Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3567
Peer-review started: December 10, 2020
First decision: January 17, 2021
Revised: January 31, 2021
Accepted: March 10, 2021
Article in press: March 10, 2021
Published online: May 26, 2021
Processing time: 140 Days and 0.9 Hours
Peripheral regional block combined with general anesthesia might be a preferable anesthetic regimen for elderly patients undergoing total hip arthroplasty.
To investigate whether ultrasound-guided, direct suprainguinal injection for fascia iliaca block accelerated recovery after general anesthesia and relieved postoperative pain after total hip arthroplasty.
Patients who underwent total hip arthroplasty under general anesthesia in 2015 or 2019 at The Second Affiliated Hospital of Xuzhou Medical University were retrospectively analyzed. The patients were grouped based on whether preoperative suprainguinal fascia iliaca block was performed or not. The time to tracheal extubation and time spent in the post-anesthesia care unit (PACU), intraoperative remifentanil dosage, fentanyl consumption in the PACU, postoperative cumulative fentanyl consumption within 48 h after operation, visual analogue scale at rest and during movement on the first and second days after surgery, and adverse reactions were compared.
Thirty-one elderly patients who underwent total hip arthroplasty were included in the study (block group, n = 16; no-block group, n = 15). The visual analog scale scores at rest and during movement on the first and second days were significantly lower in the block group than in the no-block group (all P < 0.05). Compared with the no-block group, the intraoperative remifentanil dosage was lower, the time to tracheal extubation and the time spent in the PACU were shorter in the block group (all P < 0.01). Fentanyl consumption in the PACU and postoperative cumulative fentanyl consumption in 48 h after operation were lower in the block group (all P < 0.01). The incidence of dizziness was higher in the no-block group than in the block group (P = 0.037).
Ultrasound-guided, direct suprainguinal injection for fascia iliaca block led to faster recovery after general anesthesia and early postoperative pain relief in elderly patients undergoing total hip arthroplasty.
Core Tip: Ultrasound-guided in-plane direct suprainguinal injection for fascia iliaca block is safe, leading to faster recovery after general anesthesia and early relief of postoperative pain in elderly patients undergoing unilateral total hip arthroplasty.
- Citation: Wang YL, Liu YQ, Ni H, Zhang XL, Ding L, Tong F, Chen HY, Zhang XH, Kong MJ. Ultrasound-guided, direct suprainguinal injection for fascia iliaca block for total hip arthroplasty: A retrospective study. World J Clin Cases 2021; 9(15): 3567-3575
- URL: https://www.wjgnet.com/2307-8960/full/v9/i15/3567.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i15.3567
Hip fracture is a fracture of the upper portion of the femur, typically resulting in groin and thigh pain, manifesting as a shortened affected limb if the fracture is displaced (with hip positioned in external rotation and abduction), and weight-bearing is impossible[1,2]. The incidence of hip fracture is high in adults > 65 years of age[1,3]. With the aging of the population in China, the incidence of hip fractures in elderly individuals is also increasing[4,5].
Surgical treatment, mainly total hip arthroplasty, is the preferred choice for treating hip fractures, and it effectively improves the quality of life of elderly patients, reduces complications such as pneumonia and bedsores, and lowers the mortality rate[1,3,6]. Nevertheless, the declining physiological functions of essential organs and systems or various complications in elderly patients pose significant risks and challenges to the anesthesiologists during anesthesia and surgery.
Neuraxial anesthesia (spinal and epidural anesthesia) has advantages in orthopedic surgery of the lower limbs, such as intraoperative and postoperative analgesia, reducing postoperative opioids consumption[7], blood hypercoagulability[8], and pulmonary complications after total hip arthroplasty in patients with chronic obstructive pulmonary disease[9]. Nevertheless, the application of neuraxial anesthesia has some limitations, especially for elderly patients. For example, the spinal puncture can be difficult or even fail in some elderly patients with spinal degeneration[10]; besides, the patients are often non-cooperative as intraspinal anesthesia causes pain, tension, and dementia[11]. Compared to neuraxial anesthesia, general anesthesia is often accompanied by more stable hemodynamics during hip fracture surgery[12]; thus, it is an alternative anesthetic regimen for patients with hemodynamic instability, contraindication to neuraxial anesthesia, or failure of intraspinal block puncture.
Peripheral regional block combined with general anesthesia might be a preferable anesthetic regimen for elderly patients undergoing total hip arthroplasty. This regimen reduces the incidence of postoperative delirium and early postoperative cognitive dysfunction[13]. Bullock et al[14] described superior inguinal ligament fascia iliaca compartment block for the first time. This new method might block the lateral femoral cutaneous nerve more effectively than the traditional inferior inguinal ligament fascia iliaca compartment block, providing analgesia for incision during total hip arthroplasty.
The present study aimed to determine whether preoperative suprainguinal fascia iliaca block could accelerate recovery after general anesthesia and relieve postoperative pain in elderly patients undergoing total hip arthroplasty. The results could provide clinical support for the application of preoperative suprainguinal fascia iliaca block in these patients.
This retrospective study was approved by the Ethics Committee of the Second Affiliated Hospital of Xuzhou Medical University. The requirement for individual consent was waived by the committee.
The inclusion criteria were (1) underwent total hip arthroplasty in 2015 or 2019, (2) received general anesthesia before surgery, (3) 65-90 years of age, and (4) American Society of Anesthesiologists (ASA) grades I-III. The exclusion criteria were (1) severe chronic diseases of the heart, lung, or brain, (2) history of chronic pain and chronic use of opioids, (3) history of drug allergies, (4) intellectual or understanding disorders and unable to communicate normally, or (5) failure to complete the operation and was discharged from the hospital.
All included patients were divided into two groups based on whether preoperative suprainguinal fascia iliaca block was performed. No-block group: no suprainguinal fascia iliaca block was performed before the operation in 2015. Block group: suprainguinal fascia iliaca block was performed before the operation in 2019.
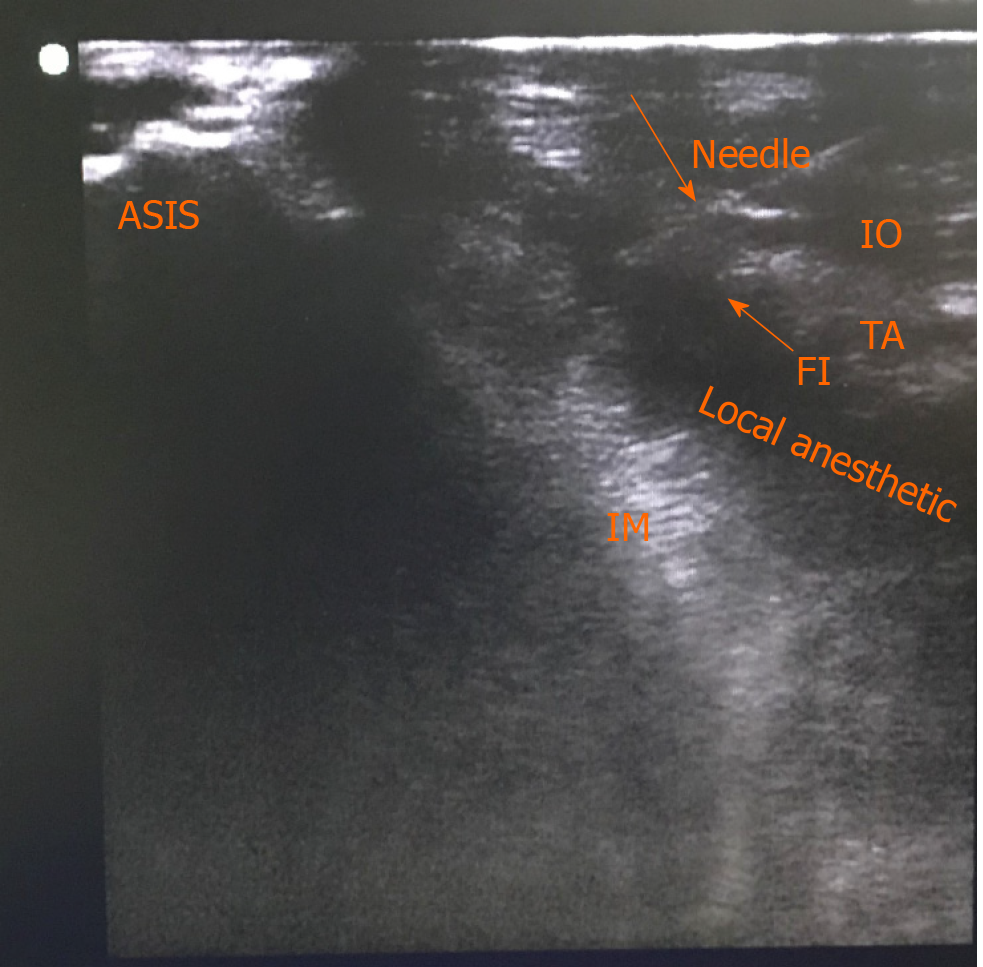
Electrocardiography, pulse oxygen saturation (SPO2), invasive radial arterial pressure, end-tidal CO2, and bispectral index (BIS) were monitored continuously during the operation. BIS was maintained between 40 and 60. The patients in the block group received suprainguinal fascia iliaca block 15 min before general anesthesia by the same anesthesiologist who was specifically trained in ultrasound-guided nerve block to ensure homogeneity of the procedures. Suprainguinal fascia iliaca block was performed according to the method described by Bullock et al[14] but was conducted under ultrasound guidance (Video). The patient was placed in the supine position, and the position of the anterior superior iliac spine was marked. Routine gloving, disinfection, and draping were conducted. A high-frequency linear array probe (6-13 MHz, Sonosite) (with sterile ultrasound gel) was transversely placed over the anterior superior iliac spine (Figure 1). The hypoechoic image of the anterior superior iliac spine was shown on the screen. The ultrasound probe was rotated towards the umbilicus until it clearly showed the anterior superior iliac spine, iliacus, fascia iliaca, medial internal oblique, transversus abdominis, and psoas major muscle. The suprainguinal fascia iliaca gap lies between the fascia iliaca and iliacus. Under ultrasound, using the in-plane technique, a 10-cm puncture needle was inserted from the umbilicus to the anterior superior iliac spine. When the needle tip reached the space between the fascia iliaca and iliacus (Figure 2), 2 mL of normal saline was injected to expand the gap between the fascia iliaca and iliacus. Then, 20 mL of 0.375% ropivacaine was injected. The diffusion of the liquid up and down along the fascia iliaca and iliacus was monitored by ultrasound.
In the two groups, anesthesia was induced with fentanyl 50 μg, propofol 1-1.5 mg/kg, rocuronium 0.6 mg/kg intravenously, and 5 mL of topical 2% lidocaine sprayed over the supraglottic before tracheal intubation. General anesthesia was maintained with sevoflurane 1.0%-1.5% and remifentanil 0-0.3 μg/kg/min (according to the BIS and hemodynamics) and continued until skin closure. The patients were ventilated with 50/50 oxygen/air mixture through tracheal intubation to maintain an end-tidal CO2 between 35 mmHg and 45 mmHg. Before suturing the skin, ondansetron 8 mg, ketochromic acid 30 mg, and fentanyl 15 μg were administered intravenously. During the operation, the vital signs were maintained at 80%-120% of baseline for systolic blood pressure and 55-75 bpm for heart rate. If necessary, vasoactive drugs such as phenylephrine, esmolol, urapidil, etc., were used to maintain the desired ranges' values.
After the operation, the patients were sent to the post-anesthesia care unit (PACU), where they were monitored for at least 30 min. When the patients opened their eyes spontaneously, responded to verbal commands, and respiratory efforts were within the normal clinical range, the tracheal tube was removed. A bolus of 10 μg of fentanyl was intravenously given at 10-min intervals until the visual analog scale (VAS) was < 4. The level of sedation was recorded as the Ramsay score. If the patients experienced severe sedation or had a Ramsay sedation score of > 5 or respiratory depression, fentanyl administration was discontinued. When the patients were fully awake and had a stable VAS of ≤ 4, they could be transferred to the general ward. All patients were provided with a patient-controlled intravenous analgesia (PCIA) pump with a 10-μg fentanyl bolus and a 20-min lockout period with no background.
The patients' baseline data, such as age, sex, body mass index, ASA grades, and adverse events after surgery, were collected. In addition to the intraoperative remifentanil dosage, time to tracheal extubation, time spent in the PACU, fentanyl dosage given by intravenous titration in the PACU and given by PCIA within 48 h after surgery, VAS score (with 0 indicating no pain and 10, the worst imaginable pain) at rest and during movement on the first and second days after surgery, and any complications and adverse events within 48 h after surgery were recorded.
Statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, United States). The Kolmogorov-Smirnov test was used to determine the normal distribution of the continuous data. Normally distributed data are presented as means ± SD and were analyzed using the Student’s t-test. Continuous data with a skewed distribution are presented as medians (interquartile range) and were analyzed using the Mann-Whitney U-test. Categorical data are presented as numbers and percentages and were compared using the Chi-square test or Fischer’s exact test. Two-sided (except for the Chi-square test) P values < 0.05 were considered statistically significant.
In this study, 15 patients who underwent surgery in 2015 were included in the no-block group, and 16 patients who underwent surgery with preoperative suprainguinal fascia iliaca block in 2019 were included in the block group. Suprainguinal fascia iliaca block was performed successfully. All patients in the block group showed a decrease or disappearance of skin sensation to cold stimuli 15 min after nerve block in the lateral thigh region. There were no significant differences in age (P = 0.74), body mass index (P = 0.739), sex (P = 0.553), ASA (P = 0.398), and operation time (P = 0.747) between the two groups (Table 1).
| Characteristics | No-block group (n = 15) | Block group (n = 16) | P value |
| Age (yr) | 80.1 ± 4.2 | 79.6 ± 4.2 | 0.740 |
| Body mass index (kg/m2) | 22.4 ± 2.3 | 22.2 ± 2.2 | 0.739 |
| Male/female | 10/5 | 10/6 | 0.553 |
| ASA II/III | 11/4 | 10/6 | 0.398 |
| Duration of surgery (min) | 60.3 ± 6.9 | 59.5 ± 8.3 | 0.747 |
The intraoperative remifentanil dosage (103.0 ± 37.9 µg vs 316.0 ± 62.5 µg, P < 0.01), fentanyl consumption given by intravenous titration in the PACU (1.9 ± 4.0 µg vs 22 ± 8.6 µg, P < 0.01), and postoperative cumulative fentanyl consumption by PCIA in 48 h after operation (204.3 ± 43.0 µg vs 406.6 ± 70.9 µg, P < 0.01) were significantly lower in the block group than in the no-block group (Table 2). The VAS at rest and during movement on the first and second days were significantly lower in the block group than in the no-block group (all P < 0.05) (Table 3).
| Analgesics | No-block group (n = 15) | Block group (n = 16) | P value |
| Intraoperative remifentanil dose (μg) | 316.0 ± 62.5 | 103 ± 37.9 | < 0.01 |
| Fentanyl given by intravenous titration in the PACU (μg) | 22 ± 8.6 | 1.9 ± 4.0 | < 0.01 |
| Fentanyl consumption by PCIA device in 48 h after operation (μg) | 406.6 ± 70.9 | 204.3 ± 43.0 | < 0.01 |
| Postoperative time (d) | VAS during rest | VAS during movement | ||||
| No-block group (n = 15) | Block group (n = 16) | P value | No-block group (n = 15) | Block group (n = 16) | P value | |
| 1st | 3.6 ± 0.5 | 2.7 ± 0.4 | < 0.01 | 4.9 ± 0.7 | 3.4 ± 0.5 | 0.011 |
| 2nd | 3.4 ± 0.6 | 3.0 ± 0.6 | < 0.01 | 4.2 ± 0.8 | 3.4 ± 0.5 | 0.002 |
The time to tracheal extubation (17.1 ± 2.2 min vs 28.0 ± 2.8 min, P < 0.01) and the time spent in the PACU (39.7 ± 9.0 min vs 68 ± 9.4 min, P < 0.01) in the block group were significantly shorter than in the no-block group (Table 4).
| Complications and adverse events | No-block group (n = 15) | Block group (n = 16) | P value |
| Dizziness, n (%) | 6 (40) | 1 (6.25) | 0.037 |
| Postoperative nausea and vomiting, n (%) | 3 (20) | 1 (6.25) | 0.333 |
| Respiratory depression, n (%) | 0 | 0 | / |
| Severe sedation, n (%) | 0 | 0 | / |
There were no significant differences in preoperative systolic blood pressure and heart rate between the two groups during surgery (all P > 0.05). However, more patients in the block group needed intraoperative intravenous phenylephrine to avoid hypotension during the operation compared with the no-block group (80.0% vs 25.0%, P < 0.01). Respiratory depression and severe sedation were not observed in either of the groups. No infections of the puncture point and local hematoma were observed in the block group. The incidence of postoperative nausea and vomiting was similar in the two groups (P = 0.333). The incidence of dizziness was higher in the no-block group than in the block group (P = 0.037) (Table 1).
This study examined whether suprainguinal fascia iliaca block could accelerate recovery after general anesthesia and relieve early postoperative pain in elderly patients undergoing total hip arthroplasty. The results suggest that ultrasound-guided in-plane suprainguinal fascia iliaca block led to faster recovery after general anesthesia and early postoperative pain relief in elderly patients undergoing unilateral total hip arthroplasty.
The innervation of the hip joint is complex, and the sensation of skin incision during total hip arthroplasty is mainly innervated by the lateral femoral cutaneous nerve. A complete lateral femoral cutaneous nerve block provides adequate postoperative incision analgesia for hip surgery[15]. The fascia iliaca compartment is a potential space for anesthesia and was initially proposed by Dalens et al[16] in 1989. It is simple to operate and does not directly involve an injection into the nerve, lowering neurovascular injury risk. It is currently the most widely used peripheral nerve block regimen for postoperative analgesia of the lower limbs. Previous studies confirmed that single or continuous block provides adequate postoperative analgesia for lower limb surgery, such as for the knee joints[14,17-23].
Nevertheless, the failure rate of lateral femoral cutaneous nerve block in the fascia iliaca compartment remains as high as 13%-37%[16,17,19], and the more significant variability of this lateral femoral cutaneous nerve below the inguinal ligament might be the cause of failure. Autopsy studies revealed that the lateral femoral cutaneous nerve either runs superficial, middle, or deep inside the inguinal ligament or runs on the lateral side of the inguinal ligament within 0-9 cm[22,24,25]. In contrast, the lateral femoral cutaneous nerve has a relatively stable route distribution in the pelvic region above the inguinal ligament and passes between the iliacus and fascia iliaca[26]. Hebbard et al[20] revealed dye distribution around the lateral femoral cutaneous nerve of the pelvic region after inserting a needle from the inferior inguinal ligament, passing through the inguinal ligament, and reaching the fascia iliaca above the inguinal ligament. Previous studies confirmed the feasibility and effectiveness of performing fascia iliaca compartment block[18,21,23].
In the present study, the patients who received suprainguinal fascia iliaca block had faster anesthesia recovery and significantly lower postoperative VAS than those without peripheral nerve block. These results suggest that general anesthesia combined with suprainguinal fascia iliaca block might be considered more suitable for elderly patients with poor baseline conditions. It can also accelerate the recovery from general anesthesia, relieve early postoperative pain, and reduce complications. In addition to effectiveness, the safety of suprainguinal fascia iliaca block was verified. During surgery, the higher needle insertion point of the fascia iliaca block between the anterior superior iliac spine and umbilicus remains far from the surgical incision and inguinal ligament, reducing the surgeons’ concerns about puncture-induced incision infection. In addition, suprainguinal fascia iliaca block reduced complications and adverse events in elderly patients undergoing unilateral total hip arthroplasty.
This study has limitations. One limitation is the small number of cases. In addition, due to the study's retrospective nature, the analgesic effect and time course could not be compared at different concentrations of local anesthetics. Finally, the patients were not included continuously because of technical and conditional restrictions. The technology of ultrasound-guided nerve block was not available in the hospital until 2019. Although the low iliac fascia blocks were used during 2015-2019, the effect was not stable. Therefore, the patients in the block group were operated on in 2019, while those in the no-block group were operated on in 2015, which could have led to an inevitable bias.
In conclusion, ultrasound-guided in-plane suprainguinal fascia iliaca block in elderly patients undergoing unilateral total hip arthroplasty might accelerate the recovery after general anesthesia and relieve early postoperative pain. This method could be reliable and could lead to better outcomes in elderly patients.
Peripheral regional block combined with general anesthesia might be a preferable anesthetic regimen for elderly patients undergoing total hip arthroplasty.
To identify an effective method of peripheral nerve block to relieve pain after hip replacement.
To investigate whether ultrasound-guided, direct suprainguinal injection for fascia iliaca block accelerated recovery after general anesthesia and relieve postoperative pain after total hip arthroplasty.
Patients who underwent total hip arthroplasty under general anesthesia in 2015 or 2019 at The Second Affiliated Hospital of Xuzhou Medical University were retrospectively analyzed. The patients were grouped based on whether preoperative suprainguinal fascia iliaca block was performed or not. The time to tracheal extubation and time spent in the post-anesthesia care unit (PACU), intraoperative remifentanil dosage, fentanyl consumption in the PACU, postoperative cumulative fentanyl consumption within 48 h after operation, visual analog scale at rest and during movement on the first and second days after surgery, and adverse reactions were compared.
The visual analog scale scores at rest and during movement on the first and second days were significantly lower in the block group than in the no-block group (all P < 0.05). Compared with the no-block group, the intraoperative remifentanil dosage was lower, and the time to tracheal extubation and the time spent in the PACU were shorter in the block group (all P < 0.01). Fentanyl consumption in the PACU and postoperative cumulative fentanyl consumption in 48 h after operation were lower in the block group (all P < 0.01). The incidence of dizziness was higher in the no-block group than in the block group (P = 0.037).
Ultrasound-guided, direct suprainguinal injection for fascia iliaca block led to faster recovery after general anesthesia and early postoperative pain relief in elderly patients undergoing total hip arthroplasty.
We will conduct a prospective study to further verify that ultrasound-guided, direct suprainguinal injection for fascia iliaca block is superior to traditional fascia iliac block for analgesia after hip replacement.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lin JA S-Editor: Gao CC L-Editor: Webster JR P-Editor: Wang LL
| 1. | Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma. 2015;29:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 254] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 2. | Sheehan SE, Shyu JY, Weaver MJ, Sodickson AD, Khurana B. Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know. Radiographics. 2015;35:1563-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | LeBlanc KE, Muncie HL Jr, LeBlanc LL. Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician. 2014;89:945-951. [PubMed] |
| 4. | Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, Wang O, Xing XP, Sun Y, Cummings SR. Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res. 2012;27:125-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 159] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 5. | Chen W, Lv H, Liu S, Liu B, Zhu Y, Chen X, Yang G, Liu L, Zhang T, Wang H, Yin B, Guo J, Zhang X, Li Y, Smith D, Hu P, Sun J, Zhang Y. National incidence of traumatic fractures in China: a retrospective survey of 512 187 individuals. Lancet Glob Health. 2017;5:e807-e817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 174] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 6. | SooHoo NF, Farng E, Chambers L, Znigmond DS, Lieberman JR. Comparison of complication rates between hemiarthroplasty and total hip arthroplasty for intracapsular hip fractures. Orthopedics. 2013;36:e384-e389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Harsten A, Kehlet H, Ljung P, Toksvig-Larsen S. Total intravenous general anaesthesia vs. spinal anaesthesia for total hip arthroplasty: a randomised, controlled trial. Acta Anaesthesiol Scand. 2015;59:298-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Song B, Qiao Y, Jiang H, Yan X. Effects of neuraxial and general anaesthesia for total joint arthroplasty:a meta-analysis. J Clini Anesthesiol. 2017;33:52-58. |
| 9. | Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional vs general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117:72-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 211] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 10. | Keorochana G, Taghavi CE, Tzeng ST, Morishita Y, Yoo JH, Lee KB, Liao JC, Wang JC. Magnetic resonance imaging grading of interspinous ligament degeneration of the lumbar spine and its relation to aging, spinal degeneration, and segmental motion. J Neurosurg Spine. 2010;13:494-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Apan A, Apan ÖC. Complications in Spinal Anaesthesia. London: IntechOpen, 2014. [DOI] [Full Text] |
| 12. | Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004;CD000521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 117] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 13. | Mei B, Zha H, Lu X, Cheng X, Chen S, Liu X, Li Y, Gu E. Peripheral Nerve Block as a Supplement to Light or Deep General Anesthesia in Elderly Patients Receiving Total Hip Arthroplasty: A Prospective Randomized Study. Clin J Pain. 2017;33:1053-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Bullock WM, Yalamuri SM, Gregory SH, Auyong DB, Grant SA. Ultrasound-Guided Suprainguinal Fascia Iliaca Technique Provides Benefit as an Analgesic Adjunct for Patients Undergoing Total Hip Arthroplasty. J Ultrasound Med. 2017;36:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Liu SS, Ngeow JE, Yadeau JT. Ultrasound-guided regional anesthesia and analgesia: a qualitative systematic review. Reg Anesth Pain Med. 2009;34:47-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69:705-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 143] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d'Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg. 1998;86:1039-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Desmet M, Vermeylen K, Van Herreweghe I, Carlier L, Soetens F, Lambrecht S, Croes K, Pottel H, Van de Velde M. A Longitudinal Supra-Inguinal Fascia Iliaca Compartment Block Reduces Morphine Consumption After Total Hip Arthroplasty. Reg Anesth Pain Med. 2017;42:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 131] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 19. | Foss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, Hougaard S, Kehlet H. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007;106:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 210] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 20. | Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66:300-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | Kumar K, Pandey RK, Bhalla AP, Kashyap L, Garg R, Darlong V, Malhotra R, Yadav CS. Comparison of conventional infrainguinal vs modified proximal suprainguinal approach of Fascia Iliaca Compartment Block for postoperative analgesia in Total Hip Arthroplasty. A prospective randomized study. Acta Anaesthesiol Belg. 2015;66:95-100. [PubMed] |
| 22. | Martins RS, Siqueira MG, Silva FC Jr, Heise CO, Teixeira MJ. A practical approach to the lateral cutaneous nerve of the thigh: an anatomical study. Clin Neurol Neurosurg. 2011;113:868-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Swenson JD, Davis JJ, Stream JO, Crim JR, Burks RT, Greis PE. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: the pattern of distribution and effects on the obturator nerve. J Clin Anesth. 2015;27:652-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 24. | Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100:600-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 154] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 25. | Benezis I, Boutaud B, Leclerc J, Fabre T, Durandeau A. Lateral femoral cutaneous neuropathy and its surgical treatment: a report of 167 cases. Muscle Nerve. 2007;36:659-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Shteynberg A, Riina LH, Glickman LT, Meringolo JN, Simpson RL. Ultrasound guided lateral femoral cutaneous nerve (LFCN) block: safe and simple anesthesia for harvesting skin grafts. Burns. 2013;39:146-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |