Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.463
Peer-review started: August 24, 2020
First decision: November 3, 2020
Revised: November 16, 2020
Accepted: November 29, 2020
Article in press: November 29, 2020
Published online: January 16, 2021
Processing time: 134 Days and 2.7 Hours
Sinistral portal hypertension associated with pancreatic pseudocysts is rare, often caused by extrinsic compression of splenic vein, the follow-up examinations by ultrasonography for early diagnosis are quietly necessary since haematemesis, a life-threatening condition. Few studies have reported the ultrasonography findings of sinistral portal hypertension.
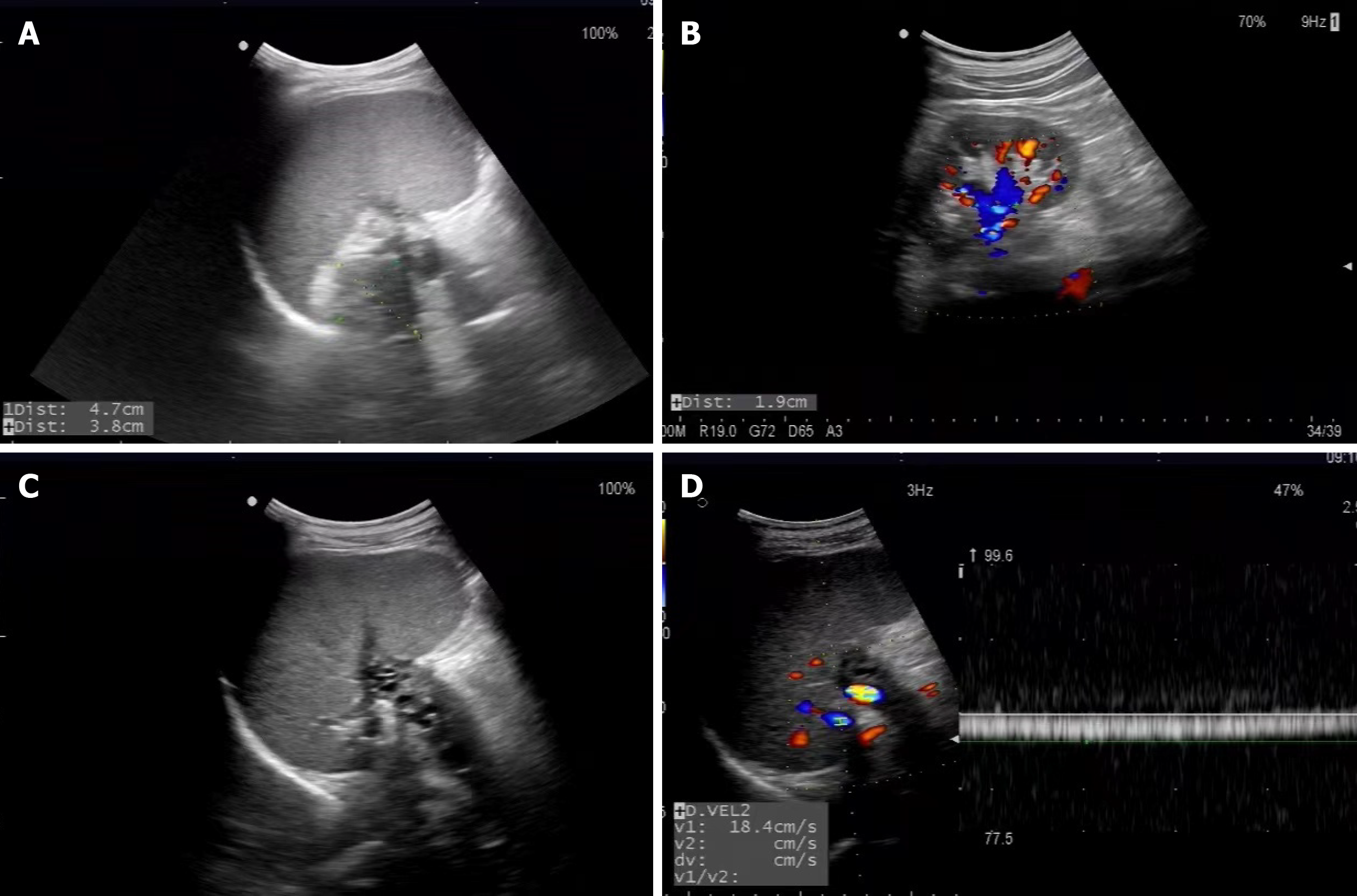
A 52-year-old man presented with acute abdominal pain after drinking, steatorrhea, weight loss and accidentally melena in the past 2 mo. He underwent ultrasound-guided fine needle aspiration in other hospital and diagnosed with pancreatic pseudocysts. Ultrasonography imaging, in our department, appeared as cystic heterogeneous hypoechoic area with the size of 4.7 cm × 3.8 cm that located posterior to the body and tail of pancreas, adjacent to splenic vein associated with thrombosis resulted from compression. Spleen incrassated to approximately 7.3 cm, but no dilation of main portal vein was presented. Color Doppler Flow Imaging demonstrated the formation of splenic venous collateral, nevertheless no significantly flow signals was observed in splenic vein. Pulsed Doppler revealed that the peak velocity of splenic venous collateral was 18.4 cm/s with continuous waveform. Laparotomy confirmed sinistral portal hypertension associated with pancreatic pseudocysts, subsequently distal pancreatectomy combined with splenectomy and partial gastrectomy was performed.
It’s important clinically to know the ultrasound appearance of sinistral portal hypertension associated with pancreatic pseudocysts for sonographer and physician.
Core Tip: Sinistral portal hypertension associated with pancreatic pseudocysts is rare, caused by compression of splenic vein, the follow-up examinations by ultrasonography for early diagnosis are quietly necessary since haematemesis, a life-threatening condition, which highlights the significance of ultrasonography imaging.
- Citation: Chen BB, Mu PY, Lu JT, Wang G, Zhang R, Huang DD, Shen DH, Jiang TT. Sinistral portal hypertension associated with pancreatic pseudocysts - ultrasonography findings: A case report. World J Clin Cases 2021; 9(2): 463-468
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/463.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.463
Sinistral portal hypertension or left-sided portal hypertension is a rare disease with normal liver function[1-3], less than 1% in the study of Kokabi et al[4], occurring often as a result of isolated obstruction of the splenic vein of which pancreatic diseases are the most commonly etiology. Delineated in previously literatures, the incidence of pancreatic pseudocysts, one of the complications of acute pancreatitis, was reported to be between 5%-16%, especially highly in patients with alcoholic etiology and fluid collection at 3 mo after discharge[5]. As a consequence, these patients should be proposed to undergo follow-up examinations by ultrasonography to timely monitor the formation of pancreatic pseudocysts[6]. However, the ultrasound appearance of compression of splenic vein is easy to be ignored by sonographer, which often results in the misdiagnosis of the sinistral portal hypertension associated with pancreatic pseudocysts. It’s determined that the ultrasonography imaging of the sinistral portal hypertension is necessary, because the complications of the sinistral portal hypertension remain mostly severe, some of which include gastric varices, upper gastrointestinal hemorrhage as well as “Nutcracker Syndrome” - left renal vein entrapment syndrome.
Herein, we report a case of sinistral portal hypertension associated with pancreatic pseudocysts, which presented with abdominal pain, accidentally melena, steatorrhea and loss of weight. Distal pancreatectomy combined with splenectomy and partial gastrectomy were performed.
On May 21, 2020, a 52-year-old man presented with acute abdominal pain after drinking, accidentally melena in the past 2 mo and weight loss.
The patient presented with acute abdominal pain, accidentally melena, steatorrhea and weight loss. He underwent ultrasound-guided fine needle aspiration in other hospital and then diagnosed with pancreatic pseudocysts.
He denied history of hepatitis virus infection, drug-induced liver injury, or autoimmune liver disease.
He denied any personal or family history.
No distinctly abnormal indicators were observed by a round of physical examinations.
At admission, laboratory examination showed that hemoglobin was 80 g/L, red blood cell count was 2.63 × 1012/L (reference range: 4.09-5.74 × 1012/L), serum total bile acid was 36.9 μmol/L (reference range: 0-15 μmol/L), total cholesterol was 5.57 mmol/L (reference range: < 5.2 mmol/L), and triglycerides was 1.87 mmol/L (reference range: < 1.7 mmol/L). Other biochemical indices revealed no obviously abnormalities.
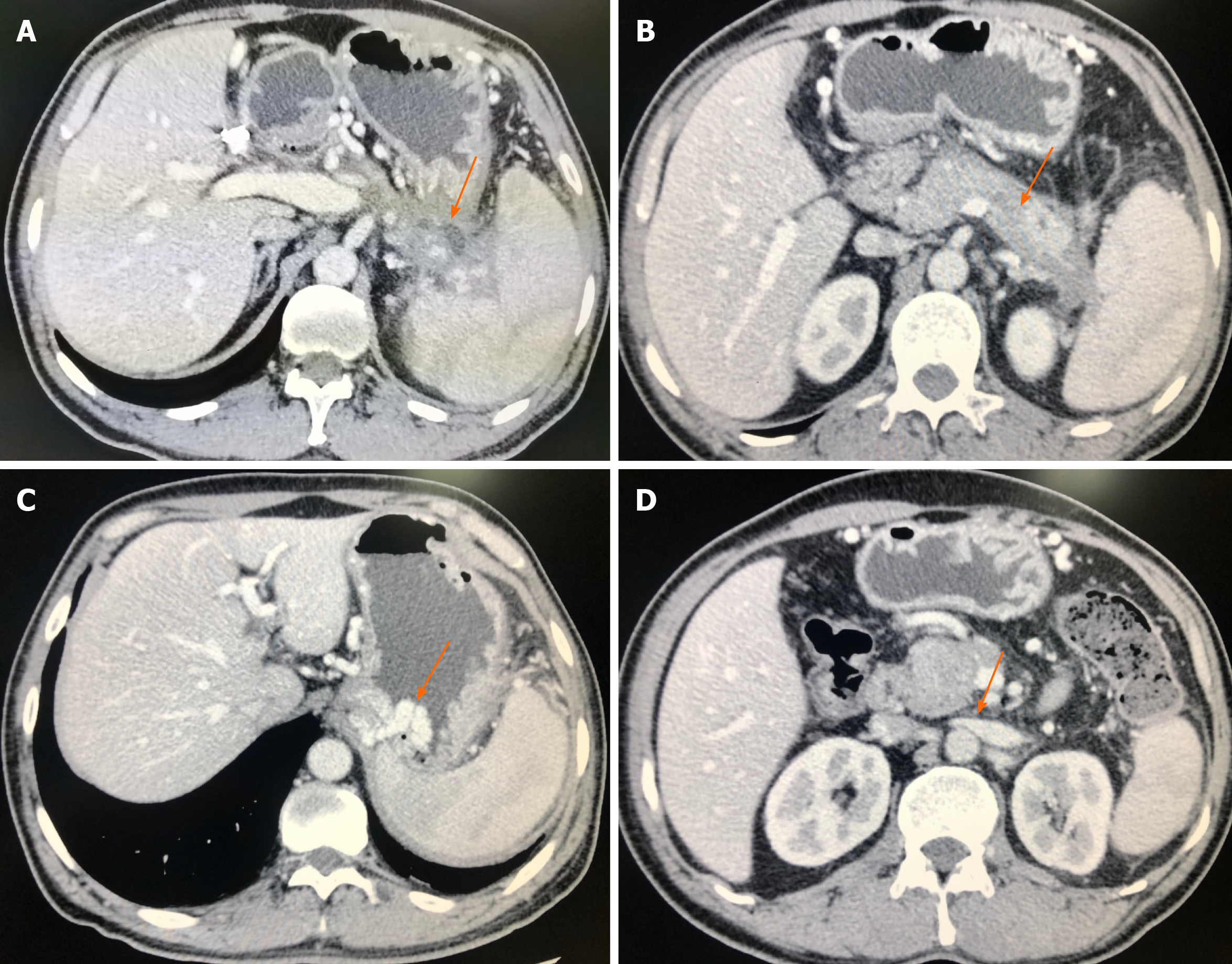
On May 29, 2020, the patient underwent ultrasonography scan, which appeared as pancreatic pseudocysts with the cystic heterogeneous hypoechoic area, the size of which was 4.7 cm × 3.8 cm. The pseudocysts located posterior to the body and tail of pancreas, and adjacent to splenic vein associated with thrombosis resulted from compression (Figure 1A). Spleen incrassated to approximately 7.3 cm but no dilation of main portal vein was presented. Color Doppler Flow Imaging (CDFI) demonstrated the formation of splenic venous collateral, nevertheless no significantly flow signals in splenic vein and the wall of pancreatic pseudocysts were observed. Pulsed Doppler (PW) revealed that the peak velocity of splenic venous collateral was 18.4 cm/s with continuous waveform (Figure 1D). Contrast-enhanced computed tomography (CT) scan suggested the formation of pancreatic pseudocysts (Figure 2A), irregular filling-defect in splenic vein (Figure 2B), the development of gastric varices (Figure 2C), and splenomegaly. Ultrasonography imaging was consistent with CT imaging in this case of sinistral portal hypertension associated with pancreatic pseudocysts.
Diagnosis of sinistral portal hypertension associated with pancreatic pseudocysts was finally confirmed by laparotomy and pathology.
He had accepted conservative treatment in other hospitals. After admitted to our hospital, he accepted distal pancreatectomy combined with splenectomy and partial gastrectomy. He recovered quickly and discharged 25 d later.
Approximately 3 mo after surgery, the patient was followed up, which manifested stable condition, according to what the doctor ordered.
Sinistral portal hypertension associated with pancreatic pseudocysts, although rare, can be prevented and managed depending on ultrasonography images to provide follow-up diagnosis in time. Hence, the complications of sinistral portal hypertension, gastric varices and upper gastrointestinal hemorrhage, can be detained[7]. CDFI and PW can indicate the flow pattern and calculate the velocity of blood flow separately, and PW analysis of variceal blood flow shows a continuous wave[8]. In this case, PW presented that the peak velocity of splenic venous collateral was 18.4 cm/s with continuous waveform, nevertheless no significantly flow signals were observed by CDFI in splenic vein. Splenic venous thrombus in this case were showed as solid hypoechoic filling in the cavity of splenic vein (Figure 1C), resulting in enlargement of splenic (approximately 7.3 cm in thickness).
Splenic vein thrombus results in back pressure with short gastric, gastroepiploic veins, the middle colonic vein, and the superior right colonic vein, all of them eventually fail to drain into the portal vein, which lead to the reversal of flow in these veins and the formation of varices[9-12]. Indeed, not only do patients with splenic vein occlusion not develop varices, but this process often needs a relatively long interval of time to become clinically evident[7]. Therefore, the blood supplying to gastrointestinal must be affected in this setting, which occurring variously acute or chronic gastrointestinal diseases associated with sinistral portal hypertension, just like our case, upper gastrointestinal hemorrhage, abdominal pain, steatorrhea and loss of weight owing to varices and malnutrition in the long run. We infer from above that poor blood supply of gastric mucosa accelerates the formation of gastrohelcosis.
CDFI can confirm the communication between the splenic vein and the left renal vein when thrombosis is observed in splenic vein, which is associated with lower spleen volume ratios and lesser rate of varices formation on long-term follow-up[13-15]. The diameter of splenic vein becomes larger as the long-term existence of splenorenal shunt, hence superior mesenteric artery is likely to prevent more blood in renal vein flowing towards ventral aorta, which causes renal venous congestion (Figure 1B), so that the relevant urinary symptoms deriving from left renal vein entrapment syndrome, also known as “Nutcracker Syndrome” may develop (Figure 2D).
In patients with pancreatic pseudocysts, the investigators should carefully seek thrombus in splenic vein. Compared with other radiological findings, ultrasonographic imaging is clearer to indicate varices if the splenic vein is only partially thrombosed[15]. The pattern and velocity of blood flow and complications are all clearly demonstrable by ultrasonographic imaging, and it is inexpensive, convenient, quick, safe and, we think, has the flexibility to examine pathology in a variety of anatomical planes[15,16]. Surgical findings in this case shown dilated and tortuous veins in the surrounding of omentum, mesentery, stomach, normal liver, an arched protrusion on the upper margin of the pancreas. Brown fluid overflow was observed after the incision of protrusion, which confirmed the presence of pancreatic pseudocysts. The pancreas and the posterior wall of stomach were too closely related to separate, therefore partial gastrectomy was performed meanwhile. Fast frozen pathology of resected pancreatic specimen also proved pancreatic pseudocysts. Final diagnosis was confirmed to be sinistral portal hypertension associated with pancreatic pseudocysts in light of above findings.
The critical imperfection of our study was the short of spleen elastography, which could have helped in the diagnosis of sinistral portal hypertension. Considering spleen vein was oppressed by pancreatic pseudocysts, disorder of blood flow in the splenic vein may lead to spleen congestion, which increased its stiffness[17]. Other authors had said that spleen stiffness may serve as a surrogate for the dynamic component of esophageal varices, which pointed out that spleen stiffness has been considered markers of esophageal varices, life-threatening upper gastrointestinal bleeding[18-20]. In short, sonographers should pay another attention to the stiffness of spleen when sinistral portal hypertension was diagnosed.
Ultrasonographic imaging is the most valuable modality for the timely diagnosis of sinistral portal hypertension associated with the pancreatic pseudocysts and allows the prediction of the risk for upper gastrointestinal hemorrhage. Clinicians and sonographers should pay more attention to ultrasonographic imaging of splenic vein, if pancreatic pseudocysts exist, so that the life-threatening complications of sinistral portal hypertension associated with pancreatic pseudocysts could be found in time.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giuffrè M S-Editor: Huang P L-Editor: Filipodia P-Editor: Li JH
| 1. | Kul M, Haliloğlu NÜ, Hürsoy N, Erden A. Sinistral Portal Hypertension: Computed Tomography Imaging Findings and Clinical Appearance-A Descriptive Case Series. Can Assoc Radiol J. 2018;69:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Tzeng YD, Liu SI, Tsai CC. An unusual cause of haematemesis: left-sided portal hypertension due to a large pancreatic tumour. Dig Liver Dis. 2012;44:e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Li T, Hu SY, Zhi XT. Education and Imaging: gastrointestinal: segmental portal hypertension caused by pancreatic mucinous cystadenoma. J Gastroenterol Hepatol. 2014;29:1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Kokabi N, Lee E, Echevarria C, Loh C, Kee S. Sinistral portal hypertension: presentation, radiological findings, and treatment options - a case report. J Radiol Case Rep. 2010;4:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Rasch S, Nötzel B, Phillip V, Lahmer T, Schmid RM, Algül H. Management of pancreatic pseudocysts-A retrospective analysis. PLoS One. 2017;12:e0184374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Lankisch PG, Weber-Dany B, Maisonneuve P, Lowenfels AB. Pancreatic pseudocysts: prognostic factors for their development and their spontaneous resolution in the setting of acute pancreatitis. Pancreatology. 2012;12:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Petrucciani N, Debs T, Rosso E, Addeo P, Antolino L, Magistri P, Gugenheim J, Ben Amor I, Aurello P, D'Angelo F, Nigri G, Di Benedetto F, Iannelli A, Ramacciato G. Left-sided portal hypertension after pancreatoduodenectomy with resection of the portal/superior mesenteric vein confluence. Results of a systematic review. Surgery. 2020;168:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 8. | Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Akaike J. Observation of gastric variceal flow characteristics by endoscopic ultrasonography using color Doppler. Am J Gastroenterol. 2008;103:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Cakmak O, Parildar M, Oran I, Sever A, Memis A. Sinistral portal hypertension; imaging findings and endovascular therapy. Abdom Imaging. 2005;30:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Mizuno S, Kato H, Yamaue H, Fujii T, Satoi S, Saiura A, Murakami Y, Sho M, Yamamoto M, Isaji S. Left-sided Portal Hypertension After Pancreaticoduodenectomy With Resection of the Portal Vein/Superior Mesenteric Vein Confluence in Patients With Pancreatic Cancer: A Project Study by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. Ann Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Canbak T, Acar A, Kıvanç AE, Başak F, Kulalı F, Baş G. Sinistral Portal Hypertension Due to Pancreatic Hydatid Cyst. Turkiye Parazitol Derg. 2017;41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Xie CL, Wu CQ, Chen Y, Chen TW, Xue HD, Jin ZY, Zhang XM. Sinistral Portal Hypertension in Acute Pancreatitis: A Magnetic Resonance Imaging Study. Pancreas. 2019;48:187-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Addeo P, De Mathelin P, Averous G, Tambou-Nguipi M, Terrone A, Schaaf C, Dufour P, Bachellier P. The left splenorenal venous shunt decreases clinical signs of sinistral portal hypertension associated with splenic vein ligation during pancreaticoduodenectomy with venous resection. Surgery. 2020;168:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Ono Y, Matsueda K, Koga R, Takahashi Y, Arita J, Takahashi M, Inoue Y, Unno T, Saiura A. Sinistral portal hypertension after pancreaticoduodenectomy with splenic vein ligation. Br J Surg. 2015;102:219-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Dörffel T, Wruck T, Rückert RI, Romaniuk P, Dörffel Q, Wermke W. Vascular complications in acute pancreatitis assessed by color duplex ultrasonography. Pancreas. 2000;21:126-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 100] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Sato T, Yamazaki K, Kimura M, Toyota J, Karino Y. Endoscopic Color Doppler Ultrasonographic Evaluation of Gastric Varices Secondary to Left-Sided Portal Hypertension. Diagnostics (Basel). 2014;4:94-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Giuffrè M, Macor D, Masutti F, Abazia C, Tinè F, Patti R, Buonocore MR, Colombo A, Visintin A, Campigotto M, Crocè LS. Evaluation of spleen stiffness in healthy volunteers using point shear wave elastography. Ann Hepatol. 2019;18:736-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Giuffrè M, Macor D, Masutti F, Abazia C, Tinè F, Bedogni G, Tiribelli C, Crocè LS. Spleen Stiffness Probability Index (SSPI): A simple and accurate method to detect esophageal varices in patients with compensated liver cirrhosis. Ann Hepatol. 2020;19:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Giuffrè M, Bedogni G, Abazia C, Masutti F, Tiribelli C, Crocè LS. Spleen stiffness can be employed to assess the efficacy of spontaneous portosystemic shunts in relieving portal hypertension. Ann Hepatol. 2020;19:691-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Giuffrè M, Fouraki S, Campigotto M, Colombo A, Visintin A, Buonocore MR, Aversano A, Budel M, Tinè F, Abazia C, Masutti F, Crocè LS. Alanine aminotransferase and spleno-portal dynamics affect spleen stiffness measured by point shear-wave elastography in patients with chronic hepatitis C in the absence of significant liver fibrosis. J Ultrasound. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |