Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7163
Peer-review started: January 5, 2021
First decision: April 29, 2021
Revised: May 31, 2021
Accepted: July 9, 2021
Article in press: July 9, 2021
Published online: August 26, 2021
Processing time: 230 Days and 17.3 Hours
Morbihan syndrome is a rare illness, which presents with recurrent pitting edema on the upper two thirds of the face causing facial contour deformities, and Morbihan syndrome obstructing the pupillary axis with ptosis was seldomly reported.
A 59-year-old woman presented with a 15-year history of facial swelling that progressively invaded bilaterally from the inner canthus and eyelids outwards. Imaging examination indicated that the bilateral periorbital and the left temporal soft tissues had swelling without cranium invasion. Histopathological analysis showed a large amount of lymphocyte infiltration, and immunohistochemistry showed positive expression of CD68 in clear-cut granulomas and D2-40 in the lymphatic endothelium. Finally, the clinical diagnosis of Morbihan syndrome was confirmed.
Morbihan syndrome is an infrequent and refractory disease, which is characteristic with recurrent woody facial edema on the upper two thirds of the face. Solid facial edema is persistent and non-pitting, causing facial contour deformities and even vision field impairment. The diagnosis of Morbihan syndrome depends on clinical features, imaging information, and pathology. Blepharoplasty is optional to improve the visual field for these patients with severe pupillary axis obstruction.
Core Tip: Morbihan syndrome is a rare and refractory condition that is characterized by persistent edema on the upper two thirds of the face. We report a Morbihan syndrome patient with progressive disfiguring facial masses to cause pupillary axis obstruction. The features and prognosis of this disease are carefully described to help clinical physicians know this illness.
- Citation: Zhang L, Yan S, Pan L, Wu SF. Progressive disfiguring facial masses with pupillary axis obstruction from Morbihan syndrome: A case report. World J Clin Cases 2021; 9(24): 7163-7168
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7163.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7163
Morbihan syndrome, first reported in 1957 by Robert Degos, is a rare, refractory, but striking disease[1]. Typically, Morbihan syndrome presents with recurrent pitting edema on the upper two thirds of the face. It also gradually evolves into persistent solid, non-pitting, asymptomatic edema without pain to cause facial contour deformities and even visual field narrowing[2]. Lymphedema is the typical histopathological feature and sarcoidal granulomas can develop gradually over time without treatment[3]. Because of few related imaging reports, Morbihan syndrome is likely to be misdiagnosed, which delays the treatment to cause syndrome progression. We herein report a case of Morbihan syndrome with bilateral periorbital masses causing pupillary axis obstruction, and carefully analyze the clinical features, imaging information, histopathology, and treatment of this patient.
A 59-year-old Asian woman presented with multiple facial masses for 15 years and blurred vision of the left eye for 3 months.
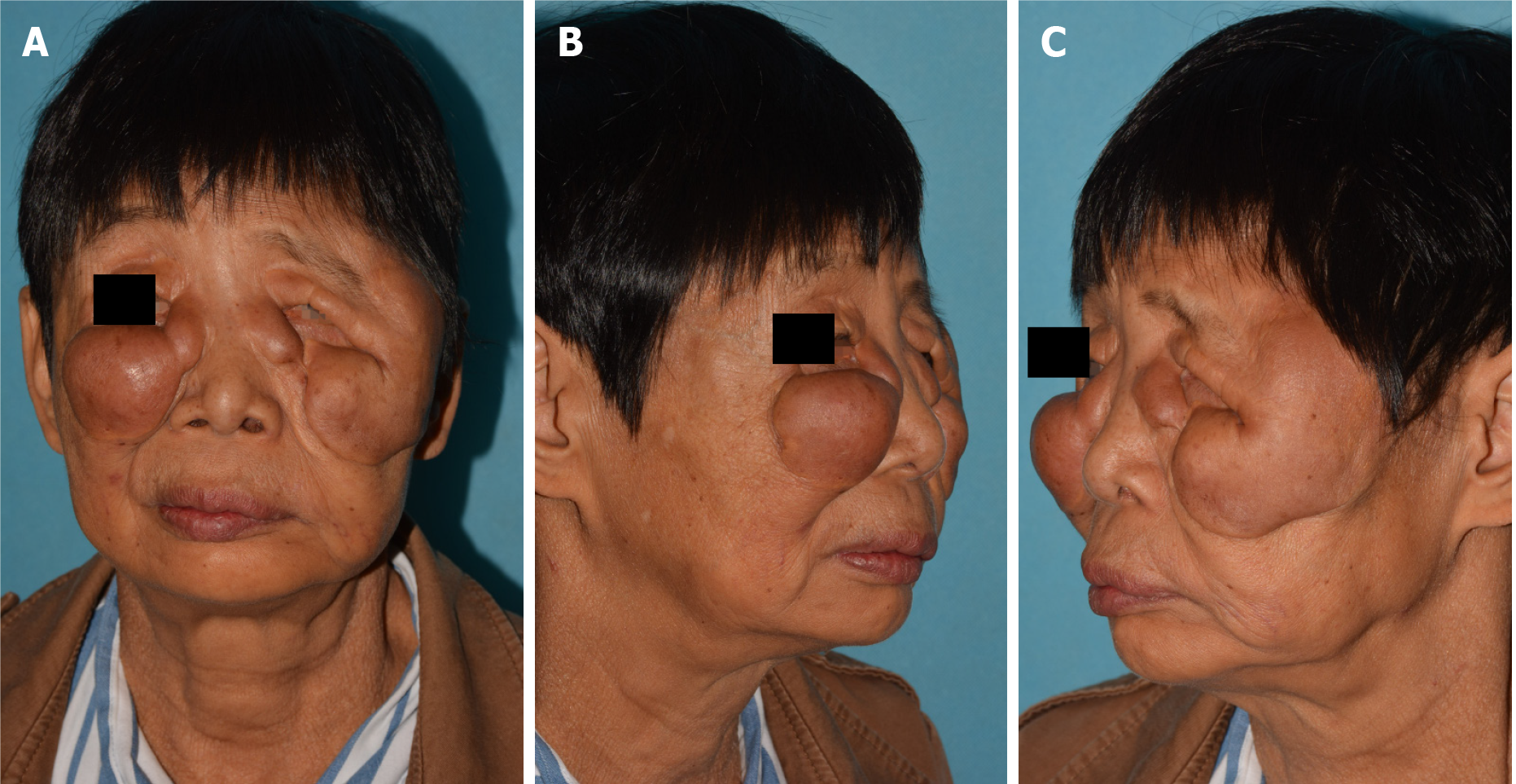
The patient presented with a 15-year history of facial swelling that progressively invaded bilaterally from the inner canthi and eyelids outwards. In recent years, the swelling gradually turned into pendulous masses causing severe disfigurements, brow ptosis, and palpebral fissure distortion (Figure 1). Three months prior to admission, the patient complained blurred vision with pupillary axis obstruction of the left eye. The patient reported no pain or itching on the lesion.
The patient denied any previous medical history.
The patient denied bad personal habits and any family history.
Physical examination showed non-pitting masses in the bilateral periocular regions including the inner canthi, upper and lower eyelids, and zygoma, and in the left temple region with a clear boundary (Figure 1), which were rigid and had no associated tenderness. She showed no signs of rosacea and no other abnormities were found on her body or limbs.
Routine blood and urine examinations, coagulation function and biochemistry parameters, and tumor markers showed normal results.
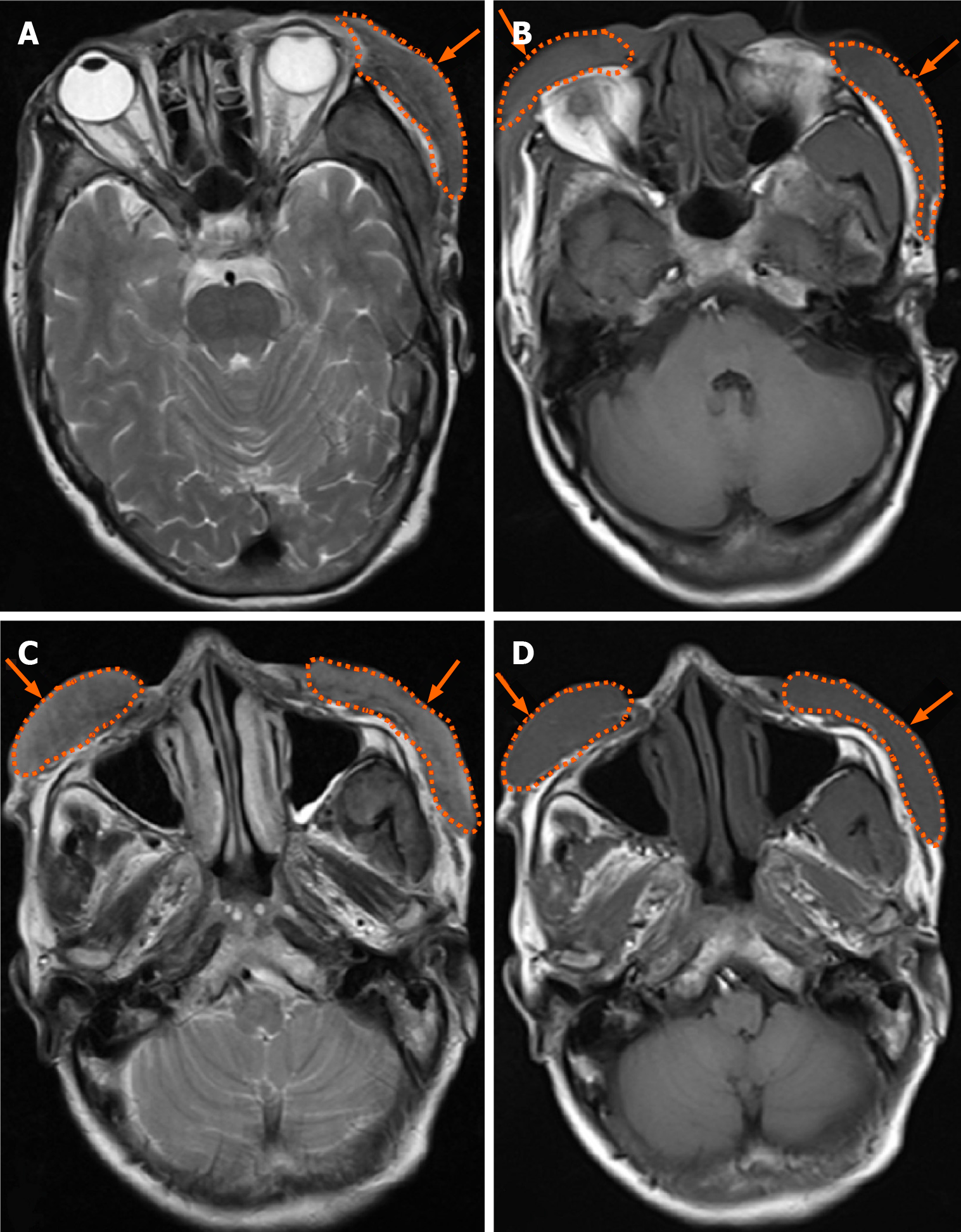
Cranial magnetic resonance imaging indicated that the bilateral periorbital and the left temporal soft tissues had swelling without cranium and intra-orbital invasion, and T1 weighted imaging and T2 weighted showed iso-intensity signals (Figure 2).
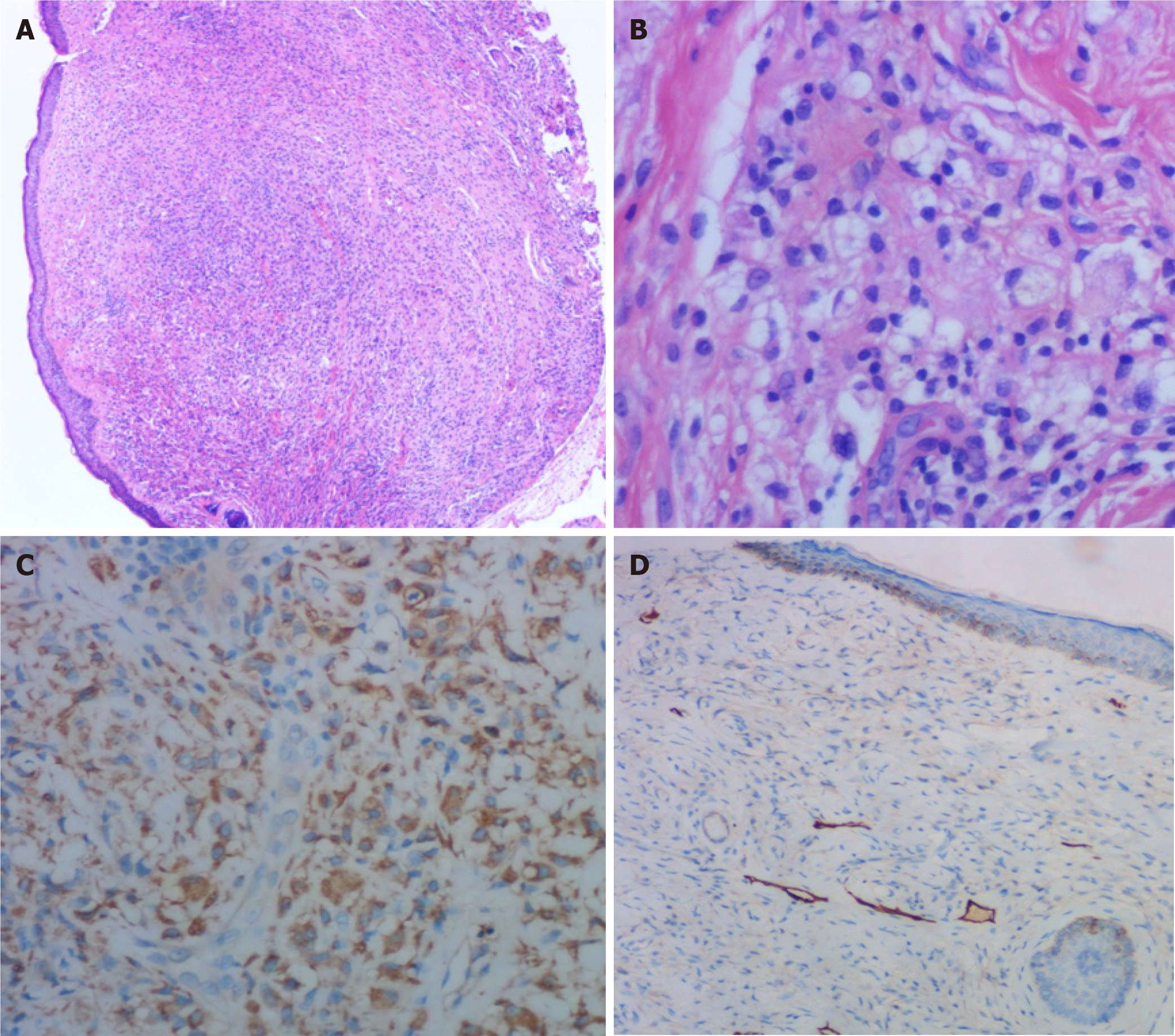
Postoperative histological findings showed a large amount of histiocyte infiltration in clear-cut granulomas (Figure 3A), and infiltration of lymphocytes, foam-like histiocytes, multinucleated giant cells, and mast cells around blood and lymphatic vessels (Figure 3B). Tissue edema was observed in the dermis with lymphatic vessel dilatation and the focal perilymphatic granulomatous reaction. Immunohistochemical staining showed positive expression of CD68 in perivascular, perilymphatic, and perifollicular histiocytic infiltration as well as fibrosis reaction (Figure 3C). The dilated lymphatic vessels were formed by the D2-40 positive lymphatic endothelium (Figure 3D).
Morbihan syndrome.
Blepharoplasty was performed under local anesthesia. The skin and mass superficial to the tarsus were totally excised and removed on the left upper eyelid. After surgery, intralesional injections of triamcinolone (80 mg) were given to the residual masses. Isotretinoin (20 mg/d) and tetracyclines (500 mg/d) were also given to the patient for 3 months.
The patient’s vision field was improved and the progression of facial mass was sluggish during 1-year follow-up.
Morbihan syndrome was first reported in 1957[2]. It is characterized by chronic persistent edema on the upper half of the face[4]. In most cases, systemic manifestations were absent and laboratory tests were negative. The diagnosis of Morbihan syndrome mainly relies upon clinical and pathological features[5]. In this case with a 15-year history of swelling, persistent lymphedema resulted in lymphatic damage and fibrosis, thus causing facial deformities and even pupillary axis obstruction.
The typical histopathological feature in early stage of Morbihan syndrome is localized lymphedema, with the presence of dilated blood vessels, and perivascular and perifollicular infiltration of histiocytes including lymphocytes, neutrophils, and mast cells[6]. Recurrent and prolonged inflammatory response would sequentially trigger the dermal lymphatic vessel dilation, obstruction, and even lymph drainage alteration. Eventually, non-pitting edema would be transformed into a persistent solid mass, which is symbolized by the generation of fibrotic induration and sarcoidal granulomas. This case showed evidence of granulomas, which indicated that the syndrome has progressed into late phase. Immunohistochemical studies showed D2-40 expression in the lymphatic endothelial cells, which was reported to be the typical phenotype of endothelial cells in Morbihan syndrome[7]. In addition, CD68 could also act as a histological marker for Morbihan syndrome to exclude carcinoma[8].
The pathogenic mechanisms of Morbihan syndrome are unclear, and some dermatologists recognized it as one of complications of rosacea[9]. However, there are also some reported cases of Morbihan syndrome that show no clinical manifestations of rosacea, which are similar to our case[10].
There is still no consensus on the standard treatment for this disease. To date, few reported cases showed medication therapies like corticosteroids and antibiotics that were beneficial for patients with Morbihan syndrome to relieve the symptoms[11]. We hold the opinion that early diagnosis and treatment are essential for the well-being of the patient. Ignorance of the syndrome progression from the physician and/or the patient, and the absence of effective treatments could possibly contribute to the chronic course of Morbihan syndrome like this patient. Patients suffering from Morbihan syndrome usually do not complain of any other symptoms until the vision field is impaired like this case. For patients with pupillary axis obstruction, surgical intervention is necessary to remove tissue mass and restore the normal visual field[12]. Blepharoplasty is supposed to treat the visual shade resulting from Morbihan syndrome progression.
Morbihan syndrome is an infrequent and refractory disease, which is characteristic with recurrent woody facial edema on the upper two thirds of the face. Solid facial edema is persistent and non-pitting, causing facial contour deformities and even vision field impairment. The diagnosis of Morbihan syndrome depends on clinical features, imaging information, and pathology. Blepharoplasty is optional to improve the visual field for these patients with severe pupillary axis obstruction.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aoun G, Bozkurt M S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wang LYT
| 1. | Yvon C, Mudhar HS, Fayers T, Siah WF, Malhotra R, Currie Z, Tan J, Rajak S. Morbihan Syndrome, a UK Case Series. Ophthalmic Plast Reconstr Surg. 2020;36:438-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Carlson JA. Lymphedema and subclinical lymphostasis (microlymphedema) facilitate cutaneous infection, inflammatory dermatoses, and neoplasia: A locus minoris resistentiae. Clin Dermatol. 2014;32:599-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): evidence of hidden immunologic contact urticaria and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52:595-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Okubo A, Takahashi K, Akasaka T, Amano H. Four cases of Morbihan disease successfully treated with doxycycline. J Dermatol. 2017;44:713-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Murphy MJ, Kogan B, Carlson JA. Granulomatous lymphangitis of the scrotum and penis. Report of a case and review of the literature of genital swelling with sarcoidal granulomatous inflammation. J Cutan Pathol. 2001;28:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Cabral F, Lubbe LC, Nóbrega MM, Obadia DL, Souto R, Gripp AC. Morbihan disease: a therapeutic challenge. An Bras Dermatol. 2017;92:847-850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Carruth BP, Meyer DR, Wladis EJ, Bradley EA, Al-Rohil R, Jones DM, Bartley GB. Extreme Eyelid Lymphedema Associated With Rosacea (Morbihan Disease): Case Series, Literature Review, and Therapeutic Considerations. Ophthalmic Plast Reconstr Surg. 2017;33:S34-S38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Ramirez-Bellver JL, Pérez-González YC, Chen KR, Díaz-Recuero JL, Requena L, Carlson JA, Llamas-Velasco M. Clinicopathological and Immunohistochemical Study of 14 Cases of Morbihan Disease: An Insight Into Its Pathogenesis. Am J Dermatopathol. 2019;41:701-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease: A Case Series Report and Review of the Literature. Arch Dermatol. 2012;148:1395-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Bechara FG, Jansen T, Losch R, Altmeyer P, Hoffmann K. Morbihan's disease: treatment with CO2 Laser blepharoplasty. J Dermatol. 2004;31:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |