Published online Jun 16, 2021. doi: 10.12998/wjcc.v9.i17.4318
Peer-review started: January 13, 2021
First decision: February 11, 2021
Revised: February 24, 2021
Accepted: April 2, 2021
Article in press: April 2, 2021
Published online: June 16, 2021
Processing time: 133 Days and 6.8 Hours
Coronal shear fractures of the distal humerus are rare injuries and are technically challenging to manage. Open reduction and internal fixation (ORIF) has become the preferred treatment because it provides anatomical reduction, stable internal fixation, and early motion, but the optimal surgical approach remains controversial.
We report three cases of coronal shear fractures of the distal humerus treated successfully by ORIF via a novel surgical approach, in which lateral epicondyle osteotomy was performed based on the extended lateral approach. We named the novel surgical approach the lateral epicondyle osteotomy approach. All patients underwent surgical treatment and were discharged successfully. All patients had excellent functional results according to the Mayo elbow performance score. The average range of motion was 118° in flexion/extension and 172° in pronation/ supination. Only case 2 had a complication, which was implant prolapse.
We demonstrated that the lateral epicondyle osteotomy approach in ORIF is effective and safe for coronal shear fractures of the distal humerus.
Core Tip: Coronal shear fractures of the distal humerus are rare and technically challenging to manage. Open reduction and internal fixation (ORIF) has become the preferred treatment, but the optimal surgical approach remains controversial. We report three cases of coronal shear fractures of the distal humerus treated successfully by ORIF via the lateral epicondyle osteotomy approach, in which lateral epicondyle osteotomy was performed based on the extended lateral approach. Our management experience in the three cases demonstrated the effectiveness and safety of this novel approach.
- Citation: Li J, Martin VT, Su ZW, Li DT, Zhai QY, Yu B. Lateral epicondyle osteotomy approach for coronal shear fractures of the distal humerus: Report of three cases and review of the literature. World J Clin Cases 2021; 9(17): 4318-4326
- URL: https://www.wjgnet.com/2307-8960/full/v9/i17/4318.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i17.4318
Coronal shear fractures of the distal humerus are rare, accounting for 6% of distal humerus fractures and 1% of elbow fractures[1]. These fractures are technically challenging to manage due to their small size, associated osteochondral fragments, and propensity to displace, and they lead to limited elbow motion. Open reduction and internal fixation (ORIF)[2-10] has become the preferred treatment because it provides anatomical reduction, stable internal fixation, and early motion, but the optimal surgical approach remains controversial. Currently, the common surgical approaches include the anterolateral approach[2,3], posterior olecranon osteotomy approach[4-7], and extended lateral approach[7-10].
We report three cases of coronal shear fractures of the distal humerus treated successfully by ORIF via a novel surgical approach, in which lateral epicondyle osteotomy was performed based on the extended lateral approach. We named the novel surgical approach the lateral epicondyle osteotomy approach. We discuss the advantages and disadvantages of various surgical approaches with regard to our management experience.
Case 1: Right elbow and right upper arm pain accompanied by limited range of motion (ROM).
Case 2: Left elbow pain accompanied by limited ROM.
Case 3: Right elbow pain accompanied by limited ROM.
Case 1: A 57-year-old man was admitted to our hospital with right elbow and right upper arm pain accompanied by limited ROM for 12 d after he accidentally fell from a ladder and landed on his right hand.
Case 2: A 64-year-old man was admitted to our hospital with left elbow pain accompanied by limited ROM for 7 d after he accidentally fell onto his outstretched left hand when walking down stairs.
Case 3: A 31-year-old man was admitted to our hospital with right elbow pain accompanied by limited ROM for 3 d after he fell accidentally and landed on his right elbow.
Case 1 underwent ORIF of the left calcaneus fracture 4 years earlier. Cases 2 and 3 had no history of other diseases.
No family history to note.
Case 1: The physical examination revealed pain in the right elbow and right upper arm accompanied by limited ROM but no open wounds.
Case 2: The physical examination revealed pain in the left elbow accompanied by limited ROM but no open wounds.
Case 3: The physical examination revealed swelling and pain in the right elbow accompanied by limited ROM but no open wounds.
No obvious abnormalities were observed in the preoperative examinations.
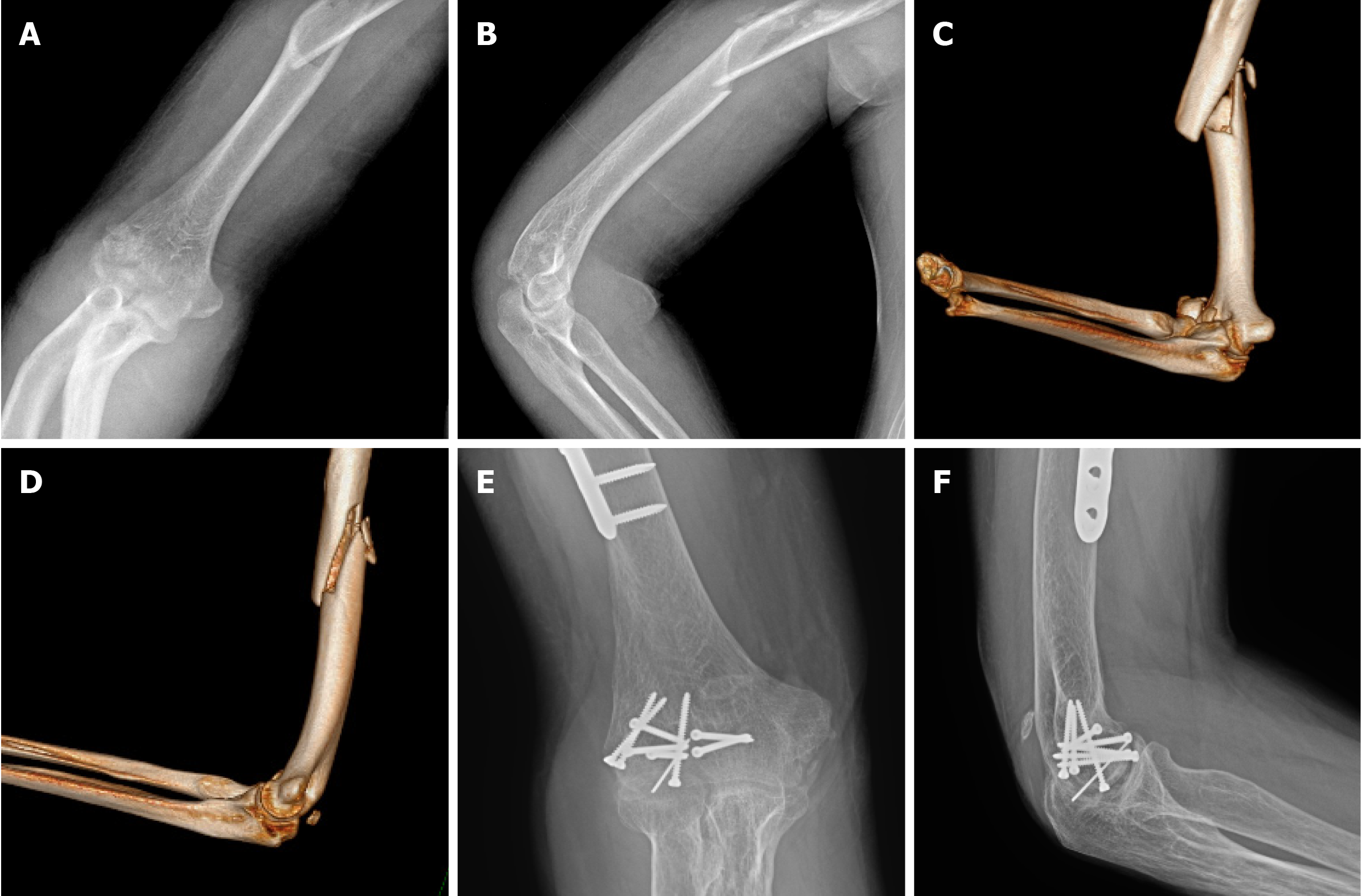
Case 1: Radiographs revealed a right humerus shaft fracture and right capitellar fracture (Figure 1A and B). A computed tomography scan revealed a right humerus shaft fracture and right capitellar and trochlea fractures (Figure 1C and D).
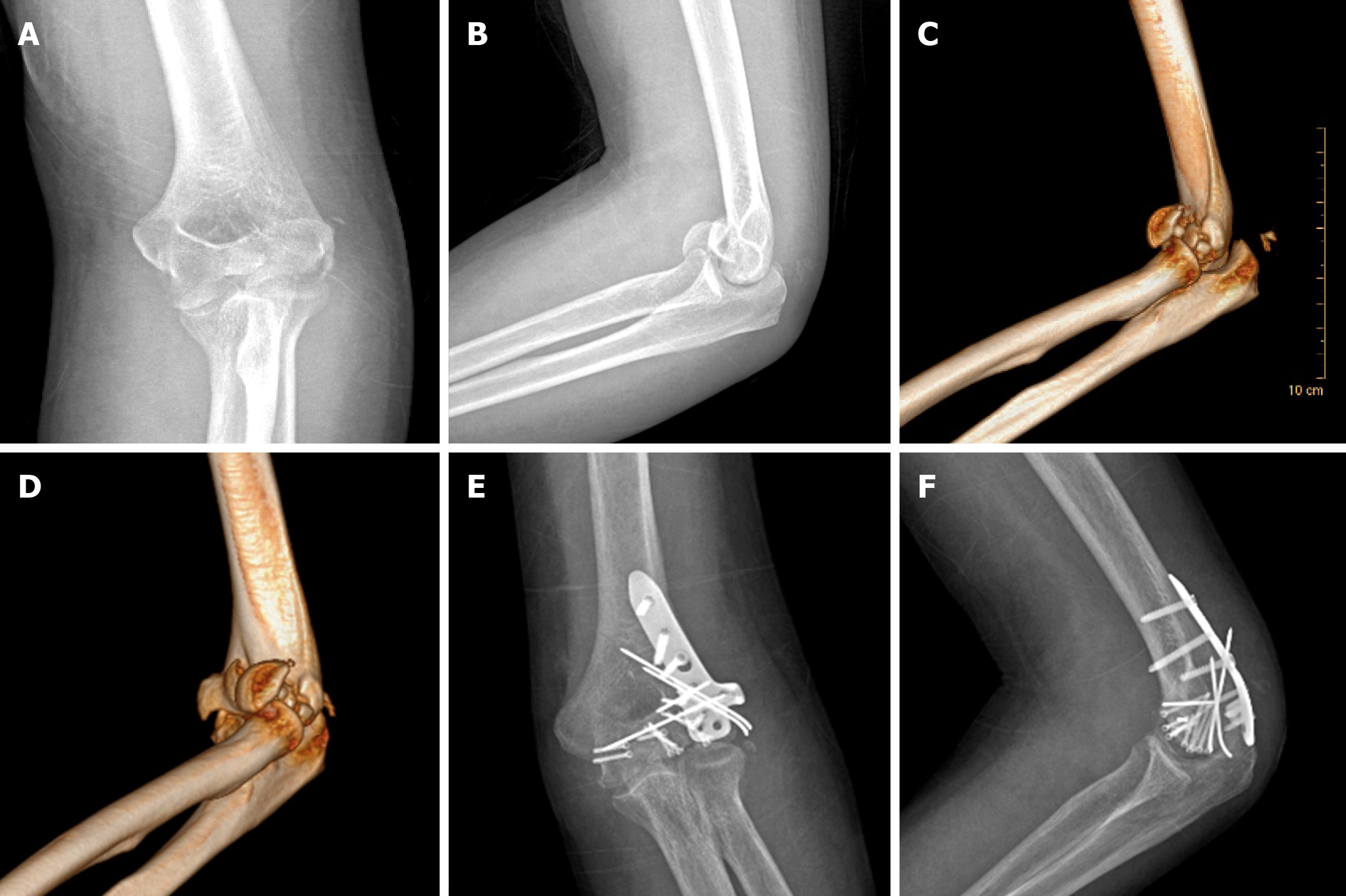
Case 2: Radiographs revealed left capitellar and trochlea fractures (Figure 2A and B). A computed tomography scan revealed left capitellar and trochlea fractures accompanied by a left olecranon avulsion fracture (Figure 2C and D).
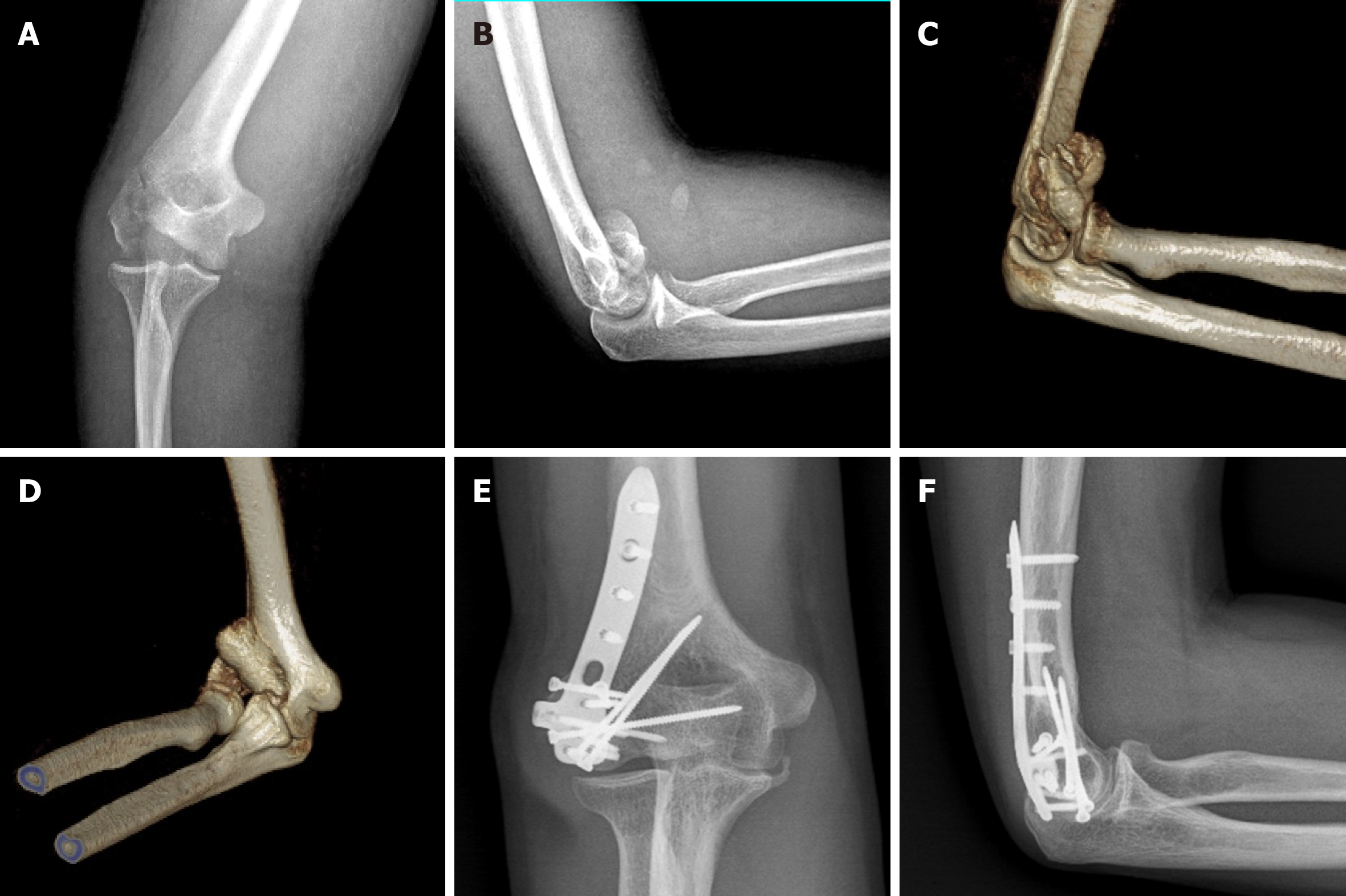
Case 3: Both radiographs and a computed tomography scan revealed right distal humerus fractures, including lateral epicondyle, capitellum, and trochlea fractures (Figure 3A-D).
The final diagnosis was coronal shear fractures of the right distal humerus (type 3A according to Dubberley et al[7]) and a right humerus shaft fracture.
The final diagnosis was coronal shear fractures of the left distal humerus (type 3B according to Dubberley et al[7]) accompanied by a left olecranon avulsion fracture.
The final diagnosis was coronal shear fractures of the right distal humerus (type 2B according to Dubberley et al[7]) accompanied by a lateral epicondyle fracture.
The examination performed after anesthesia showed that the affected elbow joint was not unstable in varus or valgus. The extended lateral approach was used in ORIF, and then, lateral epicondyle osteotomy was performed. The lateral epicondyle was mobilized distally along with the origins of the common wrist and digit extensor muscles and the lateral collateral ligament to provide ideal visualization of the distal humerus articular surface, thereby allowing the fracture fragments to be anatomically reduced under direct vision and the screws to be placed in the anterior-posterior direction. During surgery, fragmentation of the articular surface was noted, and both the capitellum and lateral trochlea were involved as separate fracture fragments. The fracture fragments were reduced and temporarily fixed with K-wires. First, six screws were placed as follows with countersinking: Five screws were placed in the anterior-posterior direction, and the remaining screw was placed in the distal-proximal direction. Then, a K-wire was inserted for bone stabilization. Finally, two lag screws were used to stabilize the osteotomy region. The right humerus shaft fracture was also treated by ORIF. Passive activities were encouraged starting on the second day after surgery.
The examination after anesthesia showed that the elbow joint was not unstable in varus or valgus. As in the first case, the extended lateral approach was used in ORIF, and then, lateral epicondyle osteotomy was performed. During surgery, we noted that the fracture involved the capitellum, medial trochlea, and posterior aspect of the lateral condyle. The fracture fragments of the capitellum and trochlea were sequentially reduced and temporarily fixed with K-wires; then, final fixation was performed by placing screws in the anterior–posterior direction and in the distal–proximal direction. All screws were inserted with the screw head buried beneath the articular surface. Three K-wires were retained. Finally, the posterolateral plate of the distal humerus was used to fix the osteotomy region and the fracture of posterior aspect of the lateral condyle at the same time. Regarding the olecranon avulsion fracture, after elevating the lateral aspect of the triceps from the distal humerus and the proximal olecranon, we removed the free fracture fragments and repaired the triceps tendon with two absorbable rivets. Passive activities were encouraged starting on the second day after surgery.
The examination after anesthesia showed that the elbow joint was unstable in varus but not unstable in valgus. The extended lateral approach was used in ORIF, and a lateral epicondyle fracture was noted. The origins of the lateral collateral ligament and the common extensor muscles were attached to the fracture piece, as in the lateral epicondyle osteotomies performed in the two cases above. During surgery, a large fracture fragment consisting of the capitellum and the medial trochlea was seen, and it was reduced and temporarily fixed with K-wires. Then, screws were placed in the anterior–posterior direction and in the lateral–medial direction for fixation. Finally, the fracture piece of the lateral epicondyle was reduced and fixed with a posterolateral plate of the distal humerus. Passive activities were encouraged starting on the second day after surgery.
At 12 mo after surgery, radiographs showed union without osteonecrosis (Figure 1E and F). At the 33-mo follow-up, the postoperative elbow ROM values were as follows, without pain or instability: Extension 33°, flexion 147°, pronation 86°, and supination 90°. The Mayo elbow performance score (MEPS) was 95 points (excellent), and the disability of the arm, shoulder, and hand (DASH) score was 10 points.
At 5.5 mo after surgery, radiographs showed union without osteonecrosis (Figure 2E and F). At 6 mo after surgery, the patient underwent hardware removal because of prominent implants, and during the second surgery, two K-wires and one loose screw were removed. At the 12.5-mo follow-up, the postoperative elbow ROM values were as follows, without pain or instability: Extension 21°, flexion 133°, pronation 78°, and supination 90°. The MEPS was 100 points (excellent), and the DASH score was 1.7 points.
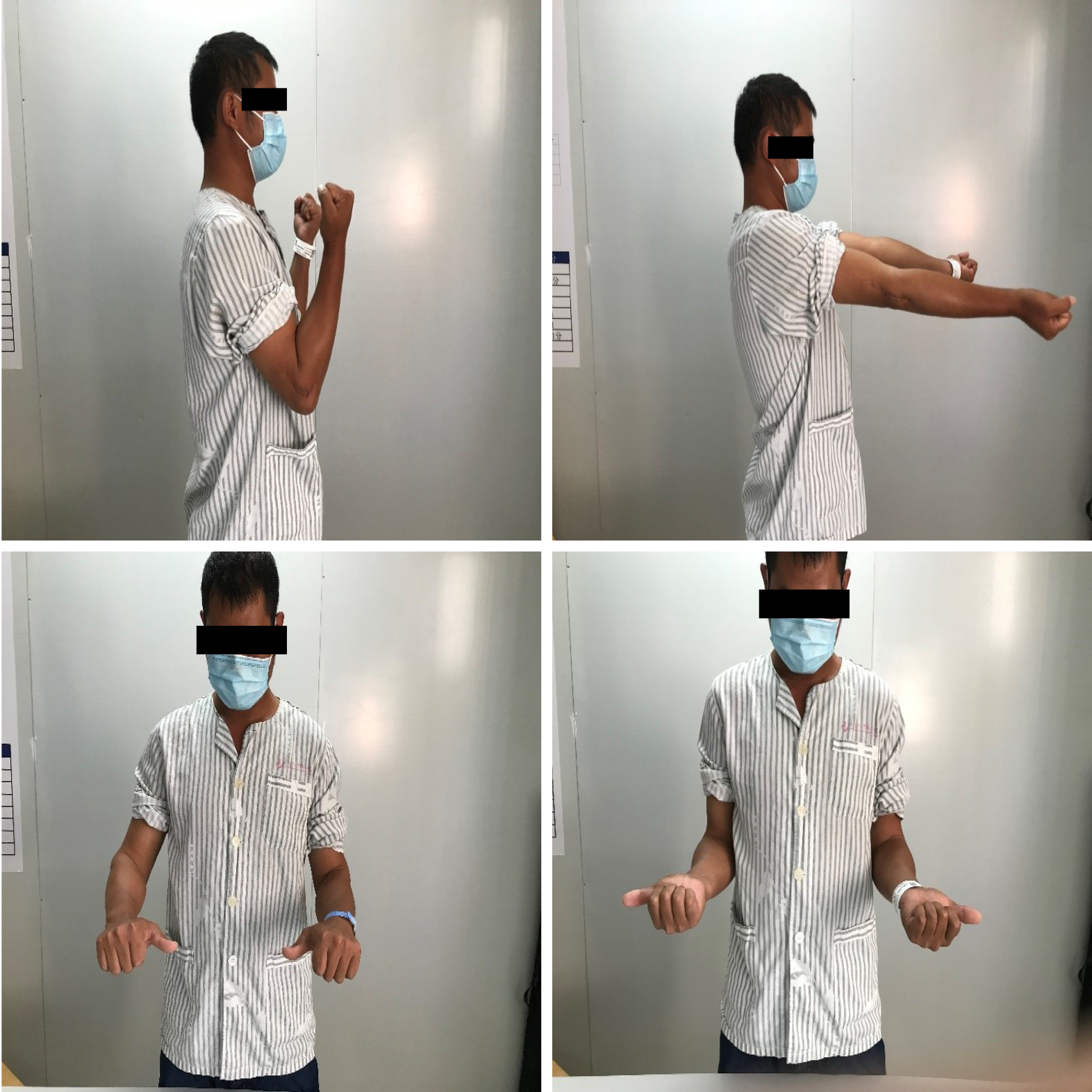
At 16 mo after surgery, radiographs showed union without osteonecrosis (Figure 3E and F). At the 20-mo final follow-up, the postoperative elbow ROM values were as follows, without pain or instability: Extension 0°, flexion 128°, pronation 82°, and supination 90° (Figure 4). The MEPS was 100 points (excellent), and the DASH score was 0 points.
Coronal shear fractures of the distal humerus are rare injuries, accounting for 6% of distal humeral fractures and 1% of elbow fractures[1]. With the development of digital imaging and computed tomographic scans, the complex nature of these fractures is now better understood[4,8]. These fractures are technically challenging to manage due to their small size, associated osteochondral fragments, and propensity to displace, and they can result in limited elbow motion. Compared to surgical treatments, nonsurgical treatments are often associated with worse results and more complications, such as elbow stiffness, traumatic arthritis, chronic pain, and joint instability[11-13]. The surgical treatments available include ORIF[2-10], arthroscopic surgery[14,15], fragment resection[16,17], and elbow joint replacement[18,19]. Currently, ORIF has become the preferred treatment because it provides anatomical reduction, stable internal fixation, and early motion. However, the limited surgical window and associated osteochondral fragments make it difficult to obtain stable internal fixation to allow early motion. Therefore, it is essential to choose a suitable surgical approach that provides direct visualization of fracture fragments and facilitates anatomical reduction of the fracture fragments to achieve good outcomes.
The common surgical approaches include the anterolateral approach, posterior olecranon osteotomy approach, and extended lateral approach. Some surgeons choose the anterolateral approach[2,3], which starts from the space between the biceps brachii and brachioradialis. The anterolateral approach provides access to trochlear fragments and facilitates anatomical reduction in the fragment without the need for lateral collateral ligament complex (LCLC) release or olecranon osteotomy, but it is difficult to stabilize the fractures with posterior comminution via this approach alone. Therefore, ORIF through the anterolateral approach is suitable for Dubberley type A fractures. However, the surgical dissection of this approach is relatively cumbersome, given the risk of neurovascular injury to the structures of the fossa cubitalis.
The posterior olecranon osteotomy approach[4-7] has been used frequently in ORIF for coronal shear fractures of the distal humerus, because it can provide the widest exposure of the articular surfaces of the distal humerus[20,21]. This approach is especially suitable for capitellar and trochlea fractures combined with posterior comminution of the lateral or medial condyle. The disadvantages of the posterior olecranon osteotomy approach include the need for additional internal fixation of the osteotomy and the risk of complications related to osteotomy, such as olecranon pain, nonunion, delayed healing, malunion, and implant prolapse[7,22,23].
We prefer the extended lateral approach[7-10]. A skin incision that is centered on the lateral epicondyle and extended from the lateral column of the distal humerus to approximately 2 cm distal to the radial head is made. The common origin of the wrist and digit extensor muscles along with the anterior capsule is elevated anteriorly as a full-thickness sleeve. A continuous full-thickness anterior soft-tissue flap is created by connecting the distal Kocher space to the proximal exposed region. However, due to obstruction from the LCLC, this approach does not provide adequate visualization of the trochlear fragments or facilitate anatomical reduction of the fragments. In cases in which the fracture involves the trochlea, the LCLC may need to be released to provide adequate visualization of the trochlear fragments[7,10,24]. However, this additional procedure increases the risk of posterolateral rotatory instability due to laxity of the lateral collateral ligament[25]. Mighell et al[26] thought that release of LCLC would affect the blood supply of the capitellum, thus affecting fracture healing. Therefore, we performed lateral epicondyle osteotomy based on the extended lateral approach to provide ideal visualization of the medial trochlea fragments and permit direct reduction and screw placement in the anterior–posterior direction. Concerning screw fixation, the ideal direction of implantation is still controversial. Sano et al[6] showed that screws placed in the posterior–anterior direction fail to fix thin fragments because the threads do not completely pass through them. Additionally, given the cancellous screw’s solid core and higher ratio of the outer-to-inner diameter, anterior-to-posterior screw insertion without countersinking may be more biomechanically robust than headless screws as well as countersunk anterior-to-posterior screws and posterior-to-anterior screws, although no direct comparisons have been made[27,28]. Matache et al[29] conducted an anatomical study and indicated that there is a nonarticulating zone for screw placement along the anterior aspect of the lateral trochlear ridge throughout the normal elbow ROM. The use of a partially threaded cancellous screw inserted anterior-to-posterior into this region without countersinking could theoretically improve the stability of some fractures that extend into the anterolateral aspect of the trochlea. Therefore, the lateral epicondyle osteotomy approach may be superior to the olecranon osteotomy approach regarding the direction of screw implantation.
In lateral epicondyle osteotomy, two hollow lag screws or the posterolateral plate of the distal humerus can be used for fixation. Regarding Dubberley type B fractures, the posterolateral plate of the distal humerus can simultaneously fix the osteotomy region and the fractured posterior aspect of the lateral condyle. The plate ensures firm internal fixation for early postoperative functional exercises and maximizes the motion of elbow joint function[8,30-32].
In conclusion, we report three cases of coronal shear fractures of the distal humerus treated by ORIF via the lateral epicondyle osteotomy approach and discuss the advantages and disadvantages of various surgical approaches. According to our management experience, the lateral epicondyle osteotomy approach is reliable and potentially useful for coronal shear fractures of the distal humerus. However, due to the limited number of cases and the short follow-up time in this study, additional high-quality clinical research needs to be conducted to verify the practicality of this surgical approach.
The three patients had excellent functional results according to the MEPS. The average ROM was 118° in flexion/extension and 172° in pronation/supination. Only case 2 had one complication, which was implant prolapse. Our experience regarding the management of these three cases initially proved the effectiveness and safety of the lateral epicondyle osteotomy approach.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Sousa Arantes Ferreira G S-Editor: Liu M L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Morrey BF, Sanchez-Sotelo J, Morrey ME. Morrey’s the Elbow and Its Disorders. 5th ed. Philadelphia, PA: Elsevier, 2018. |
| 2. | Imatani J, Morito Y, Hashizume H, Inoue H. Internal fixation for coronal shear fracture of the distal end of the humerus by the anterolateral approach. J Shoulder Elbow Surg. 2001;10:554-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Malki AA, Salloom FM, Wong-Chung J, Ekri AI. Cannulated screw fixation of fractured capitellum: surgical technique through a limited approach. Injury. 2000;31:204-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Guitton TG, Doornberg JN, Raaymakers EL, Ring D, Kloen P. Fractures of the capitellum and trochlea. J Bone Joint Surg Am. 2009;91:390-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Ashwood N, Verma M, Hamlet M, Garlapati A, Fogg Q. Transarticular shear fractures of the distal humerus. J Shoulder Elbow Surg. 2010;19:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Sano S, Rokkaku T, Saito S, Tokunaga S, Abe Y, Moriya H. Herbert screw fixation of capitellar fractures. J Shoulder Elbow Surg. 2005;14:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Dubberley JH, Faber KJ, Macdermid JC, Patterson SD, King GJ. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am. 2006;88:46-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 8. | Ring D, Jupiter JB, Gulotta L. Articular fractures of the distal part of the humerus. J Bone Joint Surg Am. 2003;85:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 168] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Ring D. Open reduction and internal fixation of an apparent capitellar fracture using an extended lateral exposure. J Hand Surg Am. 2009;34:739-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Sen MK, Sama N, Helfet DL. Open reduction and internal fixation of coronal fractures of the capitellum. J Hand Surg Am. 2007;32:1462-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Alvarez E, Patel MR, Nimberg G, Pearlman HS. Fracture of the capitulum humeri. J Bone Joint Surg Am. 1975;57:1093-1096. [PubMed] |
| 12. | Stricker SJ, Thomson JD, Kelly RA. Coronal-plane transcondylar fracture of the humerus in a child. Clin Orthop Relat Res. 1993;(294):308-311. [PubMed] |
| 13. | Ochner RS, Bloom H, Palumbo RC, Coyle MP. Closed reduction of coronal fractures of the capitellum. J Trauma. 1996;40:199-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Kuriyama K, Kawanishi Y, Yamamoto K. Arthroscopic-assisted reduction and percutaneous fixation for coronal shear fractures of the distal humerus: report of two cases. J Hand Surg Am. 2010;35:1506-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Mitani M, Nabeshima Y, Ozaki A, Mori H, Issei N, Fujii H, Fujioka H, Doita M. Arthroscopic reduction and percutaneous cannulated screw fixation of a capitellar fracture of the humerus: a case report. J Shoulder Elbow Surg. 2009;18:e6-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Grantham SA, Norris TR, Bush DC. Isolated fracture of the humeral capitellum. Clin Orthop Relat Res. 1981;(161):262-269. [PubMed] |
| 17. | Fowles JV, Kassab MT. Fracture of the capitulum humeri. Treatment by excision. J Bone Joint Surg Am. 1974;56:794-798. [PubMed] |
| 18. | Frankle MA, Herscovici D Jr, DiPasquale TG, Vasey MB, Sanders RW. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma. 2003;17:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 211] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 19. | McKee MD, Veillette CJ, Hall JA, Schemitsch EH, Wild LM, McCormack R, Perey B, Goetz T, Zomar M, Moon K, Mandel S, Petit S, Guy P, Leung I. A multicenter, prospective, randomized, controlled trial of open reduction--internal fixation vs total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg. 2009;18:3-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 270] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 20. | Wu ZZ, Wang JD, Ji XX, Ma ZJ, Wu JH, Wang QG. Surgical exposures of the distal humeral fractures: An anatomical study of the anterior, posterior, medial and lateral approaches. Chin J Traumatol. 2018;21:356-359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Wilkinson JM, Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg. 2001;10:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 158] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Deluise A, Voloshin J. Current management of distal humerus fractures. Curr Opin Orthop. 2006;17:340-347. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Allende CA, Allende BT, Allende BL, Bitar I, Gonzalez G. Intercondylar distal humerus fractures--surgical treatment and results. Chir Main. 2004;23:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | McKee MD, Jupiter JB, Bamberger HB. Coronal shear fractures of the distal end of the humerus. J Bone Joint Surg Am. 1996;78:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 190] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | O’Driscoll SW. Acute, Recurrent, and Chronic Elbow Instabilities. In: Norris TR. Orthopaedic Knowledge Update: Shoulder and Elbow 2. Rosemont, IL: The American Academy of Orthopaedic Surgeons, 2002: 313-323. |
| 26. | Mighell M, Virani NA, Shannon R, Echols EL Jr, Badman BL, Keating CJ. Large coronal shear fractures of the capitellum and trochlea treated with headless compression screws. J Shoulder Elbow Surg. 2010;19:38-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | Elkowitz SJ, Polatsch DB, Egol KA, Kummer FJ, Koval KJ. Capitellum fractures: a biomechanical evaluation of three fixation methods. J Orthop Trauma. 2002;16:503-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 28. | Burkhart KJ, Nowak TE, Appelmann P, Sternstein W, Rommens PM, Mueller LP. Screw fixation of radial head fractures: compression screw vs lag screw--a biomechanical comparison. Injury. 2010;41:1015-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Matache BA, Culliton K, Chang Y, Cron GO, Pollock JW. Lateral Trochlear Ridge: A Non-Articulating Zone for Anterior-to-Posterior Screw Placement in Fractures Involving the Capitellum and Trochlea. JBJS. 2019;101:e75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Mighell MA, Harkins D, Klein D, Schneider S, Frankle M. Technique for internal fixation of capitellum and lateral trochlea fractures. J Orthop Trauma. 2006;20:699-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Ruchelsman DE, Tejwani NC, Kwon YW, Egol KA. Open reduction and internal fixation of capitellar fractures with headless screws. J Bone Joint Surg Am. 2008;90:1321-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 32. | Goodman HJ, Choueka J. Complex coronal shear fractures of the distal humerus. Bull Hosp Jt Dis. 2005;62:85-89. [PubMed] |