Published online Jun 16, 2021. doi: 10.12998/wjcc.v9.i17.4395
Peer-review started: February 1, 2021
First decision: February 28, 2021
Revised: March 10, 2021
Accepted: March 29, 2021
Article in press: March 29, 2021
Published online: June 16, 2021
Processing time: 113 Days and 22.6 Hours
Cor triatriatum sinistrum or cor triatriatum sinister is a rare congenital heart disease that accounts for approximately 0.1% of all cardiac abnormalities. It is defined as the presence of an anomalous septum that divides the left atrium into two cavities, and in most cases, it can be asymptomatic or less frequently very severe.
A 37-year-old pregnant woman visited our hospital. In the first trimester scan, we detected signs of fluid in the pericardium (pericardial effusion) that reached the atriums. In the third trimester, an anomalous septum in the left atrium suspicious of cor triatriatum sinister was detected. Expectant management was decided, the pregnancy evolved normally and resulted in uncomplicated delivery of a healthy child. The findings in the prenatal scan were confirmed by echocardiography and the diagnosis of cor triatriatum sinister was confirmed. The newborn was asymptomatic at all times.
We show expectant management of cor triatriatum sinister and suggest an association between this entity and early pericardial effusion.
Core Tip: Cor triatriatum sinistrum is a rare finding in a prenatal diagnosis ultrasound, probably as rare as early pericardial effusion. Pericardial effusion has been associated with some congenital heart defects as cardiac diverticulum, but to the best of our knowledge, it has never been shown as the debut of cor triatriatum sinistrum. In this case, we present a case of cor triatriatum sinistrum that debuts as early pericardial effusion and shows the prenatal management.
- Citation: Cánovas E, Cazorla E, Alonzo MC, Jara R, Álvarez L, Beric D. Prenatal diagnosis of cor triatriatum sinister associated with early pericardial effusion: A case report. World J Clin Cases 2021; 9(17): 4395-4399
- URL: https://www.wjgnet.com/2307-8960/full/v9/i17/4395.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i17.4395
Cor triatriatum sinister is defined as the presence of an abnormal septum that divides the entire left atrium into two cavities. It is a rare congenital heart disease that represents approximately 0.1% of all cardiac abnormalities[1]; the right variant cor triatriatum dexter is less frequent[2]. Early pericardial effusion during the first trimester can be observed in an isolated form in up to 2% pregnancies. Furthermore, it has a good prognosis in most cases, although it is associated with certain pathologies such as specific congenital heart defects or chromosomal abnormalities[3].
Cor triatriatum sinister frequently appears to be associated with other congenital heart diseases such as abnormal drainage of the pulmonary veins, cardiac diverticula, persistence of the superior vena cava[4-6], etc. However, there is no reported case of cor triatriatum sinister associated with pericardial effusion during the first trimester.
A 37-year-old female came to our hospital for a routine pregnancy check-up.
The patient was in the 12th wk of pregnancy.
The patient had no significant pathological history, and she was in her second pregnancy and with prior vaginal delivery. She had no relatives with cardiac disease or any malformations. Her first daughter was healthy.
The patient had no significant personal nor family history.
Patient´s physical examination did not show any abnormality. She was a healthy pregnant woman.
The first trimester aneuploidy screening was 1/518 for trisomy 21 and 1/10000 for trisomy 13 and 18. The cell-free fetal DNA test was performed due to the intermediate risk for trisomy 21 and the echographic findings suggestive of heart disease. It resulted in a risk for trisomy 21, 13, and 18 less than 1/10000, and male gender. The serologies were negative for human immunodeficiency virus, syphilis, hepatitis B, and toxoplasma, and the patient was immune to rubella. Her blood group was rhesus factor-positive and irregular antibody count was negative. No thyroid or glycemic changes were observed during the follow-up of this pregnancy.
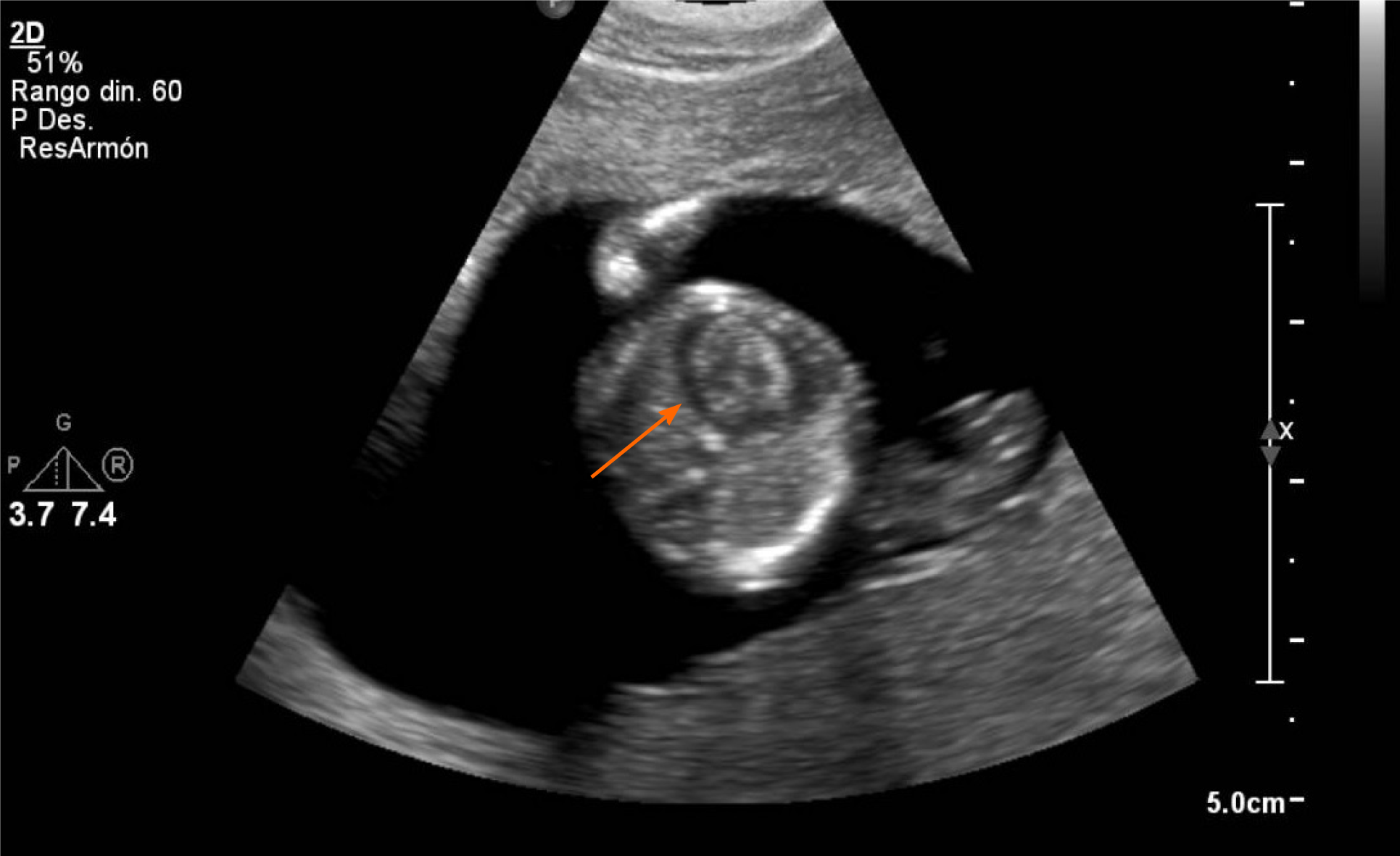
The first trimester ultrasound was performed, wherein a live fetus of 55 mm craniocaudal length was observed. Echocardiography revealed a pericardial effusion that reached the atrioventricular valves (Figure 1) in the heart with synchronous ventricular contractions, patent atrioventricular valves, and no ventricular asymmetry. Similarly, the outflow tracts of the great arteries were observed with correct arrangement, with preserved crossing. No abnormalities were observed at any other level.
Early echocardiography was performed at week 15 of pregnancy considering the finding of pericardial effusion on the first ultrasound. Pericardial effusion had disappeared, and echocardiography was normal. Morphological ultrasound was performed at week 21 of gestation, and echocardiography did not reveal any pathological findings, nor did the rest of the structures that were studied.
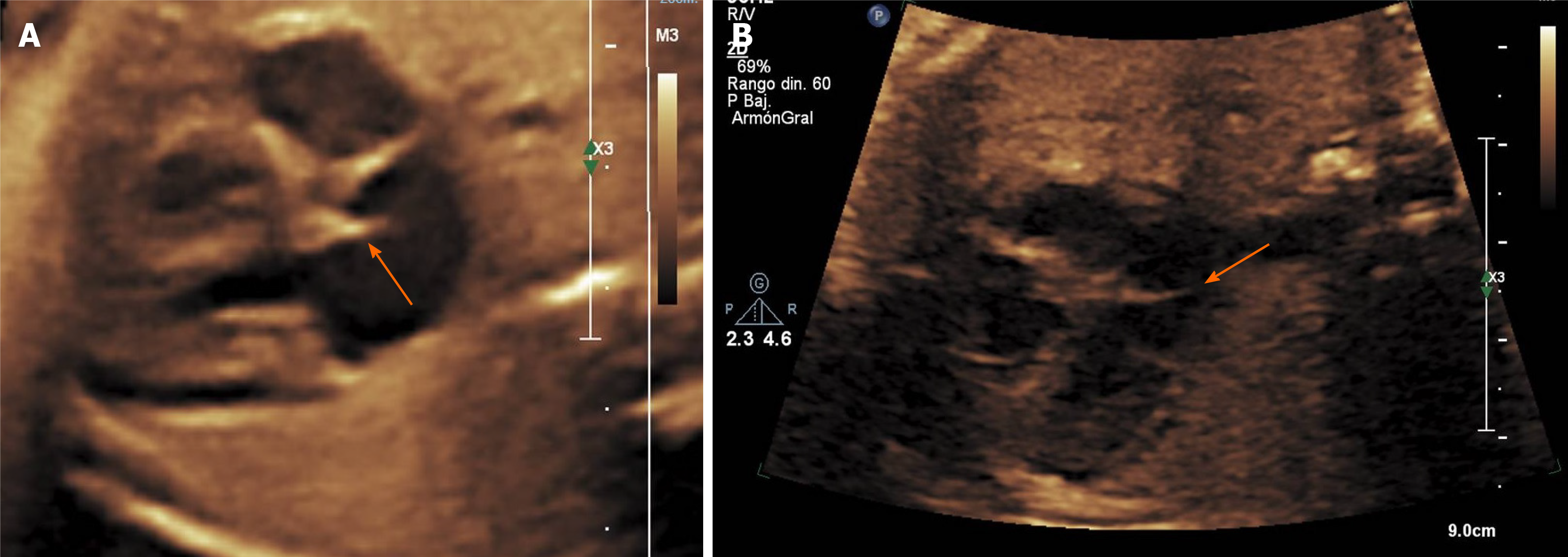
Echocardiography was performed at week 28 of gestation (Figure 2A), where a flap was observed in the left atrium, which a priori appeared to be inserted in the 7-mm interventricular septum, suggestive of cor triatriatum sinister. The other end of the lamina could not be observed, and it was not possible to determine if it completely divided the left atrium. Flow through the mitral and tricuspid valves did not present regurgitation, and there were no abnormalities in the myocardium. The remainder of the echocardiographic findings and the rest of the anatomical structures at all levels were normal. The ultrasounds at weeks 30 (Figure 2B), 33, and 37 confirmed the persistence of cor triatriatum sinister, but a complete path of the lamina crossing the entire atrium could not be verified at any time.
The final diagnosis of the presented case was cor triatriatum sinistrum.
We did not provide treatment. We decided on expectant follow-up ultrasound management every 4 wk.
The pregnancy resulted in vaginal delivery without complications. The newborn weighed 3402 g and presented an Apgar scores of 9, 10, and 10 at 1, 5, and 10 min, respectively, with good adaptation to extrauterine life without the need for special measures. Echocardiography was performed in subsequent follow-up during the first 26 mo of life, which showed a heart with normal-sized cavities, complete type I interventricular septum, and a complete patent fibrous septum in the left atrium crossing the atrium diagonally. It was unrelated to the mitral valve, dividing the atrium into two parts, without generating obstruction to the flow, consistent with cor triatriatum sinister. The four veins reached the left atrium, without acceleration within them, thus ruling out abnormal pulmonary drainage. The newborn was asymptomatic at all times.
Church had described this pathology in 1868[7]; however, a case of prenatal diagnosis of cor triatriatum sinister was first reported in 2011[8]. Since then, there have been few cases diagnosed before delivery and none were associated with pericardial effusion during the first trimester. Therefore, this case is the first report of early pericardial effusion during the first trimester associated with cor triatriatum sinister.
Pericardial effusion is an eminent pathological sign that is rare during the first trimester in the absence of fetal hydrops[9]. Since the first case recorded in 1995[10], cases of pericardial effusion associated with other cardiac malformations, especially cardiac diverticula[10,11] or cardiac tumors[12], have been published.
In this case, the associated malformation was diagnosed as cor triatriatum sinister, which despite being a rare heart disease, has several classifications according to membrane permeability such as the Loeffler classification[13] or the location of the septum and its relationship with the pulmonary veins, as the Lam et al[14] and Herlong et al[15] classifications. According to the Loeffler classification[13], it would be a case of cor triatriatum sinister type 3, with wide communication between both chambers, which entails minimal or absent hemodynamic repercussion. This is the mildest form of alteration according to this classification. If we use the Lam classifica
In this case, the management of pregnancy was expectant, with follow-up ultra
In conclusion, based on a literature review, we can deduce that the presence of early pericardial effusion during the first trimester is an indicator of cardiac malformations during the early stages of embryonic development[11]. These cardiac malformations that could not be detected early because of an ultrasound limitation due to the cardiac size could subsequently be diagnosed with fetal growth, and we should take into account the detection of early pericardial effusion as a factor of high suspicion of fetal heart disease.
In any case, whether due to its low incidence, the need for a high degree of suspicion for detection, or its low ultrasound expression, cor triatriatum sinister is an echocardiographic finding that is rare in intrauterine life and currently remains a diagnostic challenge.
A non-despicable amount of cardiac malformations could not be detected early because of an ultrasound limitation due to the cardiac size. That is why the role of early markers of cardiac defects as pericardial effusion in the prenatal diagnosis is so important. Early pericardial effusion could be the first manifestation of many cardiac malformations that includes cor triatriatum sinister, which needs a high degree of suspicion for detection due to its low ultrasound expression.
Manuscript source: Unsolicited manuscript
Specialty type: Obstetrics and gynecology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Okamoto T, Ozair A S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li JH
| 1. | Anderson JA, Kennelly MM. Successful management of antenatal presentation of cor triatriatum. Eur J Obstet Gynecol Reprod Biol. 2008;140:137-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Jha AK, Makhija N. Cor Triatriatum: A Review. Semin Cardiothorac Vasc Anesth. 2017;21:178-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Kyeong KS, Won HS, Lee MY, Shim JY, Lee PR, Kim A. Clinical outcomes of prenatally diagnosed cases of isolated and nonisolated pericardial effusion. Fetal Diagn Ther. 2014;36:320-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 4. | Maroun LL, Graem N, Skibsted L. Fetal cor triatriatum dexter: a report of two cases associated with nuchal edema in early second trimester. Pediatr Dev Pathol. 2008;11:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Dhoble A, Patel M, Shah I, Thakur RK, Abela GS. Cor triatriatum sinister with bicuspid aortic valve: a rare association. Clin Cardiol. 2009;32:E88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Kaneko T, Tsounias E, Douglas WI, Tsai FW. Cor triatriatum sinister with dilated coronary sinus from persistent left superior vena cava: a novel operative approach. Pediatr Cardiol. 2011;32:826-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Church WS. Congenital malformation of the heart: abnormal septum in left auricle. Trans Pathol Soc Lond. 1868;19:188-190. |
| 8. | Pruetz J, Detterich J, Trento L, Sklansky M. Prenatal diagnosis of cor triatriatum sinister in association with hypoplastic left heart syndrome. Pediatr Cardiol. 2011;32:818-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Benoit B, Murta MM, Leite J, Jeanty P. Intrathoracic fluid may be a normal finding at around 8 gestational weeks. Ultrasound Obstet Gynecol. 2007;30:188-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Carles D, Maugey-Laulom B, Habboud H, Alberti EM, Weichhold W, Léger F. Early prenatal diagnosis of ventricular diverticulum complicated by serous pericardial effusion. Prenat Diagn. 1995;15:778-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Garcia Rodriguez R, Rodriguez Guedes A, Garcia Delgado R, Roldan Gutierrez L, Castellano MM, Garcia Hernandez JA. Corrigendum to "Prenatal Diagnosis of Cardiac Diverticulum with Pericardial Effusion in the First Trimester of Pregnancy with Resolution after Early Pericardiocentesis". Case Rep Obstet Gynecol. 2017;2017:6207658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Yuan SM, Lin H. Fetal intrapericardial teratomas. Turk J Pediatr. 2019;61:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Loeffler E. Unusual malformation of the left atrium; pulmonary sinus. Arch Pathol (Chic). 1949;48:371-376. [PubMed] |
| 14. | Lam CR, Green E, Drake E. Diagnosis and surgical correction of 2 types of triatrial heart. Surgery. 1962;51:127-137. [PubMed] |
| 15. | Herlong JR, Jaggers JJ, Ungerleider RM. Congenital Heart Surgery Nomenclature and Database Project: pulmonary venous anomalies. Ann Thorac Surg. 2000;69:S56-S69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 4.1] [Reference Citation Analysis (0)] |