Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3733
Peer-review started: January 6, 2021
First decision: January 24, 2021
Revised: January 30, 2021
Accepted: March 3, 2021
Article in press: March 3, 2021
Published online: May 26, 2021
Processing time: 125 Days and 4.6 Hours
Ankle syndesmosis injury is difficult to diagnose accurately at the initial visit. Missed diagnosis or improper treatment can lead to chronic complications. Complete syndesmosis injury with a concomitant rupture of the interosseous membrane (IOM) is more unstable and severe. The relationship between this type of injury and Maisonneuve injury, in which the syndesmosis is also injured, has not been discussed in the literature previously.
A 16-year-old patient sustained left medial malleolar fracture, and the associated inferior tibiofibular syndesmotic instability was overlooked. After open reduction and internal fixation of the medial malleolar fracture, inferior tibiofibular syndesmosis diastasis with IOM rupture was detected by auxiliary imaging. Secondary surgical intervention was performed to reduce anatomically and fix with two trans-syndesmosis screws. Twelve weeks later, the screws were removed. At the 6-mo follow-up, the patient gained full range of motion of the ankle.
Complete syndesmosis injury with IOM rupture should be considered Maisonneuve-type injury. Open reduction and internal fixation could obtain good outcomes.
Core Tip: We present a case of medial malleolar fracture, and the associated complete syndesmosis injury with interosseous membrane rupture was overlooked, which teaches us to pay more attention to thorough physical examination and exact reading of auxiliary imaging and intraoperative stress fluoroscopy to avoid misdiagnosis. Furthermore, this is the first report describing this pattern of injury as a Maisonneuve-equivalent injury and further classifying Maisonneuve injury into three types.
- Citation: Liu GP, Li JG, Gong X, Li JM. Maisonneuve injury with no fibula fracture: A case report. World J Clin Cases 2021; 9(15): 3733-3740
- URL: https://www.wjgnet.com/2307-8960/full/v9/i15/3733.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i15.3733
Maisonneuve injury was first named after the French surgeon Maisonneuve[1] in 1840. The typical pattern of this injury is characterized by a fracture of the proximal fibula, a lesion of the inferior tibiofibular syndesmotic complex, and other possible injuries (rupture of the deltoid ligament, fracture of the medial malleolus, and avulsion fracture of the syndesmotic ligaments). Maisonneuve injury accounts for up to 7% of all ankle fractures, with approximately 5% of ankle fractures treated surgically[2,3].
Tibiofibular syndesmosis is essential for ankle stability. The incidence of syndesmosis injury accounts for 5% to 18% of ankle sprains[4]. Due to diagnostic difficulties, the injury is misidentified and, hence, poorly managed in 20% of cases[5]. Missed diagnosis or improper treatment can lead to chronic complications, especially in complete syndesmosis injury. We present a case of misdiagnosed complete syndesmosis injury involving interosseous membrane (IOM) rupture associated with medial malleolar fracture. This case report emphasizes the importance of thorough physical examination and exact reading of auxiliary imaging to detect latent syndesmosis instability. To our knowledge, this is the first time that this pattern injury was classified as a Maisonneuve-equivalent injury and further classification of Maisonneuve injury was made.
A healthy 16-year-old male student presented to the emergency department of our hospital due to left ankle trauma consequent to a car accident, complaining of severe pain and swelling on his left ankle.
The patient’s past medical history was unremarkable.
The patient’s personal and family history contained nothing of note. There was no family history of related inherent diseases.
Physical examination revealed a closed ankle injury with swelling, ecchymoses over the medial aspect, and tenderness around the ankle. There was no tenderness or crack at the proximal fibula. There was no neurological deficit. Dorsalis pedis and tibialis posterior artery pulses were palpable.
Laboratory evaluation, including complete blood count, blood biochemistry, and coagulation function, revealed no significant abnormalities.
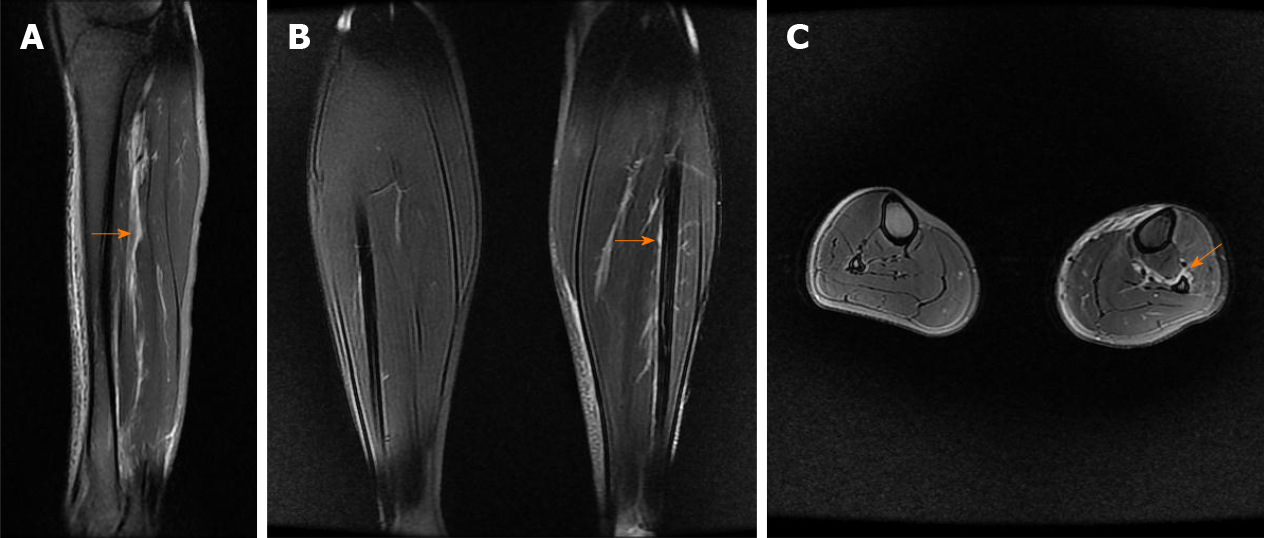
The left ankle radiographs of anteroposterior (AP) and lateral views, which were performed at another hospital, showed only medial malleolar fracture (Figure 1), which was also revealed in a computed tomography (CT) scan. Postoperatively, radiograph of AP view showed syndesmosis injury (Figure 2), and calf magnetic resonance imaging (MRI) revealed an IOM rupture, surrounded by areas of high signal intensity representing hemorrhage and edema (Figure 3).
The final diagnosis was complete syndesmosis injury with IOM rupture and medial malleolar fracture of the left ankle.
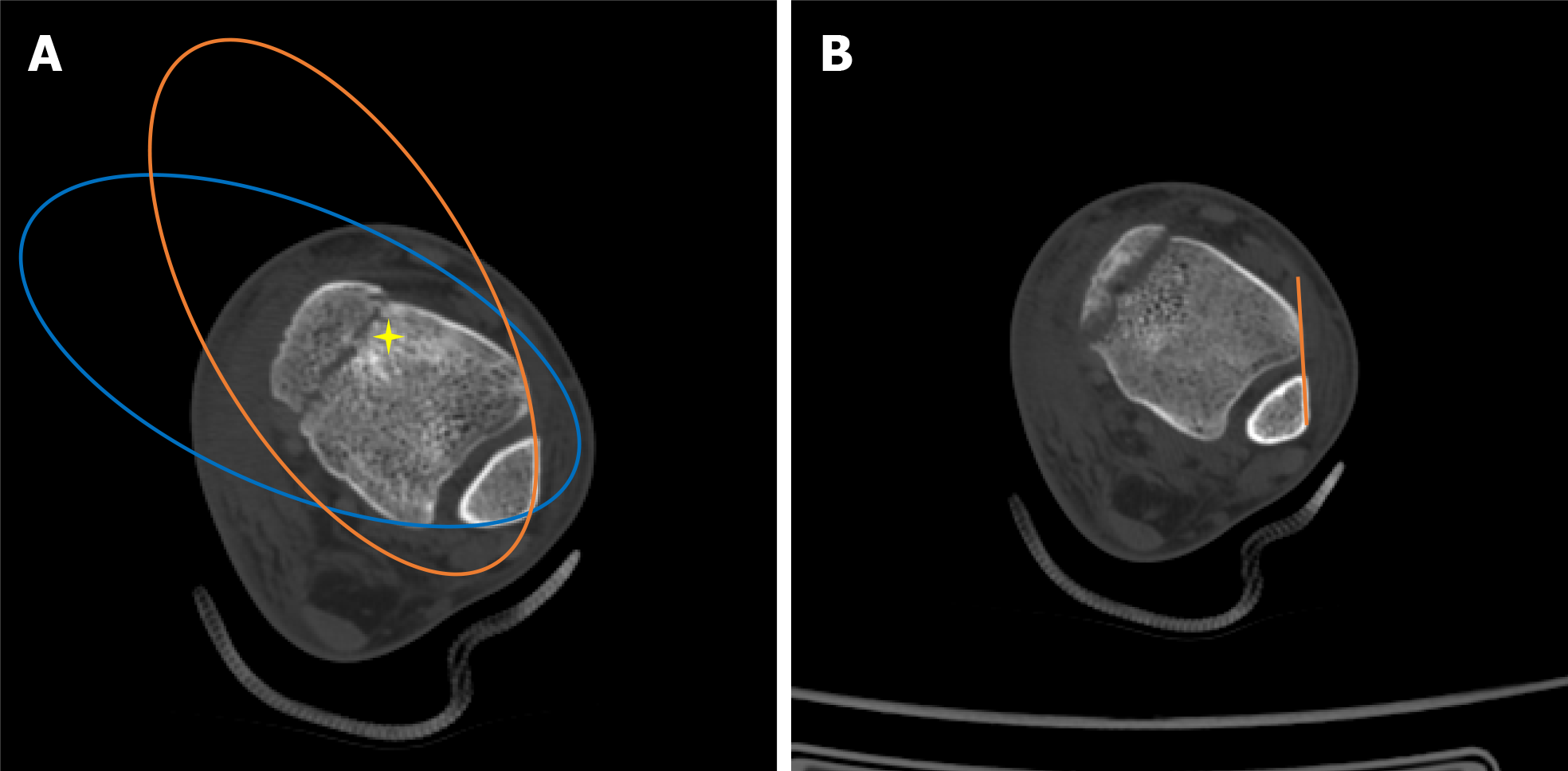
In the emergency department, radiographs of the proximal fibula were not performed because the patient reported no pain in the proximal fibula. In addition, physical examination also showed no tenderness or cracks at the proximal fibula. The injured limb was immobilized in a posterior short leg plaster, and then the patient was admitted to the orthopedic trauma ward and underwent CT scans to better identify the injury details. Except for a fractured medial malleolus, preoperative CT scans revealed no inferior tibiofibular diastasis according to Bartoníček et al[6]’s evaluation method (Figure 4A) and Gifford and Lutz[7] tibiofibular line (Figure 4B).
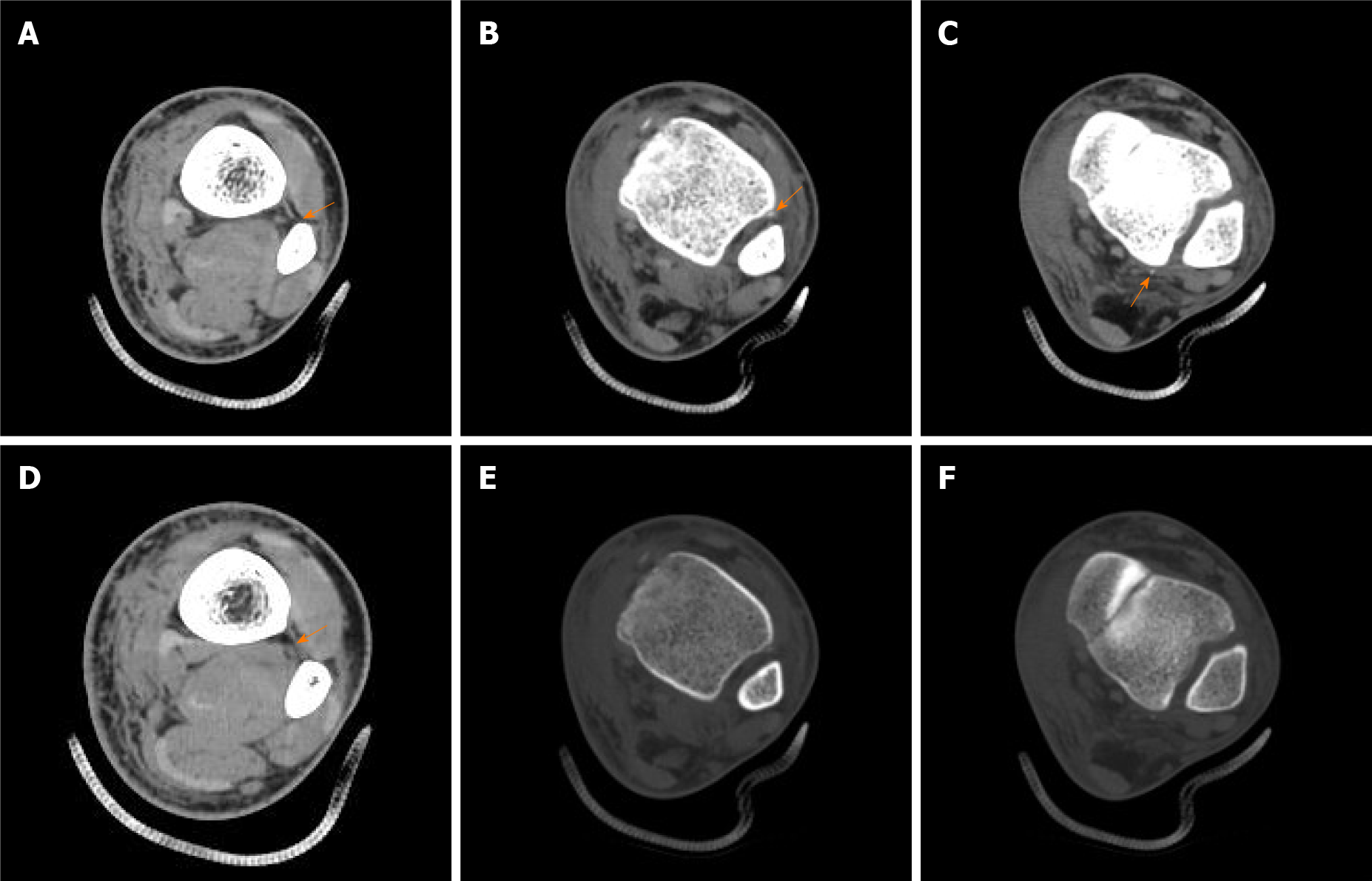
The patient underwent open reduction and internal fixation of the left medial malleolar fracture on the second day after injury. In the supine position, the surgical procedure was managed under epidural anesthesia and thigh tourniquet control. The fracture fragment was explored through an anteromedial approach. After hematoma drainage and interposed soft tissue removal, the fracture was reduced anatomically and fixed with two partially threaded cannulated screws. Intraoperative fluoroscopy indicated anatomic reduction of the medial malleolus with no widened tibiofibular clear space (TFCS) and medial clear space (MCS). However, the preoperative diagnosis was suspected and denied because postoperative radiograph of AP view showed enlarged TFCS and MCS (Figure 2). Immediately, radiographs of the proximal fibula were performed to rule out no fractures, but calf MRI revealed IOM rupture, surrounded by areas of high signal intensity representing hemorrhage and edema (Figure 3). As a windfall gain surprised us, a retrospective review of preoperative axial CT scans in the soft tissue window demonstrated that the IOM was torn from the fibular interosseous crest corresponding to the MRI findings (Figure 5A). The extent of IOM complete rupture was approximately 47.5 mm (1.25 mm/slice × 38 slices) above the talar dome. Furthermore, two minor bone fragments that could not be captured at all in the bone window were detected near the anterior tubercle and posterior tubercle of the distal tibia (a type of mini-Chaput fracture and mini-Volkmann fracture) (Figure 5B and C), which indicated avulsion fracture of the anterior inferior tibiofibular ligament (AITFL) and posterior inferior tibiofibular ligament (PITFL), respectively. In short, the inferior tibiofibular syndesmosis was completely injured and reduced spontaneously after the accident (Figure 5).
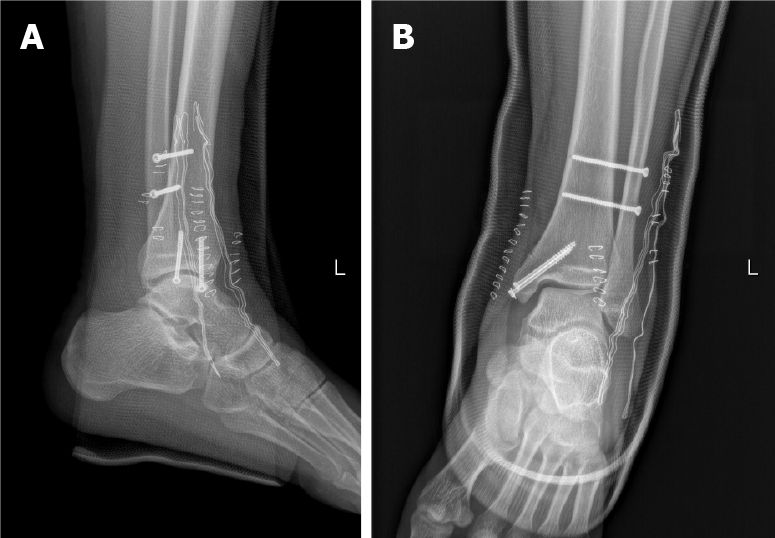
After consent was obtained from the patient and his family, secondary surgical intervention was conducted in the supine position and under epidural anesthesia on the second day post operation. An anterior incision was made to explore the inferior tibiofibular syndesmosis under direct visualization. Complete syndesmotic diastasis with the AITFL interposition was confirmed. The diastasis was reduced anatomically and maintained using two 3.5-mm fully threaded cortical screws oriented 30° from posterior to anterior with the ankle dorsiflexed (Figure 6). Rupture of the AITFL was treated by means of figure-eight suture reconstruction. Intraoperative stress fluoroscopy was performed to verify the syndesmotic stability with an external rotation test and valgus test. Postoperatively, the ankle was immobilized in a U-shaped plaster for 2 wk, and then active and passive mobilization of the ankle was started.
Before the syndesmotic screws were removed, the patient completed non-weight-bearing exercise for 10 wk, and then initiated weight bearing progressively. At the 6-mo postoperative visit, the patient gained full range of motion of the ankle and was restored to the preinjury activity level. The partially threaded cannulated screws were removed 12 mo postoperatively.
Syndesmosis injury may occur in isolation or be accompanied by other ankle injuries, accounting for 5% to 18% of ankle sprains[4]. It is difficult to diagnose accurately at the initial visit, with up to 20% overlooked in emergency[5]. Missed diagnosis or improper treatment can lead to chronic complications, such as instability, pain after activity, and osteoarthritis in the long term. Although auxiliary imaging assessment is essential to diagnosing this injury, clinical stress tests, including the valgus stress test, external rotation stress test, squeeze test, crossed-leg test, and Cotton test, also play an important role in the primary diagnosis. In the present case, we excessively assessed syndesmosis based on CT imaging and overfocused on matching the fibula and notch of the distal tibia in the bone window while ignoring syndesmotic soft tissue injury. If avulsion at the ventral and dorsal syndesmosis would have been caught in the soft tissue window before the primary surgery, the instability of the syndesmosis could potentially have raised suspicion. Stress tests could have been performed, and then secondary surgery would have been avoided. In addition, the well-known hook test is usually adopted to assess syndesmotic stability intraoperatively. If there is no lateral incision for the hook test, like the primary surgery in the present case, stress fluoroscopy of valgus or external rotation could also be performed to evaluate the syndesmotic stability.
Nonoperative treatment for patients with isolated syndesmosis injury has shown good results, even in high-level athletes[8]. Similarly, successful outcomes were obtained by surgical treatment with screws[9] or suture buttons[10]. Moreover, a minimum 2-year follow-up recommend that surgeons not only open reduction of the syndesmosis under direct visualization but perform postoperative CT scans with comparison to the contralateral extremity to reduce the rate of malreduction[11]. Reviewing the literature, nonoperative treatment is recommended for stable syndesmosis injury[12], whereas unstable syndesmosis injury (frank or latent) should be managed operatively[13]. The present case involved syndesmosis injury with a concomitant rupture of IOM, which is a fibrous connective tissue with a thickness of approximately 1 mm connecting the tibia and fibula. IOM plays an important role in maintaining the appropriate correlation between the tibia and fibula. Due to the strain of IOM, the distance between the tibia and fibula is not widened under external force to avoid lateral translation of the fibula, but it cannot prevent rotation or anterior-posterior translation of the fibula. When the IOM is injured, it unburdens the fibula in load transference by more than 30%[14]. Based on that, we believed that the present injury was caused by high energy (car accident), and the dynamic stability of syndesmosis was more difficult to maintain although the fractured medial malleolus was reduced and fixed firmly. Therefore, we chose open reduction and internal fixation for the syndesmosis injury to prevent spontaneous diastasis and eventually obtained good clinical outcomes in the follow-up.
IOM rupture was also found in all Maisonneuve injuries that previous studies reported[15,16]. The AITFL is not only the first involved structure when the talus rotates externally but also the weakest ligament of the tibiofibular syndesmotic complex, whereas the PITFL was confirmed to be intact in some Maisonneuve injuries. Therefore, except for upper third fibula fracture, one of the essential features of Maisonneuve injury may be rupture of the IOM, which continues distally and thickens into the interosseous ligament (IOL). Manyi et al[17] reported that the extent of IOM rupture was lower than the level of fibula fracture in all 12 patients with Maisonneuve fracture, ranging from 32-112 mm to the talar dome. He et al[18]’s study showed that the rupture of the IOM was not only limited to the distal one-third of the calf, on average 6.6 cm above the articular surface of the distal tibia, but also near the fibular fracture, while the IOM was intact between the two rupture sites in some patients. The wider the extent of the IOM rupture, the more severe the syndesmosis injury[17]. In our opinion, although the present case did not involve fracture of the upper third of the fibula, syndesmosis injury with IOM rupture could also be classified as Maisonneuve-equivalent injury according to the range of IOM rupture, the instability of the syndesmosis, and the similar management.
The injury mechanism of most Maisonneuve injuries is pronation-external rotation (PER)[19], in which the fibular fracture line extends from the anterior edge in a posteroinferior direction. Some studies have reported that the supination-external rotation mechanism could also lead to such injury, which is different from the former, being an intact medial structure (no fracture of the medial malleolus or rupture of the deltoid ligament)[6,20], and the fibular fracture line extended from the anterior edge in a posterosuperior direction[21]. Most authors have classified Maisonneuve injury as PER III or IV according to the Lauge-Hansen[22] classification. In a typical Maisonneuve injury, the involved structures caused by the PER IV mechanism include the fracture of the medial malleolus (or the rupture of the deltoid ligament), rupture of the AITFL (or avulsion fracture of the insertion), rupture of the IOL, rupture of the IOM, fracture of the proximal fibula, and rupture of the PITFL (or avulsion fracture of the insertion). On this basis, we concluded that the present case belongs to the PER IV mechanism, which was also one of the reasons that we classified it as Maisonneuve-equivalent injury.
In Maisonneuve injury, the force caused by talus external rotation runs from the medial aspect of the ankle, passing through the tibiotalar joint to the inferior tibiofibular syndesmosis. Rupture of the AITFL first occurs, followed by rupture of the IOL and IOM when the force persists. If the force is strong enough and continues to transmit up to the upper fibula, it may result in a stress concentration at the upper fibula due to the limitation of the upper tibiofibular syndesmosis; subsequently, upper fibula fracture occurs[23]. The fracture site of the fibula acts as a breakthrough point to release the force. When the transmitted force exceeds the limitation of upper tibiofibular syndesmosis, the superior tibiofibular joint is dislocated as a breakthrough point of the force, which is considered to be another kind of Maisonneuve-equivalent injury. Only five cases of that kind of Maisonneuve-equivalent injury have been reported in the literature[24]. According to the intensity of the transmitted force and the location of the breakthrough point, we further classified Maisonneuve injury as syndesmosis injury with IOM rupture (type I), syndesmosis injury with upper fibula fracture (type II), and syndesmosis injury with superior tibiofibular joint dislocation (type III).
The present injury pattern is different from simple syndesmosis injury and could be considered a Maisonneuve-equivalent injury. Comprehensive measures, including thorough physical examination and exact reading of auxiliary imaging and intraoperative stress fluoroscopy, should be performed to avoid misdiagnosis. The associated disruption of the IOM indicates the severity of syndesmosis injury. Good results could be achieved by open reduction and internal fixation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Santiago F S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Maisonneuve MJG. Recherches sur la fracture du péroné. Arch Gen Med. 1840;7:165-187. |
| 2. | Stufkens SA, van den Bekerom MP, Doornberg JN, van Dijk CN, Kloen P. Evidence-based treatment of maisonneuve fractures. J Foot Ankle Surg. 2011;50:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 3. | Lock TR, Schaffer JJ, Manoli A 2nd. Maisonneuve fracture: case report of a missed diagnosis. Ann Emerg Med. 1987;16:805-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1328-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res. 2019;105:S275-S286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 6. | Bartoníček J, Rammelt S, Kašper Š, Malík J, Tuček M. Pathoanatomy of Maisonneuve fracture based on radiologic and CT examination. Arch Orthop Trauma Surg. 2019;139:497-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Gifford PB, Lutz M. The tibiofibular line: an anatomical feature to diagnose syndesmosis malposition. Foot Ankle Int. 2014;35:1181-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Fort NM, Aiyer AA, Kaplan JR, Smyth NA, Kadakia AR. Management of acute injuries of the tibiofibular syndesmosis. Eur J Orthop Surg Traumatol. 2017;27:449-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | van den Bekerom MP, de Leeuw PA, van Dijk CN. Delayed operative treatment of syndesmotic instability. Current concepts review. Injury. 2009;40:1137-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Förschner PF, Beitzel K, Imhoff AB, Buchmann S, Feuerriegel G, Hofmann F, Karampinos DC, Jungmann P, Pogorzelski J. Five-Year Outcomes After Treatment for Acute Instability of the Tibiofibular Syndesmosis Using a Suture-Button Fixation System. Orthop J Sports Med. 2017;5:2325967117702854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 337] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 12. | Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc Rev. 2006;14:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, Ciuffreda M, Denaro V. Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24:1217-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Vukicević S, Stern-Padovan R, Vukicević D, Keros P. Holographic investigations of the human tibiofibular interosseous membrane. Clin Orthop Relat Res. 1980;210-214. [PubMed] |
| 15. | Babis GC, Papagelopoulos PJ, Tsarouchas J, Zoubos AB, Korres DS, Nikiforidis P. Operative treatment for Maisonneuve fracture of the proximal fibula. Orthopedics. 2000;23:687-690. [PubMed] |
| 16. | Yoshimura I, Naito M, Kanazawa K, Takeyama A, Ida T. Arthroscopic findings in Maisonneuve fractures. J Orthop Sci. 2008;13:3-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Manyi W, Guowei R, Shengsong Y, Chunyan J. A sample of Chinese literature MRI diagnosis of interosseous membrane injury in Maisonneuve fractures of the fibula. Injury. 2000;31 Suppl 3:C107-C110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | He JQ, Ma XL, Xin JY, Cao HB, Li N, Sun ZH, Wang GX, Fu X, Zhao B, Hu FK. Pathoanatomy and Injury Mechanism of Typical Maisonneuve Fracture. Orthop Surg. 2020;12:1644-1651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Charopoulos I, Kokoroghiannis C, Karagiannis S, Lyritis GP, Papaioannou N. Maisonneuve fracture without deltoid ligament disruption: a rare pattern of injury. J Foot Ankle Surg 2010; 49: 86.e11-86. e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Pankovich AM. Maisonneuve fracture of the fibula. J Bone Joint Surg Am. 1976;58:337-342. [PubMed] |
| 22. | Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957-985. [PubMed] |
| 23. | Yu GS, Lin YB, Xiong GS, Xu HB, Liu YY. Diagnosis and treatment of ankle syndesmosis injuries with associated interosseous membrane injury: a current concept review. Int Orthop. 2019;43:2539-2547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Alencar Neto JB, Cavalcante MLC, Pinto Neto LH, Lucena IF, Garrido RJ, Rocha PHMD. Maisonneuve Variant Lesion with Proximal Tibiofibular Dislocation. Rev Bras Ortop (Sao Paulo). 2019;54:339-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |