Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.389
Peer-review started: June 27, 2020
First decision: July 28, 2020
Revised: August 11, 2020
Accepted: November 21, 2020
Article in press: November 21, 2020
Published online: January 16, 2021
Processing time: 195 Days and 3.3 Hours
Pancreatic pseudocyst may cause serious gastrointestinal complications including necrosis, infection, and perforation of the gastrointestinal tract wall, but massive gastric bleeding is very rare.
We report a rare case of a 49-year-old man with life-threatening gastric bleeding from a pseudoaneurysm of the splenic artery perforating the stomach induced by pancreatic pseudocyst. During hospitalization, gastroscopy revealed a bare blood vessel in an ulcer-like depression of the greater gastric curvature, and computed tomography scan confirmed a pancreatic pseudocyst invading part of the spleen and gastric wall of the greater curvature. Arteriography showed that the bare blood vessel originated from a pseudoaneurysm of the splenic artery. The bleeding was controlled by the trans-arterial embolization, the patient’s recovery was rapid and uneventful.
Massive gastrointestinal bleeding could be a rare complication of pancreatic pseudo aneurysm.
Core Tip: Massive hemorrhage of the gastrointestinal tract is an infrequent complication of the pancreatic pseudocyst and pseudoaneurysm. We present herein, a novel case of a patient with life-threatening gastric bleeding from a pseudoaneurysm of the splenic artery as a complication of pancreatic pseudocyst perforating into the stomach, with trans-arterial embolization as a potential therapeutic modality for achieving hemostasis.
- Citation: Jin Z, Xiang YW, Liao QS, Yang XX, Wu HC, Tuo BG, Xie R. Massive gastric bleeding - perforation of pancreatic pseudocyst into the stomach: A case report and review of literature. World J Clin Cases 2021; 9(2): 389-395
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/389.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.389
Erosion caused by the pancreatic inflammatory process or pseudocyst development in an adjacent vessel may lead to a pseudoaneurysm. Its rupture in the gastrointestinal tract can target the pancreatic duct, stomach, duodenum, or colon[1,2]. Massive hemorrhage of the gastrointestinal tract is an infrequent complication of pancreatic pseudocyst and pseudoaneurysm but can be lethal, with a reported death rate of approximately 50%[3,4]. Therefore, spontaneous rupture of a pancreatic pseudocyst into adjacent organs with massive bleeding from a pseudoaneurysm requires rapid management. Here, we report a novel case of a 49-year-old man with life-threatening gastric bleeding from a pseudoaneurysm of the splenic artery as a complication of pancreatic pseudocyst perforating into the stomach, with trans-arterial embolization (TAE) as a potential therapeutic modality for achieving hemostasis.
A 49-year-old male presented to the emergency room with pain in the left upper abdomen and melena, accompanied by symptoms of dizziness and weakness.
Patient had intermittent left upper abdomen pain and melena for 5 d.
He had a history of alcoholism and was diagnosed with pancreatitis and type 2 diabetes for 1 year.
On admission, physical examination revealed only slight tenderness in the left upper abdomen and pale conjunctiva of eye. No muscular tension or rebound tenderness was noted. Digital rectal examination showed negative results.
Laboratory tests showed that hemoglobin was 63 g/L (normal range: > 120 g/L). The fecal occult blood result was positive, and the remaining biochemical tests including amylase were normal.
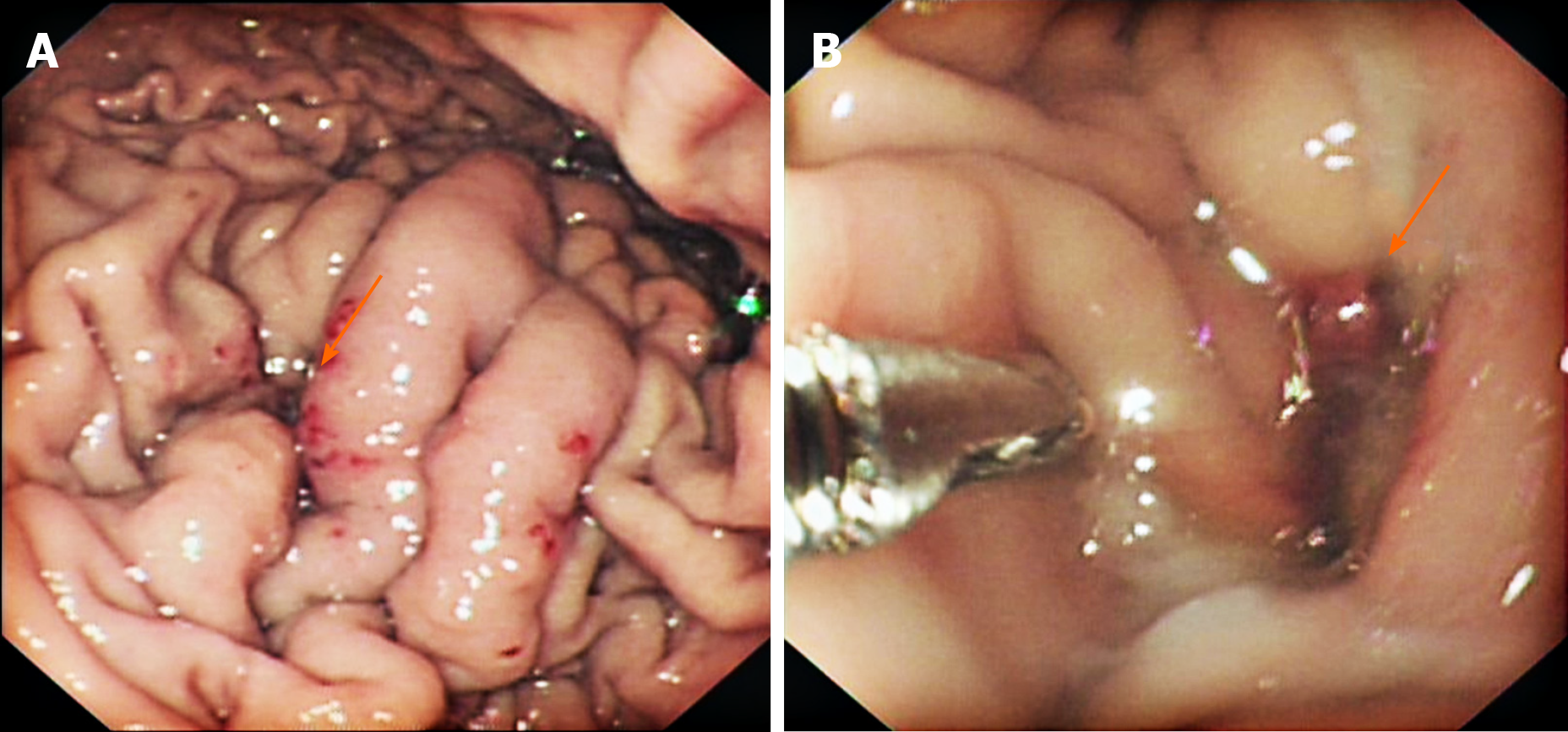
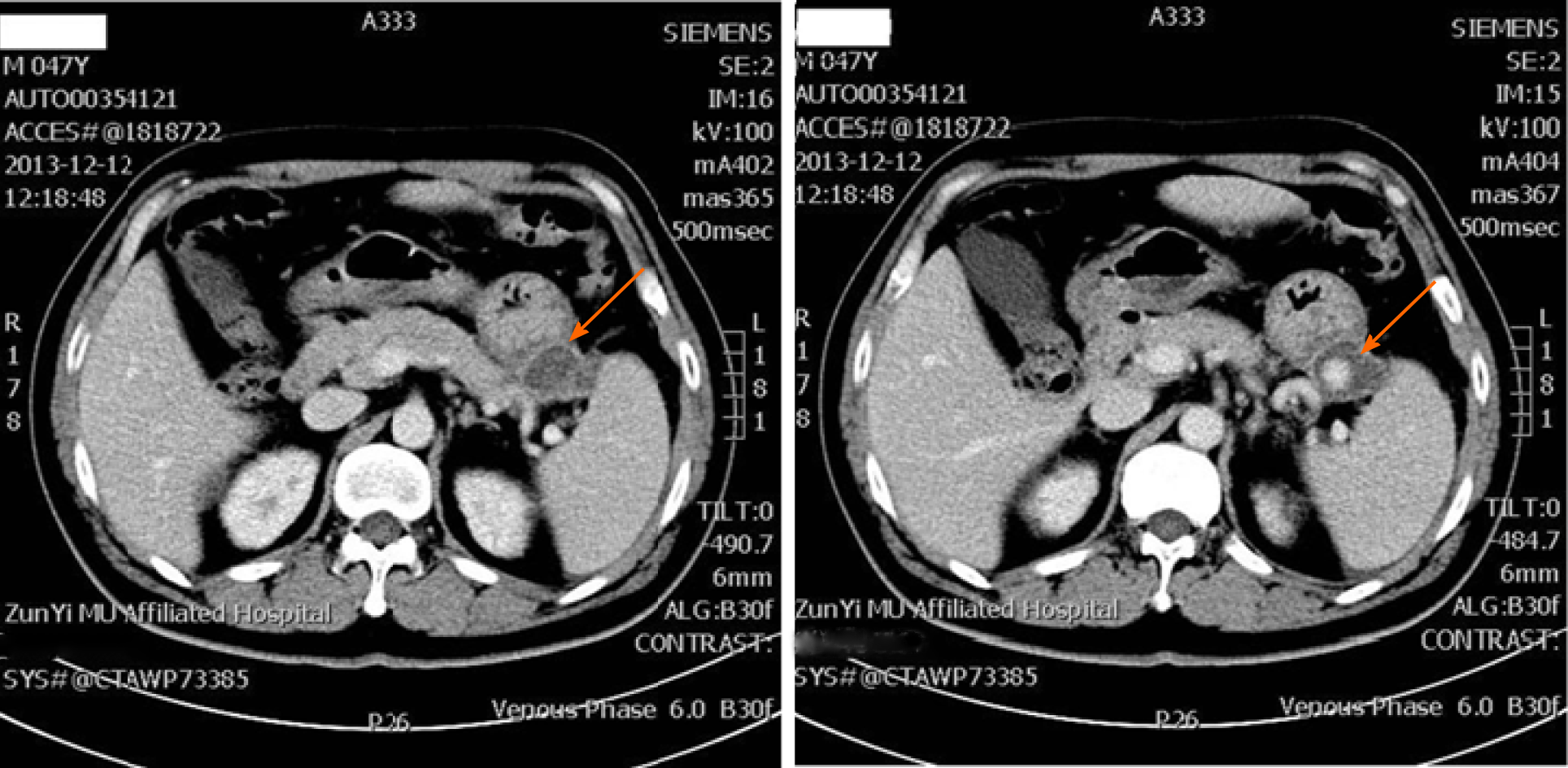
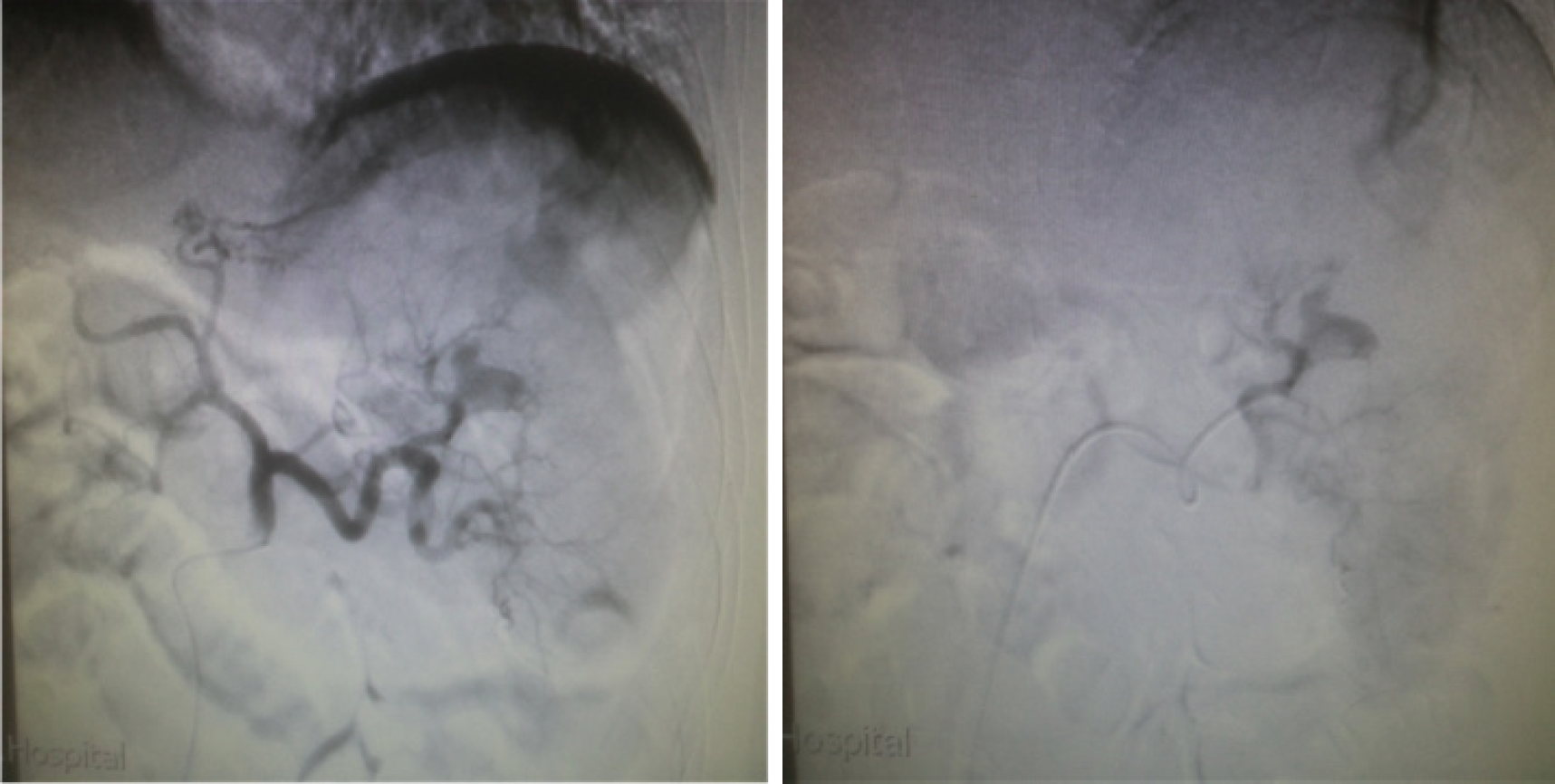
Gastroscopic examination revealed an ulcer-like depression on the upper part of the greater gastric curvature and mucus secretions adhered to the epithelial surface. The surrounding mucosa exhibited thickening and edema with obscured structural outlines. The gastric folds could not be fully extended after gas charging. We suspected that upper gastrointestinal bleeding was caused by a gastric ulcer or gastric cancer. The condition improved after proton pump inhibitors and octreotide pumping hemostasis treatment for 1 wk, but the patient suddenly excreted watery dark red stool again, accompanied by massive hematemesis. Gastroscopy was repeated, and oozing blood was found in the ulcer-like depression of the gastric greater curvature previously observed, blood vessels were exposed after repeated rinsing (Figure 1). Computed tomography (CT) scan confirmed widespread subversion of pancreatic parenchyma, with evidence of multiple inhomogeneous hypodense and partially confluent cystic formations. The pancreatic pseudocyst invaded part of the spleen and greater curvature of the stomach; the invaded gastric mucosa was irregularly thickened and emitted an uneven signal (Figure 2). Emergency digital subtraction angiography (DSA) revealed that the pseudoaneurysm arose from the splenic artery (Figure 3).
Finally, the patient was diagnosed with upper gastrointestinal bleeding from a pseudo aneurysm of the arteria lienalis secondary to perforated pancreatic pseudoaneurysm invading into the stomach.
The patient underwent surgical treatment with TAE (coil embolization) of the splenic artery, which was successfully performed and the bleeding was effectively controlled (Figure 4).
One week after the operation, the patient’s recovery was rapid and uneventful.
The incidence of pancreatic pseudocyst associated with hemorrhage is approximately 5%-10%, with a mortality rate of about 50%[3,4]. The clinical feature varies depending on the location and severity of the bleeding, thus presenting in different forms, from abdominal pain to hypovolemic shock[5,6]. Massive bleeding has been reported in 2%-10% of patients with pancreatitis and occurs as upper or lower gastrointestinal tract bleeding[7,8]. The rapid development of an abdominal painful mass suggests intracystic bleeding. Intraperitoneal bleeding causes abdominal distension and hemorrhagic shock.
The main pathogenesis involves erosion of the pancreas, peripancreatic vessels, and surrounding tissues because of elastase and trypsin, which weaken tensile strength and cause rupture or bleeding after pseudoaneurysm formation. The splenic artery is the most frequently involved site of pancreatitis complicated with pseudoaneurysm[9]. Other sites include the gastroduodenal artery, the pancreaticoduodenal artery, and the hepatic artery. We conducted a review of published case reports. These reports described patients with pancreatic pseudoaneurysms that communicated with the bowel lumen in the past 5 years (Table 1)[10-26]. When the cyst invades the gastro-intestinal tract, bleeding can appear in the abdomen, stomach, duodenum and even the lower digestive tract, presenting as massive bloody stool and hematemesis or chronic intermittent bleeding after abdominal pain[27,28]. Regarding hemorrhage of the digestive tract or abdominal cavity in pancreatitis, localization of the bleeding in a timely and accurate manner is very important. CT and B-ultrasound are the first choices for imaging evaluation of pancreatitis. These methods clarify the severity and extent of pancreatitis to determine whether the condition is associated with pancreatic abscess or pseudoaneurysms, and accurately assess the condition of peripancreatic vessels[29,30]. Computed-tomography angiography (CTA) can improve the diagnostic positive rate during the bleeding period. CTA can demonstrate the full extent of a pseudoaneurysm, in case of partial thrombosis, and its effect on the adjacent viscera. But CTA has the disadvantage of radiation exposure, which is particularly critical in young patients[31]. DSA is the gold standard for the diagnosis of hemorrhage of pancreatic pseudoaneurysms, contrast agent extravasation can be found when the bleeding is greater than 0.5 mL/min, which is important for the diagnosis of hemorrhage position. We compared three therapeutic modalities (Table 2).
| Ref. | Age in yr | Sex | Involved hollow viscus and bleeding part | Treatment |
| Fujio et al[10], 2017 | 75 | Male | Jejunum | TAE |
| Eftimie et al[11], 2017 | 55 | Male | Colon | Surgery |
| 59 | Male | Stomach | Surgery | |
| Budzyński et al[12], 2016 | 42 | Female | Stomach | TAE |
| O’Brien et al[13], 2016 | 88 | Female | Colon | TAE |
| Zhang et al[14], 2016 | 58 | Female | Stomach | TAE |
| Zhao et al[15], 2014 | 64 | Male | Colon | Surgery |
| Razik et al[16], 2016 | 62 | Female | Duodenum | TAE |
| Hoshimoto et al[17], 2016 | 61 | Male | Stomach | TAE |
| Larrey Ruiz et al[18], 2016 | 40 | Male | Duodenum | TAE and Surgery |
| Chia et al[19], 2015 | 24 | Male | Stomach | Surgery |
| Sawicki et al[20], 2015 | 57 | Male | Stomach and abdominal cavity | Surgery |
| Ferreira et al[21], 2015 | 54 | Male | Duodenum | TAE |
| Shah et al[22], 2015 | 69 | Male | Duodenum | TAE |
| Maddah et al[23], 2015 | 32 | Female | Stomach | Surgery |
| 54 | Male | Stomach | Surgery | |
| Peynircioğlu et al[24], 2015 | 62 | Male | Duodenum | TAE |
| Mandaliya et al[25], 2014 | 61 | Female | Duodenum | TAE |
| Herrera-Fernández et al[26], 2014 | 34 | Female | Stomach | Surgery |
| Therapeutic options | Advantages | Disadvantages |
| Endoscopic | Minimally invasive, accurate localization, rapid, safe, high success rate, few complications, and rapid recovery | Limited for operating site, rebleeding |
| Endovascular | Minimally invasive, accurate localization, rapid, safe, high success rate, few complications, and rapid recovery | Radiation exposure, rebleeding |
| Surgical | Selection after endoscopy and endovascular are ineffective in the treatment of gastrointestinal bleeding | Massive trauma, many complications, slow recovery |
In such cases, effective therapeutic procedures include percutaneous, intravascular embolization (TAE), or immediate laparotomy[28], laparotomy during hemorrhagic shock can give rise to serious complications. Endovascular treatment has several advantages compared to open surgical repair, allowing accurate localization of pseudoaneurysm and assessment of collateral vessels; it is associated with a lower post-operative morbidity and mortality (4%-19%) compared to surgery and a high rate of technical success (67%-97%)[32]. Moreover, if rebleeding occurs, the procedure can be promptly repeated. Therefore, for patients who are at risk for massive bleeding, accompanied with unstable vital signs, selectively DSA examination should be performed immediately to identify the bleeding location, and TAE is likely to be the first choice for temporary control of bleeding. Supplementary endovascular options include use of liquid embolic agents, temporary embolic materials (Gelfoam slurry; Upjohn Co., Kalamazoo, MI, United States) or coil embolization[33]. Many endovascular treatment options are today available mainly depending on expendability of parent artery and size of pseudoaneurysmal neck. Parent artery is expendable when adequate extensive collateral circulation is present; in this case aggressive coil embolization can be performed. Coil embolization of expendable arteries is preferable distally and proximally to the site of extravasation (the so called “sandwich” technique), thereby preventing backflow from the collateral circulation[34,35]. Rebleeding has been reported in 37% of patients, and urgent surgery should be limited to when embolization fails. Even after successful immediate embolization[28], the safety and success rate of TAE treatment for the pseudoaneurysm hemorrhage need to be improved in the future.
Gastrointestinal bleeding is a relatively rare but potentially lethal complication of pancreatic pseudoaneurysms. Endovascular treatment should always be considered the first-line option for the management of peripancreatic pseudoaneurysm in patients who are at risk of massive bleeding, accompanied by unstable vital signs.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aziz M S-Editor: Chen XF L-Editor: Filipodia P-Editor: Wang LL
| 1. | Lin YH, Chen CY, Chen CP, Kuo TY, Chang FY, Lee SD. Hematemesis as the initial complication of pancreatic adenocarcinoma directly invading the duodenum: a case report. World J Gastroenterol. 2005;11:767-769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Tanaka A, Takeda R, Utsunomiya H, Kataoka M, Mukaihara S, Hayakawa K. Severe complications of mediastinal pancreatic pseudocyst: report of esophagobronchial fistula and hemothorax. J Hepatobiliary Pancreat Surg. 2000;7:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Gagliano E, Barbuscia MA, Tonante A, Taranto F, Paparo D, Papalia E, Cascio R, Damiano C, Sturniolo G. Pancreatic pseudocyst: case report and short literature review. G Chir. 2012;33:415-419. [PubMed] |
| 4. | Lee P, Sutherland D, Feller ER. Massive gastrointestinal bleeding as the initial manifestation of pancreatic carcinoma. Int J Pancreatol. 1994;15:223-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Kim KO, Kim TN. Acute pancreatic pseudocyst: incidence, risk factors, and clinical outcomes. Pancreas. 2012;41:577-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Braganza JM, Lee SH, McCloy RF, McMahon MJ. Chronic pancreatitis. Lancet. 2011;377:1184-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 343] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 7. | Xiao B, Zhang XM, Tang W, Zeng NL, Zhai ZH. Magnetic resonance imaging for local complications of acute pancreatitis: a pictorial review. World J Gastroenterol. 2010;16:2735-2742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Lerch MM, Gorelick FS. Models of acute and chronic pancreatitis. Gastroenterology. 2013;144:1180-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 316] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 9. | Urakami A, Tsunoda T, Kubozoe T, Takeo T, Yamashita K, Imai H. Rupture of a bleeding pancreatic pseudocyst into the stomach. J Hepatobiliary Pancreat Surg. 2002;9:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Fujio A, Usuda M, Ozawa Y, Kamiya K, Nakamura T, Teshima J, Murakami K, Suzuki O, Miyata G, Mochizuki I. A case of gastrointestinal bleeding due to right hepatic artery pseudoaneurysm following total remnant pancreatectomy: A case report. Int J Surg Case Rep. 2017;41:434-437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Eftimie MA, Stanciulea OM, David L, Lungu V, Dima S, Mosteanu I, Tirca L, Popescu I. Surgical Treatment of Splenic Artery Pseudoaneurysm with Digestive Tract Communication - Presentation of Two Cases. Chirurgia (Bucur). 2017;112:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Budzyński J, Meder G, Suppan K. Giant gastroduodenal artery pseudoaneurysm as a pancreatic tumor and cause of acute bleeding into the digestive tract. Prz Gastroenterol. 2016;11:299-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | O'Brien J, Muscara F, Farghal A, Shaikh I. Haematochezia from a Splenic Artery Pseudoaneurysm Communicating with Transverse Colon: A Case Report and Literature Review. Case Rep Vasc Med. 2016;2016:8461501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Zhang YM, Wang J, Chen DF. A Rare Cause of Massive Upper Gastrointestinal Bleeding. Gastroenterology. 2016;151:e5-e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Zhao J, Kong X, Cao D, Jiang L. Hematochezia From Splenic Arterial Pseudoaneurysm Ruptured Into Pancreatic Pseudocyst Coexisting With Fistula to the Colon: A Case Report and Literature Review. Gastroenterology Res. 2014;7:73-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Razik R, May GR, Saibil F. Non-operative Management of Necrotic Pancreatic Collection and Bleeding Pseudoaneurysm Communicating with Bowel Lumen at Multiple Sites: a Case Report and Review of the Literature. J Gastrointestin Liver Dis. 2016;25:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Hoshimoto S, Aiura K, Shito M, Kakefuda T, Sugiura H. Successful resolution of a hemorrhagic pancreatic pseudocyst ruptured into the stomach complicating obstructive pancreatitis due to pancreatic cancer: a case report. World J Surg Oncol. 2016;14:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Larrey Ruiz L, Luján Sanchis M, Peño Muñoz L, Barber Hueso C, Cors Ferrando R, Durá Ayet AB, Sempere García-Argüelles J. Pseudoaneurysm associated with complicated pancreatic pseudocysts. Rev Esp Enferm Dig. 2016;108:583-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Chia C, Pandya GJ, Kamalesh A, Shelat VG. Splenic Artery Pseudoaneurysm Masquerading as a Pancreatic Cyst-A Diagnostic Challenge. Int Surg. 2015;100:1069-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 20. | Sawicki M, Marlicz W, Czapla N, Łokaj M, Skoczylas MM, Donotek M, Kołaczyk K. Massive Upper Gastrointestinal Bleeding from a Splenic Artery Pseudoaneurysm Caused by a Penetrating Gastric Ulcer: Case Report and Review of Literature. Pol J Radiol. 2015;80:384-387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Ferreira J, Tavares AB, Costa E, Maciel J. Hemosuccus pancreaticus: a rare complication of chronic pancreatitis. BMJ Case Rep. 2015;2015:bcr2015209872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Shah AA; Sultan-E-Rome; Charon JP. Haemosuccus pancreaticus, an uncommon cause of upper gastro intestinal bleeding: Case report and review of the literature. J Pak Med Assoc. 2015;65:669-671. [PubMed] |
| 23. | Maddah G, Abdollahi A, Golmohammadzadeh H, Abdollahi M. Hemosuccus pancreaticus as a rare cause of gastrointestinal bleeding: a report of two cases. Acta Med Iran. 2015;53:320-323. [PubMed] |
| 24. | Peynircioğlu B, Karaosmanoğlu AD, İdilman İS, Akata D, Şimşek H. Intrapancreatic pseudoaneurysm causing massive gastrointestinal hemorrhage and chronic pancreatitis. Turk J Gastroenterol. 2015;26:270-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Mandaliya R, Krevsky B, Sankineni A, Walp K, Chen O. Hemosuccus Pancreaticus: A Mysterious Cause of Gastrointestinal Bleeding. Gastroenterology Res. 2014;7:32-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Herrera-Fernández FA, Palomeque-Jiménez A, Serrano-Puche F, Calzado-Baeza SF, Reyes-Moreno M. [Rupture of splenic artery pseudoaneurysm: an unusual cause of upper gastrointetinal bleeding]. Cir Cir. 2014;82:551-555. [PubMed] |
| 27. | Araki K, Shimura T, Watanabe A, Kobayashi T, Suzuki H, Suehiro T, Kuwano H. Gastric bleeding from a penetrating pancreatic pseudocyst with pseudoaneurysm of the splenic artery. Hepatogastroenterology. 2009;56:1411-1413. [PubMed] |
| 28. | Boudghène F, L'Herminé C, Bigot JM. Arterial complications of pancreatitis: diagnostic and therapeutic aspects in 104 cases. J Vasc Interv Radiol. 1993;4:551-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 131] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Balthazar EJ, Fisher LA. Hemorrhagic complications of pancreatitis: radiologic evaluation with emphasis on CT imaging. Pancreatology. 2001;1:306-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 104] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 30. | Mir MF, Shaheen F, Gojwari TA, Singh M, Nazir P, Ahmad S. Uncomplicated spontaneous rupture of the pancreatic pseudocyst into the gut--CT documentation: a series of two cases. Saudi J Gastroenterol. 2009;15:135-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Glockner JF. Three-dimensional gadolinium-enhanced MR angiography: applications for abdominal imaging. Radiographics. 2001;21:357-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Kim J, Shin JH, Yoon HK, Ko GY, Gwon DI, Kim EY, Sung KB. Endovascular intervention for management of pancreatitis-related bleeding: a retrospective analysis of thirty-seven patients at a single institution. Diagn Interv Radiol. 2015;21:140-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Lopera JE. Embolization in trauma: principles and techniques. Semin Intervent Radiol. 2010;27:14-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 34. | Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25 Suppl 1:S173-S189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 352] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 35. | Barge JU, Lopera JE. Vascular complications of pancreatitis: role of interventional therapy. Korean J Radiol. 2012;13 Suppl 1:S45-S55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |