Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3752
Peer-review started: January 10, 2021
First decision: February 12, 2021
Revised: February 15, 2021
Accepted: March 8, 2021
Article in press: March 8, 2021
Published online: May 26, 2021
Processing time: 121 Days and 7.5 Hours
Pheochromocytoma is a rare endocrine tumor arising from chromaffin cells and having extensive and profound effects on the cardiovascular system by continuously or intermittently releasing catecholamines. The clinical manifestations of pheochromocytoma are diverse, and the typical triad, including episodic headache, palpitations, and sweating, only occurs in 24% of pheochromocytoma patients, which often misleads clinicians into making an incorrect diagnosis. We herein report the case of a patient with intermittent chest pain and elevated myocardial enzymes for 2 years who was diagnosed with pheochromocytoma.
A 49-year-old woman presented with intermittent chest pain for 2 years. Two years ago, the patient experienced chest pain and was diagnosed with acute myocardial infarction, with 25% stenosis in the left circumflex. The patient still had intermittent chest pain after discharge. Two hours before admission to our hospital, the patient experienced chest pain with nausea and vomiting, lasting for 20 min. Troponin I and urinary norepinephrine and catecholamine levels were elevated. An electrocardiogram indicated QT prolongation and ST-segment depression in leads II, III, aVF, and V3-V6. A coronary computed tomography angiogram revealed no evidence of coronary artery disease. Echocardiography showed left ventricular enlargement and a decreased posterior inferior wall motion amplitude. Contrast-enhanced computed tomography demonstrated an inhomogeneous right adrenal mass. The patient successfully underwent laparoscopic right adrenalectomy, and histopathology confirmed adrenal pheochromocytoma. During the first-year follow-up visits, the patient was asymptomatic. The abnormal changes on echocardiography and electrocardiogram disappeared.
Clinicians should be aware of pheochromocytoma. A timely and accurate diagnosis of pheochromocytoma is essential for alleviating serious cardiac complications.
Core Tip: Pheochromocytoma releases excessive amounts of catecholamines, which can have mild to catastrophic effects on the cardiovascular system, such as hypertension, myocardial infarction, cardiomyopathy, arrhythmias, and heart failure. However, most of the cardiovascular complications are reversible after pheochromocytoma resection. Clinicians should be aware of pheochromocytoma. A timely and accurate diagnosis of pheochromocytoma is essential for alleviating serious cardiac complications.
- Citation: Wu HY, Cao YW, Gao TJ, Fu JL, Liang L. Pheochromocytoma in a 49-year-old woman presenting with acute myocardial infarction: A case report. World J Clin Cases 2021; 9(15): 3752-3757
- URL: https://www.wjgnet.com/2307-8960/full/v9/i15/3752.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i15.3752
Pheochromocytoma is a rare endocrine tumor arising from chromaffin cells of the adrenal medulla or extra-adrenal paraganglion and having extensive and profound effects on the cardiovascular system by continuously or intermittently releasing catecholamines, mainly epinephrine and norepinephrine[1,2]. Pheochromocytoma has two main types, high norepinephrine/epinephrine secretion and high epinephrine/ norepinephrine secretion. The norepinephrine type affects mainly the cardiovascular system, manifesting mainly as hypertension, while the epinephrine type affects mainly the metabolism, manifesting mainly as hyperglycemia. A timely and accurate diagnosis of pheochromocytoma is essential for alleviating serious cardiac complications caused by an overdose of catecholamines. We report the case of a patient with intermittent chest pain and elevated myocardial enzymes for 2 years who was diagnosed with pheochromocytoma, and the abnormal changes in electrocardiogram (ECG) and echocardiography caused by pheochromocytoma disappeared after tumor resection.
A 49-year-old woman presented with intermittent chest pain for 2 years.
Two years ago, the patient experienced chest pain lasting for 20 min. The patient was diagnosed with acute myocardial infarction with a significant increase in troponin in a local hospital, and coronary angiography showed 25% stenosis in the left circumflex. The patient was treated with aspirin, clopidogrel, and statins. However, she still had intermittent chest pain, lasting for 5-10 min each time, after discharge. Two hours before admission to our hospital, the patient experienced chest pain with nausea and vomiting lasting for 20 min.
A history of hypertension and diabetes was denied.
The patient had a free personal history and denied a family history of premature coronary artery disease.
Vital signs on arrival showed body temperature of 36.8 ℃, blood pressure of 140/80 mmHg, a regular pulse of 84 beats per minute, and a respiratory rate of 18 breaths per minute. Heart and lung examinations showed no abnormalities. Jugular vein engorgement or peripheral edema was not found.
The troponin I level was 1.14 ng/mL (normal range < 0.04). The urinary norepinephrine level was 296.2 nmol/24 h (normal range 80.3-164.0), and the urinary catecholamine level was 327.8 nmol/24 h (normal range 94.5-238.3). The fasting blood glucose level was 5.6 mmol/L (normal range 3.9-6.1). B-type natriuretic peptide, 24-h urinary epinephrine, hemoglobin, leukocytes, amylase, electrolytes, liver function, renal function, and D-dimer were not significantly abnormal.
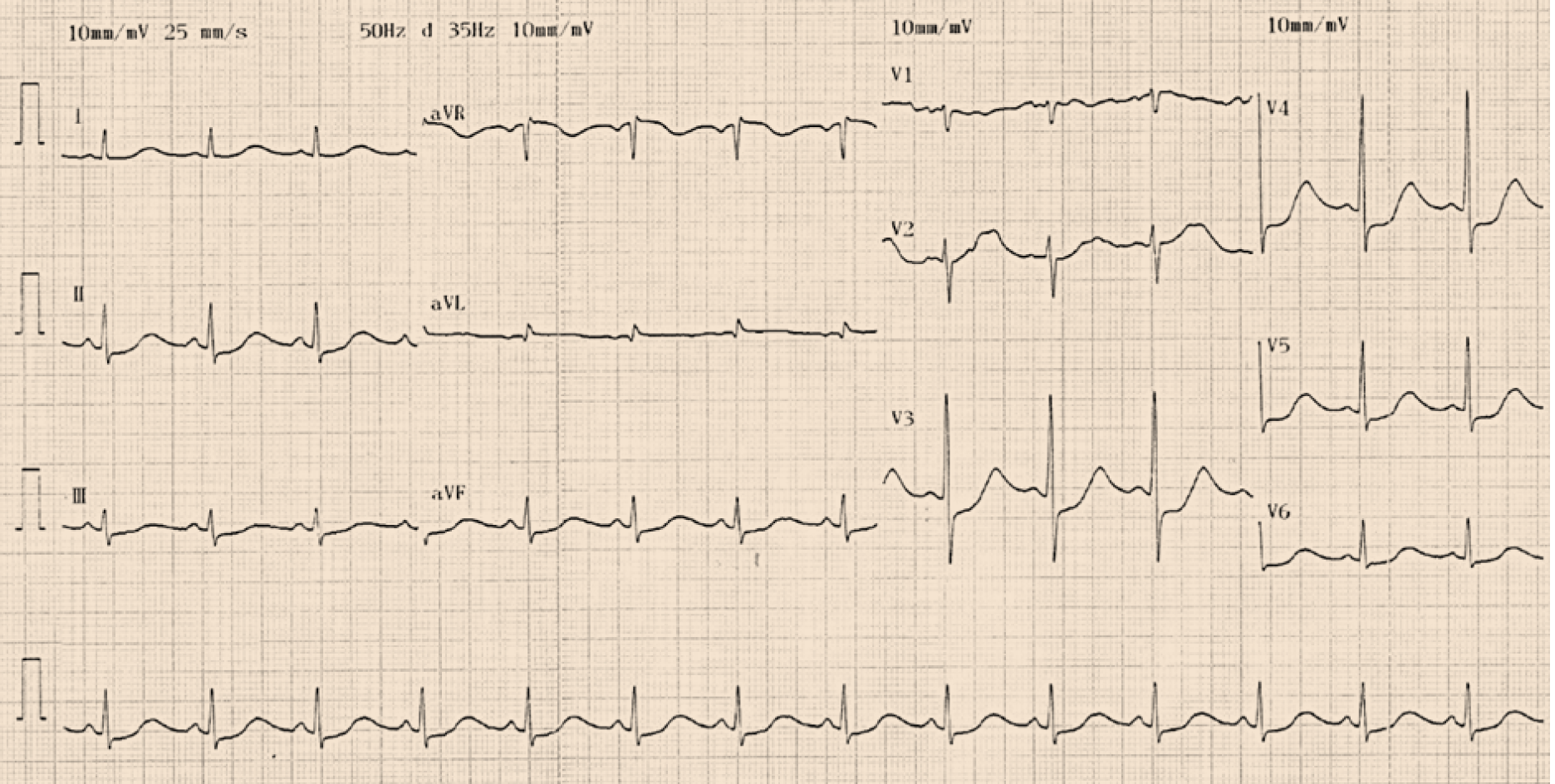
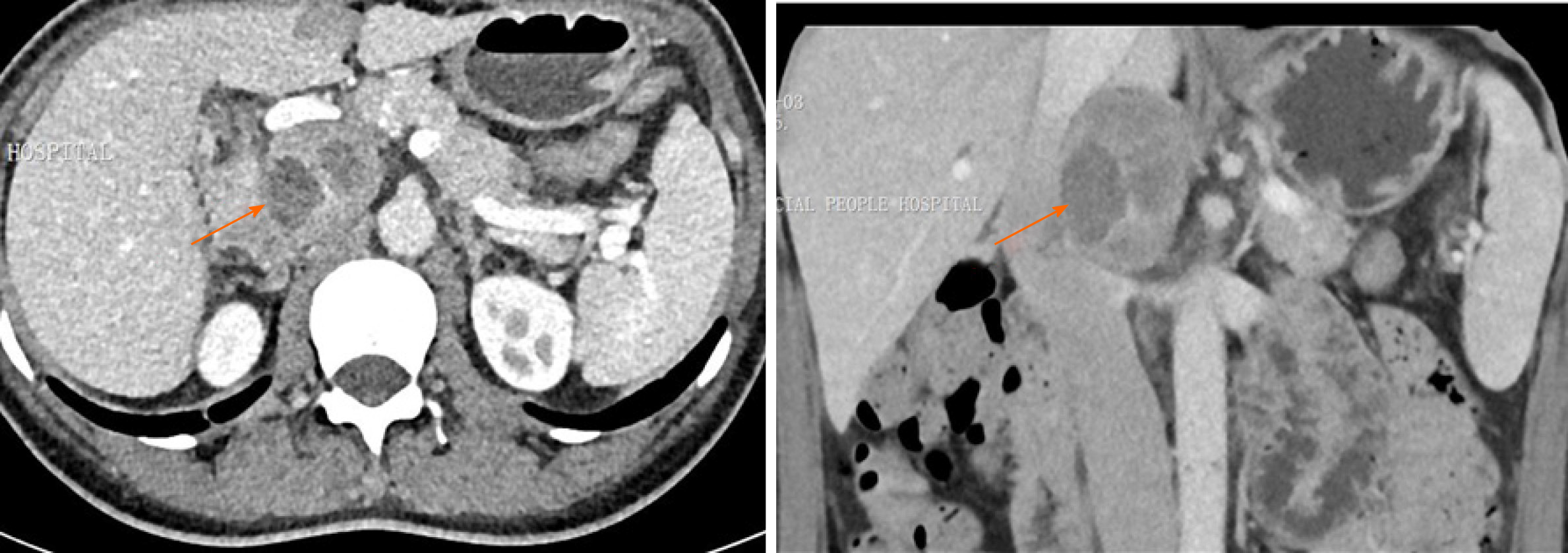
A 12-lead ECG indicated QT prolongation (QTc 533 ms) and ST-segment depression in leads II, III, aVF, and V3-V6 (Figure 1). A coronary computed tomography angiogram revealed no evidence of coronary artery disease (Figure 2). Echocardiography showed left ventricular enlargement (systolic and diastolic diameters of 45 mm and 57 mm, respectively) and a decreased posterior inferior wall motion amplitude (left ventricular ejection fraction of 51%). Chest computed tomography showed no obvious abnormality, but abdominal computed tomography showed an adrenal mass. Contrast-enhanced computed tomography demonstrated an inhomogeneous right adrenal mass (6.1 cm × 3.9 cm, Figure 3).
The patient was diagnosed with pheochromocytoma.
The patient was transferred to the urology department and underwent successful laparoscopic right adrenalectomy. Histopathology confirmed adrenal pheochromocytoma.
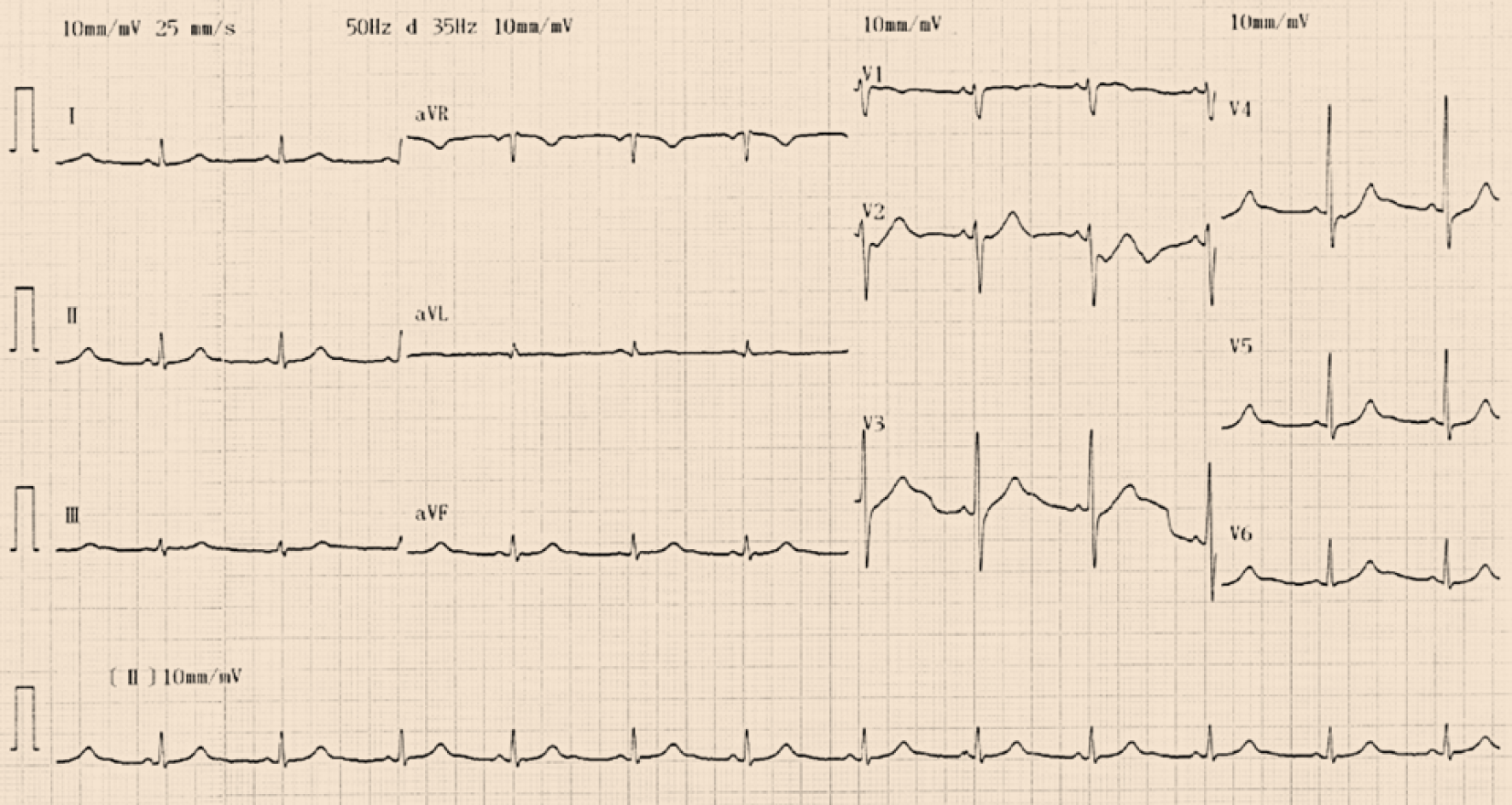
The patient was free of complications during hospitalization. During the first-year follow-up visits, the patient was asymptomatic and had normal blood pressure. Echocardiography showed a normal left ventricular size (systolic and diastolic diameters of 32 mm and 48 mm, respectively), no abnormal wall motion, and normal left ventricular function (left ventricular ejection fraction of 63%). ECG showed that QT prolongation and ST-segment depression in leads II, III, aVF, and V3-V6 disappeared (Figure 4). The patient showed no signs of recurrence and had normal urine norepinephrine and catecholamine levels.
Pheochromocytoma, which is derived from chromaffin cells, produces excessive amounts of catecholamines, especially epinephrine and norepinephrine, whose continuous or intermittent release can cause serious cardiovascular complications, such as hypertension, myocardial infarction, cardiomyopathy, arrhythmias, and heart failure[3,4]. It is estimated that the prevalence of pheochromocytoma during a lifetime is approximately 0.015%-0.04%, while its prevalence at autopsy is even higher (approximately 0.05%), which indicates that many pheochromocytomas are not diagnosed during the lifetime and may be the cause of death[5]. According to the laboratory results, the patient in our case belongs to high norepinephrine secreting pheochromocytoma.
Hypertension is one of the most common cardiovascular manifestations of pheochromocytoma, which can manifest as persistent or paroxysmal hypertension, mainly depending on the pattern of catecholamine secretion[6]. Approximately 90% of patients with pheochromocytoma have persistent or paroxysmal hypertension. Persistent hypertension is more common in patients with pheochromocytomas that continuously release high levels of norepinephrine. Paroxysmal hypertension is more common in patients with pheochromocytomas that intermittently secrete large amounts of epinephrine[7]. It is worth noting that a small proportion of patients with pheochromocytoma have normal blood pressure[8].
Patients with pheochromocytoma can develop catecholamine cardiomyopathy (including hypertrophic cardiomyopathy, dilated cardiomyopathy, and Takotsubo-like cardiomyopathy), myocardial ischemia, or even myocardial infarction. An increase in catecholamine levels can lead to increased production of reactive oxygen species, increased oxygen consumption, increased cardiac afterload, vasoconstriction, cell hypertrophy, cardiac remodeling, and even myocarditis[1,9]. The patient may present with chest pain, chest tightness, and sweating. ECG may show ST segment elevation or depression and T-wave inversion. Myocardial enzymes can also be elevated.
Approximately 50%-70% of pheochromocytoma patients complain of palpitations. Patients with pheochromocytoma may have a variety of arrhythmias, including atrial flutter, atrial fibrillation, supraventricular tachycardia, torsade de pointe ventricular tachycardia, ventricular fibrillation, and asystolic arrest[10]. Catecholamines can also cause the QT interval to be prolonged, which may induce torsade de pointes ventricular tachycardia and be life-threatening[11,12]. The reasons for arrhythmias caused by pheochromocytoma are considered to be multifactorial. Excessive catecholamine stimulation of beta-adrenergic receptors is one of the main reasons[13-16].
Although pheochromocytoma can cause many cardiovascular complications, most of them are reversible after pheochromocytoma resection[17-20]. In our case, the patient did not have the typical triad of pheochromocytoma but presented with acute myocardial infarction that caused abnormal changes in ECG and cardiac structure and function. However, the abnormal changes in ECG and echocardiography caused by pheochromocytoma disappeared after tumor resection.
The clinical manifestations of pheochromocytoma vary, and many patients do not have the typical triad, which easily leads to missing the diagnosis of pheochro-mocytoma. Pheochromocytoma causes an excess of catecholamines, which has a variety of potentially damaging effects on the cardiovascular system. However, most of the cardiovascular complications are reversible after pheochromocytoma resection. Clinicians should be familiar with clinical manifestations of pheochro-mocytoma, which helps raise clinical suspicion and facilitate the early diagnosis and treatment of pheochromocytoma.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Roysommuti S S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Gu YW, Poste J, Kunal M, Schwarcz M, Weiss I. Cardiovascular Manifestations of Pheochromocytoma. Cardiol Rev. 2017;25:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Jia Z, Wang BJ, Li X, Zhang X. Pheochromocytoma with delayed tumor thrombus detection in renal vein: A case report. World J Clin Cases. 2020;8:2849-2854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Galetta F, Franzoni F, Bernini G, Poupak F, Carpi A, Cini G, Tocchini L, Antonelli A, Santoro G. Cardiovascular complications in patients with pheochromocytoma: a mini-review. Biomed Pharmacother. 2010;64:505-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Zelinka T, Petrák O, Turková H, Holaj R, Strauch B, Kršek M, Vránková AB, Musil Z, Dušková J, Kubinyi J, Michalský D, Novák K, Widimský J. High incidence of cardiovascular complications in pheochromocytoma. Horm Metab Res. 2012;44:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Eisenhofer G, Rivers G, Rosas AL, Quezado Z, Manger WM, Pacak K. Adverse drug reactions in patients with phaeochromocytoma: incidence, prevention and management. Drug Saf. 2007;30:1031-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Shin JY, Kim BH, Kim YK, Kim TH, Kim EH, Lee MJ, Kim JH, Jeon YK, Kim SS, Kim IJ. Pheochromocytoma as a rare cause of hypertension in a 46 X, i(X)(q10) turner syndrome: a case report and literature review. BMC Endocr Disord. 2018;18:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Farrugia FA, Charalampopoulos A. Pheochromocytoma. Endocr Regul. 2019;53:191-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Pappachan JM, Tun NN, Arunagirinathan G, Sodi R, Hanna FWF. Pheochromocytomas and Hypertension. Curr Hypertens Rep. 2018;20:3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Hernández-Montoliu L, Simó-Servat A, Villabona C. Tako-Tsubo cardiomyopathy induced by pheochromocytoma. Endocrinol Diabetes Nutr. 2018;65:549-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Agrawal S, Shirani J, Garg L, Singh A, Longo S, Longo A, Fegley M, Stone L, Razavi M, Radoianu N, Nanda S. Pheochromocytoma and stress cardiomyopathy: Insight into pathogenesis. World J Cardiol. 2017;9:255-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Y-Hassan S, Falhammar H. Cardiovascular Manifestations and Complications of Pheochromocytomas and Paragangliomas. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 12. | Oruganti SS, Gambeer Rao M, Pisapati VL. Adrenal and extra-adrenal pheochromocytomas presenting as life-threatening ventricular arrhythmias: Report of three cases. Indian Heart J. 2016;68:381-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Zhang MM, Mao W, Wu D, Liu P. Pheochromocytoma with Ventricular Tachycardia as the Presenting Symptom. Chin Med J (Engl). 2016;129:1505-1506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth. 2017;31:1427-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 15. | Bai S, Yao Z, Zhu X, Li Z, Jiang Y, Wang R, Wen N. Risk factors for postoperative cardiovascular morbidity after pheochromocytoma surgery: a large single center retrospective analysis. Endocr J. 2019;66:165-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Lenders JWM, Eisenhofer G. Update on Modern Management of Pheochromocytoma and Paraganglioma. Endocrinol Metab (Seoul). 2017;32:152-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 105] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 17. | Brunt LM, Moley JF, Doherty GM, Lairmore TC, DeBenedetti MK, Quasebarth MA. Outcomes analysis in patients undergoing laparoscopic adrenalectomy for hormonally active adrenal tumors. Surgery. 2001;130:629-34; discussion 634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 68] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Anai T, Oka K, Yokota Y, Nishimura Y, Hagiya H, Otsuka F. Massive pheochromocytoma. Clin Case Rep. 2020;8:2308-2309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Worrest TC, Gilbert EW, Sheppard BC. Pheochromocytoma: 20 years of improving surgical care. Am J Surg. 2019;217:967-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Afana M, Panchal RJ, Simon RM, Hejab A, Lahiri SW, Khandelwal AK, Hudson MP. Pheochromocytoma-Induced Takotsubo Cardiomyopathy. Tex Heart Inst J. 2019;46:124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |