Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.457
Peer-review started: August 25, 2020
First decision: October 27, 2020
Revised: October 28, 2020
Accepted: November 13, 2020
Article in press: November 13, 2020
Published online: January 16, 2021
Processing time: 135 Days and 19.3 Hours
Paratesticular liposarcoma accounts for approximately 7% of scrotal tumors. They are rare lesions of the reproductive system with approximately 90% of the lesions originating from the spermatic cord. Surgery, with the goal of complete resection, is the mainstay for treatment of this disease. However, treatment consisting of extended resection to decrease local recurrence remains controversial.
We report the cases of two patients with paratesticular liposarcomas who were treated with radical testicular tumor resection without adjuvant therapy. Follow-up investigations at 9 mo showed no sign of recurrence.
Surgery is the first-line treatment, regardless of whether it is a recurrent or primary tumor. Extended resection carries a higher risk of complications and should not be performed routinely. Preoperative radiotherapy can reduce the local recurrence rate without affecting the overall survival.
Core Tip: Atypical liposarcoma/well-differentiated liposarcoma is commonly distributed in the retroperitoneum, deep tissue of the extremities, and mediastinum, but rarely in the scrotum. We report the cases of two patients with paratesticular liposarcomas who were treated with radical testicular tumor resection without adjuvant therapy. The cases highlight surgery as the first choice of treatment, regardless of primary or recurrent liposarcoma, and show that extended resection is not beneficial for overall survival. Further, radiotherapy can provide a balance between the local recurrence rate and overall survival.
- Citation: Zheng QG, Sun ZH, Chen JJ, Li JC, Huang XJ. Paratesticular liposarcoma: Two case reports. World J Clin Cases 2021; 9(2): 457-462
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/457.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.457
Liposarcomas account for 5.75% of all tissue subtypes[1]. Atypical liposarcoma/well-differentiated liposarcoma (ALT/WDLPS) is the most common type of liposarcoma. ALT/WDLPS is mostly distributed in the retroperitoneum and deep tissue of the extremities and mediastinum, but rarely in the scrotum[2], with fewer than 200 similar cases reported to date in the English literature[3]. Surgery is currently the most effective treatment for patients with liposarcomas.
A retrospective multi-institutional study of 382 patients (including 106 WDLPSs) showed that the overall local recurrence rate was 49%[4]. Because of the high local recurrence rate, patients have to undergo repeated operations. However, subsequent operations can be disturbed by the scar from previous operations, leading to distortion of the normal anatomy. Hence, the quality and scope of the first operation need to be assessed. During treatment, factors under the surgeon’s control (including tumor integrity and extent of resection) and those reflective of tumor biology (grade and multifocality) affect patient outcomes[5].
We describe two rare cases of paratesticular liposarcomas in which the patients were treated with radical testicular tumor resection. Considering the rarity of cases, we review the literature regarding the application of surgical treatment.
Case 1: A 57-year-old Chinese man was hospitalized in the Urology Department of The Second Affiliated Hospital of Zhejiang Chinese Medical University (Hangzhou, China) because of a painless mass in his left scrotum for 1 year.
Case 2: A 62-year-old man presented with a mass in his left scrotum close to the abdomen, and it had grown slowly over about 30 d.
Case 1: He reported that the mass grew from the size of a soybean to the size of a fist in 1 year.
Case 2: He reported that the mass grew from the size of a soybean to the size of an egg within 20 d.
Case 1: The patient had no history of other illness and had no known allergies.
Case 2: He underwent left radical orchiectomy in our hospital 10 years ago due to the presence of a left scrotal mass. The pathological analysis indicated malignant fibrous histiocytoma. He had no known allergies.
Case 1: The patient did not smoke or drink, and had no relevant family history.
Case 2: The patient did not smoke or drink, and no relevant family history was reported.
Case 1: The mass was firm with no tenderness, and the testicles were away from the scrotum. The results of the light transmission test were negative.
Case 2: A firm and non-tender mass was found in the left scrotum close to the abdomen and the left testicle was absent.
Case 1: Serum carcinoembryonic antigen (CEA) level was 4.2 ng/mL (normal range: 0-5 ng/mL), and alpha-fetoprotein level was 3.0 ng/mL (normal value 8.0 ng/mL).
Case 2: The serum CEA level was 5.4 ng/mL, and CYFRA21-1 cytokeratin 19 fragment level was 2.49 ng/mL (normal range: 0-2.08 ng/mL).
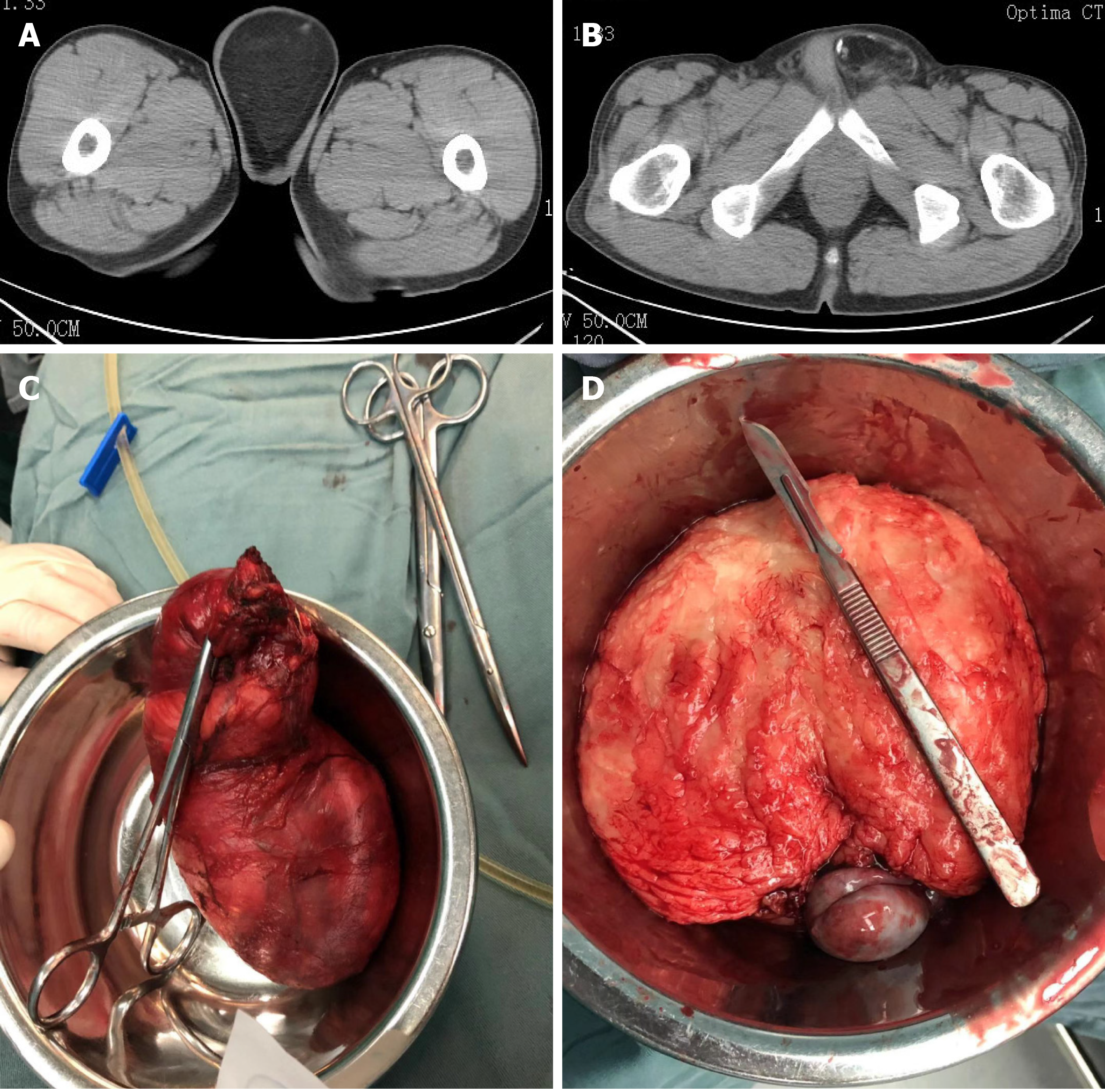
Case 1: Computed tomography (CT) did not show the left testicle; however, there were massive low-density foci (CT value: -80 U) in the left scrotal region; the maximum cross-sectional area was approximately 8.6 cm × 6.8 cm (Figure 1A). Mainly, mature lipid density was noted with spotted nodular calcification (Figure 1B). Initially, we considered this to be a teratoma.
Case 2: Ultrasonography (US) showed a heterogeneous echo mass in the median fat layer of the perineum. CT showed a nodular high-density shadow above the left scrotum in the lower abdomen, approximately 3.2 cm × 2.2 cm in size, and the boundary was unclear.
Based on the findings of the examination and imaging, a provisional diagnosis of liposarcoma was made.
Based on the above findings, a provisional diagnosis of liposarcoma was made.
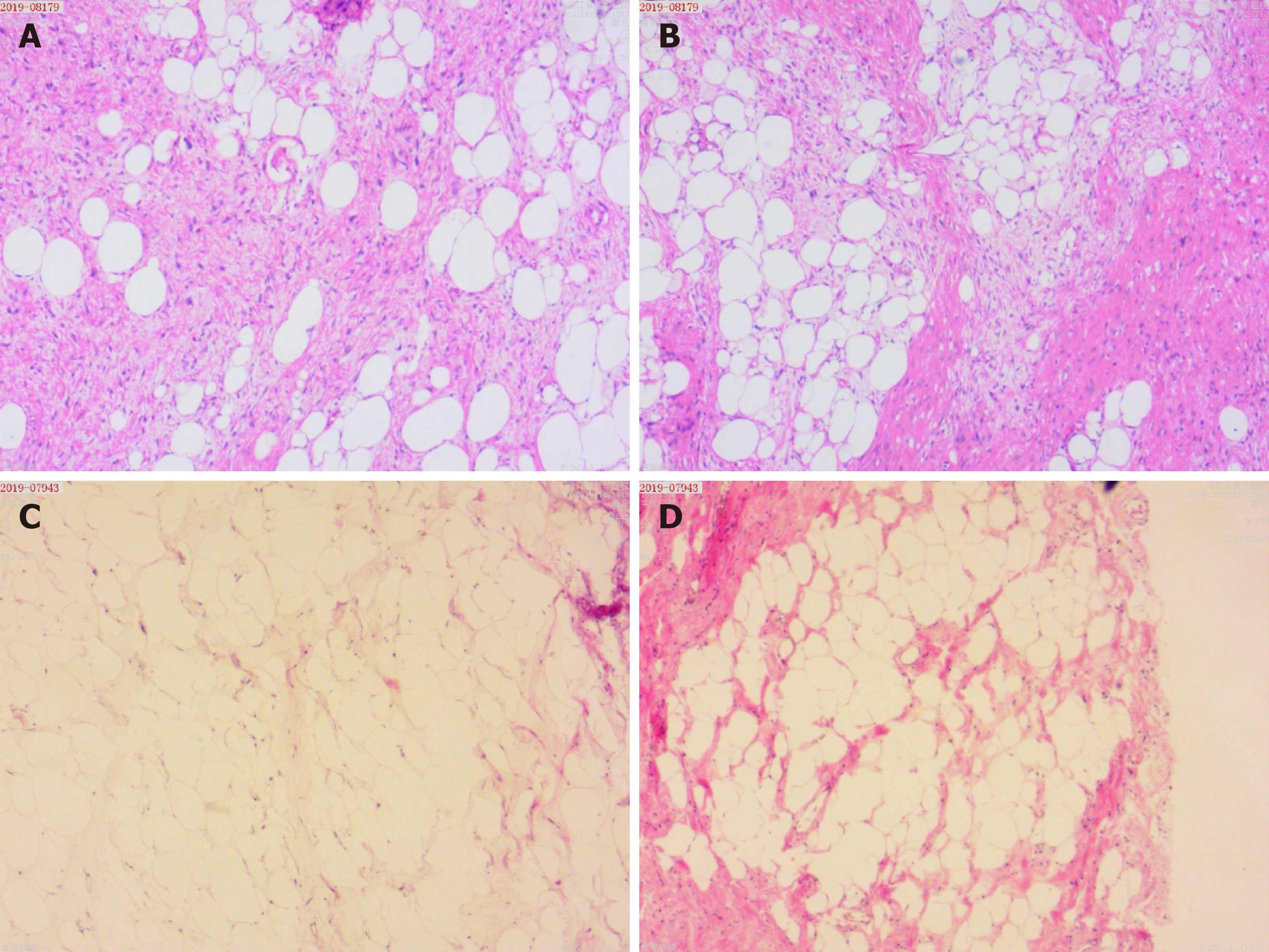
He underwent radical resection of the left testicular tumor on the 4th d after admission. The surgeon dissociated the entire spermatic cord up to the inner ring at the epididymis muscle. The spermatic cord was severed at the inner ring and sutured separately. The entire tumor and left testis, outside of the sheath, were resected. The tumor was a 14 cm × 8 cm × 6 cm, soft, gray-yellow mass (Figure 1C and D) with its capsule was intact and close to the testis. Pathological analysis showed that the tumor was composed of relatively mature adipocytes, single vesicular adipoblasts in the focal area, fibrous tissue with mucus deformation in the stroma (Figure 2A and B), and an intact tumor capsule. Immunohistochemical analysis revealed S100+, cluster of differentiation 34 (CD34), CD34+, vimentin-positive (Vim+), smooth muscle actin-positive (SMA+), CD68, and Ki67 < 1%+, which supported the diagnosis of ALT/WDLPS.
The patient underwent resection of the left inguinal tumor. The surgeon separated the tumor from the scrotum by 1 cm for R0 resection, and then resected it. The tumor measured about 7 cm × 5.5 cm × 2.5 cm, and we found a 3.5 cm × 3 cm × 2.5 cm gray-white mass in the middle with a clear boundary. Pathological analysis indicated that the tumor was an atypical liposarcoma (Figure 2C and D). Immunohistochemical analysis showed CD34+, S-100+, SMA-, VIM-, actin-negative (Act-), CD68 partial+, and KI67 30%+, supporting the diagnosis of ALT/WDLPS.
The patient was discharged 4 d after the operation without drugs or adjuvant therapy. At 9 mo postoperatively, there was no signs of recurrence.
The patient showed good postoperative recovery without any adjuvant therapy. His symptoms were relieved 9 mo postoperatively, and there were no signs of recurrence.
To date, surgeons believe that extended resection should be performed for liposar-comas to reduce the possibility of local recurrence. In a French retrospective multi-institutional study of 315 patients with retroperitoneal sarcomas who underwent complete gross tumor resection (R0/R1), 250 (79%) patients underwent compartmental organ resections including 120 (38%) patients who underwent compartmental complete resection. In the multivariate analysis, compartmental complete resection was associated with an improved 3-year cumulative incidence of local recurrence (10% compared with 47% after simple resection and 52% after non-compartmental organ resection)[4]. On the basis of these results, Bonvalot et al[4] recommended routine compartmental resection, regardless of histology. Nevertheless, this view is now being questioned. A retrospective analysis of 76 patients after complete resection (R0/R1) showed that 38 (46%) underwent organ resection; however, only 6 (7%) patients had organ invasion[6]. The data demonstrated that organ resection was not associated with overall survival (OS) or disease-free survival (DFS), whereas organ preservation was associated with a reduced risk of postoperative complications[6]. When analyzing relapsed patients undergoing secondary surgery, the same conclusion was reached[7].
If we only focus on the rate of local recurrence but not on patients’ postoperative survival time, this is a typical “analysis paralysis” situation. Patients undergoing extended resection have a higher risk of complications than those not undergoing extended resection. Bonvalot et al[4] reported that 16% of patients who underwent extended surgery have complications, and half of them require a second operation. The above situation can be aggravated by malnutrition[8]. Therefore, conservative resection is undoubtedly more suitable for patients with poor physical condition, such as elderly men. Thus, for the two patients described herein, considering their ages, only gross marginal negative resection (R1) was performed.
In the past, pathologists thought that chemotherapy and radiotherapy were limited with regard to the biological characteristics of liposarcomas. In a recent retrospective analysis of patients with liposarcomas who were mainly treated with an anthracycline-containing regimen, the objective response rate was 12%; additionally, there was no correlation between chemotherapy and OS or DFS; however, radiotherapy can reduce the local recurrence rate[9]. An analysis of 261 patients with liposarcomas showed that local failure-free survival was significantly improved if adjuvant radiotherapy was performed preoperatively instead of simple surgery (hazard ration [HR] = 0.42, 95% confidence interval [CI]: 0.21-0.86, P < 0.05)[10]. When performing radiotherapy for the same type of tumor, the required field of vision and dose are smaller preoperatively than postoperatively, and this modality is associated with fewer complications. Additionally, there is no evidence that radiotherapy has an effect on OS[10]. Hence, surgeons should pay more attention to the positive effect of radiotherapy before performing surgery for liposarcomas; however, the two patients discussed herein did not undergo radiotherapy before surgery.
Surgery is the first choice of treatment, regardless of primary or recurrent liposarcoma. However, extended resection is not beneficial for OS and should not be performed routinely. We recommend selective resection of compartmental organs only if there is a clinical suspicion of invasion at the time of surgical resection. Radiotherapy can create a balance between the local recurrence rate and OS. Preoperative radiotherapy is a less harmful than extended resection to reduce the burden of marginal viable tumor.
The article was supported by the National Clinical Key Specialist.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Machairas N, Shimada S S-Editor: Gao CC L-Editor: Filipodia P-Editor: Xing YX
| 1. | Vos M, Boeve WC, van Ginhoven TM, Sleijfer S, Verhoef C, Grünhagen DJ. Impact of primary tumor location on outcome of liposarcoma patients, a retrospective cohort study. Eur J Surg Oncol. 2019;45:2437-2442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 2. | Jo VY, Fletcher CD. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology. 2014;46:95-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 666] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 3. | Mouden K, Wakrim S, Semmar A. Paratesticular liposarcoma: a case report. Pan Afr Med J. 2019;33:282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Bonvalot S, Rivoire M, Castaing M, Stoeckle E, Le Cesne A, Blay JY, Laplanche A. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009;27:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 441] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 5. | Keung EZ, Hornick JL, Bertagnolli MM, Baldini EH, Raut CP. Predictors of outcomes in patients with primary retroperitoneal dedifferentiated liposarcoma undergoing surgery. J Am Coll Surg. 2014;218:206-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Ikoma N, Roland CL, Torres KE, Chiang YJ, Wang WL, Somaiah N, Mann GN, Hunt KK, Cormier JN, Feig BW. Concomitant organ resection does not improve outcomes in primary retroperitoneal well-differentiated liposarcoma: A retrospective cohort study at a major sarcoma center. J Surg Oncol. 2018;117:1188-1194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Ikoma N, Roland CL, Torres KE, Chiang YJ, Wang WL, Somaiah N, Mann GN, Hunt KK, Cormier JN, Feig BW. Salvage Surgery for Recurrent Retroperitoneal Well-Differentiated Liposarcoma: Early Reoperation may not Provide Benefit. Ann Surg Oncol. 2018;25:2193-2200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Kirov KM, Xu HP, Crenn P, Goater P, Tzanis D, Bouhadiba MT, Abdelhafidh K, Kirova YM, Bonvalot S. Role of nutritional status in the early postoperative prognosis of patients operated for retroperitoneal liposarcoma (RLS): A single center experience. Eur J Surg Oncol. 2019;45:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Italiano A, Toulmonde M, Cioffi A, Penel N, Isambert N, Bompas E, Duffaud F, Patrikidou A, Lortal B, Le Cesne A, Blay JY, Maki RG, Schwartz GK, Antonescu CR, Singer S, Coindre JM, Bui B. Advanced well-differentiated/dedifferentiated liposarcomas: role of chemotherapy and survival. Ann Oncol. 2012;23:1601-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 114] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 10. | Sampath S, Hitchcock YJ, Shrieve DC, Randall RL, Schultheiss TE, Wong JY. Radiotherapy and extent of surgical resection in retroperitoneal soft-tissue sarcoma: multi-institutional analysis of 261 patients. J Surg Oncol. 2010;101:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |