Published online Jun 16, 2021. doi: 10.12998/wjcc.v9.i17.4408
Peer-review started: February 2, 2021
First decision: March 25, 2021
Revised: March 27, 2021
Accepted: April 7, 2021
Article in press: April 7, 2021
Published online: June 16, 2021
Processing time: 112 Days and 19.9 Hours
Four-level lumbar spondylolysis is extremely rare. So far, only 1 case has been reported in the literature.
A 19-year-old man presented with severe back pain irresponsive to conservative therapies for 2 years. Lumbar radiographs and two-dimensional computed tomography scan showed four segment lumbar spondylolysis on both sides of L2-L5. Lumbar magnetic resonance imaging showed normal signal in all lumbar discs. Because daily activities were severely limited, surgery was recommended for the case. The patient underwent four-level bilateral isthmic repair at L2-L5. During surgery, L2-L5 isthmi were curetted bilaterally, freshened, and then grafted with autologous iliac bone that was bridged and compressed with a pedicular screw connected to a sub-laminar hook by a short rod. The symptoms of back pain almost disappeared. He has been followed-up for 96 mo, and his symptoms have never recurred. Fusion was found in all repaired isthmi 14 mo after surgery according to evaluation of lumbar radiography and computed tomography scan.
We report here 1 case of four-level lumbar spondylolysis that was treated successfully with direct isthmic repair.
Core Tip: Four-level lumbar spondylolysis is extremely rare. So far, only 1 case has reported in the literature. In the present study, we report 1 case of four-level lumbar spondylolysis that was treated successfully with direct isthmic repair.
- Citation: Li DM, Peng BG. Surgical treatment of four segment lumbar spondylolysis: A case report . World J Clin Cases 2021; 9(17): 4408-4414
- URL: https://www.wjgnet.com/2307-8960/full/v9/i17/4408.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i17.4408
Four-level lumbar spondylolysis is extremely rare[1-3]. So far, only 1 case has been reported in the literature[4]. We report here 1 case of four-level lumbar spondylolysis that was treated successfully with direct isthmic repair.
A 19-year-old man presented with low back pain without radicular pain in both lower extremities for 2 years.
His back pain worsened from stretching and standing for a long time. He had no history of trauma. He rated himself as 7 on a 10-point visual analogue scale. Conservative treatment, such as rest, lumbosacral brace immobilization, oral non-steroidal anti-inflammatory drugs, and physical therapy, did not relieve his back pain, which seriously affected his daily activities.
He had no relevant traumatic history.
Physical examination revealed a reduced range of motion in the lumbar spine, especially with limited lumbar extension. Tenderness was noted over and beside L2-L5 spinous processes. Bilateral straight leg raising test was negative. The sensory, motor, and tendon reflexes of both lower limbs were normal.
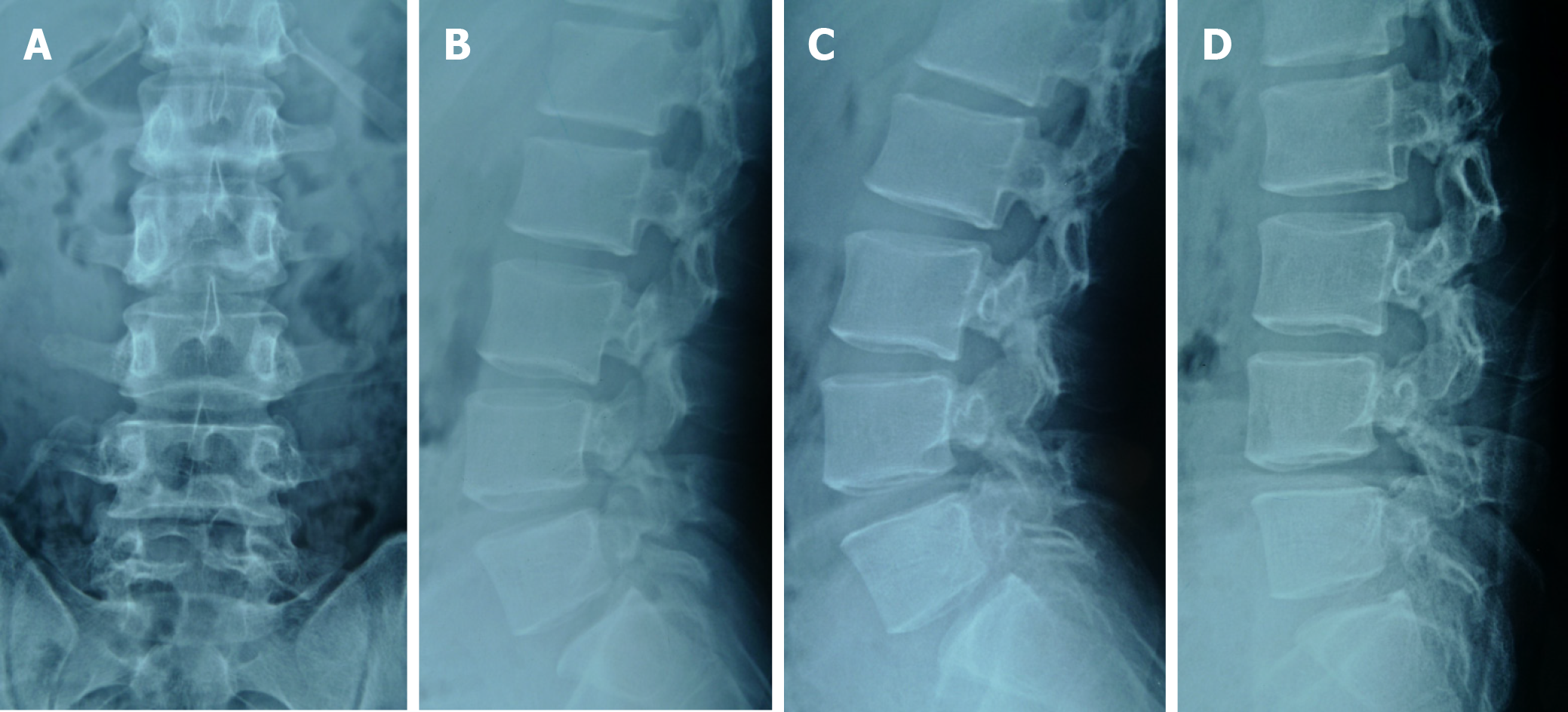
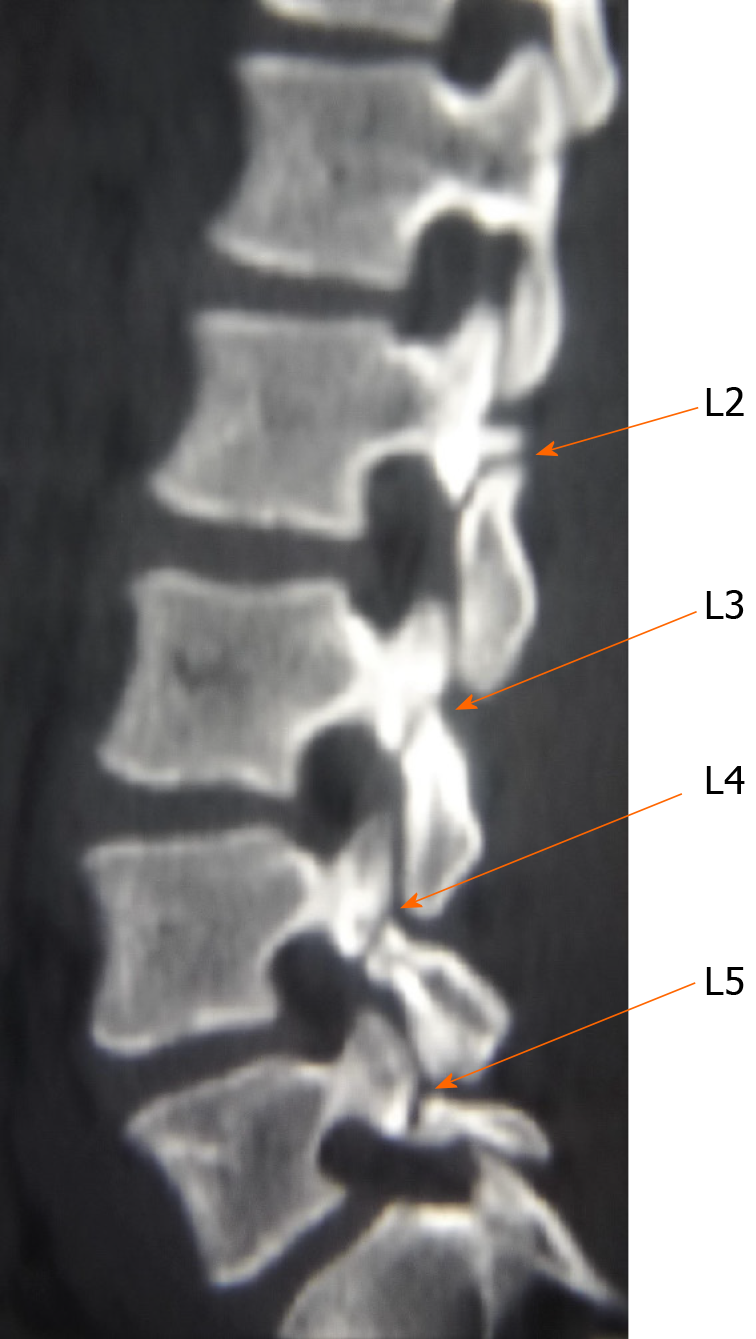
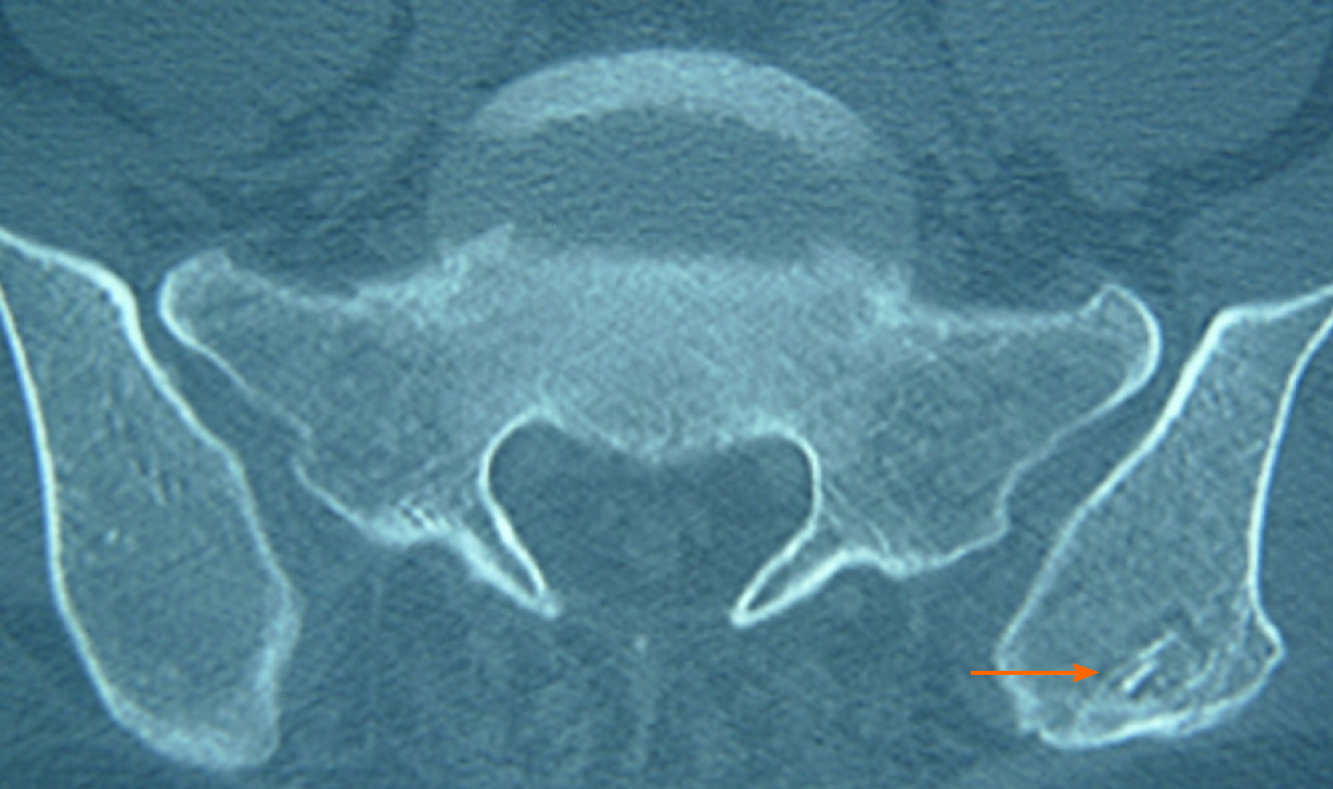
Lumbar dynamic radiographs showed no instability (Figure 1), two-dimensional computed tomography (CT) scan showed lumbar spondylolysis at bilateral L2-L5 levels (Figure 2), and lumbar magnetic resonance imaging showed no signs of lumbar disc degeneration (Figure 3). Because daily activities were severely limited, surgery was recommended for the case.
Four segment lumbar spondylolysis.
This case underwent a surgery of direct isthmic repair in eight lytic defects at bilateral L2-L5 levels. Under general anesthesia, the conventional posterior midline approach was used to expose L2-L5 spinous processes, lamina, and facet joints. Firstly, under the guidance of fluoroscopy, a 6.0 mm × 45 mm pedicle screw was implanted into the vertebral body. Secondly, the involved lysis area was scraped and freshened, and autologous iliac bone grafting was performed. Finally, the sub-laminar hook was placed and connected through a short rod under compression with corresponding pedicle screw. Subsequently, the remaining repair of seven lyses was completed in the same manner. Total operation time was 3.5 h, and blood loss was 350 mL. The neurological function of the patient remained intact after operation. A lumbosacral-brace was used for 3 mo.
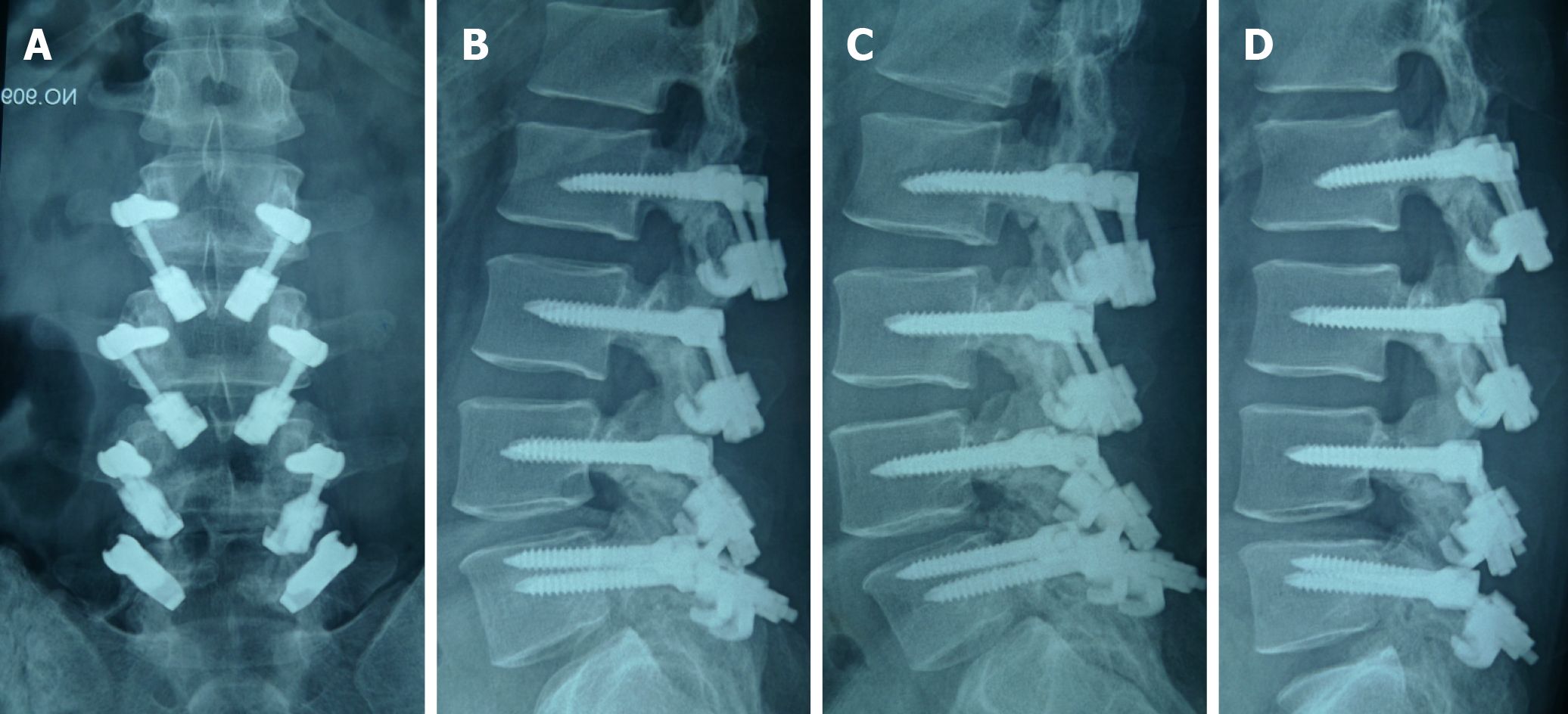
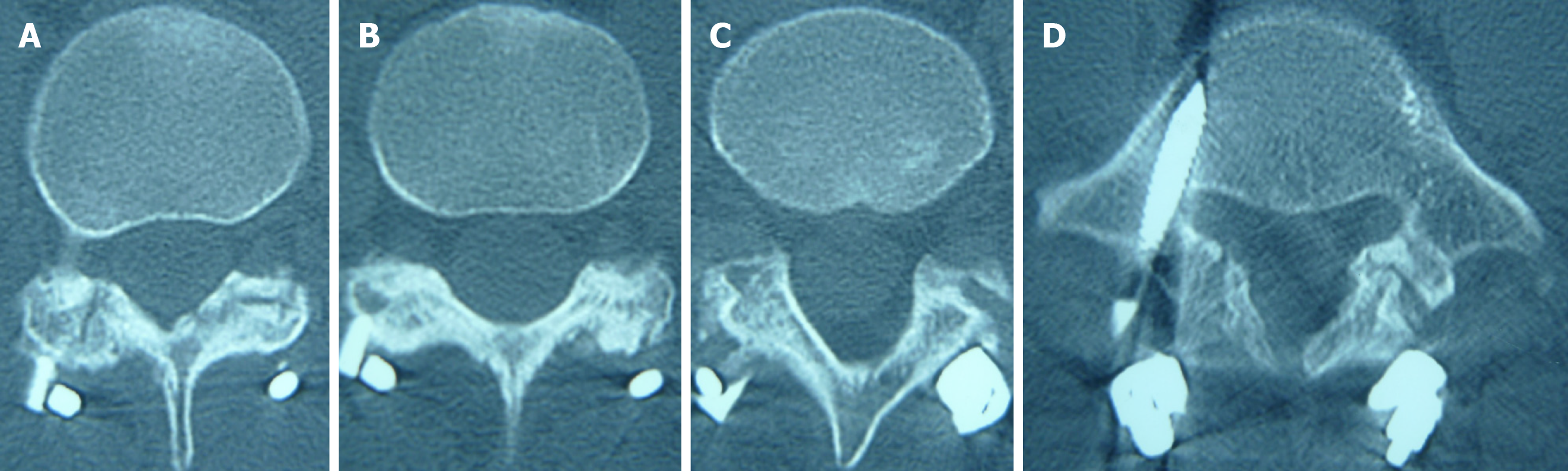
After the operation, the patient's back pain disappeared, and he returned to work 3 mo later. During the 8-year follow-up, he had no complaints of low back pain. The dynamic plain films showed that movement was retained (Figure 4). Bone healing was found in all eight lytic defects (Figure 5). After the donor site of iliac crest was filled with allogeneic bone, osteogenesis was formed (Figure 6).
Lumbar spondylolysis is a common cause of low back pain in adolescents. It occurs in about 6% of the population and is reported to be more common in men. It usually occurs in L5, accounting for more than 80% of patients with lumbar spondylolysis. Multi-segmental spondylolysis is rare[1]. According to Ravichandran[2], multilevel lumbar spondylolysis only accounts for 1.48% of patients with spondylolysis. The incidence rate of three level lumbar spondylolysis is very low, less than 0.1% of lumbar spondylolysis[3]. To our knowledge, only 1 case of four segment lumbar spondylolysis has been reported in the literature[4]. The possible causes of lumbar spondylolysis include dysplasia, excessive exercise, fatigue fracture, etc. The cause of multilevel lumbar spondylolysis is not clear. Ogawa et al[5] considered that the causes of multi-segmental lumbar spondylolysis are the same as single segmental lumbar spondylo
Treatment for multi-segmental lumbar spondylolysis is still controversial[5,7]. If lumbar spondylolysis occurs in adolescents, conservative treatment is usually the first choice[8]. Clinical observation found that new onset spondylolysis may be cured by restricting lumbar spine movement with a brace[2,5,9,10]. A retrospective study showed that a union rate of conservative treatment in adolescents was 76%[11]. However, about 90% of end-stage L5 spondylolysis patients are first diagnosed in adulthood. In addition, about 40% of cases had no sports history or low back pain experience in their growth period[12]. If patients with lumbar spondylolysis have low back pain, conservative treatment is ineffective, or imaging shows spondylolisthesis, surgical treatment is required[5]. Studies have observed that lumbar spondylolysis is often accompanied by degeneration of adjacent upper and lower discs[13]. Lumbar spondylolysis increases disc stresses at the affected as well as adjacent levels, which may lead to disc degeneration. However, increase in stresses and angular displace
For the surgical treatment of lumbar spondylolysis, several techniques have been reported in the literature[2,5,17,18], and these can be divided into two categories: The first is lumbar fusion, including interbody fusion and postero-lateral arthrodesis; the second is direct isthmic repair, bone grafting, fusion, and fixation. Several surgical techniques using various internal fixation devices for direct repair of the pars defect were reported in the literature, including Buck’s operation, Morscher’s hook-screw system, Scotting’s wiring technique, segmental pedicle screw-hook fixation, and Gillet’s rod-screw construction[14,19,20].
How to choose the surgical method to treat lumbar spondylolysis is mainly based on whether there is the degeneration of the disc in the pathological segment[19]. If the lumbar disc in the pathological segment is normal, it usually indicates that the back pain is originated from the isthmus region, and the chosen surgical method should be direct isthmus repair. If the disc of the pathological segment is degenerative or protruded or has already had lumbar spondylolisthesis, the lumbar interbody fusion operation should be selected. According to the different conditions of the lumbar intervertebral discs, combination lumbar fusion and isthmus direct repair to treat multi-segmental lumbar spondylolysis should be performed[21]. Preoperative radiog
Our clinical results suggest that active surgical treatment should be considered in young patients with multilevel lumbar spondylolysis. According to the different conditions of the upper and lower discs of each damaged segment, the operation methods should be direct isthmic repair or combination direct isthmic repair and lumbar fusion. The incidence rate of multi-segmental lumbar spondylolysis is low in young people. More cases and longer follow-up time are needed to evaluate the curative effect.
We report here 1 case of four-level lumbar spondylolysis that was treated successfully with direct isthmic repair and pedicle screw-hook system fixation.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cawley DT S-Editor: Zhang H L-Editor: Filipodia P-Editor: Wang LL
| 1. | Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699-707. [PubMed] |
| 2. | Ravichandran G. Multiple lumbar spondylolyses. Spine (Phila Pa 1976). 1980;5:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Darnis A, Launay O, Perrin G, Barrey C. Surgical management of multilevel lumbar spondylolysis: a case report and review of the literature. Orthop Traumatol Surg Res. 2014;100:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Gu SX, Ma Y, Chen X, Cai XJ, Cui X, Bao D, Huang FS, Luo ZP, Li DW, Luo XB, Li LT. Re : He B, Yan L, Guo H, et al. The difference in superior adjacent segment pathology after lumbar posterolateral fusion by using 2 different pedicle screw insertion techniques in 9-year minimum follow-up. Spine (Phila Pa 1976) 2014;39:1093-8. Spine (Phila Pa 1976). 2014;39:E1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Ogawa H, Nishimoto H, Hosoe H, Suzuki N, Kanamori Y, Shimizu K. Clinical outcome after segmental wire fixation and bone grafting for repair of the defects in multiple level lumbar spondylolysis. J Spinal Disord Tech. 2007;20:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Wiltse LL. Etiology of spondylolisthesis. Clin Orthop. 1957;10:48-60. [PubMed] |
| 7. | Song D, Chen Z, Song D. Surgical treatment of double-level isthmic spondylolisthesis. J Neurosurg Spine. 2014;20:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Sairyo K, Sakai T, Yasui N, Dezawa A. Conservative treatment for pediatric lumbar spondylolysis to achieve bone healing using a hard brace: what type and how long? J Neurosurg Spine. 2012;16:610-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Park KH, Ha JW, Kim HS, Moon ES, Moon SH, Lee HM, Kim HJ, Kim JY. Multiple levels of lumbar spondylolysis - a case report -. Asian Spine J. 2009;3:35-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Eingorn D, Pizzutillo PD. Pars interarticularis fusion of multiple levels of lumbar spondylolysis. A case report. Spine (Phila Pa 1976). 1985;10:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Tatsumura M, Gamada H, Okuwaki S, Eto F, Nagashima K, Iwabuchi S, Ogawa T, Mammoto T, Hirano A, Yamazaki M. Union evaluation of lumbar spondylolysis using MRI and CT in adolescents treated conservatively. J Orthop Sci. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Sakai T, Goda Y, Tezuka F, Abe M, Yamashita K, Takata Y, Higashino K, Nagamachi A, Sairyo K. Clinical features of patients with pars defects identified in adulthood. Eur J Orthop Surg Traumatol. 2016;26:259-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Sairyo K, Goel VK, Faizan A, Vadapalli S, Biyani S, Ebraheim N. Buck's direct repair of lumbar spondylolysis restores disc stresses at the involved and adjacent levels. Clin Biomech (Bristol, Avon). 2006;21:1020-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52:432-437. [PubMed] |
| 15. | Chang JH, Lee CH, Wu SS, Lin LC. Management of multiple level spondylolysis of the lumbar spine in young males: a report of six cases. J Formos Med Assoc. 2001;100:497-502. [PubMed] |
| 16. | Hersh DS, Kim YH, Razi A. Multi-level spondylolysis. Bull NYU Hosp Jt Dis. 2011;69:339-343. [PubMed] |
| 17. | Liu X, Wang L, Yuan S, Tian Y, Zheng Y, Li J. Multiple-level lumbar spondylolysis and spondylolisthesis. J Neurosurg Spine. 2015;22:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Al-Sebai MW, Al-Khawashki H. Spondyloptosis and multiple-level spondylolysis. Eur Spine J. 1999;8:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Arai T, Sairyo K, Shibuya I, Kato K, Dezawa A. Multilevel direct repair surgery for three-level lumbar spondylolysis. Case Rep Orthop. 2013;2013:472968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Chung CH, Chiu HM, Wang SJ, Hsu SY, Wei YS. Direct repair of multiple levels lumbar spondylolysis by pedicle screw laminar hook and bone grafting: clinical, CT, and MRI-assessed study. J Spinal Disord Tech. 2007;20:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Dai LY. Disc degeneration in patients with lumbar spondylolysis. J Spinal Disord. 2000;13:478-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Delawi D, Dhert WJ, Castelein RM, Verbout AJ, Oner FC. The incidence of donor site pain after bone graft harvesting from the posterior iliac crest may be overestimated: a study on spine fracture patients. Spine (Phila Pa 1976). 2007;32:1865-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |