Published online Jun 16, 2021. doi: 10.12998/wjcc.v9.i17.4433
Peer-review started: February 10, 2021
First decision: March 11, 2021
Revised: March 16, 2021
Accepted: March 24, 2021
Article in press: March 24, 2021
Published online: June 16, 2021
Processing time: 104 Days and 20.4 Hours
Intraneural ganglion cysts are benign gelatinous masses that form within the epineurium of a peripheral nerve. Only few cases of intraneural ganglion cyst arising from the hip joint have been reported.
A previously healthy 65-year-old woman who had been experiencing left buttock pain radiating to the dorsum of the foot for 2 years visited our clinic. Prior to visiting the clinic, she underwent lumbar spine magnetic resonance imaging and received physiotherapy, pain killers, and epidural injections based on a presumptive diagnosis of spinal stenosis for 2 years in other hospitals. Repeat magnetic resonance imaging revealed joint connection of the articular branch of the hip joint and rostral extension of the cyst along the L5 spinal nerve near the L5-S1 neural foramen. The patient was diagnosed with intraneural ganglion cyst arising from the articular branch of the hip joint based on high-resolution magnetic resonance neurography. Using the arthroscopic approach, a cystic opening within the intra-articular space was detected, and cyst decompression was then performed. The pain in the left leg was significantly relieved during the 6-mo follow-up.
Although intraneural ganglion cysts arising from the hip joint are rare, they can cause typical radicular pain and mimic common L5 radiculopathy. Typical cyst ascent phenomenon starting from the termination of the articular branch on magnetic resonance imaging is a crucial finding indicative of intraneural ganglion cysts arising from the hip joint.
Core Tip: This report presents a rare case of an intraneural ganglion cyst arising from the hip joint. At present, the patient demonstrated typical radicular pain of lower extremity. If there is no lesion in the lumbar spine that can be associated with radicular pain, the hip joint pathology must be comprehensively evaluated, with consideration of the possibility of intraneural ganglion cysts. High-resolution magnetic resonance neurography can be helpful in identifying a possible joint connection in juxta-articular ganglia cysts, and arthroscopic debridement and cyst decompression can be alternative treatments to cyst resection.
- Citation: Lee JG, Peo H, Cho JH, Kim DH. Intraneural ganglion cyst of the lumbosacral plexus mimicking L5 radiculopathy: A case report. World J Clin Cases 2021; 9(17): 4433-4440
- URL: https://www.wjgnet.com/2307-8960/full/v9/i17/4433.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i17.4433
Ganglion cysts are common masses found adjacent to large joints including the knee, shoulder, ankle, and hip joints[1,2]. However, neurologic symptoms are less frequently observed in juxta-articular ganglion cyst arising from the hip than in those arising from other joints[1,2]. In hip-related ganglion cysts, these symptoms may be classified as intraneural and extraneural[3]. Extraneural ganglion cysts are more common than intraneural ganglion cysts (INGCs)[2-4]. Spinner et al[5] have proposed the articular (synovial) theory to explain the development of INGCs[5]. Based on this theory, the articular branch connected to the synovial joint through a labral/capsular rent is a conduit for intraneural propagation along the parent nerve[5].
INGCs are relatively rare and are characterized by non-neoplastic and mucinous cystic formation within the epineurium of a peripheral nerve[1]. INGCs commonly involve the common peroneal nerve at the knee, but cases of proximal sciatic nerve or lumbosacral plexus involvement are extremely uncommon[1].
INGCs involving proximal sciatic nerve or lumbosacral plexus may mimic common causes of sciatica, such as lower lumbosacral herniated disc or foraminal stenosis[6,7]. Under-recognized disease entity may delay the diagnosis and appropriate treatment. This report presents the case of an INGC involving the lumbosacral plexus arising from the articular branch of the hip joint. A literature review of previously published articles, mostly isolated case reports on INGCs of the proximal sciatic nerve or lumbosacral plexus, was performed. We present the following case in accordance with the CARE reporting checklist.
A previously healthy 65-year-old woman who had been experiencing left buttock pain radiating to the dorsum of the foot for 2 years visited my spine clinic.
She had sudden onset of left buttock pain 2 years ago; the pain slowly radiated to the dorsum of the foot and worsened over time. Prior to visiting the clinic, she underwent lumbar spine magnetic resonance imaging (MRI) and abdominal computed tomography scan for the evaluation of left buttock pain. She was managed conservatively. However, the condition did not improve. She received physiotherapy, pain killers, and epidural injections based on a presumptive diagnosis of spinal stenosis and varicose vein for 2 years in other hospitals.
The patient had a free previous medical history.
Upon presentation at the clinic, her pain was aggravated by sitting and walking for a long time. When walking 500 m or sitting on the chair, she experienced sensory loss in the dorsum of the left foot. However, she had no significant previous medical history or surgeries. Physical examination revealed no atrophy and dilated veins in both lower extremities. According to the motor examination, there was no definite weakness on both lower limbs. Hypoesthesia to light touch and pin prick was observed on the dorsum of the right foot and lateral side of the right calf. Deep tendon reflex revealed a mild decrease in ankle reflex at the left side. The results of the straight-leg-raise test, femoral nerve stretching test, Patrick test, and flexion, adduction, and internal rotation test were negative. Moreover, the range of motion of the hip joint and lumbar spine and pedal pulses were normal.
The results of the electrodiagnostic evaluations, including motor and sensory nerve conduction studies, H-reflex test, and electromyography, were normal.
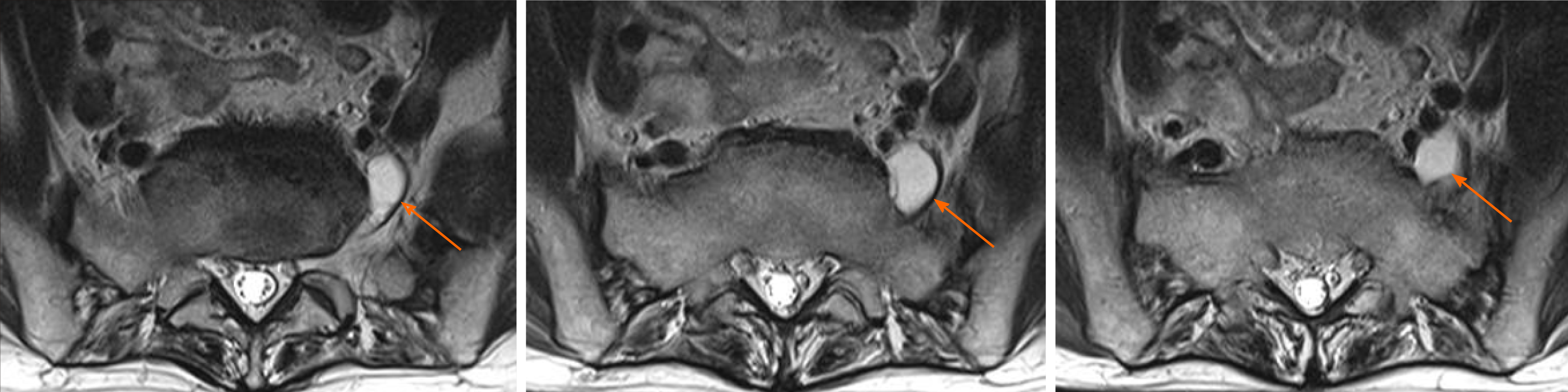
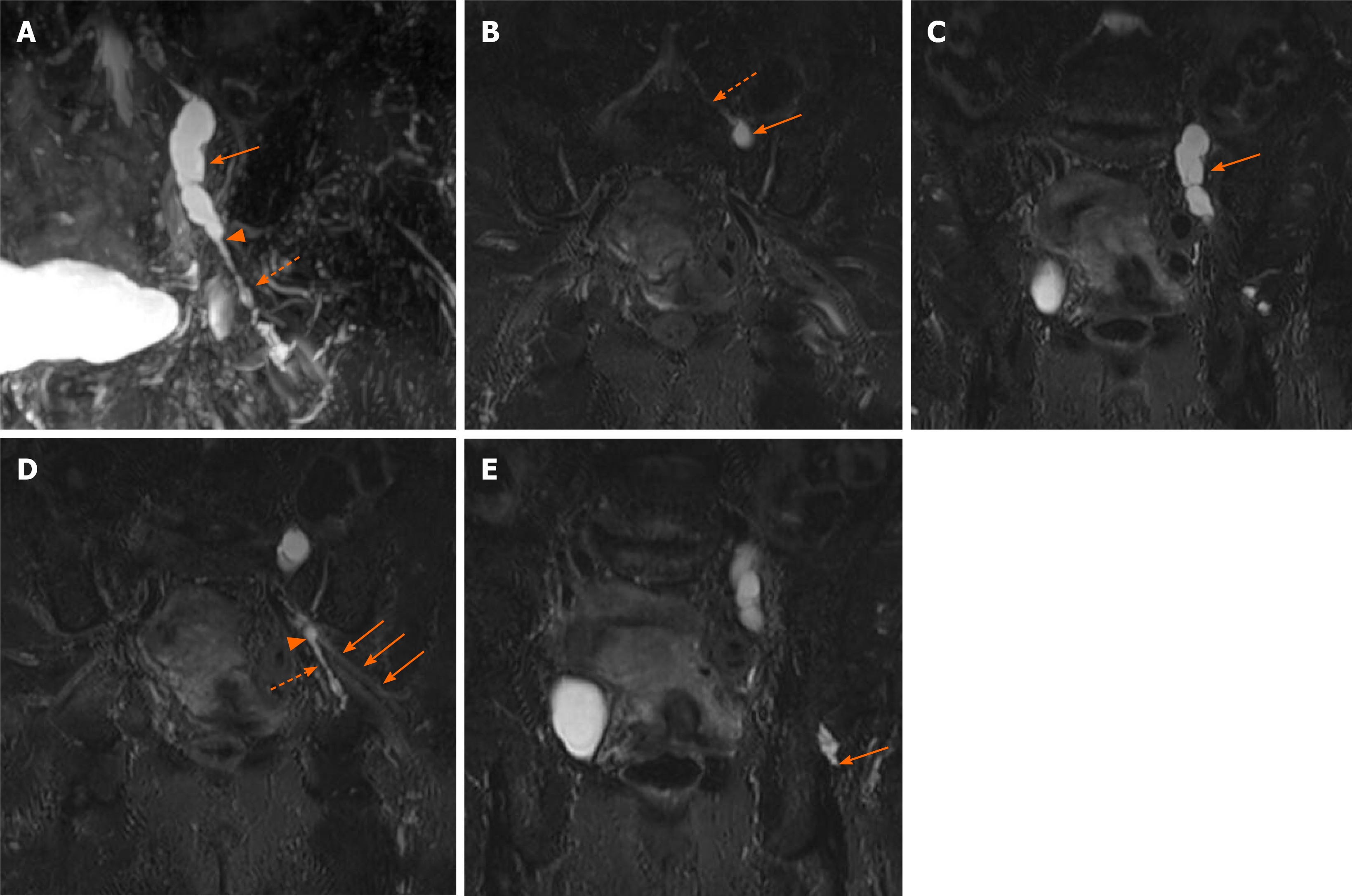
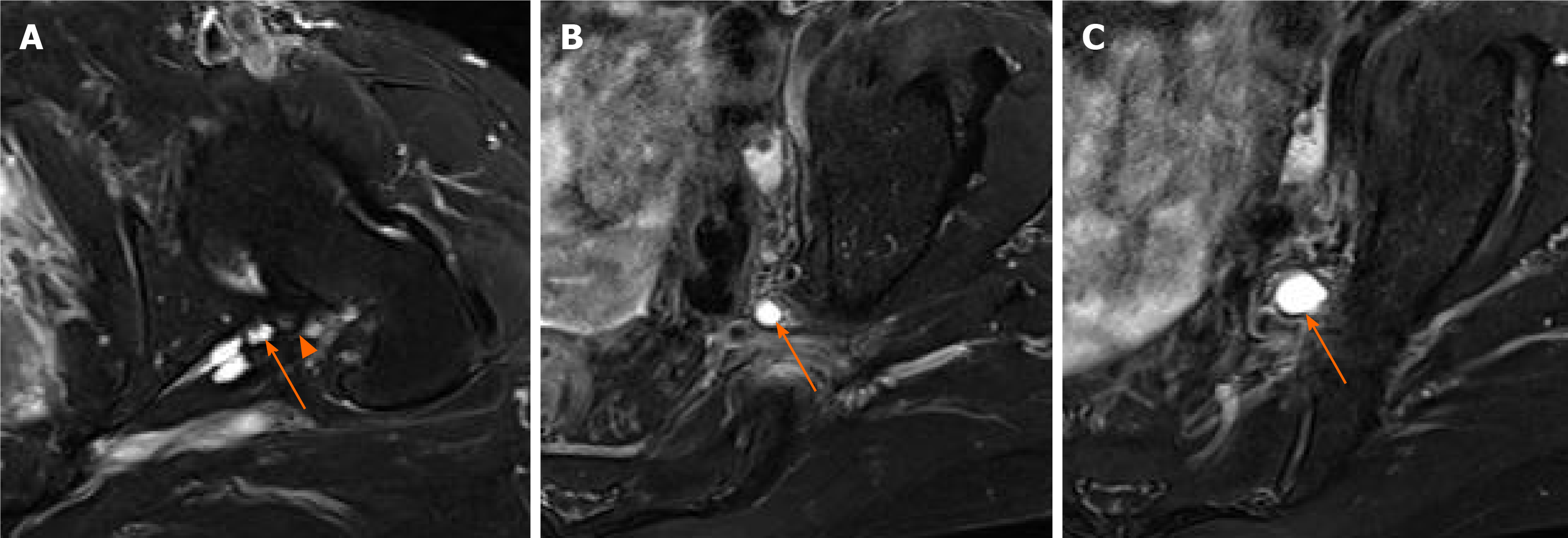
A retrospective review of previous lumbar spine MRI findings revealed no significant evidence of spinal stenosis. However, a cystic mass was observed in the left L5-S1 extraforaminal space (Figure 1). The lesion was indicative of an INGC because of its location along the path of the L5 spinal nerve. The patient was not aware of the cystic lesion. Thus, to confirm the nature and extent of the cystic mass, hip MRI, including high-resolution magnetic resonance neurography (MRN), was recommended. High-resolution MRN revealed an INGC arising from the articular branch of the hip joint, which extended to the lumbosacral plexus and L5 spinal nerve (Figure 2). Moreover, a degenerative change in the posterior labrum was observed (Figure 3A). The cystic lesion had a tubular-like feature from the termination of the articular branch to the level of the sciatic notch, where crossover at the level of the sciatic nerve and/or lumbosacral plexus occurs (Figure 2). However, the balloon-like feature above the crossover expanded to the far-lateral extraforaminal space at the L5-S1 level along the left L5 spinal nerve (Figures 2, 3B, and 3C).
The patient was diagnosed with INGC arising from the articular branch of the hip joint based on high-resolution MRN.
Hip arthroscopic surgery was performed to confirm and remove the communication between the intra-articular space and the articular branch of the hip joint. Arthroscopic examination revealed a mild degenerative change in the posterosuperior portion of the acetabular labrum with synovitis. During arthroscopic debridement of the posterior labrum, a cystic opening within the intra-articular space was detected; cyst decompression was then performed to drain the fluid from the ganglion cyst within the articular branch of the sciatic nerve.
She experienced significant pain relief in the left leg with mild residual tingling sensation on the dorsum of the foot during the 6-mo follow-up.
An extensive literature search was performed on PubMed, Scopus, and KoreaMed. The combined search terms used were as follows: (“intraneural ganglion cyst” OR “intraneural ganglia” OR “synovial ganglion” OR “intraneural cyst” OR “intraneural cystic degeneration”) and (“hip” OR “pelvis” OR “sciatic” OR “lumbosacral plexus”). A total of 220 studies were identified after the initial search. Then, these studies were assessed for eligibility based on the inclusion criteria: The studies should discuss proximal sciatic or lumbosacral plexus INGCs arising from the hip joints and include MRI findings. Articles related to extraneural ganglion cyst, obturator nerve-related INGCs, and sciatic nerve-related INGCs arising from the knee joints were excluded. We found five studies with nine patients. Table 1 presents patient characteristics, clinical manifestations, electrodiagnostic and MRI findings, treatment methods, and prognosis in all cases, including the current case.
| No. | Ref. | Male/age | Clinical presentations or exam | Electrodiagnosis | MRI findings | Treatments | Outcomes | Follow-up MRI (interval from treatment) | ||
| Shape | Intra-articular communication | Intrapelvic extension | ||||||||
| 1 | Kim et al[12], 2019 | M/46 | Radicular pain. Ankle dorsiflexor 0, big toe extensor 0 | Plexopathy | Serpentile channel-like expansion and fusiform cyst expansion | Yes | Yes | Arthroscopic debridement and caspsulotomy | Pain–partial relief. Motor–partial improvement | No evidence of recurrence (18 mo) |
| 2 | Panwar et al[13], 2017 | NA/NA | NA | NA | Balloon-like cyst expansion | Yes | Yes | NA | NA | NA |
| 3 | Briem et al[6], 2016 | M/48 | Radicular pain. No weakness | Normal | Pearl-necklace-like form | Yes | Yes | Posterolateral approach | Pain–partial relief | No evidence of recurrence (12 mo) |
| 4 | Spinner et al[3], 2009 | M/23 | Peroneal dysfunction | NC | Balloon-like cyst expansion | Yes | Yes | Posterior transgluteal exploration and cyst evacuation | Pain-complete relief. Motor–partial improvement | Recurrent intraneural cyst within the articular branch (2 mo) |
| 5 | Spinner et al[3], 2009 | M/33 | Peorneal (dominant) and tibial dysfunction | Peroneal neuropathy at knee | Balloon-like cyst expansion | Yes | Yes | Anterior transabdominal approach | Pain-Partial relief. Motor–partial improvement | NC |
| 6 | Spinner et al[3], 2009 | M/53 | Normal exam | Normal | Pearl-necklace-like form & fusiform swelling | Yes | Yes | Offset procedure and labral repair, no decompression of intraneural cyst | Pain-Partial relief. Motor–partial improvement | No evidence of recurrence (2 yr) |
| 7 | Spinner et al[3], 2009 | F/55 | Peorneal (dominant) and tibial dysfunction | NC | Balloon-like cyst expansion | Yes | Questionable | Posterior transgluteal exploration and cyst evacuation | Pain-Partial relief. Motor–partial improvement | NC |
| 8 | Swartz et al[7], 2009 | F/37 | Radicular pain. Hip extension weakness | Plexopathy | Pearl-necklace-like form | Yes | Yes | Explorative decompression of perineural cyst | Pain–partial relief. Motor–partial improvement | No evidence of recurrence, but residual cyst (4 mo) |
| 9 | 1Sugita et al[17], 1997 | NA/NA | NA | NA | Fusiform cyst expansion to superior gluteal nerve | Yes | Yes | Subtotal cyst resection | Pain–partial relief. Motor–partial improvement | NA |
| 10 | Our case | F/65 | Radicular pain. No weakness | Normal | Balloon-like cyst expansion | Yes | Yes | Arthroscopic debridement and cyst decompression | Pain–partial relief | NA |
In 2016, Desy et al[1] performed a systematic review of the literature, and 648 cysts were found in 645 patients with 648 cysts[1]. In previous studies, the sciatic nerve or superior gluteal nerve was affected in only 10 patients. Moreover, three studies conducted by Desy et al[1], which did not include MRI findings or were not written in English language, and one article about a questionable cystic lesion (whether intraneural or extraneural) were excluded from the present literature review[8-11]. After the studies conducted by Desy et al[1], three cases report[6,12,13] were published. The diagnosis of INGCs of the peroneal nerve is increasing because MRI is now commonly performed. Moreover, large INGCs of the peroneal nerve around the knee joint, which is the most commonly involved area, are easily palpated, and ultrasonography can be performed to identify these lesions. By contrast, INGCs around the hip are often characterized by radicular pain. Thus, physicians often misjudge this pain as a symptom of back problems. The hip and joint joints are anatomically similar as they are surrounded by the labrum. Labral lesions in both the hip and shoulder joints are common. In the shoulder joints, suprascapular neuropathy associated with paralabral cyst is frequently observed. However, INGCs of the suprascapular nerve have not been discussed in depth[14-16]. Based on the author’s opinion, INGCs of both the hip and shoulder joints have been underdiagnosed because of the lack of knowledge among physicians. Thus, future studies must involve high-resolution MRN to identify cystic lesions of the shoulder and hip joints and to confirm the communication between the articular branch and intra-articular space.
Patients’ age ranged from 23 to 65 years. Because INGCs seems to be originated from intra-articular branch, it might be related with underlying degenerative joint changes (such as arthritis, synovitis, labral tears, or femoroacetabular impingement)[3,4,6]. INGCs of the hip joint commonly seem to develop after the age of 40 years. There were five male and three female participants. All eight patients presented with radicular pain. Among them, five experienced weakness (n = 2, the peroneal nerve territory; n = 2, the peroneal and tibial nerve territory; and n = 1, the superior gluteal nerve territory). Three patients did not experience any weakness. Three of the six patients had electrodiagnostic abnormalities indicating axonal damage.
Studies about the clinical manifestations of INGCs arising from other joints are limited. Motor symptoms can range from no muscle weakness to almost foot drop. Motor weakness was more likely to affect personal division than tibial division. INGCs around the hip joints are typically characterized by radicular pain mimicking radiculopathy. Based on the clinical manifestations, INGCs are difficult to differentiate from radiculopathy. If there is no lesion in the lumbar spine that can be associated with radicular pain, the hip joint pathology must be comprehensively evaluated, with consideration of the possibility of INGCs.
INGCs of the articular branch of the hip joint have typical MRI findings. Typical cyst ascent phenomenon starting from the termination of the articular branch may be pathognomonic[3,4]. From the termination to the sciatic notch, the shape of cystic expansion can be tubular, serpentine channel-like, pearl necklace-like, or multiple interconnected cyst[3,4,6,7,12,13]. Rostral to the level of the sciatic notch (crossover point where the articular branch joins the proximal sciatic nerve and/or lumbosacral plexus), the cyst may be more expansile and can have a fusiform or balloon-like feature[3,6,7,12]. Moreover, it can extend to the level of the juxta-neural foramen, preferentially involving the L4 and L5 spinal nerve[3,4,6,7,12,13]. This finding explains why patients with L4 or L5 radiculopathy present with buttock or hip pain. Rostral extension to the intrapelvic space was observed in nine of ten patients. In one patient, extension into the pelvis was questionable. Two patients underwent high-resolution MRN, and one patient underwent high-resolution magnetic resonance (MR) arthrography. High-resolution MRN or MR arthrography revealed the direct connection between the hip joint and intraneural cyst in all three patients. These findings support the articular theory for the pathogenesis of INGCs. Although the role of high-resolution MRN in lumbosacral plexus lesions has not been clearly elucidated, a high-resolution MRI technique would be advantageous in detecting the presence of intra-articular communication of the articular branch and exact extent of cyst involvement preoperatively.
The open surgical treatment methods for INGCs include cyst resection, nerve resection with or without nerve transfer, and ligation of the articular branch[1,3]. The present literature review revealed that six patients underwent explorative open surgery with cystic evacuation or cyst decompression[3,6,7,17]. Moreover, two patients underwent arthroscopic debridement and cyst decompression, and only one underwent arthroscopic debridement and repair without cyst decompression[3,12]. There has been no standard treatment method for patients with INGCs arising from the hip joint. Based on the articular theory, ligation of the articular branch may be ideal[1]. However, this method has not been previously used for INGCs arising from the hip joint probably because of its surgical difficulty. With cyst resection, the extrapelvic portion of INGCs from the labrum to the sciatic notch can be excised[6]. However, approaching the intrapelvic portion can be difficult. Briem et al[6] have reported that even after partial resection, postoperative MRI revealed regression of a proximal cyst without any sign of residual cystic structures[6]. With the arthroscopic approach, cysts can be decompressed to drain the fluid from the ganglion cyst[12]. Arthroscopic treatment has a risk of recurrence because the synovial membrane is maintained[1]. The present literature review showed that three patients were managed with arthroscopic debridement and/or cyst decompression through the intra-articular cystic opening. The procedure was found to be effective in relieving symptoms. Thus, it can be an alternative treatment method.
Although INGCs arising from the hip joint are rare, they can cause typical radicular pain and mimic common L5 radiculopathy. Typical cyst ascent phenomenon starting from the termination of the articular branch on MRI is a crucial finding indicative of INGCs arising from the hip joint. High-resolution MRN can be helpful in identifying a possible joint connection in juxta-articular ganglia cysts, and arthroscopic debridement and cyst decompression can be alternative treatments to cyst resection.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Munakomi S S-Editor: Fan JR L-Editor: A P-Editor: Li JH
| 1. | Desy NM, Wang H, Elshiekh MA, Tanaka S, Choi TW, Howe BM, Spinner RJ. Intraneural ganglion cysts: a systematic review and reinterpretation of the world's literature. J Neurosurg. 2016;125:615-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 2. | Yang G, Wen X, Gong Y, Yang C. Sciatica and claudication caused by ganglion cyst. Spine (Phila Pa 1976). 2013;38:E1701-E1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Spinner RJ, Hébert-Blouin MN, Trousdale RT, Midha R, Russell SM, Yamauchi T, Sasaki S, Amrami KK. Intraneural ganglia in the hip and pelvic region. Clinical article. J Neurosurg. 2009;111:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Spinner RJ, Hébert-Blouin MN, Tanaka S, Amrami KK, Swartz KR, Fee DB, Sugita M. Hip- and pelvic-related intraneural ganglia. J Neurosurg. 2010;112:1353-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Spinner RJ, Atkinson JL, Tiel RL. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003;99:330-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 193] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Briem T, Haemmerle G, Kramers-de Quervain I, Leunig M. Synovial Ganglion of the Hip as a Rare Cause of L5 Radiculopathy: A Case Report. JBJS Case Connect. 2016;6:e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Swartz KR, Wilson D, Boland M, Fee DB. Proximal sciatic nerve intraneural ganglion cyst. Case Rep Med. 2009;2009:810973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Hasturk AE, Basmaci M, Canbay S, Harman F, Erten F. Painful lumbosacral plexopathy due to ganglion cyst: magnetic resonance image findings and treatment. J Musculoskelet Pain. 2013;21:75-80. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Hwang DS, Kang C, Lee JB, Cha SM, Yeon KW. Arthroscopic treatment of piriformis syndrome by perineural cyst on the sciatic nerve: a case report. Knee Surg Sports Traumatol Arthrosc. 2010;18:681-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Spinner RJ, Wang H, Hébert-Blouin MN, Skinner JA, Amrami KK. Sciatic cross-over in patients with peroneal and tibial intraneural ganglia confirmed by knee MR arthrography. Acta Neurochir (Wien). 2009;151:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Westerheide KJ, Karzel RP. Ganglion cysts of the shoulder: technique of arthroscopic decompression and fixation of associated type II superior labral anterior to posterior lesions. Orthop Clin North Am. 2003;34: 521-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Kim JL, Do JG, Yoon YC, Lim SJ, Sung DH. Intraneural Ganglion Cyst of the Sciatic Nerve Treated Using Arthroscopic Hip Surgery: A Case Report. PM R. 2019;11:895-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Panwar J, Mathew A, Thomas BP. Cystic lesions of peripheral nerves: Are we missing the diagnosis of the intraneural ganglion cyst? World J Radiol. 2017;9:230-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 14. | Prasad NK, Spinner RJ, Smith J, Howe BM, Amrami KK, Iannotti JP, Dahm DL. The successful arthroscopic treatment of suprascapular intraneural ganglion cysts. Neurosurg Focus. 2015;39:E11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Spinner RJ, Hébert-Blouin MN, Dahm DL, Amrami KK. Two different pathways for suprascapular intraneural ganglion cysts along two distinct articular branches from the glenohumeral joint. Clin Anat. 2010;23:462-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. J Bone Joint Surg Am. 2010;92:2348-2364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 17. | Sugita M, Terauchi T, Kusuzaki K, Hirasawa T. Intraneural ganglion arising from the superior gluteal nerve preoperatively diagnosed by MRI: a case report. Orthop Trauma Surg. 1997;40:99-102. |