Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3773
Peer-review started: January 9, 2021
First decision: January 17, 2021
Revised: January 30, 2021
Accepted: March 17, 2021
Article in press: March 17, 2021
Published online: May 26, 2021
Processing time: 121 Days and 19.5 Hours
Trauma is the leading cause of death in young adults up to the age of 45 years. Hemothorax is a frequent consequence of penetrating thoracic trauma, and is usually associated with pneumothorax and pneumoderma. Intercostal arterial bleeding or intrathoracic hemorrhage occurs after penetrating thoracic trauma, and uncontrolled bleeding is the main cause of death.
In this case report, a patient who developed a right hemopneumothorax after penetrating thoracic trauma was examined. A 19-year-old male patient, who was brought to the emergency room with a penetrating stab injury to the posterior of the left hemithorax, was diagnosed with a right hemopneumothorax after physical examination and thoracic imaging. Chest tube thoracostomy was performed as the initial intervention. Bleeding control was achieved with right posterolateral thoracotomy in the patient, who developed massive hemorrhage after 1 h and hemodynamic instability. The patient recovered and was discharged on the fourth postoperative day.
Contralateral hemopneumothorax that accounts for 30% of thoracic traumas and can be encountered in penetrating thoracic traumas requiring major surgery in 15-30% of cases was emphasized and the contralateral development mechanism was addressed.
Core Tip: Trauma is the leading cause of death in young adults up to the age of 45 years. Hemothorax is a frequent consequence of penetrating thoracic trauma, and is usually associated with pneumothorax and pneumoderma. Contralateral thoracic trauma is rare and easily overlooked in the initial evaluation. Here, we review the clinical presentation, radiographic features, diagnosis and treatment for contralateral hemopneumothorax after penetrating thoracic trauma.
- Citation: İşcan M. Contralateral hemopneumothorax after penetrating thoracic trauma: A case report. World J Clin Cases 2021; 9(15): 3773-3778
- URL: https://www.wjgnet.com/2307-8960/full/v9/i15/3773.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i15.3773
Trauma is the leading cause of death in young adults up to the age of 45 years[1]. Thoracic trauma, which is the third most common trauma after cranial and limb trauma, accounting for 25% of all trauma-related deaths, can create a domino effect in survival by affecting the functioning of other systems involving vital organs and leading to oxygenation imbalance of the impaired cardiopulmonary system[2,3]. In penetrating thoracic trauma, accounting for 30% of thoracic trauma cases, 15%-30% of patients require major surgery as a result of hemothorax and pneumothorax, which are among the primary outcomes of this injury[4]. The outcomes of penetrating trauma depend on the route that the penetrating object follows within the thorax[5].
We present a patient with penetrating thoracic trauma to emphasize that this injury can increase the risk of contralateral hemithorax.
A 19-year-old male patient presented to the emergency department with back pain and dyspnea after a penetrating stab injury.
The patient was brought to the emergency room area within 30 min after the injury.
The patient had no history of other illness and had no known allergies.
The patient had no family history of illness.
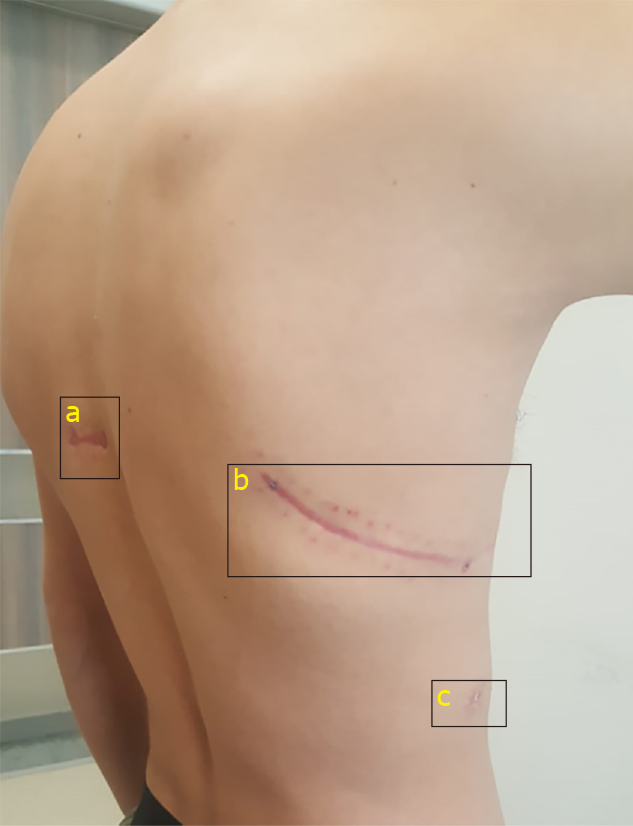
On physical examination, the patient was conscious, cooperative, and oriented. In the posterior left hemithorax, the injury site (possibly caused by a 3 cm long sharp object) was observed at the fourth rib level, between the left border of the spinal line and the medial border of the left scapula. There was no active bleeding or air leak. A pneumoderma was present around the wound, which was approximately 2 cm in diameter and caused crepitation. The patient’s respiratory sounds were reduced in the right hemithorax. His systolic blood pressure was 100 mmHg, heart rate was 112 beats/min, and respiratory rate was 12 breath/min. The partial pressure of oxygen (PaO2) was 95% in room air.
Arterial blood gas pH was 7.36, PaCO2 was 36.3 mmHg, PaO2 was 92 mmHg, and lactate level was 1.4 mmol/L. In the blood tests, leukocytosis was observed (13600/mm3), while other values were normal. His electrocardiogram revealed sinus tachycardia.
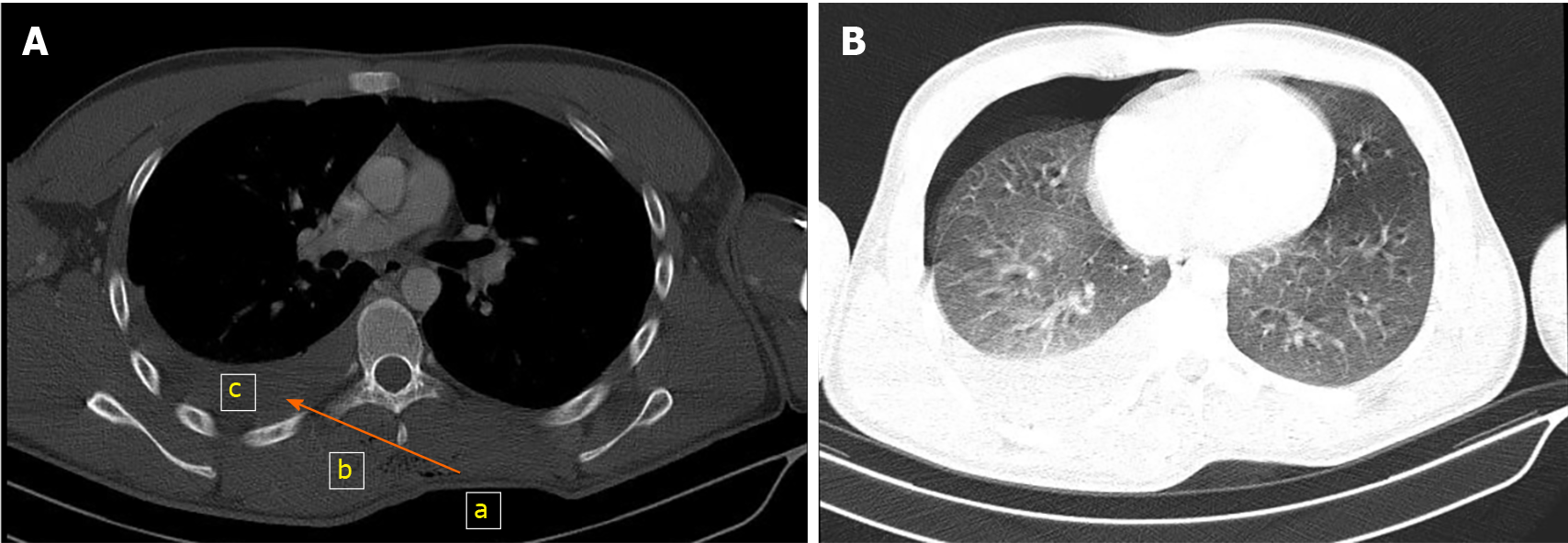
Computed tomography (CT) of the thorax showed a right hemopneumothorax and pneumoderma around the penetration site of the sharp object. No pathology was visualized in the left hemithorax (Figure 1).
Contralateral right hemopneumothorax after penetrating thoracic trauma.
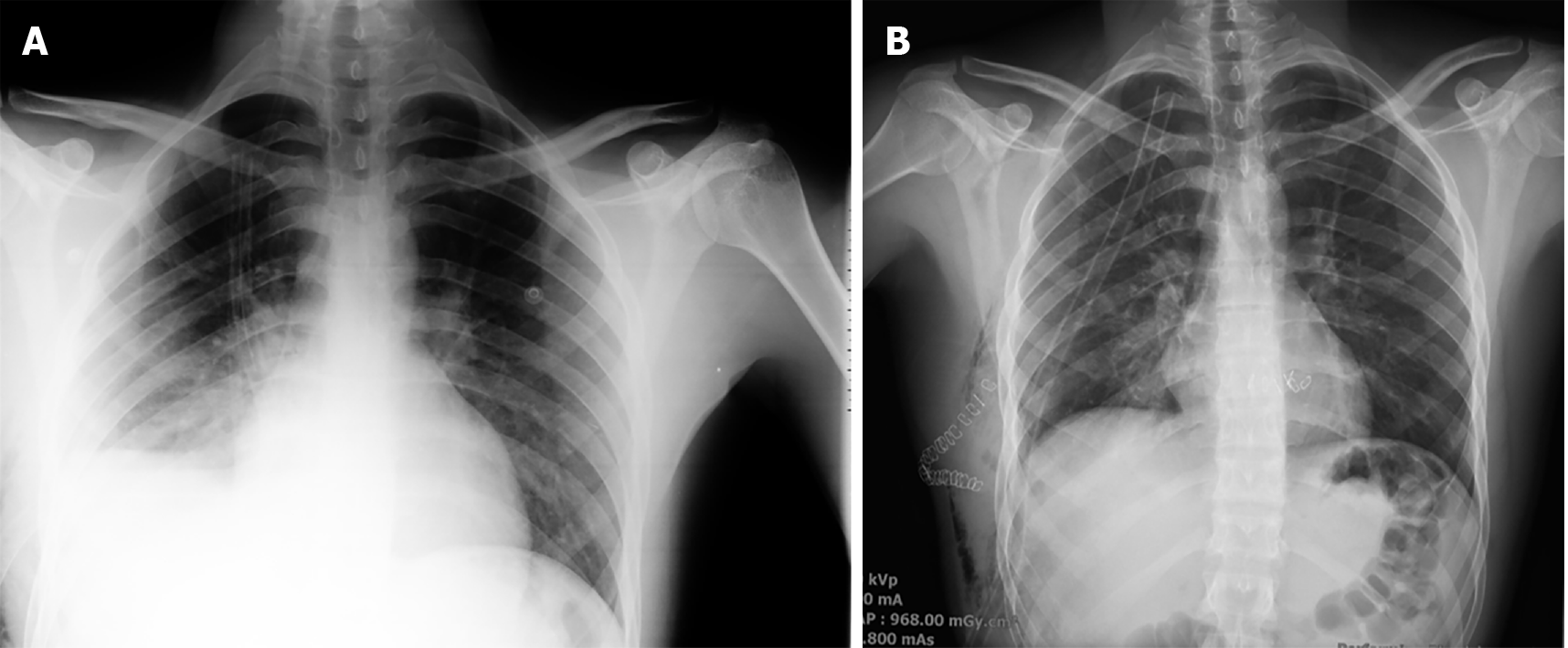
After the tube thoracostomy procedure was performed, with a 32 F chest tube inserted at the seventh intercostal space in the lateral direction under local anesthesia, 700 cc hemorrhagic drainage and air leak were observed. A posteroanterior chest X-ray was taken immediately afterwards and showed that the pneumothorax line almost completely regressed, but an increased density consistent with hematoma was present in the right hemothorax base (Figure 2A). There was no additional drainage in the first hour of the patient’s follow-up in the emergency room and the blood tests revealed leukocytosis (17680/mm3) along with a decrease in hemoglobin from 15.2 g/dL to 12.9 g/dL, while other values were within normal range. During transfer of the patient from the emergency room to the thoracic surgery ward using a stretcher, massive drainage of 1600 cc was observed in the chest drain, which developed within minutes. His blood pressure was 60/40 mmHg and heart rate was 124 beats/min. The patient underwent emergency right posterolateral thoracotomy, with the diagnosis of massive hemorrhage. About 1000 cc hematoma/hemorrhagic fluid was evacuated from the right hemithorax cavity. The hemorrhage focus in the right hemithorax posterior fifth intercostal artery that was injured by the sharp object was sutured. A laceration site of 2 cm in length that caused the air leak in the right lower lobe posterior segment was sutured. The patient received 3 U of erythrocyte suspension and 1 U of fresh frozen plasma replacement perioperatively. A 36 F chest drain was placed from the previous drain site, and the operation was completed without any complication (Figure 2B).
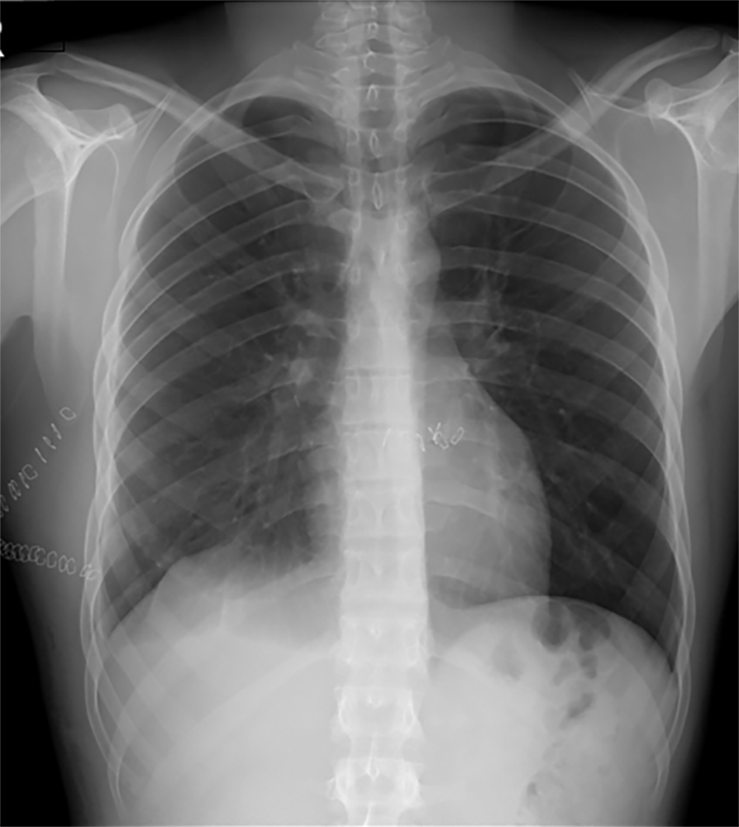
The patient was followed up in extubated status for 24 h in the level 2 intensive care unit, and was discharged on the fourth postoperative day without any complication (Figure 3). The patient was followed up for 12 mo and had no complaints (Figure 4).
Because penetrating thoracic trauma depends on the type of penetrating sharp object and the route within the thorax, it is necessary to be prepared for more severe results than the findings obtained from initial examination. The mechanisms underlying contralateral and contrecoup thoracic trauma are effective thorax anatomy in the transmission of trauma[5,6]. In our case, the trauma damaged the contralateral part of the chest wall, which is an ellipsoid formation consisting of ribs, sternum, and spine, through the influence of scapulothoracic joint kinematics. During shoulder girdle movements, the elevation, depression, protraction, retraction, and upward and downward rotation movements of the scapula change the direction of the sharp object, causing hemorrhage in the intercostal artery of the opposite hemithorax, which is the most frequently injured structure in penetrating thoracic trauma, as well as parenchymal damage in the right lower lobe posterior segment[6-9]. This case shows that auscultation of lung sounds and immediate thoracic imaging (e.g., chest X-ray, thoracic ultrasound, CT of the thorax) are important steps in determining the side of hemithorax injury. In this context, physical examination and auscultation have high sensitivity (90%) and specificity (98%)[1].
In thoracic trauma causing disruption in the pleural space, the first step is usually tube thoracostomy, although there is no randomized study regarding the size of the placed tube. However, according to Poiseuille’s law and the results of Fanning’s equation, an increase in pipe diameter leads to an exponential increase in the fluid and gas flowing through it. Therefore, the Advanced Trauma Life Support recommends that chest drains larger than 28 F be used to accurately assess the true volume of blood loss in cases of acute hemothorax[1]. In our case, the initial intervention was tube thoracostomy using a 32 F chest drain with the diagnosis of pneumohemothorax in the emergency department. After subsequent massive drainage, a 36 F chest drain was inserted during the emergency thoracotomy. In cases of rapidly deteriorating general condition, uncontrolled bleeding, development of cardiac arrest, severe hypotension due to pericardial tamponade, massive thoracic, or thoracoabdominal bleeding in the patient with penetrating thoracic trauma, surgery is recommended in 15%-30% of cases[10]. Stability of vital signs was achieved after tube thoracostomy in the patient with a right hemopneumothorax caused by penetrating trauma to the left hemithorax. However, emergency thoracotomy was performed due to acute massive hemorrhage, which likely occurred due to inactivation of coagulation factors in the hemorrhage focus during mobilization of the patient to the ward, creating hemodynamic instability with risk of mortality.
Hemothorax is a condition that requires rapid diagnosis and treatment. Treatment with tube thoracostomy is typically sufficient due to the buffering effect of the expanded lung, the presence of intense thromboplastin support in the lung parenchyma, and the low blood pressure in the pulmonary parenchyma[4]. However, the flow rate of the intercostal artery reportedly increases to a maximum of 169 mL/min, and can therefore result in 1 L of blood loss within minutes, if injured[11]. In our case, injury of the fifth intercostal artery led to 1600 cc blood loss within minutes. Clinical progression depends on the correct selection of patients’ vital signs and intervals for monitoring of drainage and hemogram, and rapid and accurate decisions about treatment with the synthesis of patient data.
Rapid diagnosis and correct intervention should be performed for patients with penetrating thoracic trauma, keeping in mind that both hemithoraces may have been injured.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gedik IE S-Editor: Gao CC L-Editor: A P-Editor: Li X
| 1. | Bertoglio P, Guerrera F, Viti A, Terzi AC, Ruffini E, Lyberis P, Filosso PL. Chest drain and thoracotomy for chest trauma. J Thorac Dis. 2019;11:S186-S191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Imamoglu OU, Oncel M, Enginel T, Tunçay E, Dalkılıc G, Acar H. Toraks travmalarında yaklaşım: 110 olgunun için. Türk J Thorac Cardiovasc Surg. 1999;7:450-453. |
| 3. | Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. J Trauma. 1988;28:298-304. [PubMed] [DOI] [Full Text] |
| 4. | Yıldız O, Kılıç D. Factors affecting morbidity and mortality in thoracic trauma. In: Özyurtkan MO, Bostancı K, Özpolat B. Thoracic trauma. Ankara: Ankara Nobel Medical Bookstores, 2018: 53-57. |
| 5. | Döner E, Sivrikoz C. Traumatic pneumothorax and hemothorax. In: Özyurtkan MO, Bostancı K, Özpolat B, editors. Thoracic Trauma. Ankara: Ankara Nobel Medical Bookstores, 2018: 145-151. |
| 6. | Güvenç EÇ, Ünal M, Gülmez B, Üçvet A, Gürsoy S. Penetrating contralateral hemothoraces. J Izmir Chest Hospital. 2018;3:203-205. |
| 7. | Rashid MA, Rashid MA. Cardiothoracic contralateral shoes: nomenclature, mechanism and importance. J Cardiothoracic Trauma. 2016;1:4-7. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Sharma OP, Blaney J, Oswanski MF, Assi Z, Disalle R, Latocki V. Stab wound of the neck with contralateral hemo-pneumothorax. J Emerg Med. 2010;39:e135-e138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Seth A, Matias R, Veloso AP, Delp SL. A Biomechanical Model of the Scapulothoracic Joint to Accurately Capture Scapular Kinematics during Shoulder Movements. PLoS One. 2016;11:e0141028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 10. | Temel U, Temel AGA. Surgical Procedures in Patients with Thoracic Trauma. In: Özyurtkan MO, Bostancı K, Özpolat B. Thoracic Trauma. Ankara: Ankara Nobel Medical Bookstores, 2018: 83-89. |
| 11. | Koyanagi T, Kawaharada N, Kurimoto Y, Ito T, Baba T, Nakamura M, Watanebe A, Higami T. Examination of intercostal arteries with transthoracic Doppler sonography. Echocardiography. 2010;27:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |