Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.403
Peer-review started: July 9, 2020
First decision: October 27, 2020
Revised: November 26, 2020
Accepted: December 10, 2020
Article in press: December 10, 2020
Published online: January 16, 2021
Processing time: 183 Days and 1.2 Hours
Most intrahepatic arterioportal fistulae (IAPF) are acquired. The few cases of congenital fistulae are diagnosed in infants and children.
We report a 31-year-old female patient presenting with haematemesis and melena three weeks after delivering her second child. The patient had a 20-year history of abdominal distention and nausea. IAPF, along with splenomegaly and ascites, was found by Doppler sonography and confirmed by computed tomography angiography. The patient was treated with endovascular coil embolization, resulting in occlusion of the fistula.
This was an unusual case of possible congenital IAPF that manifested during a second pregnancy and was complicated by portal hypertension.
Core Tip: Our study describes an unusual case of possible congenital intrahepatic arterioportal fistula that manifested during a second pregnancy and was complicated by portal hypertension. Coil embolization of the fistula provides a less invasive and effective therapeutic option in this case. Only 35 cases of congenital intrahepatic arterioportal fistula were reported until 2015, and no case in the peripartum setting was described.
- Citation: Stepanyan SA, Poghosyan T, Manukyan K, Hakobyan G, Hovhannisyan H, Safaryan H, Baghdasaryan E, Gemilyan M. Coil embolization of arterioportal fistula complicated by gastrointestinal bleeding after Caesarian section: A case report. World J Clin Cases 2021; 9(2): 403-409
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/403.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.403
Intrahepatic fistulae are categorized as arteriovenous, arterioportal and portosystemic. These three types of fistulae represent anomalous communications between the hepatic artery, portal vein and hepatic vein. Arterioportal fistulae can be intrahepatic (IAPF) and extrahepatic (EAPF). Optimal management of these fistulae has not been established due to the rarity of the anomalies[1-4].
IAPF was first reported by Gryboski et al[5] in 1967, but its aetiology remains unclear. Most IAPFs are acquired; fewer than 10% of cases are congenital, and they are diagnosed mostly in infants and children[6].
These fistulae have the potential to damage the portal vein and bowel and should be treated immediately after confirmation of the diagnosis. Congenital IAPF is typically caused by vascular malformation. Acquired IAPF and EAPF are more common and seen in hepatocellular carcinoma, ruptured hepatic artery aneurysm, post-liver biopsy, iatrogenic injury, blunt or penetrating trauma, interventional hepatic procedure, hepatectomy, Kasai portoenterostomy, segmental liver transplantation, cirrhosis, biliary atresia, and hereditary haemorrhagic telangiectasia[7-11].
Interventional radiology has a key role in the treatment of congenital arterioportal fistulae (APF)[12]. Congenital and acquired APFs require coil embolization or surgical intervention that involves hepatic artery ligation[13,14]. The treatment of APF has shifted from surgical ligation or hepatic resection to an endovascular-first approach[15].
Currently, the treatment of choice for most arterioportal fistulae is trans-arterial coil embolization. Symptomatic IAPFs and EAPFs can be occluded using steel coils, micro-coils, polyvinyl alcohol and/or microspheres, and detachable balloons[13,14]. Embolization of APF is technically feasible and effective and can be considered the first-choice therapy in selected patients[16]. The curative embolization of congenital IAPF is usually achieved in unilobar lesions[13,17,18]. For management of bilobar or complex lesions, a combination of embolization and surgery or a primary surgical approach is preferred[19-21].
A 31-year-old woman was referred to our clinic from a district hospital after two episodes of haematemesis and melena requiring transfusions.
There was no history of trauma, iatrogenic causes or tumour. A month prior, the patient had experienced the first episode of gastrointestinal bleeding during the 38th wk of her second pregnancy. After 7 d of conservative therapy (i/v fluids and observation), a caesarean section was performed without any complications.
Of interest, the patient reported a history of periodical abdominal distention since she was 10 years old and nausea since she was 20 years old. An abdominal ultrasound two years prior had revealed hepatomegaly and splenomegaly.
Personal and family history was unremarkable.
The physical examination on admission revealed abdominal distension. The patient’s pulse rate was 110 beats/min, and the blood pressure was 90/60 mmHg.
Laboratory results are shown in Table 1. There was no encephalopathy detected. Viral and autoimmune hepatitis markers were negative.
| Laboratory marker | On admission | Day 17 after coil embolization | Normal range | Unit |
| RBC | 1.99 | 2.6 | 3.5-5.6 | × 1012/L |
| Haemoglobin | 53 | 92 | 112-152 | g/L |
| WBC | 10.3 | 7.5 | 4.0-9.0 | × 109/L |
| Platelets | 113 | 214 | 180-400 | × 109/L |
| INR | 2.12 | 1.9 | 0.9-1.5 | - |
| Albumin | 28.9 | 41 | 35-52 | g/L |
| Bilirubin-total | 12.7 | 1.17 | 0.1-1.2 | mg/dL |
| AST | 85 | 15 | 0.1-50.0 | IU/L |
| ALT | 37 | 17 | 0.1-41.0 | IU/L |
| Creatinine | 143 | 90 | 44-97 | µm/L |
| Glucose | 7.9 | 5.6 | 4.1-6.1 | mm/L |
As seen on Doppler ultrasound, arterial inflow to the fistula occurred via a hypertrophied right hepatic artery draining into a dilated venous varix of the right branch of the portal vein. The portal vein showed arterialization with reversal of flow. There was associated splenomegaly detected. Approximately 4000 mL of free fluid was detected in the abdomen.
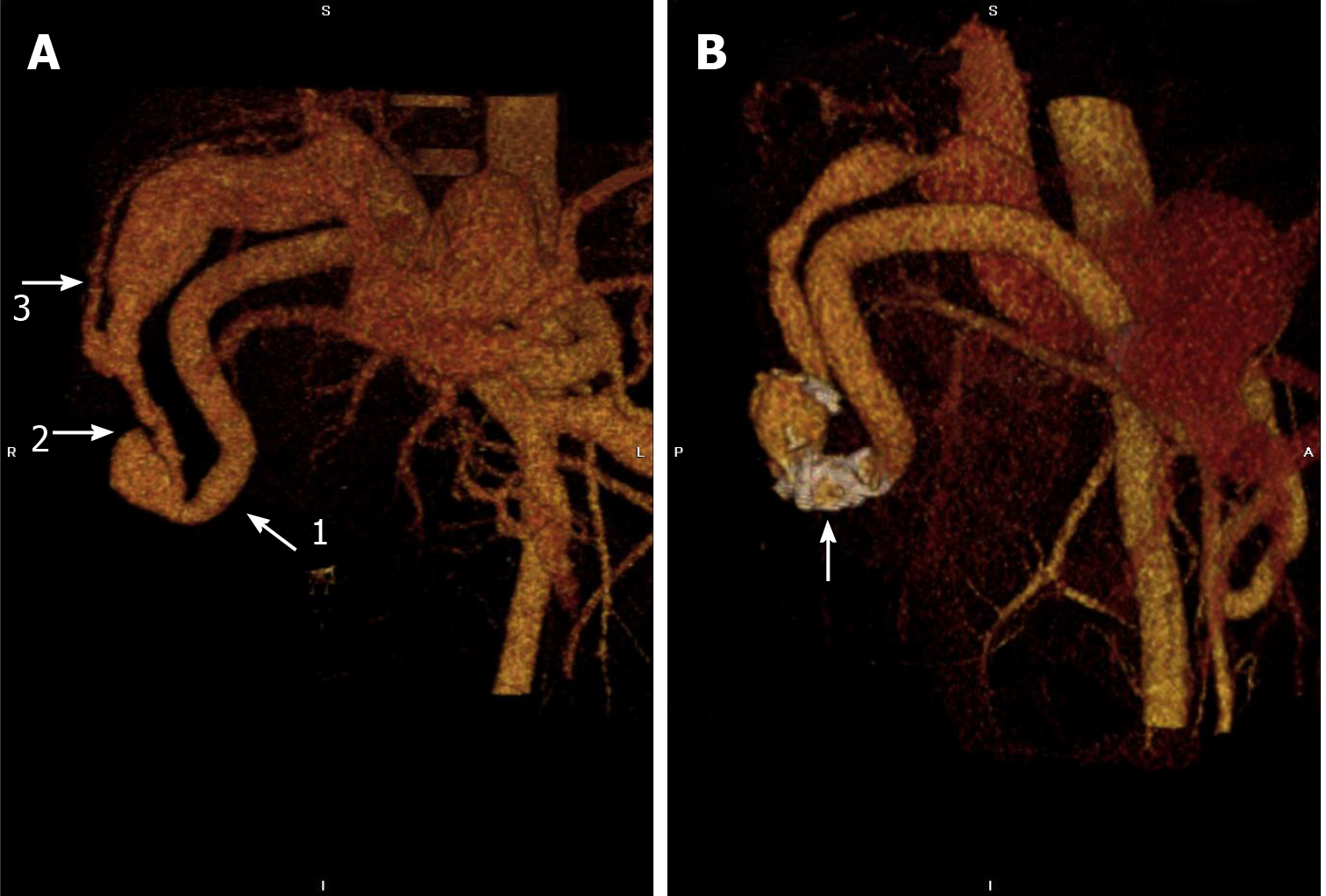
Computed tomography (CT) angiography confirmed the ultrasound findings, showing a round irregular vascular malformation with a size of 28.0 mm × 27.1 mm × 22.4 mm in segment 5 of the liver above the gallbladder with a shunt between the right hepatic artery and right portal vein (Figure 1A). The right hepatic artery near the vascular malformation was 11.8 mm (normal 3-5 mm), the right portal vein was 23.6 mm (normal 4-6 mm) and the fistula was 12 mm in diameter. Upper gastrointestinal endoscopy showed multiple large oesophageal varices as the cause of bleeding.
Intrahepatic arterioportal fistula complicated by portal hypertension and acute upper gastrointestinal bleeding from esophageal varices.
Endoscopic band ligation of oesophageal varices was performed. There was no bleeding after the procedure.
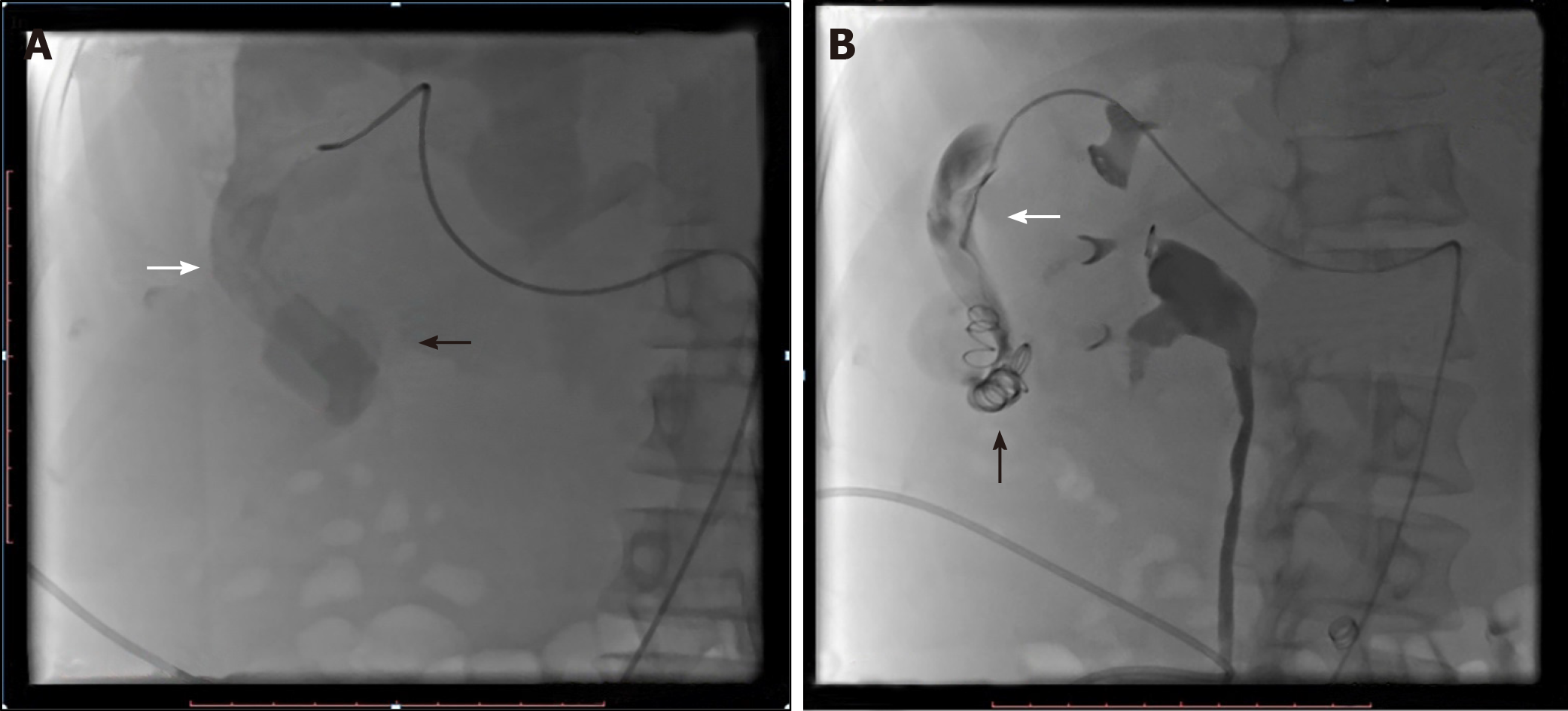
On the 11th day of hospitalization, the ascites became severe, and the abdominal cavity was drained with a 10-Fr pigtail catheter. On the 12th day of hospitalization, endovascular coil embolization of the arterioportal fistula was performed under local anaesthesia and mild intravenous sedation through the right femoral artery route using a 5F Cobra catheter (Terumo Corporation, Tokyo, Japan). Images were obtained of the celiac arteries, and further images were obtained of the right hepatic artery. The right hepatic artery was dilated, with the widest dilation of 12.2 mm. Continuation showed aneurysmal dilatation. The fistulous connection was 12 mm in diameter (Figure 2A). The decision was made to close the distal segments of the right hepatic artery by embolization with metallic coils (MRAY Cook medical, Bloomington, IN, United States), two coils of size 12-3 and six coils of size 8-5 (Figure 2B).
Following placement of coils, the flow gradually decreased. With stable vitals and an alert state of consciousness, the patient was transferred to the intensive care unit (ICU). The embolization procedure was completed without complications.
The patient’s symptoms and laboratory markers improved after the procedure (Table 1). On day 20 after the procedure, a second upper gastrointestinal endoscopy was performed, revealing scars after ligation of variceal veins in the middle and lower portions of the oesophagus. There were varices (0.7 cm in diameter) near the Z-line, and a second ligation procedure was performed.
The postoperative outcome of the patient was excellent. At 1 mo of follow-up, the patient had no signs of portal hypertension or malabsorption. Compared to before the procedure, follow-up CT angiography 2 years later revealed significantly less blood flow from the hepatic artery towards the portal system and a reduction in the size of the liver and spleen. Along with a reduction in the size of the right hepatic artery (9.5 mm), fistula (5.8 mm) and right portal vein (11.1 mm), no migration of the coil was noted (Figure 1B).
Acquired IAPF is more common than congenital IAPF and is seen in cases of disease and trauma of the liver and its vessels[22]. Congenital arterioportal fistulae in adults are very rare. If hepatic arterioportal fistula is revealed in adulthood, it is difficult to establish the cause as congenital[23].
In 2015, only 35 cases of congenital IAPF were reported, and no case in the peripartum setting was described Zhang et al[11] (2015) presented 4 cases (65-year-old female, 33-year-old female, 74-year-old male, and 43-year-old male patients) of congenital IAPF. There was no history of trauma or liver disease. The clinical manifestations were haemorrhage from oesophageal varices in two cases, ascites in one case and encephalopathy in one case. In all cases, endovascular embolization was performed[11].
Patients with IAPF may be asymptomatic or present with haemobilia, portal hypertension, or mesenteric steal syndrome[15]. Our patient did not have a history of abdominal trauma or any previous procedures related to the abdominal cavity. The present case was considered to be congenital because of its symptomatic presentation in childhood (periodical abdominal distention and nausea) and lack of any secondary factors. While the patient had preserved synthetic function, the worsening of her condition was related to portal hypertension and bleeding from oesophageal varices during the 38th week of her second pregnancy.
Ward et al[15] (2015) described a case of extrahepatic arterioportal fistula in a 40-year-old woman with a history of multiple pregnancies and no previous trauma. The fistula was formed between the left hepatic artery off the left gastric artery and the left portal vein. Endovascular embolization was performed with Amplatzer vascular plugs I. APF formation after visceral artery aneurysm rupture, often in the setting of pregnancy, is an alternative precipitating event and possibly the aetiology in this patient.
The present case is rare because clinical manifestations of portal hypertension started at the end of the second pregnancy. We could not identify cases in the literature describing the manifestation of IAPF during pregnancy.
Non-invasive examinations such as ultrasonography (US), colour Doppler US, CT or magnetic resonance imaging (MRI) are helpful in these cases. Catheter angiography is the confirmative diagnostic method for arterioportal fistulae[7]. In our case, Doppler US, CT angiography and catheter angiography were performed before the procedure, and the type, site and size of the arterioportal fistula were detected. As bleeding from oesophageal varices is life-threatening, endoscopic ligation and haemostasis play an important role in the treatment.
The treatment of IAPF includes percutaneous trans-arterial embolization, implicated-hepatic artery surgical ligation, partial hepatectomy and liver transplantation. Interventional radiological treatment is considered the preferred procedure[11]. Overall, slightly more than half of the cases of IAPFs are unilobar lesions. In this setting, curative embolization of intrahepatic arterioportal fistula is usually performed[12,13,24].
There is a wide range of embolic agents and devices available, including ethanol, Gelfoam, steel coils, detachable balloons, a combination of micro-coils and N-butyl 2-cyanoacrylate (NBCA), Amplatzer vascular plugs I, and a combination of Guglielmi detachable coils with NBCA injection[11,15].
In the present case, a single fistula between the right hepatic artery and the right portal vein was discovered. This finding allowed for successful treatment with coil embolization. Post-embolization angiogram showed occlusion of the arteriovenous fistula. In this report, we emphasize fistulae management and endovascular treatment. Embolization provides a less invasive and effective therapeutic option in this case.
IAPF is a rare but treatable cause of portal hypertension, and it may cause gastrointestinal bleeding and ascites. Embolization of IAPF is technically feasible and effective and can be considered the first-choice treatment in selected patients. This case highlights an unusual cause of IAPF that manifested during a second pregnancy and was complicated by portal hypertension.
The authors wish to extend their acknowledgements to Dr. Poghosyan A who performed the ultrasound and Doppler assessment of the patient, and to Dr. Shekherdimian S, MD (UCLA Mattel Children’s Hospital, Los Angeles, United States) for reviewing this paper and giving valuable input.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: United European Gastroenterology, Meeting of Members; Armenian Association of Gastroenterology; and European Association for the Study of the Liver.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Armenia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coco D, Rong GH S-Editor: Gao CC L-Editor: A P-Editor: Wang LL
| 1. | Wu L, Zhao L, Lu Y, He L, Hu X. Interventional embolization of congenital intrahepatic shunts in children. Pediatr Radiol. 2016;46:541-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Paley MR, Farrant P, Kane P, Heaton ND, Howard ER, Karani JB. Developmental intrahepatic shunts of childhood: radiological features and management. Eur Radiol. 1997;7:1377-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Gallego C, Miralles M, Marín C, Muyor P, González G, García-Hidalgo E. Congenital hepatic shunts. Radiographics. 2004;24:755-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 107] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Chandrasekharan R, Kp S, Moorthy S, Kulkarni C. Traumatic hepatic arteriohepatic venous fistula managed with selective coil embolization: a case report. BJR Case Rep. 2017;3:20150512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Gryboski JD, Clemett A. Congenital hepatic artery aneurysm with superior mesenteric artery insufficiency: a steal syndrome. Pediatrics. 1967;39:344-347. [PubMed] |
| 6. | Vauthey JN, Tomczak RJ, Helmberger T, Gertsch P, Forsmark C, Caridi J, Reed A, Langham MR Jr, Lauwers GY, Goffette P, Lerut J. The arterioportal fistula syndrome: clinicopathologic features, diagnosis, and therapy. Gastroenterology. 1997;113:1390-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 130] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Eastridge BJ, Minei JP. Intrahepatic arterioportal fistula after hepatic gunshot wound: a case report and review of the literature. J Trauma. 1997;43:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Gabriel S, Maroney TP, Ringe BH. Hepatic artery-portal vein fistula formation after percutaneous liver biopsy in a living liver donor. Transplant Proc. 2007;39:1707-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sachdeva R, Yapor M, Schwersenz A, Mitty H, Norton K, Rosh J, Borcich A, Benkov K, LeLeiko NS. Massive variceal bleeding caused by a hepatic artery-portal vein fistula: a manifestation of hepatocellular carcinoma in a 12-year-old. J Pediatr Gastroenterol Nutr. 1993;16:468-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Tanaka H, Iwai A, Sugimoto H, Yoshioka T, Sugimoto T. Intrahepatic arterioportal fistula after blunt hepatic trauma: case reports. J Trauma. 1991;31:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Zhang DY, Weng SQ, Dong L, Shen XZ, Qu XD. Portal hypertension induced by congenital hepatic arterioportal fistula: report of four clinical cases and review of the literature. World J Gastroenterol. 2015;21:2229-2235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Teplisky D, Tincani EU, Lipsich J, Sierre S. Congenital arterioportal fistulas: radiological treatment and color Doppler US follow-up. Pediatr Radiol. 2012;42:1326-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Raghuram L, Korah IP, Jaya V, Athyal RP, Thomas A, Thomas G. Coil embolization of a solitary congenital intrahepatic hepatoportal fistula. Abdom Imaging. 2001;26:194-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Zhang WG, Li Z, Ding PX, Ren JZ, Ma J, Zhou PL, Wang ZG, Han XW. Endovascular treatment of an unusual primary arterioportal fistula complicated by cavernous transformation of the portal vein caused by portal thrombosis. Ann Vasc Surg 2014; 28: 491.e5-491. e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Ward TJ, Marin ML, Lookstein RA. Embolization of a giant arterioportal fistula requiring multiple Amplatzer vascular plugs. J Vasc Surg. 2015;62:1636-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Nie L, Luo XF, Li X. Gastrointestinal bleeding caused by extrahepatic arterioportal fistula associated with portal vein thrombosis. World J Gastroenterol. 2012;18:6501-6503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Kumar N, de Goyet Jde V, Sharif K, McKiernan P, John P. Congenital, solitary, large, intrahepatic arterioportal fistula in a child: management and review of the literature. Pediatr Radiol. 2003;33:20-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Ozyer U, Kirbas I, Aytekin C, Hasdogan B. Coil embolization of a congenital intrahepatic arterioportal fistula: increasing experience in management. Pediatr Radiol. 2008;38:1253-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Guzman EA, McCahill LE, Rogers FB. Arterioportal fistulas: introduction of a novel classification with therapeutic implications. J Gastrointest Surg. 2006;10:543-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 76] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Sutcliffe R, Mieli-Vergani G, Dhawan A, Corbally M, Karani J, Heaton N. A novel treatment of congenital hepatoportal arteriovenous fistula. J Pediatr Surg. 2008;43:571-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Tannuri AC, Tannuri U, Lima FR, Ricardi LR, Leal AJ, da Silva MM. Congenital intrahepatic arterioportal fistula presenting as severe undernutrition and chronic watery diarrhea in a 2-year-old girl. J Pediatr Surg. 2009;44:e19-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Hirakawa M, Nishie A, Asayama Y, Ishigami K, Ushijima Y, Fujita N, Honda H. Clinical outcomes of symptomatic arterioportal fistulas after transcatheter arterial embolization. World J Radiol. 2013;5:33-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Van Way CW 3rd, Crane JM, Riddell DH, Foster JH. Arteriovenous fistula in the portal circulation. Surgery. 1971;70:876-890. [PubMed] |
| 24. | Norton SP, Jacobson K, Moroz SP, Culham G, Ng V, Turner J, John P. The congenital intrahepatic arterioportal fistula syndrome: elucidation and proposed classification. J Pediatr Gastroenterol Nutr. 2006;43:248-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |