Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7117
Peer-review started: January 1, 2021
First decision: May 24, 2021
Revised: May 27, 2021
Accepted: July 6, 2021
Article in press: July 6, 2021
Published online: August 26, 2021
Processing time: 234 Days and 14.9 Hours
Malignant peripheral nerve sheath tumors (MPNSTs) are a group of rare and aggressive sarcomas that often arise from major peripheral nerves and represent a notable challenge to efficacious treatment. MPNSTs can occur in any body surface and visceral organs with nerve fiber distribution. The treatment options for MPNSTs include surgery, chemotherapy, and adjuvant radiotherapy.
A 26-year-old female cellist presented with chest pain on her left side when she squatted to lift the cello. One week later, a chest X-ray was performed and revealed fracture of the fourth rib on the left side. Three months later, the patient inadvertently touched a mass on the left side of the chest wall. Chest computed tomography (CT) three-dimensional reconstruction of the ribs revealed bone destruction of the fourth rib on the left side with a soft tissue mass shadow measuring 5.7 cm × 3.7 cm. CT-guided puncture biopsy of the tumor showed that heterotypic cells (spindle cells) tended to be nonepithelial tumor lesions. PET-CT demonstrated bone destruction and a soft tissue mass with avid 18F-fluorodeoxyglucose activity (SUVmax7.5) in the left fourth rib. The tumor of the left chest wall was resected under general anesthesia, and reconstruction of the chest wall was performed. The postoperative pathological report exhibited an MPNST.
MPNSTs are relatively chemo-insensitive tumors. The mainstay of treatment for MPNSTs remains resection with tumor-free margins.
Core Tip: Malignant peripheral nerve sheath tumors (MPNSTs) are a group of rare and aggressive sarcomas that often arise from major peripheral nerves and represent a notable challenge to efficacious treatment. We present a rare case of MPNST of the chest wall in a female cellist who initially presented with a pathological rib fracture. We used the Synthes MatrixRib Precontoured Plate system to reconstruct her chest wall and restore its appearance. The mainstay of treatment for MPNST remains resection with tumor-free margins. Furthermore, functional reconstructions can play an important role in improving functional status.
- Citation: Guo X, Wu WM, Wang L, Yang Y. Reconstruction of the chest wall after resection of malignant peripheral nerve sheath tumor: A case report. World J Clin Cases 2021; 9(24): 7117-7122
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7117.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7117
Malignant peripheral nerve sheath tumors (MPNSTs) are a class of rare and aggressive neurogenic malignant tumors, accounting for 5% to 10% of soft tissue sarcomas. The World Health Organization (WHO) named MPNST as a heterogeneous tumor composed of fibroblasts, epithelial cell membrane antigen positive perineural cells, Schwann cells, CD34-positive dendritic cells, and primitive neuroepithelial cells. At present, MPNST is also known as a sarcoma originating from peripheral nerves or malignant transformation of neurofibroma. MPNST can occur in any body surface and visceral organs with nerve fiber distribution[1-4]. We report a case of MPNST of the chest wall in a patient who initially presented with a pathological rib fracture and underwent reconstruction of the chest wall after resection.
A 26-year-old female cellist presented with chest pain on her left side when she squatted to lift the cello. She thought that it was only a muscle strain and did not go to the hospital for treatment. However, chest pain worsened and could not be alleviated. One week later, she sought medical attention for worsened symptoms. A chest X-ray was performed and revealed fracture of the fourth rib on the left side. After oral administration of painkillers for 10 d, the symptoms of chest pain gradually relieved.
Three months later, the patient inadvertently touched a mass on the left side of the chest wall, which could be moved without obvious pain. She sought medical attention for this mass.
The patient had no significant past medical history or surgical history and did not take any medications.
The patient’s personal and family histories were negative.
Physical examination revealed a massive (approximately 5.7 cm × 3.7 cm) soft tissue mass bulging from his left anterolateral chest wall.
The laboratory examination findings were all within normal limits, including the complete blood count, and kidney and liver function test results. Serum levels of all female tumor markers were within normal ranges.
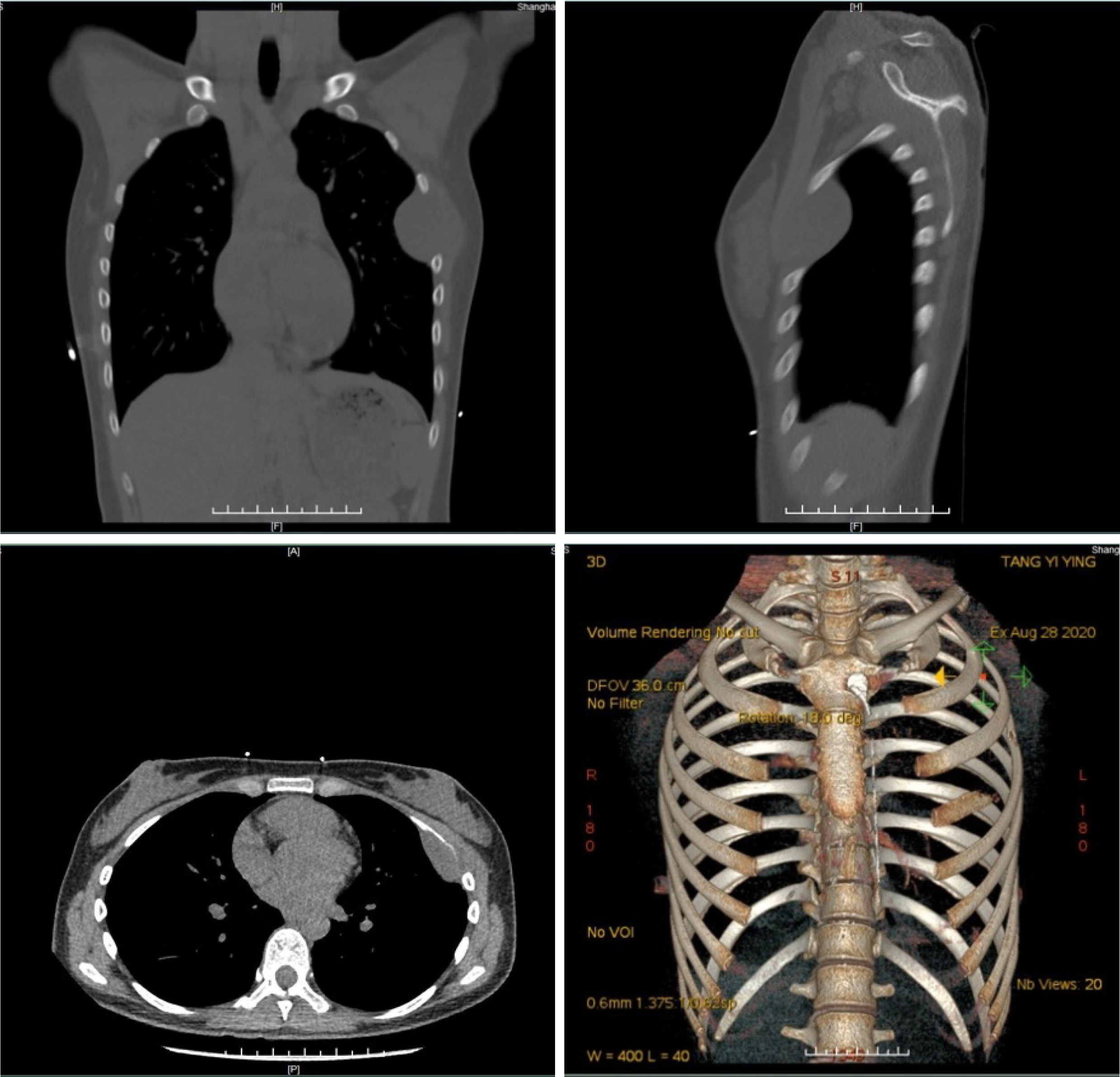
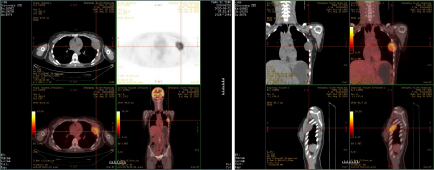
Ultrasound revealed a cystic-solid mass on the left chest wall. A chest computed tomography (CT) three-dimensional reconstruction of the ribs revealed bone destruction of the fourth rib on the left side with a soft tissue mass shadow measuring 5.7 cm × 3.7 cm (Figure 1). CT-guided puncture biopsy of the tumor revealed that heterotypic cells (spindle cells) tended to be nonepithelial tumor lesions. PET-CT showed bone destruction and a soft tissue mass with avid 18F-fluorodeoxyglucose activity (SUVmax7.5) in the left fourth rib (Figure 2).
The postoperative pathological report revealed an MPNST measuring 5.7 cm × 4 cm × 3.7 cm. The fourth rib and the intercostal muscle were involved in the tumor. No tumor was found in the third rib and the fifth rib. Immunohistochemical results are as follows: CK (-), CK19 (-), calponin (-), CD34 (-), TLE-1 (+), S100 (-), Ki67 (80% +), NKX2.2 (weakly +), CD99 (-), Bcl-2 (+), SMA (-), H3K27Me3 (-), caldesmon (-), SOX10 (-), NSE (-), and GFAP (-). SYT-related gene translocation was negative. A diagnosis of MPNST of the chest wall was confirmed.
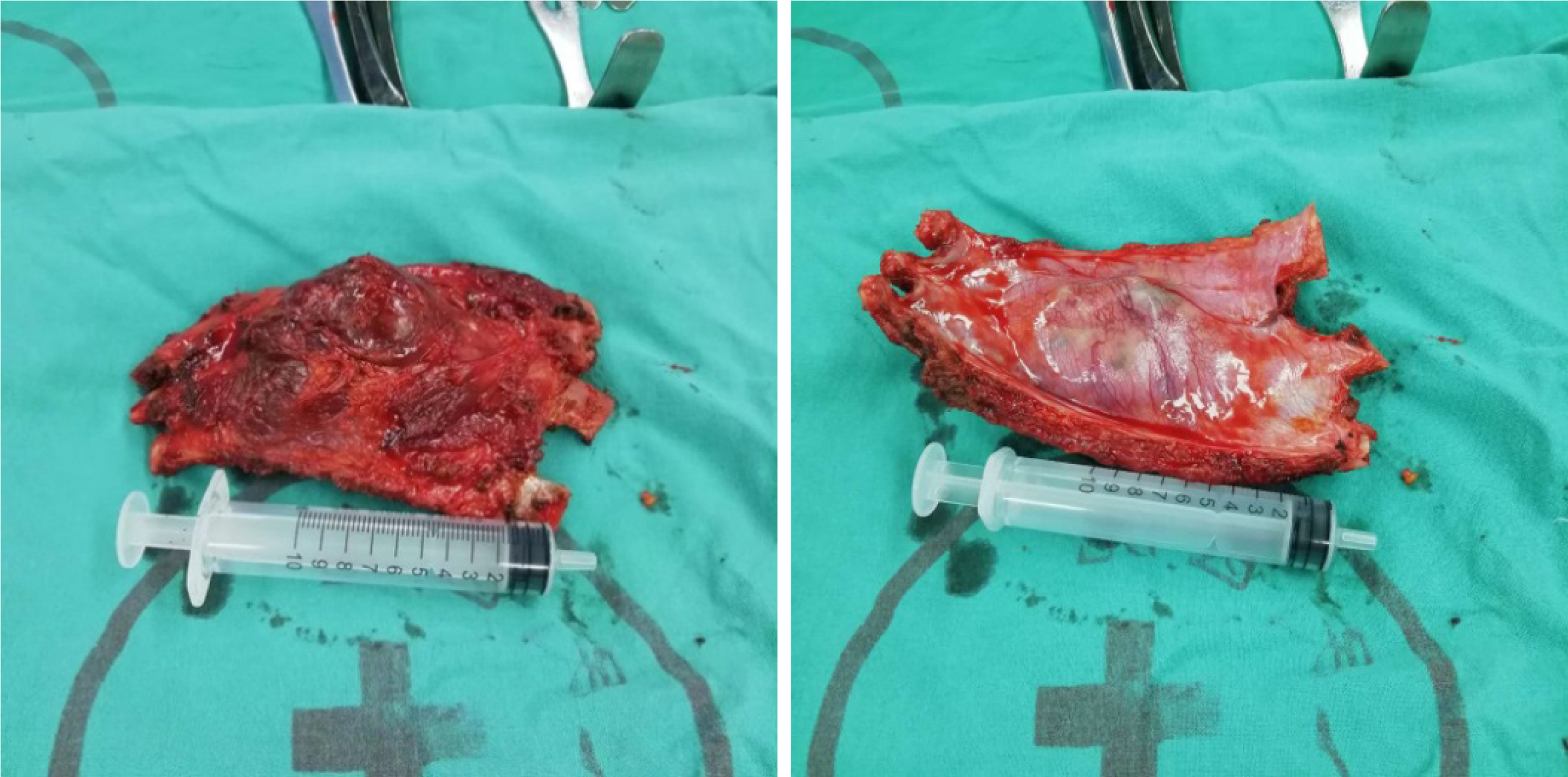
After completing the relevant preoperative examination, the tumor of the left chest wall was resected under general anesthesia and reconstruction of the chest wall was performed. The extent of resection included several partial ribs above and below the lesion (from the upper edge of the 3rd rib to the lower edge of the 5th rib), with surgical margins of 5 cm. Attached structures, including the serratus anterior, the pectoralis minor, the intercostal muscle, and the parietal pleura, were also excised except for the pectoralis major (Figure 3). Rapid frozen pathology showed spindle cell sarcoma and no tumor infiltration in the margin of resection. The chest wall defect was reconstructed with MatrixRib plates, and the soft tissue defect was repaired with a heart Dacron patch. Two drainage tubes were placed superficially to the Dacron patch and thoracic cavity. The thoracotomy was closed routinely.
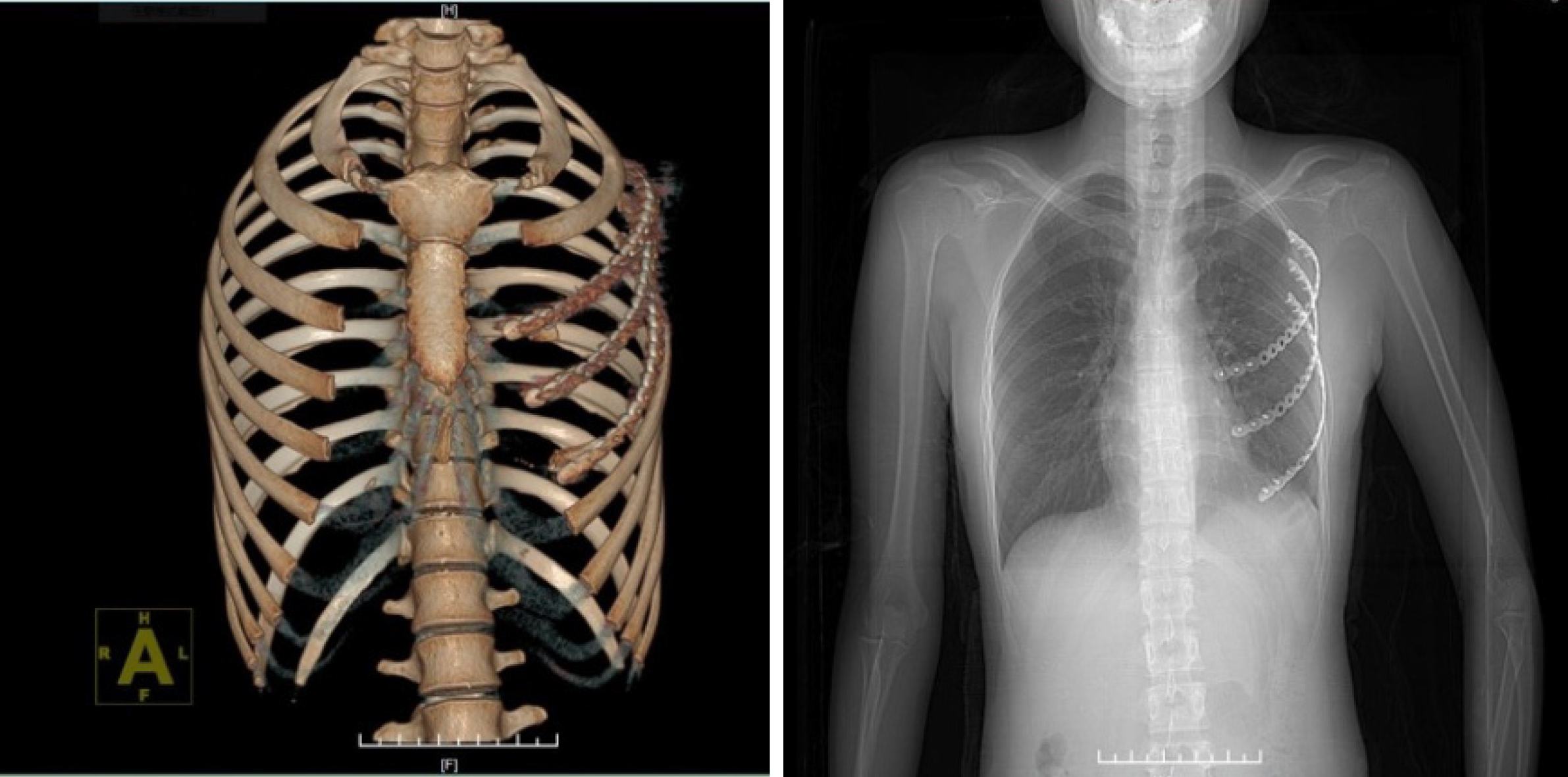
The patient was discharged 7 d after surgery. Three months after the operation, the plates remained intact with no signs of loosening or infection and no local recurrence or metastasis was found on chest CT (Figure 4).
MPNSTs are a group of rare and aggressive sarcomas that often arise from major peripheral nerves and represent a notable challenge to efficacious treatment. Up to 50% of MPNSTs occur in association with neurofibromatosis type 1 (NF-1), which is present in patients at younger ages and with larger tumors that are commonly associated with extensive plexiform neurofibromas compared with patients without NF1[5,6]. MPNSTs are associated with poorer clinical outcomes. The treatment options for MPNST include surgery, chemotherapy, and adjuvant radiotherapy.
The role of chemotherapy in the management of MPNST remains controversial. In recent years, it has been reported that chemotherapy before and after surgery has a specific effect on MPNST. Preoperative neoadjuvant chemotherapy can reduce the size of the tumor to facilitate resection[7]. In Kroep et al[8]’s report, the doxorubi
The only known definitive treatment for MPNST is surgical resection with wide negative margins. The prognostic indicators for MPNST include the tumor grade, presence of distant metastases, and positive surgical resection margins. Wong et al[12] observed that MPNST patients with positive margins exhibited 3-year and 5-year overall survival rates of 47% and 22%, respectively, whereas those with negative margins exhibited higher rates of 74% and 67%, respectively. Complete surgical resection with wide negative margins can offer significant long-term benefits on survival in patients with MPNST and should be the principal goal of MPNST treatment[13]. Complete surgical resection can result in large defects requiring reconstruction to maintain chest wall integrity. Previously, methyl methacrylate was the popular choice to reconstruct the bony thorax. Recent advances in rib fixation devices have simplified the procedure, in particular the Synthes MatrixRib Precontoured Plate system[14]. Both muscle and omentum can be used to reconstruct soft tissue defects of the chest wall. Muscle can be transposed as muscle alone or as a musculocutaneous flap and is the tissue of choice for closure of most full-thickness soft tissue defects. The omentum is reserved for partial-thickness reconstruction or as a remedial procedure when muscle is not available or has failed in a previous full-thickness repair[15].
We present a rare case of MPNST of the chest wall in a female cellist who initially presented with pathological rib fracture. Considering that she is a cellist with a musical dream, we used the Synthes MatrixRib Precontoured Plate system to reconstruct her chest wall and restore its appearance. The pectoralis major without tumor invasion was preserved so that she could still have sufficient strength to play the cello after recovery. In addition, she was just married with no kids. To realize her wish to be a mother, she refused chemotherapy and radiotherapy. In conclusion, MPNSTs are relatively chemo-insensitive tumors. Adjuvant radiotherapy is recommended for establishing local control in R1 resections. Therefore, the mainstay of treatment for MPNST remains resection with tumor-free margins. Furthermore, functional reconstructions can play an important role in improving functional status.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee SS S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Li JH
| 1. | Woodruff JM, Christensen WN. Glandular peripheral nerve sheath tumors. Cancer. 1993;72:3618-3628. [PubMed] |
| 2. | Ferner RE, Gutmann DH. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis. Cancer Res. 2002;62:1573-1577. [PubMed] |
| 3. | Fuchs B, Spinner RJ, Rock MG. Malignant peripheral nerve sheath tumors: an update. J Surg Orthop Adv. 2005;14:168-174. [PubMed] |
| 4. | Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica. 2021;113:70-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 551] [Article Influence: 110.2] [Reference Citation Analysis (0)] |
| 5. | Farid M, Demicco EG, Garcia R, Ahn L, Merola PR, Cioffi A, Maki RG. Malignant peripheral nerve sheath tumors. Oncologist. 2014;19:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 245] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 6. | Watson KL, Al Sannaa GA, Kivlin CM, Ingram DR, Landers SM, Roland CL, Cormier JN, Hunt KK, Feig BW, Ashleigh Guadagnolo B, Bishop AJ, Wang WL, Slopis JM, McCutcheon IE, Lazar AJ, Torres KE. Patterns of recurrence and survival in sporadic, neurofibromatosis Type 1-associated, and radiation-associated malignant peripheral nerve sheath tumors. J Neurosurg. 2017;126:319-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 7. | Stucky CC, Johnson KN, Gray RJ, Pockaj BA, Ocal IT, Rose PS, Wasif N. Malignant peripheral nerve sheath tumors (MPNST): the Mayo Clinic experience. Ann Surg Oncol. 2012;19:878-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 246] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 8. | Kroep JR, Ouali M, Gelderblom H, Le Cesne A, Dekker TJA, Van Glabbeke M, Hogendoorn PCW, Hohenberger P. First-line chemotherapy for malignant peripheral nerve sheath tumor (MPNST) versus other histological soft tissue sarcoma subtypes and as a prognostic factor for MPNST: an EORTC soft tissue and bone sarcoma group study. Ann Oncol. 2011;22:207-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 155] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Zehou O, Fabre E, Zelek L, Sbidian E, Ortonne N, Banu E, Wolkenstein P, Valeyrie-Allanore L. Chemotherapy for the treatment of malignant peripheral nerve sheath tumors in neurofibromatosis 1: a 10-year institutional review. Orphanet J Rare Dis. 2013;8:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Kim A, Stewart DR, Reilly KM, Viskochil D, Miettinen MM, Widemann BC. Malignant Peripheral Nerve Sheath Tumors State of the Science: Leveraging Clinical and Biological Insights into Effective Therapies. Sarcoma. 2017;2017:7429697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 11. | Bradford D, Kim A. Current treatment options for malignant peripheral nerve sheath tumors. Curr Treat Options Oncol. 2015;16:328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Wong WW, Hirose T, Scheithauer BW, Schild SE, Gunderson LL. Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J Radiat Oncol Biol Phys. 1998;42:351-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 298] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 13. | James AW, Shurell E, Singh A, Dry SM, Eilber FC. Malignant Peripheral Nerve Sheath Tumor. Surg Oncol Clin N Am. 2016;25:789-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 105] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 14. | Ng CS. Recent and Future Developments in Chest Wall Reconstruction. Semin Thorac Cardiovasc Surg. 2015;27:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Sanna S, Brandolini J, Pardolesi A, Argnani D, Mengozzi M, Dell'Amore A, Solli P. Materials and techniques in chest wall reconstruction: a review. J Vis Surg. 2017;3:95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 100] [Article Influence: 12.5] [Reference Citation Analysis (0)] |