mg/dL |
| Hemoglobin A1c | 6.3 | 4.9-6.0 | % |
| Carcinoembryonic antigen | 3.7 | < 5.0 | ng/mL |
| Colorectal carcinoma antigen 199 | 2.6 | < 37.0 | U/mL |
| Alpha fetoprotein | 1.7 | < 10.0 | ng/mL |
| Protein induced by vitamin K absence or antronist-2 | 369.71 | < 40.0 | mAU/mL |
| pancreatic cancer-associated antigen-2 | < 25 | < 150 | U/mL |
| SPan-1 | < 10 | < 30 | U/mL |
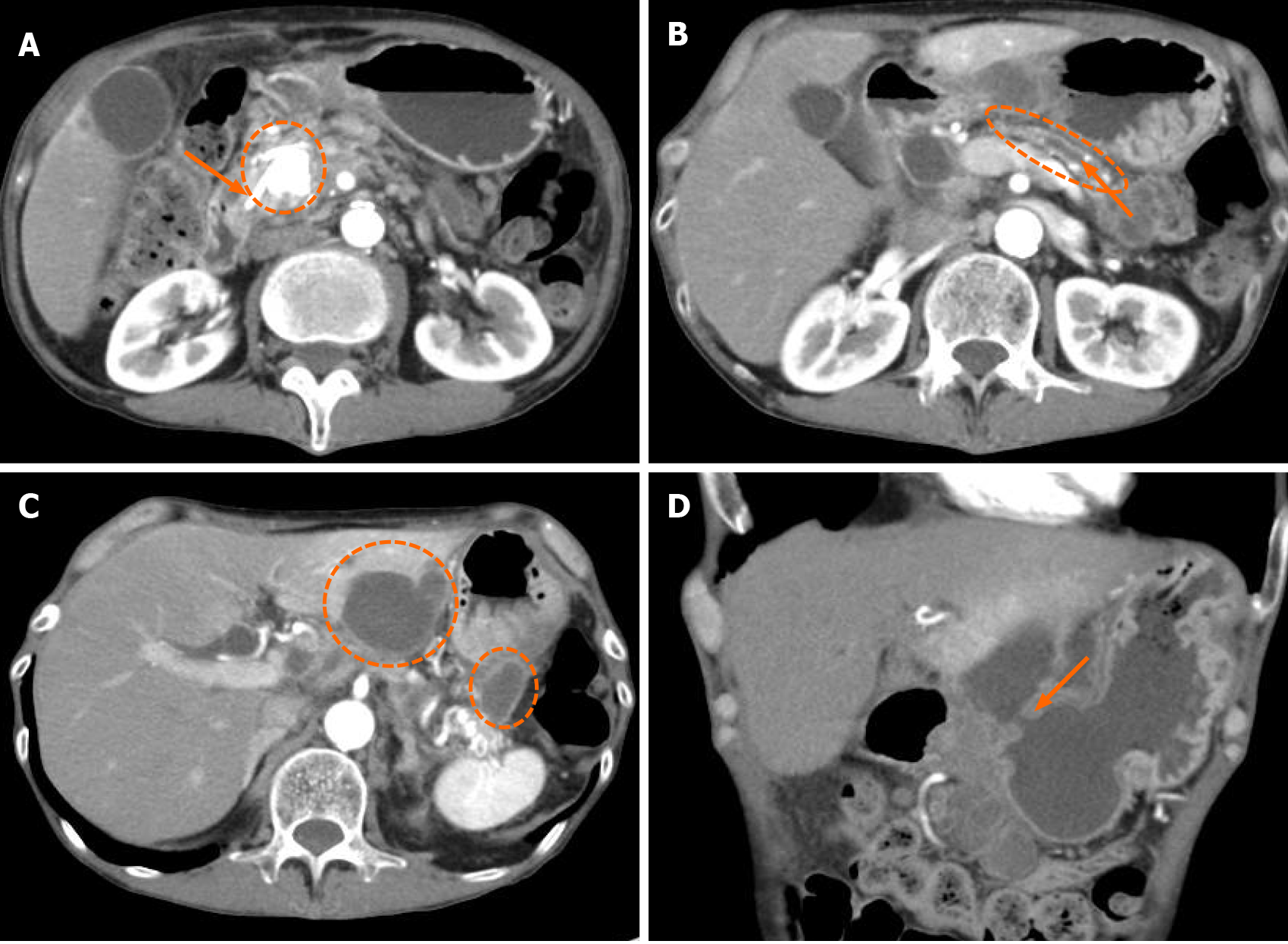
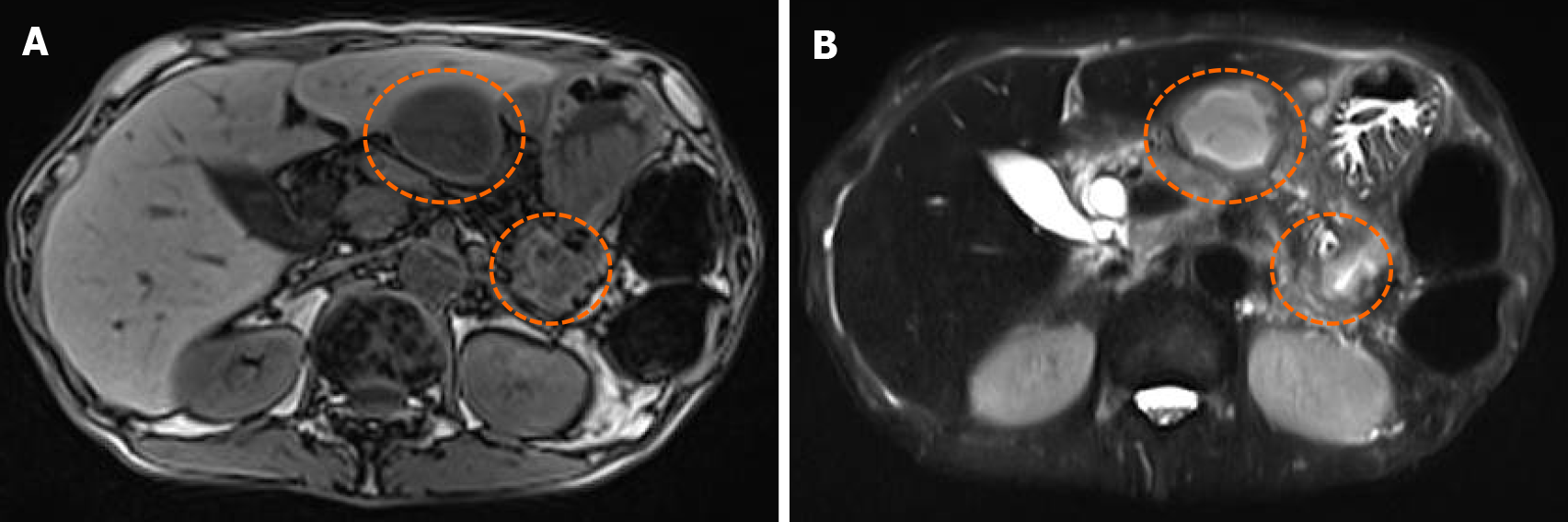
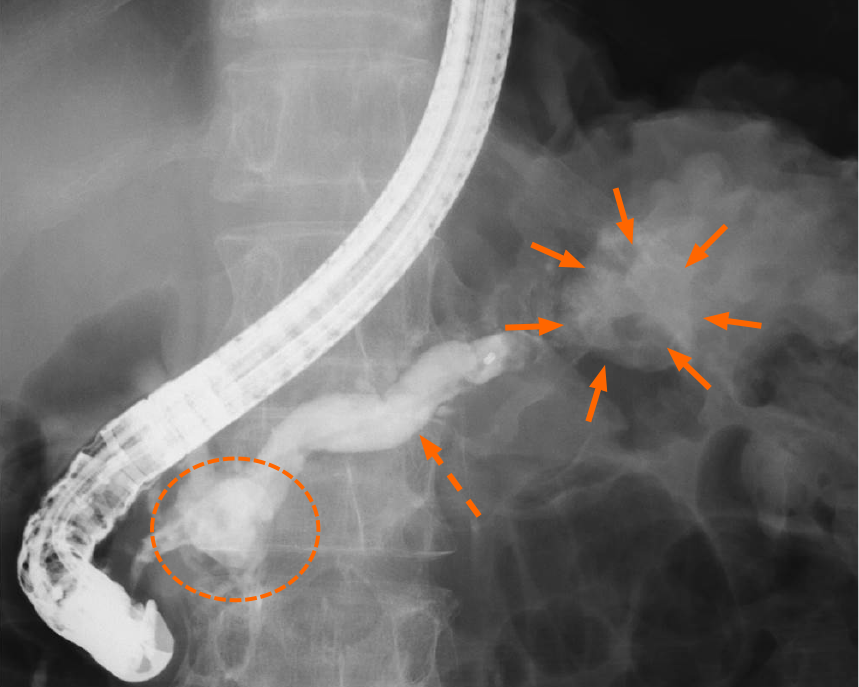
Computed tomography (CT) showed a stent in the pancreatic duct inserted 10 years ago (Figure 1A), multiple stones with various large and small sizes in the whole pancreas, but mainly in the pancreas head (Figure 1A), expansion of main pancreatic duct (Figure 1B), thinning of the pancreatic parenchyma (Figure 1B), and pancreatic cysts in the pancreas tail (Figure 1C). Moreover, a large high density cystic wall in the early phase was noted between the lateral segment of the liver and the pancreas; the cyst was connected to the stomach with a fistula (Figure 1D). Magnetic resonance cholangiopancreatography revealed multiple heterogeneous cysts diagnosed as infected cysts around the pancreas (Figure 2A). The cysts also demonstrated a high signal in diffusion weighted images (Figure 2B). Then, endoscopic retrograde pancrea
The patient was diagnosed with chronic pancreatitis and infected pancreatic cysts. The large stone in the pancreas head caused the pancreatic duct occlusion. Moreover, he had pseudocysts, infected cysts, and a fistula to the stomach from those cysts.
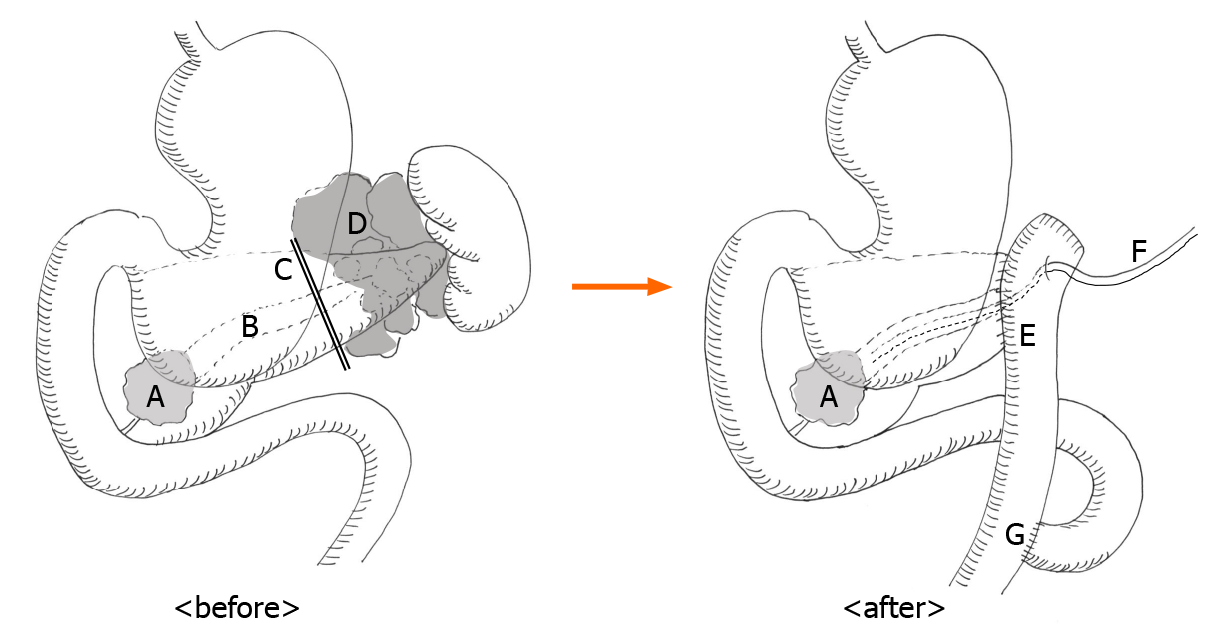
A whole pancreatectomy was one of the surgical options for this case because of the multiple stones and multiple pseudocysts; however, that option was seemed to be too invasive for the patient. Therefore, we chose to proceed with a distal pancreatomy, splenectomy and retrograde pancreatojejunostomy for drainage of the remaining pancreas.
During the procedure, we noted an extended moderate adhesion in the intraperitoneal space, and a severe adhesion in the gastric cecum. First, a distal pancreatomy and splenectomy were performed for the infected pancreatic cysts at the hilum of the spleen. Moreover, a partial gastrectomy of the fistula connected to the stomach from the infected pancreatic cyst was also performed. There was an aneurysm of the splenic artery and a severe adhesion with the infected pancreatic cysts between the pancreas tail and spleen. Therefore, it was impossible to preserve the splenic artery. Moreover, there was a large stone in the pancreas head, and pancreatic juice from the remaining pancreatic parenchyma was blocked by those stones. The jejunum was divided by an automatic anastomotic device at 10 cm from the Treitz' ligament, and we performed a retrograde pancreatojejunostomy to the amputation stump of the remaining pancreas by Modified Blumgart Mattress Suture Methods as previously described[6]. A 6 Fr external pancreatic stent was placed retrograde in the main pancreatic duct. The jejunum-loop was pulled up antecolic over the transverse mesocolon. Moreover, a Roux-en-Y anastomosis was performed by an end-to-side jejunojejunostomy at 20 cm from the pancreatojejunostomy anastomosis (Figure 4).
Histopathologic examination after surgery showed the pancreatic tissue with acinar depletion and prominent fibrosis, accompanied by mild to moderate chronic inflammatory infiltrates and dilated pancreatic ducts, filled with protein plugs, canaliculi and aggregates of microorganisms compatible with chronic pancreatitis. There was no malignant tissue. Lymph nodes attached to the specimen showed no malignant cells.
The patient experienced no postoperative complications, and was discharged from the hospital on postoperative day fourteen. His complaints of epigastric pain and anorexia were completely resolved after surgery, and he had no recurrence of symp
The initial treatment for chronic pancreatitis is medication. In patients with chronic pancreatitis that is resistant to medication, endoscopic treatments, such as an endoscopic retrograde cholangiopancreatographic stent placement and endoscopic ultrasound guided cyst drainage, must be performed[4]. Several reports have been shown that endoscopic treatments offer pain relief for patients with chronic pancreatitis, and they have been established as standard treatments for intractable chronic pancreatitis[7]. On the other hand, surgical procedures are sometimes required in cases resistant to medications and endoscopic therapy[5]. Also in our case, cannulation to the pancreatic duct by endoscopy was impracticable due to the pancreatic stone in the pancreas head. Furthermore, there was a risk of developing peritonitis or an intractable pancreatic fistula by diapedesis of an abscess from the infected cyst during endoscopic drainage treatment. Therefore, we proceeded with surgical treatment in this case.
Several surgical procedures for chronic pancreatitis have been reported. A longitudinal pancreatojejunostomy[8] and the Frey procedure[9] have shown satisfactory outcomes. These surgical procedures decrease abdominal pain by 50% to 100%. On the other hand, a surgical procedure would be too invasive for patients with benign disease considering the rate of postoperative complications reach 10%[8]. Moreover, irregular surgical procedures such as a pancreatojejunostomy and the Frey procedure tend to be complicated compared with conventional surgical procedures for pancreatic cancer such as a pancreatoduodenectomy and distal pancreatectomy. In this case, we performed a conventional distal pancreatomy and splenectomy, and added the conventional pancreatojejunostomy. Longitudinal pancreatojejunostomy could be the best treatment for this case. However, there are few cases which need surgical procedures for chronic pancreatitis in our institution. Inexperienced surgical procedures would cause many complications after surgery. Moreover, the patient strongly requested treatments in our institution. Then, we pondered how we can perform treatment by our usual surgical procedures and performed distal pancrea
Infected pancreatic pseudocysts have been reported as a complication of chronic pancreatitis[10]. Surgical treatment for chronic pancreatitis with infected pancreatic pseudocysts could be even more complicated by severe adhesions and inflammation, which more frequently leads to postoperative complications[11]. In our case, we could not preserve the spleen by the infected pancreatic pseudocysts between the hilus of the spleen and the dorsal of the stomach. Therefore, we had to perform a splenectomy. Moreover, the conventional distal pancreatomy and splenectomy did not enable the drainage of pancreatic juice to the duodenal papilla because of pancreatic stones in the pancreas head. We thought that a pancreatic fistula would certainly develop; therefore, we performed a retrograde pancreatojejunostomy. No postoperative complications developed, and a favorable outcome was obtained. Furthermore, an external pancreatic duct stent was inserted which enabled us to perform a pancreatography after surgery. Moreover, additional treatment such as the rendezvous technique[12] could be performed by guidewires passing through the stent after surgery.
We obtained a favorable outcome by performing conventional surgery of the pancreas. In the case of coexisting lesions in the pancreas head and tail, a distal pancreatectomy and splenectomy along with a retrograde pancreatojejunostomy with pancreatic duct stent insertion could be one option of surgical treatment for chronic pancreatitis.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Ge X, Luo XZ, Yang TY S-Editor: Wang JL L-Editor: A P-Editor: Ma YJ
| 1. | Olesen SS, Bouwense SA, Wilder-Smith OH, van Goor H, Drewes AM. Pregabalin reduces pain in patients with chronic pancreatitis in a randomized, controlled trial. Gastroenterology. 2011;141:536-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Issa Y, Bruno MJ, Bakker OJ, Besselink MG, Schepers NJ, van Santvoort HC, Gooszen HG, Boermeester MA. Treatment options for chronic pancreatitis. Nat Rev Gastroenterol Hepatol. 2014;11:556-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Díte P, Ruzicka M, Zboril V, Novotný I. A prospective, randomized trial comparing endoscopic and surgical therapy for chronic pancreatitis. Endoscopy. 2003;35:553-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 322] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 4. | Binmoeller KF, Jue P, Seifert H, Nam WC, Izbicki J, Soehendra N. Endoscopic pancreatic stent drainage in chronic pancreatitis and a dominant stricture: long-term results. Endoscopy. 1995;27:638-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 174] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Strate T, Taherpour Z, Bloechle C, Mann O, Bruhn JP, Schneider C, Kuechler T, Yekebas E, Izbicki JR. Long-term follow-up of a randomized trial comparing the beger and frey procedures for patients suffering from chronic pancreatitis. Ann Surg. 2005;241:591-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 133] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Hirono S, Kawai M, Okada KI, Miyazawa M, Kitahata Y, Hayami S, Ueno M, Yamaue H. Modified Blumgart Mattress Suture Versus Conventional Interrupted Suture in Pancreaticojejunostomy During Pancreaticoduodenectomy: Randomized Controlled Trial. Ann Surg. 2019;269:243-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 7. | Rösch T, Daniel S, Scholz M, Huibregtse K, Smits M, Schneider T, Ell C, Haber G, Riemann JF, Jakobs R, Hintze R, Adler A, Neuhaus H, Zavoral M, Zavada F, Schusdziarra V, Soehendra N; European Society of Gastrointestinal Endoscopy Research Group. Endoscopic treatment of chronic pancreatitis: a multicenter study of 1000 patients with long-term follow-up. Endoscopy. 2002;34:765-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 289] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 8. | Sakorafas GH, Zobolas B. Lateral pancreatojejunostomy in the surgical management of chronic pancreatitis. Current concepts and future perspectives. Dig Liver Dis. 2001;33:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2:701-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 267] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Zhang K, Li C, Gao C, Zhao C, Tang Q, Zhai J, Li Y. Efficacy and safety of acupuncture as an adjuvant treatment for acute pancreatitis: a protocol of systematic review and meta-analysis. BMJ Open. 2019;9:e029327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Bakshi S. Pancreatic abscess within hepato-gastric ligament: case report of an extremely rare disease. BMC Surg. 2020;20:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Krafft MR, Nasr JY. Anterograde Endoscopic Ultrasound-Guided Pancreatic Duct Drainage: A Technical Review. Dig Dis Sci. 2019;64:1770-1781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |