Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7073
Peer-review started: March 23, 2021
First decision: June 24, 2021
Revised: July 4, 2021
Accepted: July 13, 2021
Article in press: July 4, 2021
Published online: August 26, 2021
Processing time: 153 Days and 19.2 Hours
Peptic ulcer (PU) is more prevalent in patients with liver cirrhosis. The role of Helicobacter pylori (H. pylori) infection in the pathogenesis of PU in patients with cirrhosis is still not elucidated.
To perform a meta-analysis on the prevalence of H. pylori infection and PU and their association in liver cirrhosis patients.
We searched PubMed, EMBASE, Web of Science, Cochrane, CNKI, Wangfang, and CQVIP databases from inception to July 10, 2020. Odds ratio (OR) and 95% confidence interval (CI) were pooled using a random-effects model. The statistical heterogeneity among studies (I2-index), subgroup analyses, regression analysis, sensitivity analysis, and the possibility of publication bias were assessed.
A total of 14 studies (13 cross-sectional studies; 1 cohort study) involving 2775 individuals (611 cases with PU and 2164 controls) were included in our meta-analysis. The prevalence of PU in patients with cirrhosis was 22%. The prevalence of H. pylori infection was 65.6% in cirrhotic patients with PU, and 52.5% in those without. The pooled overall OR was 1.73 (95%CI: 1.16-2.56, I2 = 66.2%, P < 0.001, Z = 2.7, Pz < 0.05). We did not find the cause of heterogeneity in the subgroup analyses and meta-regression analysis except for one study. Funnel plot did not show significant publication bias. The results of Begg’s test and Egger’s test indicated no evidence of substantial publication bias (PBegg = 0.732, PEgger = 0.557).
There is a weakly positive association between H. pylori infection and PU in patients with liver cirrhosis. It is suggested that H. pylori infection may play a role in the pathogenesis of PU in liver cirrhotic patients.
Core Tip: Peptic ulcer (PU) is more prevalent in patients with liver cirrhosis than in the general population. What’s more, cirrhotic patients with PU have a high risk of PU bleeding than the general population. So, if studies can prove that Helicobacter pylori (H. pylori) is also an independent risk factor for PU in patients with liver cirrhosis, the eradication of H. pylori can indirectly prevent PU bleeding in cirrhotic patients. This study showed that there is a weak positive association between H. pylori infection and PU in patients with liver cirrhosis.
- Citation: Wei L, Ding HG. Helicobacter pylori infection and peptic ulcer disease in cirrhotic patients: An updated meta-analysis. World J Clin Cases 2021; 9(24): 7073-7084
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7073.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7073
Based on endoscopy screening, the prevalence of peptic ulcer (PU) in cirrhotic patients has been reported to be approximately 5%-20% compared to 2%-4% in the general population[1-5]. It has been shown that cirrhotic patients have a significantly higher risk of PU bleeding than the general population[6]. There are data indicating that upper gastrointestinal hemorrhage (UGIB) due to PU worsens the prognosis of cirrhotic patients. The morbidity and mortality of patients with liver cirrhosis and PUs are very high. Leontiadis et al[7] performed a meta-analysis on the effect of comor
This meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, and the protocol for this meta-analysis is available on international prospective register of systematic reviews (PROSPERO; registration number CRD42020218033).
PubMed, EMBASE, Web of Science, Cochrane, CNKI, Wangfang, and CQVIP data
The inclusion criteria were as follows: (1) Cross-sectional, case-control, or cohort studies published as original articles that explored the association between PU and H. pylori in cirrhotic patients; (2) H. pylori infection had to be confirmed by at least one positive test as follows: Serological testing (using H. pylori immunoglobulin G enzyme-linked immunosorbent assays), 13C-labeled or 14C-labeled urea breath test (UBT), rapid urease test (RUT), histology, or fecal antigen test; (3) Cirrhosis had to be diagnosed by histology, or by clinical, analytical, and imaging (mostly ultrasonography) methods; etiology and Child-Pugh score were specified; (4) The diagnosis of PU was obtained by endoscopy; and (5) All the studies included a control group.
Criteria for exclusion were as follows: (1) Letters, abstracts, case reports, animal studies, editorials, reviews, and meta-analyses; (2) Irrelevant literature and duplicate studies; and (3) The lack of data made it impossible to derive an exact number of patients with or without H. pylori and with or without PU by endoscopy.
Two investigators (Ding HG and Wei L) independently screened the titles and abstracts of all studies identified using the previously described search criteria to identify studies meeting the inclusion criteria. Each study meeting the requirements of the inclusion criteria then underwent an independent full-text review by both investigators. Disagreements about the inclusion of studies between investigators were resolved by discussion.
We extracted the following data from each study: (1) Study characteristics, including the name of the first author, publication year, country of publication, study design, and sample size; and (2) The number of positive/negative H. pylori infections in the PU with liver cirrhosis group, the number of positive/negative H. pylori infections in the control group, method of detection of H. pylori infection, method of detection of liver cirrhosis, and case/control ratio. We assessed the quality of each study according to the Agency for Health care Research and Quality (AHRQ), which is a validated scale for cross-sectional studies[23].
We used STATA version 12.0 software (Stata Corporation, College Station, TX, United States) to perform meta-analyses. Odds ratio (OR) with 95% confidence interval (CI) was pooled to describe the ratio of the prevalence of H. pylori infection in cirrhotic patients with and without PU. Heterogeneity was assessed by Chi-square-based Q test and I2 index was used to evaluate the statistical heterogeneity between the studies[24]. The significance for the Q test was defined as P value < 0.1. Heterogeneity was classified as follows: I2 value of 0%-25% indicated no heterogeneity, 26%-50% indicated low heterogeneity, 51%-75% indicated moderate heterogeneity, and 76%-100% indicated high heterogeneity. A fixed effect model was used when I2 value was < 50%, and a random effect model was used when I2 value was > 50%[24]. Subgroup analysis and regression analysis were performed to explore sources of heterogeneity. The forest plot was used to assess the relationship between H. pylori infection and PU in cirrhotic patients. The funnel plot and Begg’s and Egger’s tests were used to investigate publication bias. P < 0.05 was considered statistically significant.
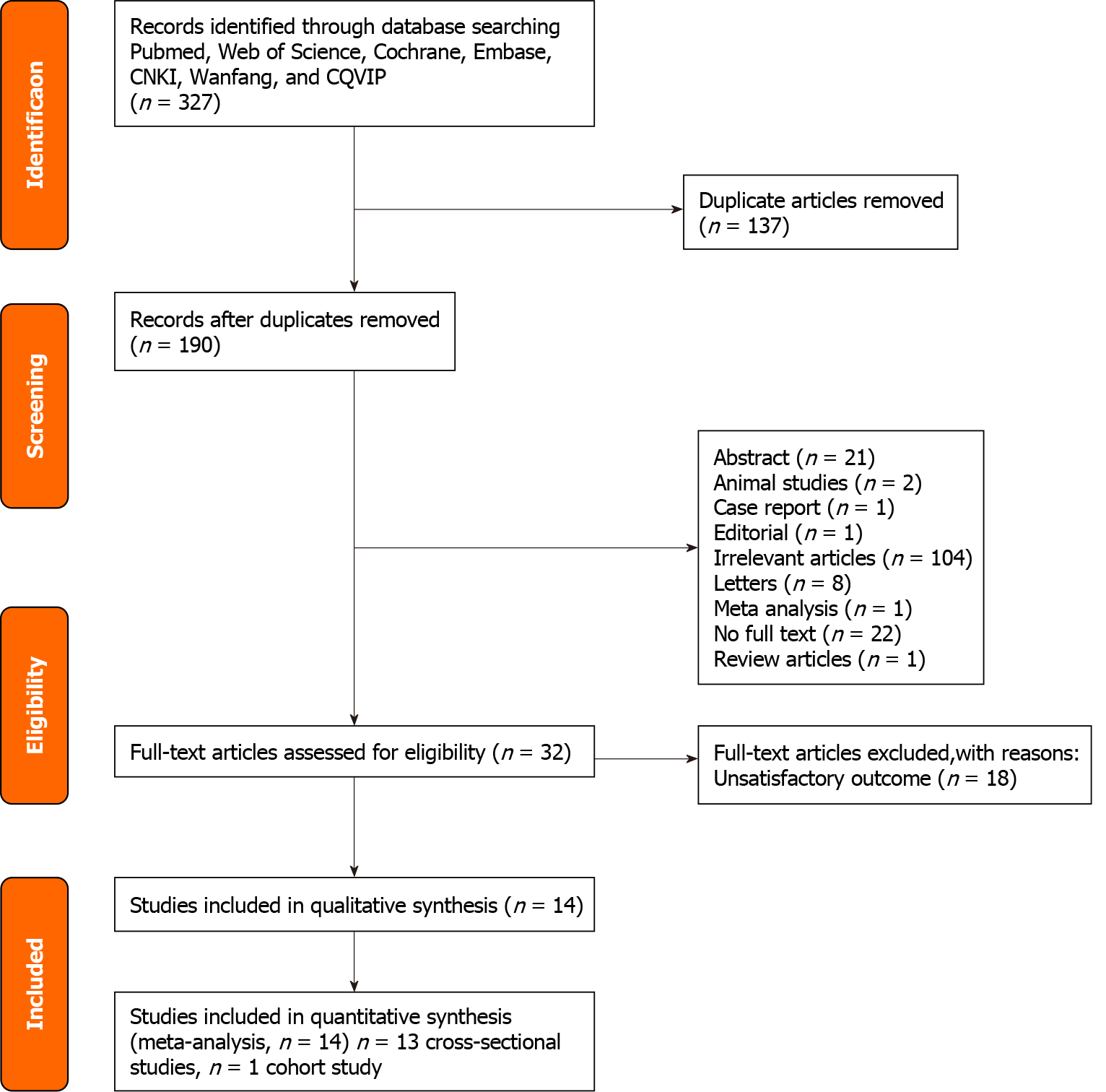
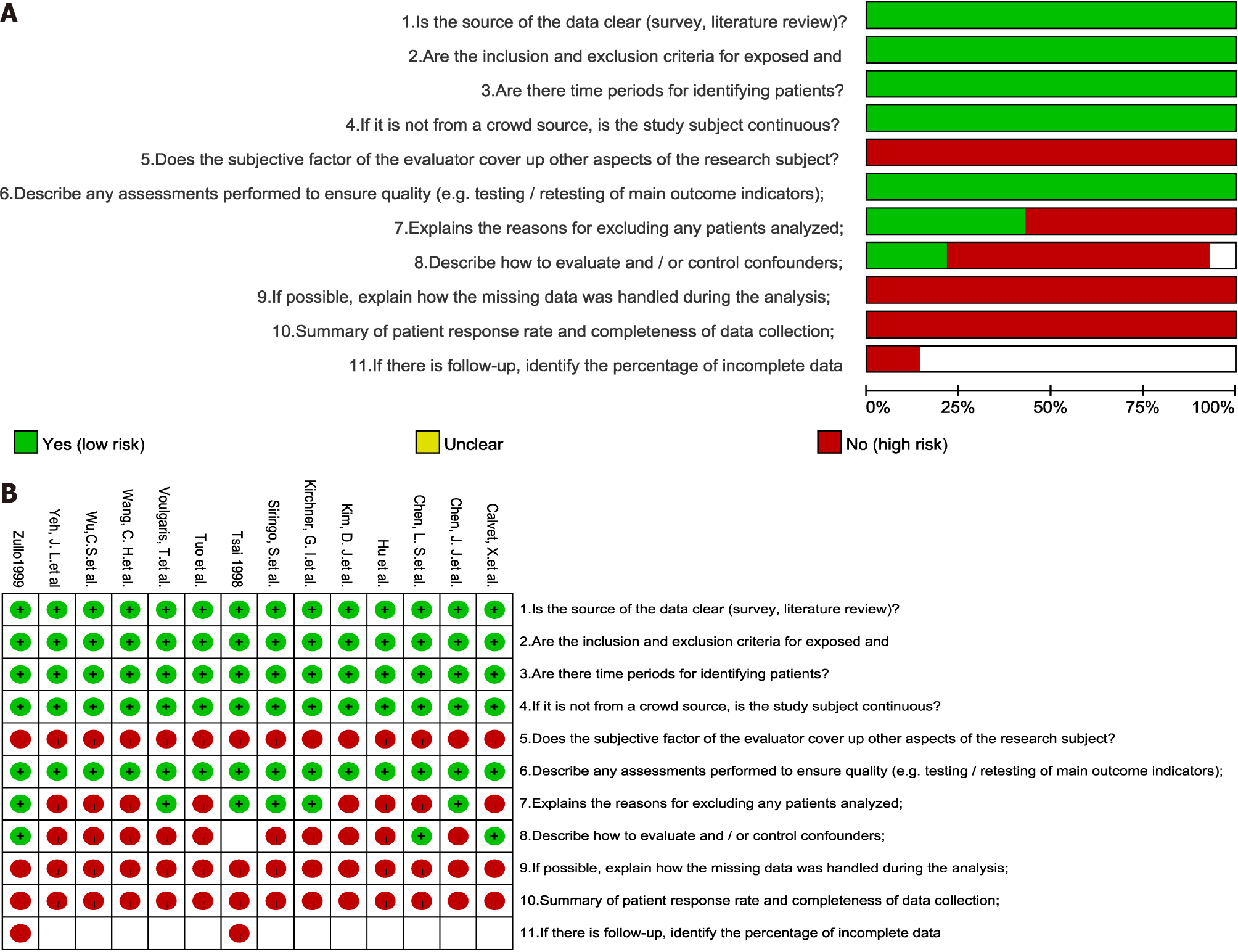
The initial database search identified 327 records. After removing 137 duplicates, 190 records remained. Of these 190 studies, 176 were excluded. Thus, 14 studies were included in the meta-analysis. A flow diagram of the literature search is shown in Figure 1. The main characteristics of the 14 studies are summarized in Table 1. A total of 14 studies involving 2775 individuals were included in our meta-analysis[5,9-21]. These studies were published between 1994 and 2019. Our meta-analysis contained 13 cross-sectional studies and 1 cohort study[19]. Figure 2 shows the results of quality assessment according to the AHRQ.
| Study | Area | Study type | Peptic ulcer (Hp+/Hp-) | Prevalence | Non-ulcer (Hp+/Hp-) | Prevalence | D of Hp | D of LC |
| Wu et al[11], 1995 | Asia | Cross-sectional | 23/6 | 82.1% | 59/32 | 64.8% | ELISA | Ultrosound |
| Kim et al[13], 2008 | Asia | Cross-sectional | 24/46 | 34.3% | 76/142 | 34.9% | Multiple | Multiple |
| Siringo et al[12], 1997 | Europe | Cross-sectional | 39/2 | 95.1% | 78/34 | 69.4% | ELISA | Multiple |
| Kirchner et al[10], 2011 | Europe | Cross-sectional | 11/7 | 61.1% | 65/27 | 70.7% | ELISA | Multiple |
| Voulgaris et al[16], 2019 | Europe | Cross-sectional | 9/10 | 47.4% | 45/36 | 55.6% | Multiple | Multiple |
| Wang et al[15], 1997 | Asia | Cross-sectional | 12/18 | 40.0% | 7/12 | 36.8% | Multiple | Multiple |
| Chen et al[17], 1994 | Asia | Cross-sectional | 14/17 | 45.2% | 33/44 | 42.9% | ELISA | Multiple |
| Chen et al[18], 1995 | Asia | Cross-sectional | 9/7 | 56.3% | 18/16 | 52.9% | RUT | Multiple |
| Yeh et al[19], 2001 | Asia | Cohort | 26/19 | 57.8% | 31/33 | 48.4% | UBT | Multiple |
| Hu et al[20], 2002 | Asia | Cross-sectional | 86/8 | 91.5% | 373/189 | 66.4% | Multiple | Multiple |
| Tuo et al[21], 2000 | Asia | Cross-sectional | 29/45 | 39.2% | 143/279 | 33.9% | Multiple | Multiple |
| Calvet et al[14], 1998 | Europe | Cross-sectional | 14/6 | 70.0% | 79/91 | 46.5% | Multiple | Multiple |
| Zullo et al[9], 1999 | Europe | Cross-sectional | 51/9 | 85.0% | 84/82 | 50.6% | Multiple | Multiple |
| Tsai[5], 1998 | Asia | Cross-sectional | 54/10 | 84.4% | 46/20 | 69.7% | Multiple | Multiple |
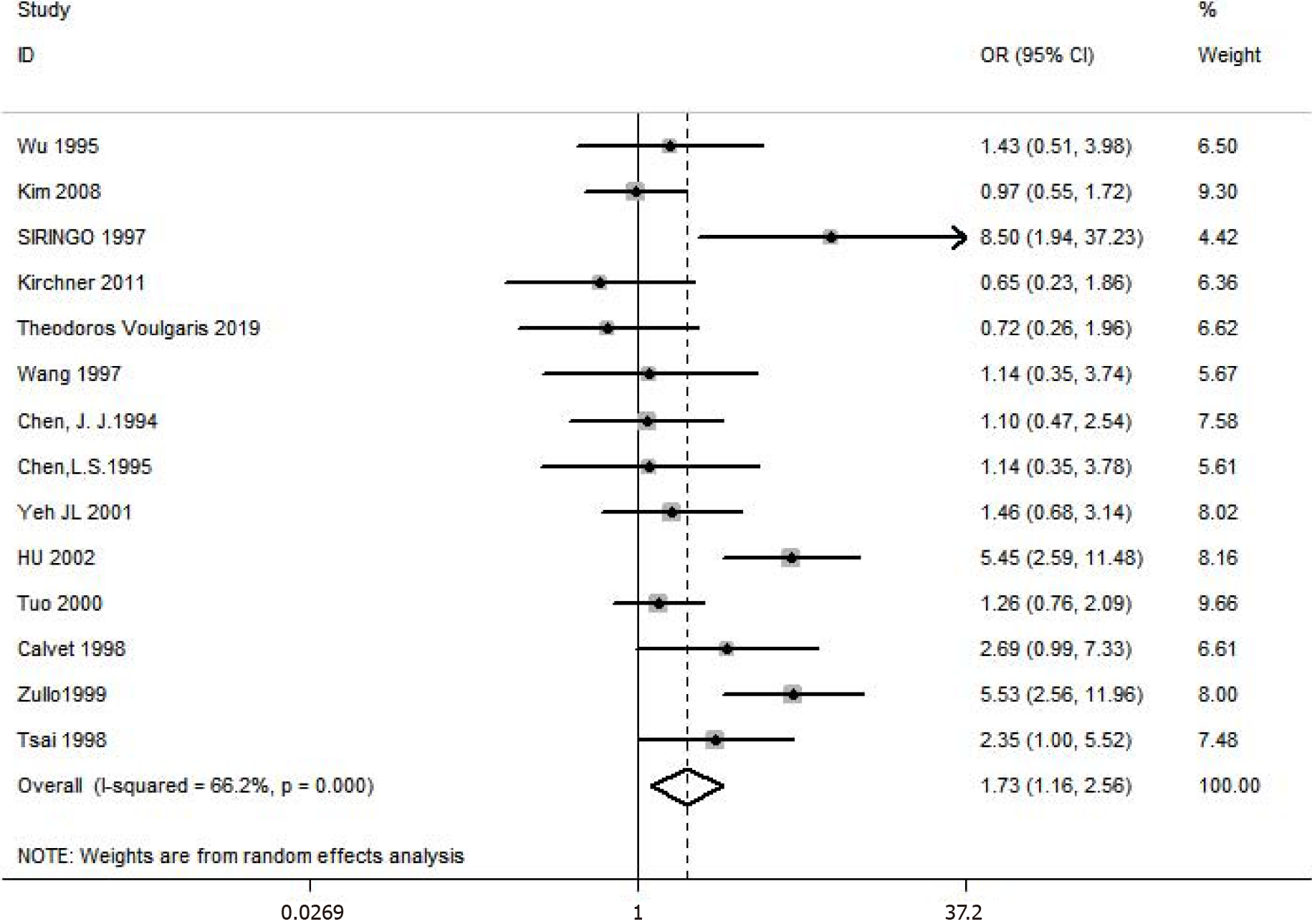
The prevalence of PU in patients with cirrhosis was 22%. The prevalence of H. pylori infection in cirrhotic patients with PU was 65.6%, and the prevalence in those without PU was 52.5%. Figure 3 shows the forest plot and pooled estimates of H. pylori infection for cirrhotic patients with and without PU in the 14 studies (involving 2775 middle-aged individuals, 611 cases with PU, and 2164 controls). The pooled overall OR was 1.73 (95%CI: 1.16-2.56, I2 = 66.2%, P < 0.005, Z = 2.7 Pz < 0.05). This result suggests that patients with H. pylori infection were 1.73 times more likely to develop PU than those without.
Given the heterogeneity in the results, we carried out subgroup analyses and meta-regression of the studies according to the publication year, location, diagnosis of H. pyloriinfection, sample size, case/control ratio, diagnosis of H. pylori infection, diagnosis of liver cirrhosis, and language. Unfortunately, we did not find the cause of the heterogeneity in the subgroup analyses and meta-regression analysis. The results of the subgroup and meta-regression analyses are shown in Table 2. Notably, the prevalence of H. pylori infection in cirrhotic patients with and without PU was consistent in most subgroups examined.
| Subcategory | Random-effects model | Meta-regression | |||||
| n | OR (95%CI) | P value | I2 | Ajusted-R2 | P value | χ2 | |
| Year | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | 4.64% | 0.241 | 33.29% |
| Before 2000 | 8 | 2.19 (1.31-3.67) | 0.039 | 52.60% | |||
| After 2000 (2000) | 6 | 1.34 (0.75-2.38) | 0.02 | 73.50% | |||
| Area | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -5.48% | 0.467 | 36.82% |
| Asia | 9 | 2.19 (0.81-5.97) | 0.001 | 79.0% | |||
| Europe | 5 | 1.67 (0.56-4.97) | 0.09 | 74% | |||
| Study type | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -14.28% | 0.817 | 39.89% |
| Cross-sectional study | 13 | 1.75 (1.14-2.70) | < 0.01 | 68.7% | |||
| Cohort study | 1 | 1.46 (0.68-3.14) | |||||
| Diagnosis of Hp | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -13.83% | 0.935 | 39.73% |
| ELISA | 4 | 1.52 (0.62-3.74) | 0.036 | 64.80% | |||
| Multiple | 8 | 1.95 (1.12-3.39) | 0.003 | 75.30% | |||
| RUT | 1 | 1.14 (0.35-3.78) | |||||
| UBT | 1 | 1.46 (0.68-3.14) | |||||
| Diagnosis of liver cirrhosis | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -11.75% | 0.817 | 39.01% |
| Ultrasound | 1 | 1.43 (0.51-3.98) | |||||
| Multiple | 13 | 1.75 (1.15-2.67) | < 0.01 | 68.70% | |||
| Case/control ratio | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -14.36% | 0.787 | 39.92% |
| ≥ 0.3 | 9 | 1.80 (1.11-2.90) | 0.009 | 60.60% | |||
| < 0.3 | 5 | 1.59 (0.73-3.47) | 0.001 | 77.90% | |||
| Sample size | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | 5.11% | 0.24 | 33.12% |
| ≥ 100 | 12 | 1.89 (1.23-2.91) | < 0.01 | 68.70% | |||
| < 100 | 2 | 0.87 (0.40-1.88) | 0.5611 | ||||
| Language | 14 | 1.73 (1.16-2.56) | < 0.01 | 66.20% | -7.60% | 0.439 | 37.56% |
| English | 12 | 1.59 (1.05-2.42) | 0.005 | 58.7% | |||
| Chinese | 2 | 2.55 (0.58-11.14) | 0.001 | 90.6% | |||
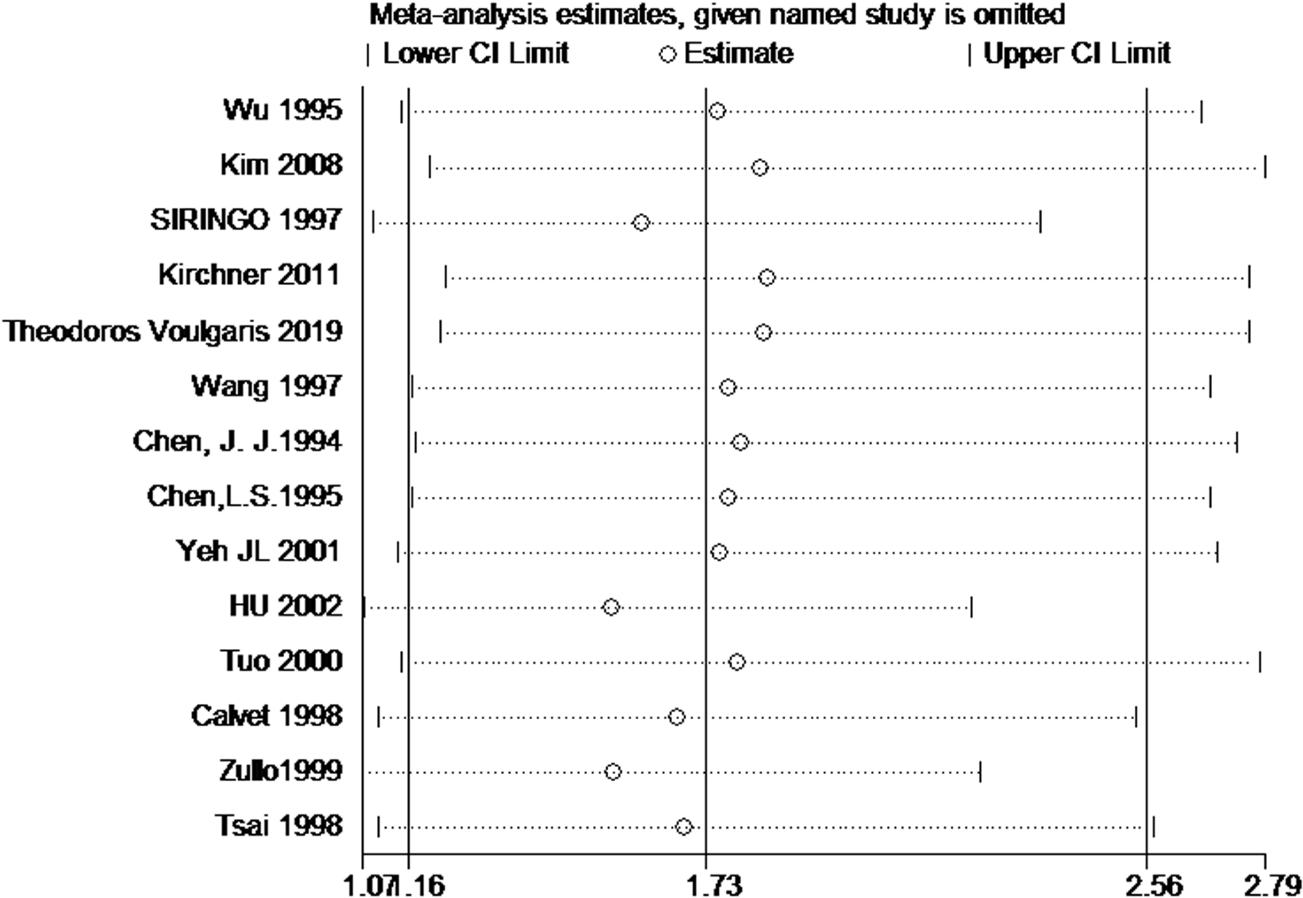
We performed a sensitivity analysis using the one-study removed (leave-one-out) approach to examine the influence of each study on the overall effect size. As shown in Figure 4, through sensitivity analysis, we found one study may be the source of the statistical heterogeneity. The pooled I2 was 56%, and the OR was 1.55 (95%CI: 1.07-2.23, I2 = 56%, P = 0.007, Z = 2.35, Pz = 0.02).
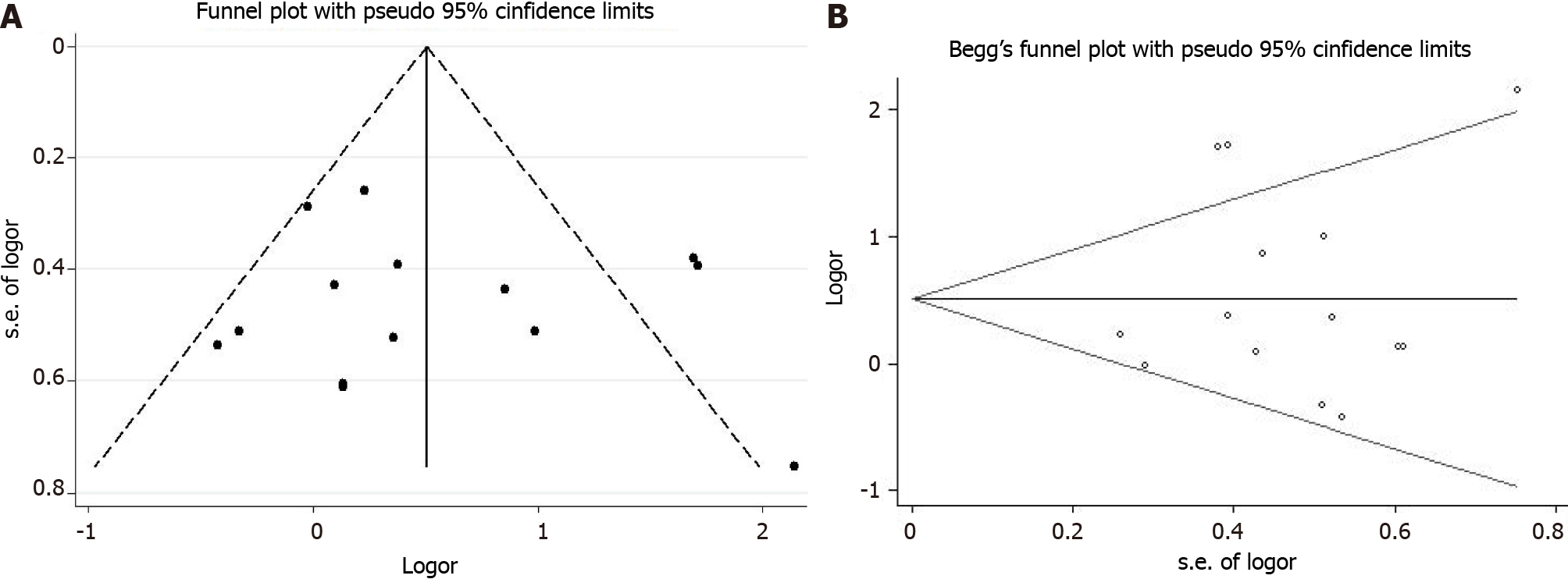
We used a funnel plot to qualitatively detect publication bias, and Egger’s and Begg’s tests were used to quantify publication bias. The funnel plots were almost symmetric (Figure 5A). The results of Begg’s test and Egger’s test indicated no evidence of substantial publication bias (PBegg = 0.732, PEgger = 0.557) and are shown in Figure 5B.
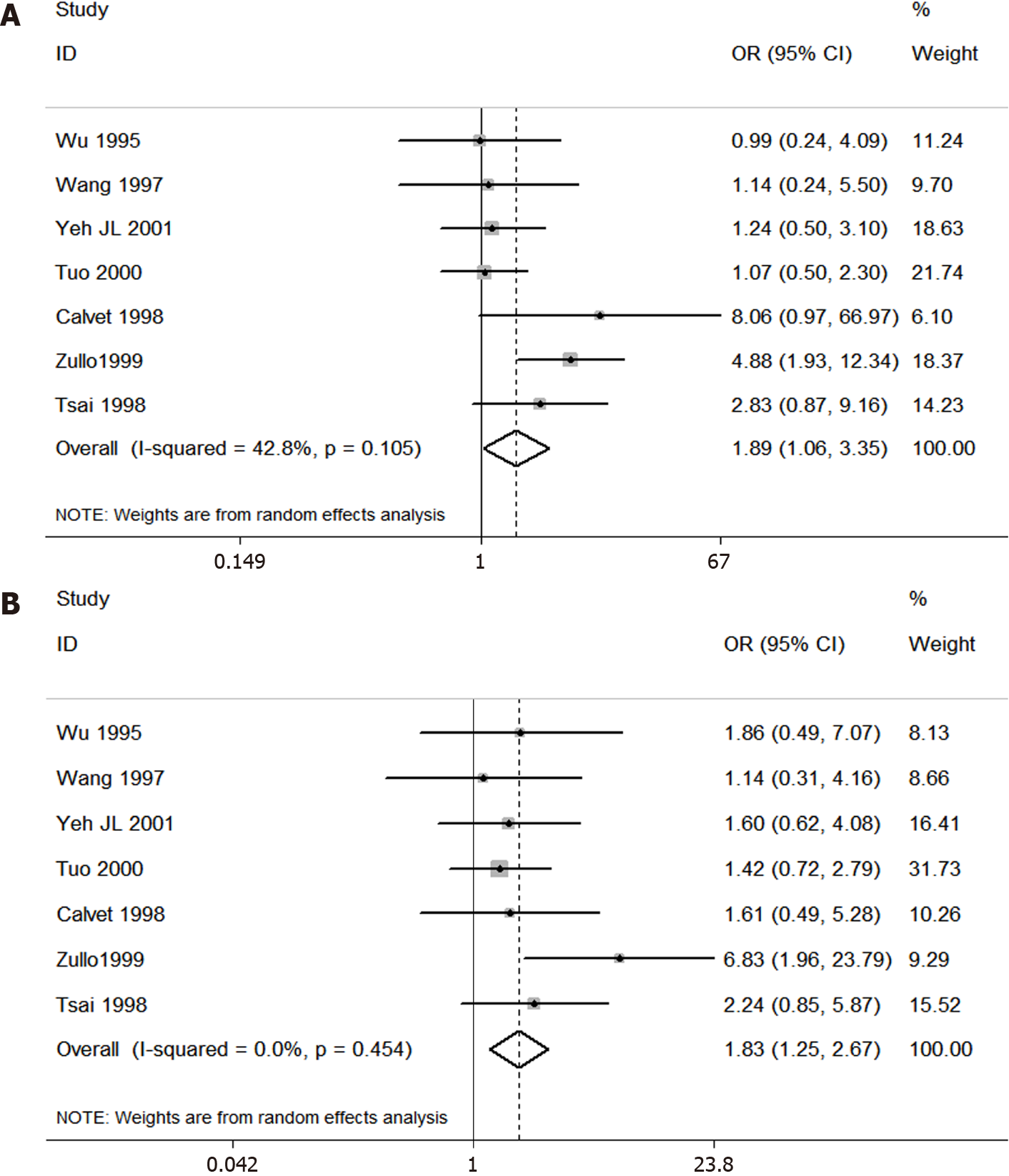
We also performed two other analyses of H. pylori infection in cirrhotic patients with and without duodenal or gastric ulcer diseases. The results showed that H. pylori was essentially equally associated with duodenal and gastric ulcer in cirrhotic patients. Figure 6 shows that the OR was 1.83 (95%CI: 1.25-2.67, I2 = 0.0%, P = 0.454, Z = 3.11, Pz = 0.002) for duodenal ulcer and 1.89 (95%CI: 1.06-3.35, I2 = 42.8%, P = 0.105, Z = 2.16, Pz = 0.031) for gastric ulcer. These two results are basically consistent with the previous results of liver cirrhosis with PU.
The exact mechanism underlying the association between H. pylori infection and PU in patients with liver cirrhosis has not been fully elucidated. At present, there are some hypotheses. Since the PU prevalence is considerably higher in liver cirrhosis patients than in the general population, it is reasonable to postulate that there are “ulcerogenic mechanisms” specific to cirrhotic patients which may cause PU in the absence of H. pylori infection and which could additionally increase the ulcerogenic effects of H. pylori infection. Several possible ulcerogenic mechanisms have been suggested in cirrhotic patients: A decrease in gastric prostaglandin E2 levels, hypergastrinemia, portosystemic shunting allowing the ulcerogenic factors to escape hepatic clearance, and an impairment of gastric mucosal defense secondary to portal hypertension and congestive gastropathy which may make the mucosa more susceptible to damage from other agents or reduce its capacity to repair damage[25-31]. Taken together, the pathogenic mechanisms of PU in cirrhotic patients seems to be a multifactorial event, which may increase the ulcerogenic effects of H. pylori infection.
Our meta-analysis included 14 studies, of which 9 showed that there was no significant difference in the incidence of H. pylori infection in cirrhotic patients with or without PU[10-13,15-18,21]. The other five studies showed that H. pylori infection was positively or weakly correlated with PU in liver cirrhosis[5,9,14,19,20]. The results of the 14 studies showed that the incidence of liver cirrhosis complicated with PU was 22%, and the H. pylori infection rate of patients with liver cirrhosis complicated with PU was 65.6%. This study found that there was a weakly positive correlation between H. pylori infection and PU in patients with liver cirrhosis. In other words, H. pylori infection may be a reason why patients with liver cirrhosis are more likely to develop PU than the general population, and H. pylori may be one of the factors causing PU. However, because of the weak correlation and data from retrospective studies, more prospective studies are needed to evaluate the incidence of H. pylori infection in patients with liver cirrhosis complicated with PU in the future.
In 2002, Vergara et al[3] published a meta-analysis of the relationship between H. pylori infection and PU in patients with liver cirrhosis. The meta-analysis included seven studies, four of which suggested that H. pylori infection did not increase the risk of PU in liver cirrhosis, while three others suggested a positive or weak correlation[3]. That meta-analysis suggested that H. pylori infection increases the risk of PU in patients with liver cirrhosis. The OR was 2.70 (95%CI: 1.91–3.82), which is consistent with our collective results. And the meta-analysis of Vergara et al[3] showed that the relationship between H. pylori infection and PU in patients with liver cirrhosis does not seem to be as intense as in the general population. The reason may be that in most studies, H. pylori infection is diagnosed by serology. Although serology is the pre
Our meta-analysis has some limitations. First and foremost, only the study of Voulgaris et al[16] had a prospective design, and most of original studies are retro
Therefore, the relationship between H. pylori infection and PU in patients with liver cirrhosis is of great clinical significance. Future prospective studies and reliable clinical trial designs are of great importance to determine whether H. pylori is an independent risk factor for PU in liver cirrhosis. If studies can prove that H. pylori is also an independent risk factor for PU in patients with liver cirrhosis, the eradication of H. pylori can indirectly prevent bleeding in patients with liver cirrhosis complicated with PU. Therefore, it is very important for cirrhotic patients that also have H. pylori infection to eradicate H. pylori in advance. In addition, microbiome is booming, especially intestinal microbiome, and many studies describe the role of bacterial microbiome in H. pylori-associated diseases. Whether bacterial microbiome can be applied to cirrhotic patients with PU is a subject worth studying[32].
There is a weakly positive association between H. pylori infection and PU in patients with cirrhosis. It is suggested that H. pylori infection may increase the PU risk and play a role in the pathogenesis of PU in patients with cirrhosis. In the future, prospective studies and reliable experimental designs should be used to determine if H. pylori is an independent risk factor for PU in liver cirrhotic patients. If this link is confirmed in the near future, the eradication of H. pylori may become a new specific strategy to prevent PU bleeding.
Peptic ulcer (PU) is more prevalent in patients with liver cirrhosis than in the general population. What’s more, cirrhotic patients with PU have a significantly higher risk of PU bleeding than the general population. The role of Helicobacter pylori (H. pylori) infection in the pathogenesis of PU in patients with cirrhosis is still not elucidated.
Why cirrhotic patients have a higher risk of peptic ulcer? Whether this is related to H. pylori infection? If studies can prove that H. pylori is also an independent risk factor for PU in patients with liver cirrhosis, eradication of H. pylori can indirectly prevent PU bleeding in cirrhotic patients. With these doubts and questions, we performed this meta-analysis.
To perform a meta-analysis on the prevalence of H. pylori infection and PU and their association in liver cirrhosis patients.
We searched PubMed, EMBASE, Web of Science, Cochrane, CNKI, Wangfang, and CQVIP databases from inception to July 10, 2020. Odds ratio (OR) and 95% confidence interval (CI) were pooled with a random-effects model. The statistical heterogeneity among studies (I2-index), subgroup analyses, regression analysis, sensitivity analysis, and the possibility of publication bias were assessed.
The prevalence of PU in patients with cirrhosis was 22%. The prevalence of H. pylori infection was 65.6% in cirrhotic patients with PU, and 52.5% in those without. The pooled overall OR was 1.73 (95%CI: 1.16-2.56, I2 = 66.2%, P < 0.001, Z = 2.7, Pz < 0.05). We did not find the cause of heterogeneity in the subgroup analyses and meta-regression analysis. We found that one study may be the source of the statistical heterogeneity through sensitivity analysis.
There is a weakly positive association between H. pylori infection and PU in patients with liver cirrhosis.
Prospective studies and reliable experimental designs should be further used to determine if H. pylori is an independent risk factor for PU in liver cirrhotic patients. If this link is confirmed in the near future, the eradication of H. pylori may become a new specific strategy to prevent non-variceal bleeding, especially PU hemorrhage in cirrhotic patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cho JH, Dahiya DS, Pichon M, Sezgin O S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Yuan YY
| 1. | Chen LS, Lin HC, Hwang SJ, Lee FY, Hou MC, Lee SD. Prevalence of gastric ulcer in cirrhotic patients and its relation to portal hypertension. J Gastroenterol Hepatol. 1996;11:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Siringo S, Burroughs AK, Bolondi L, Muia A, Di Febo G, Miglioli M, Cavalli G, Barbara L. Peptic ulcer and its course in cirrhosis: an endoscopic and clinical prospective study. J Hepatol. 1995;22:633-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Vergara M, Calvet X, Roqué M. Helicobacter pylori is a risk factor for peptic ulcer disease in cirrhotic patients. A meta-analysis. Eur J Gastroenterol Hepatol. 2002;14:717-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Lo GH, Yu HC, Chan YC, Chen WC, Hsu PI, Lin CK, Lai KH. The effects of eradication of Helicobacter pylori on the recurrence of duodenal ulcers in patients with cirrhosis. Gastrointest Endosc. 2005;62:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Tsai CJ. Helicobacter pylori infection and peptic ulcer disease in cirrhosis. Dig Dis Sci. 1998;43:1219-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Luo JC, Leu HB, Hou MC, Huang CC, Lin HC, Lee FY, Chang FY, Chan WL, Lin SJ, Chen JW. Cirrhotic patients at increased risk of peptic ulcer bleeding: a nationwide population-based cohort study. Aliment Pharmacol Ther. 2012;36:542-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Leontiadis GI, Molloy-Bland M, Moayyedi P, Howden CW. Effect of comorbidity on mortality in patients with peptic ulcer bleeding: systematic review and meta-analysis. Am J Gastroenterol. 2013;108:331-345; quiz 346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (37)] |
| 8. | Marmo R, Koch M, Cipolletta L, Capurso L, Pera A, Bianco MA, Rocca R, Dezi A, Fasoli R, Brunati S, Lorenzini I, Germani U, Di Matteo G, Giorgio P, Imperiali G, Minoli G, Barberani F, Boschetto S, Martorano M, Gatto G, Amuso M, Pastorelli A, Torre ES, Triossi O, Buzzi A, Cestari R, Della Casa D, Proietti M, Tanzilli A, Aragona G, Giangregorio F, Allegretta L, Tronci S, Michetti P, Romagnoli P, Nucci A, Rogai F, Piubello W, Tebaldi M, Bonfante F, Casadei A, Cortini C, Chiozzini G, Girardi L, Leoci C, Bagnalasta G, Segato S, Chianese G, Salvagnini M, Rotondano G. Predictive factors of mortality from nonvariceal upper gastrointestinal hemorrhage: a multicenter study. Am J Gastroenterol. 2008;103:1639-1647; quiz 1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Zullo A, Rinaldi V, Meddi P, Folino S, Lauria V, Diana F, Winn S, Attili AF. Helicobacter pylori infection in dyspeptic cirrhotic patients. Hepatogastroenterology. 1999;46:395-400. [PubMed] |
| 10. | Kirchner GI, Beil W, Bleck JS, Manns MP, Wagner S. Prevalence of Helicobacter pylori and occurrence of gastroduodenal lesions in patients with liver cirrhosis. Int J Clin Exp Med. 2011;4:26-31. [PubMed] |
| 11. | Wu CS, Lin CY, Liaw YF. Helicobacter pylori in cirrhotic patients with peptic ulcer disease: a prospective, case controlled study. Gastrointest Endosc. 1995;42:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Siringo S, Vaira D, Menegatti M, Piscaglia F, Sofia S, Gaetani M, Miglioli M, Corinaldesi R, Bolondi L. High prevalence of Helicobacter pylori in liver cirrhosis: relationship with clinical and endoscopic features and the risk of peptic ulcer. Dig Dis Sci. 1997;42:2024-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Kim DJ, Kim HY, Kim SJ, Hahn TH, Jang MK, Baik GH, Kim JB, Park SH, Lee MS, Park CK. Helicobacter pylori infection and peptic ulcer disease in patients with liver cirrhosis. Korean J Intern Med. 2008;23:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Calvet X, Navarro M, Gil M, Lafont A, Sanfeliu I, Brullet E, Campo R, Dalmau B, Rivero E, Mas P. Epidemiology of peptic ulcer disease in cirrhotic patients: role of Helicobacter pylori infection. Am J Gastroenterol. 1998;93:2501-2507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Wang CH, Ma LR, Lin RC, Kuo JY, Chang KK. Helicobacter pylori infection and risk of peptic ulcer among cirrhotic patients. J Formos Med Assoc. 1997;96:55-58. [PubMed] |
| 16. | Voulgaris T, Karagiannakis D, Siakavellas S, Kalogera D, Angelopoulos T, Chloupi E, Karamanolis G, Papatheodoridis G, Vlachogiannakos J. High prevalence of asymptomatic peptic ulcers diagnosed during screening endoscopy in patients with cirrhosis. Ann Gastroenterol. 2019;32:451-456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Chen JJ, Changchien CS, Tai DI, Chiou SS, Lee CM, Kuo CH. Role of Helicobacter pylori in cirrhotic patients with peptic ulcer. A serological study. Dig Dis Sci. 1994;39:1565-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Chen LS, Lin HC, Lee FY, Hou MC, Lee SD. Prevalence of duodenal ulcer in cirrhotic patients and its relation to Helicobacter pylori and portal hypertension. Zhonghua Yi Xue Za Zhi (Taipei). 1995;56:226-231. [PubMed] |
| 19. | Yeh JL, Peng YC, Tung CF, Chen GH, Chow WK, Chang CS, Yeh HZ, Poon SK. Role of Helicobacter pylori in cirrhotic patients with dyspepsia: a 13C-urea breath test study. Adv Ther. 2001;18:140-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Hu ZW, Guo JW, Luo J. Study on Helicobacter pylori infection in patients with liver cirrhosis. Zhonghua Xiaohua Neijing Zazhi. 2002;19:349-350. [DOI] [Full Text] |
| 21. | Tuo BG, Yu AY, Zhou DS, Zhao K, Wen XQ. Association between Helicobacter pylori and peptic ulcer with liver cirrhosis. Zhonghua Neike Zazhi. 2000;39:44-45. |
| 22. | Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2016;354:i4086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 23. | Pede S, Uguccioni M. [AHCPR/AHRQ guidelines. Agency for Health Care Policy and Research and Agency for Health Care Research and Quality]. Ital Heart J. 2001;2 Suppl 1:60-68. [PubMed] |
| 24. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46435] [Article Influence: 2110.7] [Reference Citation Analysis (3)] |
| 25. | Arakawa T, Satoh H, Fukuda T, Nakamura H, Kobayashi K. Endogenous prostaglandin E2 in gastric mucosa of patients with alcoholic cirrhosis and portal hypertension. Gastroenterology. 1987;93:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Samloff IM. Multiple gastric red spots, capillary ectasia, hypergastrinemia and hypopepsinogenemia I in cirrhosis: a new syndrome? Hepatology. 1988;8:699-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Guslandi M, Foppa L, Sorghi M, Pellegrini A, Fanti L, Tittobello A. Breakdown of mucosal defences in congestive gastropathy in cirrhotics. Liver. 1992;12:303-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Balan KK, Jones AT, Roberts NB, Pearson JP, Critchley M, Jenkins SA. The effects of Helicobacter pylori colonization on gastric function and the incidence of portal hypertensive gastropathy in patients with cirrhosis of the liver. Am J Gastroenterol. 1996;91:1400-1406. [PubMed] |
| 29. | Perini RF, Camara PR, Ferraz JG. Pathogenesis of portal hypertensive gastropathy: translating basic research into clinical practice. Nat Clin Pract Gastroenterol Hepatol. 2009;6:150-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Batmanabane V, Kate V, Ananthakrishnan N. Prevalence of Helicobacter pylori in patients with portal hypertensive gastropathy--a study from south India. Med Sci Monit. 2004;10:CR133-CR136. [PubMed] |
| 31. | Bahnacy A, Kupcsulik P, Elés ZS, Jàray B, Flautner L. Helicobacter pylori and congestive gastropathy. Z Gastroenterol. 1997;35:109-112. [PubMed] |
| 32. | Pichon M, Burucoa C. Impact of the Gastro-Intestinal Bacterial Microbiome on Helicobacter-Associated Diseases. Healthcare (Basel). 2019;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |