Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3177
Peer-review started: December 17, 2020
First decision: January 24, 2021
Revised: February 2, 2021
Accepted: March 4, 2021
Article in press: March 4, 2021
Published online: May 6, 2021
Processing time: 125 Days and 23.7 Hours
Duplicate renal malformation is a congenital disease of the urinary system, with an incidence rate of 0.8%. Surgical treatment is suitable for symptomatic patients. Urinary fistula is one of the complications of heminephrectomy. Long-term urinary fistula has a great impact on patients' lives.
This article mainly reports on a 47-year-old man with duplication of kidney deformity, long urinary fistula after partial nephrectomy, and no improvement after conservative treatment. We have achieved positive results in the arterial embolization treatment of the residual renal artery, indicating that selective arterial embolization is a good way to treat urinary fistula after partial nephrectomy. It is worth noting that this patient violated the Weigert-Meyer law, which also gave us more consideration.
Renal artery embolization may be a simple and safe method to treat urinary fistula inefficacy with conservative treatment.
Core Tip: Urine leakage is one of the complications of heminephrectomy, and it leads to a serious decline in the patient’s quality of life. For patients who fail conservative treatment, they may also face the risk of reoperation. We successfully treated a patient with urine leakage after heminephrectomy through selective renal artery embolization. After 3 years of follow-up observation, the patient's renal function was normal and no urinary fistula recurred.
- Citation: Yang T, Wen J, Xu TT, Cui WJ, Xu J. Renal artery embolization in the treatment of urinary fistula after renal duplication: A case report and review of literature. World J Clin Cases 2021; 9(13): 3177-3184
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3177.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3177
Duplicate renal malformation is a rare congenital disease of the urinary system, with an incidence rate of 0.8%. There is no significant difference in the incidence of bilateral kidneys. The incidence of women is twice that of men. There is genetic susceptibility, with about 1/8 of patients’ parents or siblings having similar conditions. Asymptomatic patients did not need treatment. Surgical treatment is suitable for patients with hydronephrosis, repeated urinary tract infections, and (or) urinary incontinence[1].
A 47-year-old patient suffered a urinary fistula for up to 14 mo after nephrectomy.
Within 1 wk after heminephrectomy, the patient’s daily drainage tube drained about 30-50 mL of light red liquid. From the 10th day after surgery, the patient’s wound began to seep light yellow transparent fluid, up to 350 mL in large quantities. A computed tomography (CT) scan showed a large amount of fluid around the right kidney 2 mo after the surgery. After repeated local puncture and drainage, the wound still did not heal. The symptoms had lasted for 14 mo.
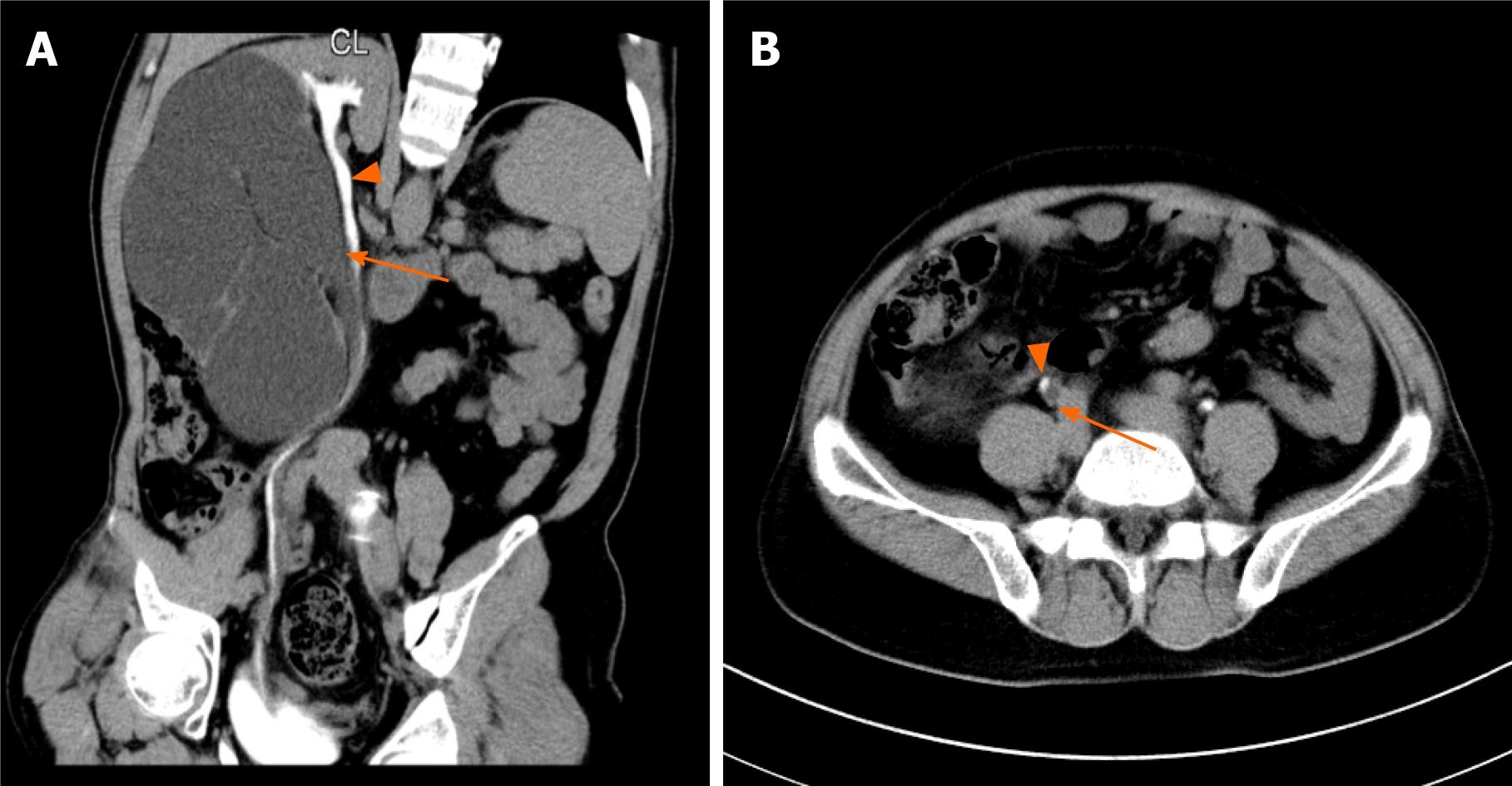
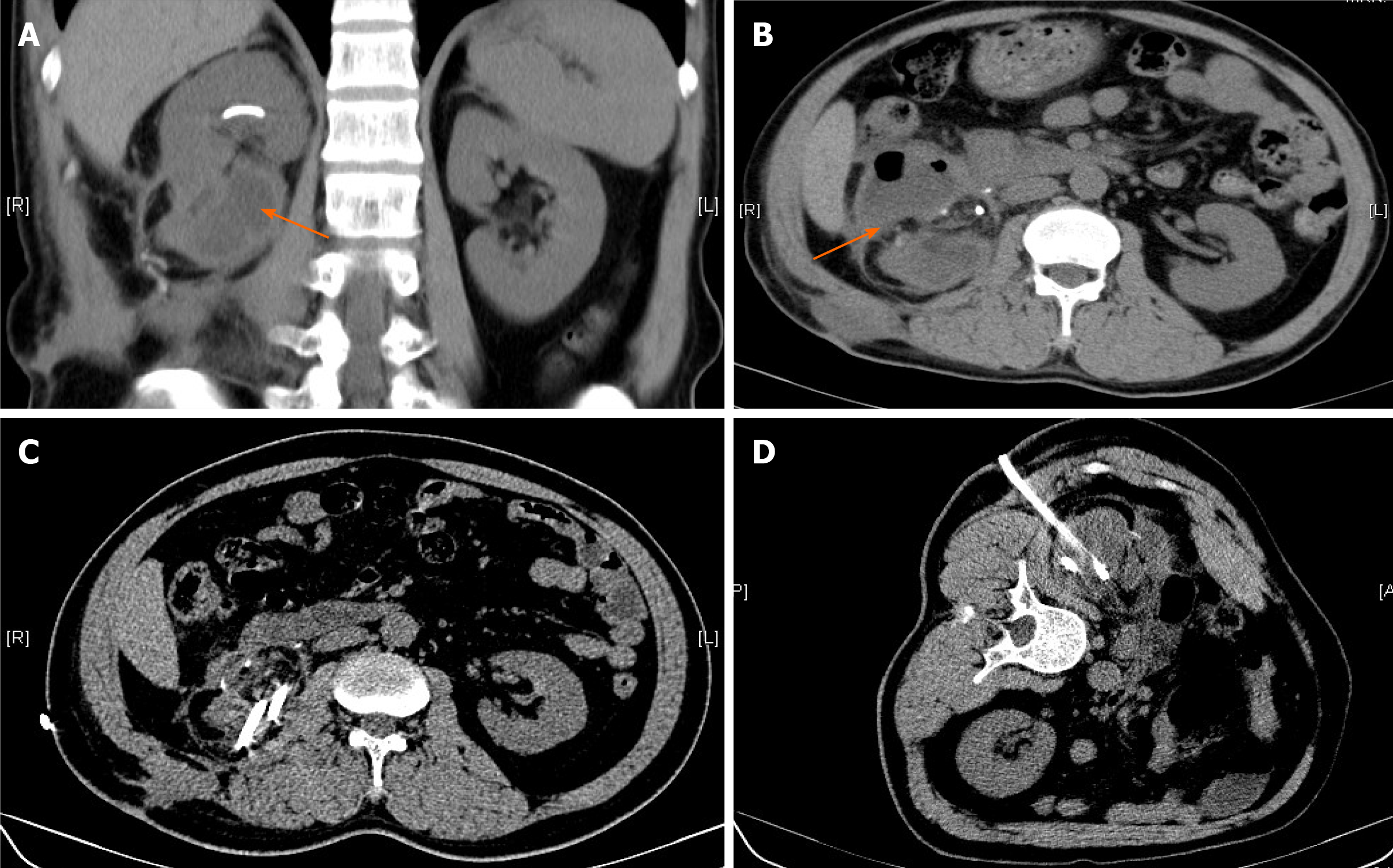
The 47-year-old patient suffered from symptoms of recurrent right sided flank pain and discomfort. At the local hospital for the first time, CT examination results confirmed duplicate kidney on the right side, severe hydrops, and ureteral stones in the right kidney. Next, lithotripsy was performed. After 4 mo, she went to a senior hospital again because of persistent symptoms. CT was performed again and showed that the upper 1/3 renal pelvis and ureter were normal and the lower 2/3 renal pelvis was severely hydrolyzed without ureter display (Figure 1). After doctor-patient consultation, the right ureteroscopy was performed, and a double J tube was released into the right side of the normal renal pelvis and ureter. One month later, she underwent "laparoscopic right side repeated nephrectomy" under general anesthesia (Figure 2). Visible in the surgery were hydrops in the right lower kidney and normal upper right kidney. The blood supply of the upper and lower parts of the right kidney was each supplied by the renal artery and vein, and the upper and lower parts had independent ureters. The ureter belonging to the lower right kidney was significantly dilated. An ultrasonic knife was used to free completely the junction of the hydronephrosis kidney and the normal kidney to remove the diseased kidney. The ureter was cut about 15 cm away from the renal pelvis. A perinephric drainage tube was placed that led out through the puncture hole above the iliac crest. Postoperative anti-infection and hemostasis treatment was performed. Postoperative pathology proved a duplicate kidney.
The patient’s temperature was 36.2 °C, heart rate was 76 bpm, respiratory rate was 18 breaths/min, and blood pressure was 127/74 mmHg.
Re-admitted to hospital on December 16, 2016, the drainage fluid biochemical examination showed creatinine 225 μmol/L, urea 9.0 mmol/L, and serum creatinine 68 μmol/L.
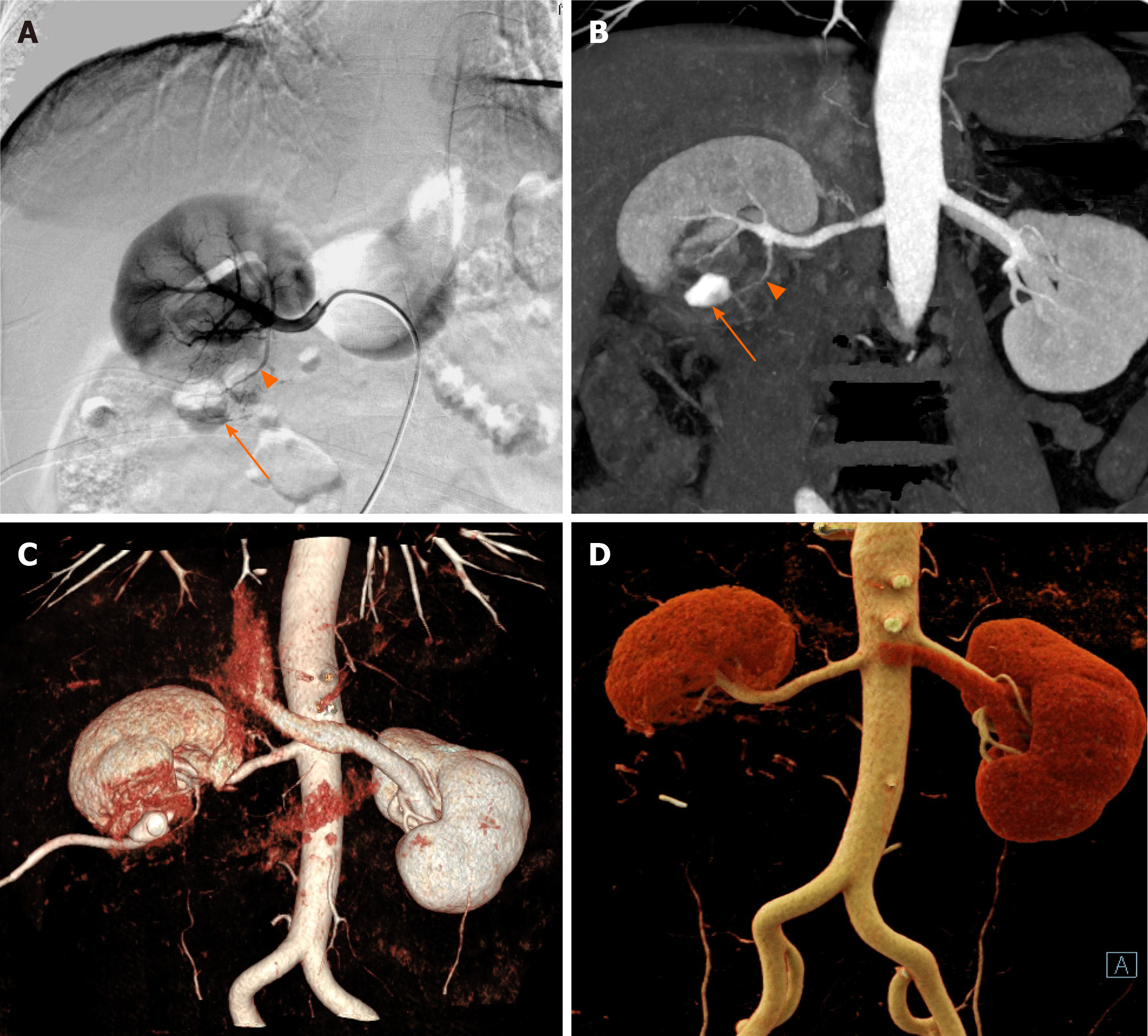
Renal CT angiography showed that a branch artery of the lower pole of the right kidney ran along the lower part of the right kidney (Figure 3).
Fistulography showed that the fistula was located in the lower part of the right kidney, which was a limited residual cavity without entering the abdominal cavity.
The final diagnosis of the presented case was urinary fistula.
The right renal digital subtraction angiography (DSA) and renal artery embolization were performed based on the patient’s informed consent. DSA showed that the right inferior renal artery branched to the residual kidney tissue of the right kidney (Figure 3). Polyvinyl alcohol (PVA) particles (100-300 μm) embolized the blood supply artery of the residual kidney by super-selective intubation. After embolization, DSA showed only the main trunk of the residual renal artery. One day after the operation, the drainage tube fluid was significantly reduced.
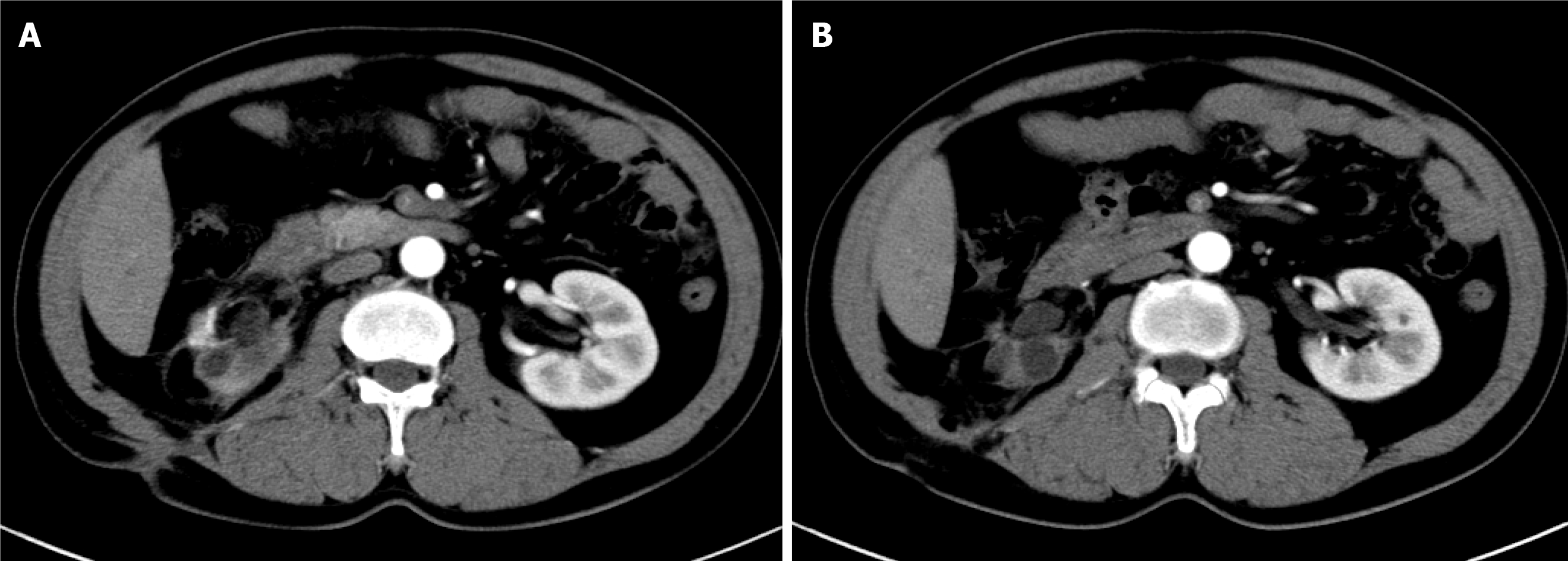
One month after the operation, the drainage tube was removed. The wound was completely healed 3 mo after the operation. On January 8, 2018, the abdominal CT angiography (CTA) showed that only the main trunk of the right renal residual artery remained (Figure 4). After 3 years of follow-up, the patient did not leak urine again and her renal function was normal. After 3 years of follow-up observation, the patient's renal function was normal, and no urinary fistula recurred.
This patient’s kidney has two sets of ureters. The lower kidney was accompanied by obvious ureteral dilation and hydronephrosis. CT urography suggested that the upper kidney had normal secretory function and urinary system. The lower kidney has no urinary function. This case does not conform to the Meyer-Weigert rule; the Meyer-Weigert rule predicts the double ureteral drainage pattern of bipolar renal repetition. The upper pole is generally considered to be ectopic, so it is hypoplastic resulting in obstruction[2]. Although the Meyer-Weigert rule applies to most duplication kidney cases, some case reports in recent years have pointed out exceptions to this rule[3-7]; this is true for our case.
According to the Meyer-Weigert rule, the clinical symptoms of duplication of kidney deformity are often related to the superior kidney. The suitable surgical treatment is heminephrectomy[8]. Since the right upper kidney of this patient had normal function, heminephrectomy was performed for the right lower kidney. Partial nephrectomy is widely used in the resection of early renal cancer due to its lower overall mortality and cardiovascular morbidity compared to radical resection[9-11]. However, the complication rate of urinary fistula after heminephrectomy is between 0.8% and 5.2%[12-14]. After heminephrectomy, if the remaining nephrons can still secrete urine, the urine will extravasate through the damaged collecting system. The extravasated urine will gather in the perinephric space and be wrapped by fibrous tissue to form a urinoma[15,16]. The patient’s drainage tube extravasated liquid contained urine, which was proved by biochemical verification after the operation. It met the diagnostic criteria for urinary fistula. Most heminephrectomy-related urinary fistula can be resolved by conservative treatment (e.g., percutaneous nephrostomy or percutaneous drainage)[17]. However, when conservative treatment is not effective, we should consider changing the treatment plan.
Conservative treatment achieved a therapeutic effect by continuous drainage to reduce the pressure on the renal pelvis to close the damaged collection system. However, a small number of patients require re-surgical removal of the residual kidney[18]. Meeks et al[17] reported 21 cases of urinary fistula after heminephrectomy, with an average continuous urinary fistula time of up to 53 d. Li et al[19] reported a case of ureteral stent implantation in the treatment of urinoma; the urinoma gradually disappeared after 5 mo. Re-surgical treatment may cause more serious complications because of difficulty in separating the residual kidney and blood vessel due to tissue adhesion. As far as we know, as early as the 1980s, scholars reported that four patients with urinary fistula after heminephrectomy were cured by the residual renal artery embolization[20,21]. In 1993, Japan’s Ogawa et al[22] reported that renal artery embolization was used to treat a severely impaired renal function patient with kidney urinary fistula and achieved good therapeutic effect. Wang et al[23] used arterial embolization to treat urinary fistula after repeated renal surgery and got satisfactory effect. Since then, Yamamoto et al[25] and Nohara et al[24] reported three cases of super-selective renal artery embolization in the treatment of renal carcinoma heminephrectomy with urinary fistula. The curative effect was satisfactory, and no obvious complications occurred[24,25].
In our patient, we observed the remnant renal arteries through preoperative CTA, which clarified the relationship between renal artery lesions and surrounding tissues and organs and provided a reliable basis for the choice of surgical methods. Previous studies on CTA, as a minimally invasive vascular imaging technique, have demonstrated that CTA can clearly show the renal artery and its branches, and the diagnostic accuracy of the anatomical variation of the renal artery is 100%[26,27]. DSA not only confirmed the residual renal artery but also realized the precise embolization of the residual renal artery, achieving the purpose of treatment while protecting the renal function. Permanent embolic agents have been used in previous cases, including coils, N-butyl-cyanoacrylate (NBCA) glue, and PVA particle embolic agents. We used 3F microcatheter to enter super-selectively the residual renal artery and embolized with 100-300 μm PVA granules. After embolization, only the stump of the artery remained. PVA particles are made from a polyvinyl alcohol foam sheet. They are a permanent embolic agent that can activate inflammatory reaction and focal angionecrosis, with vessel fibrosis developing over time[28]. Complications of renal artery embolism mainly include fever, nausea, abdominal and (or) waist pain, ectopic embolism, infection, etc. The incidence rate is less than 10% in the literature[29]. In previous reports, there have been many successful cases of using fibrin glue, coils, or NBCA glue for percutaneous obliteration of urinary fistula[30-37]. However, the operation can be cumbersome sometimes, and multiple uses of materials could also lead to excessive hospitalization costs. For instance, Nouri et al[30] used percutaneous puncture coils combined with NBCA glue to seal the urinary fistula tract and urinoma in 10 patients, and the highest case used 18 coils to seal the urinary fistula. In our case, residual renal artery embolization was used to treat urinary fistula, and a significant effect was achieved.
Although it is currently difficult to report large samples of arterial embolization for the treatment of urinary fistula, with the increase in the number of case reports and the development of interventional techniques, super-selective renal artery embolization is a minimally invasive, safe, effective and maximize retention renal function method to treat urinary fistula after heminephrectomy.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vermandois JAR S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li JH
| 1. | Jednak R, Kryger JV, Barthold JS, González R. A simplified technique of upper pole heminephrectomy for duplex kidney. J Urol. 2000;164:1326-1328. [PubMed] |
| 2. | Mackie GG, Stephens FD. Duplex kidneys: a correlation of renal dysplasia with position of the ureteral orifice. J Urol. 1975;114:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 352] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Darr C, Krafft U, Panic A, Tschirdewahn S, Hadaschik BA, Rehme C. Renal duplication with ureter duplex not following Meyer-Weigert-Rule with development of a megaureter of the lower ureteral segment due to distal stenosis - A case report. Urol Case Rep. 2020;28:101038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Zamani R, Martinez R, Reddy MP. Duplicated collecting system: not following Weigert-Meyer rule as a result of renal stone obstructing the lower ureteropelvic junction. Clin Nucl Med. 2004;29:386-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Jain P, Parelkar S, Shah H, Sanghavi B, Mishra P. Uncrossed complete ureteral duplication with dysplastic lower moiety: a violation of the Weigert-Meyer law. J Pediatr Urol. 2008;4:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Slaughenhoupt BL, Mitcheson HD, Lee DL. Ureteral duplication with lower pole ectopia to the vas: a case report of an exception to the Weigert-Meyer law. Urology. 1997;49:269-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Brown DM, Peterson NR, Schultz RE. Ureteral duplication with lower pole ectopia to the epididymis. J Urol. 1988;140:139-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Chen DX, Wang ZH, Wang SJ, Zhu YY, Li N, Wang XQ. Retroperitoneoscopic approach for partial nephrectomy in children with duplex kidney: A case report. World J Clin Cases. 2019;7:1169-1176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Huang WC, Elkin EB, Levey AS, Jang TL, Russo P. Partial nephrectomy vs radical nephrectomy in patients with small renal tumors--is there a difference in mortality and cardiovascular outcomes? J Urol. 2009;181:55-61; discussion 61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 629] [Cited by in RCA: 600] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 10. | Fergany AF, Saad IR, Woo L, Novick AC. Open partial nephrectomy for tumor in a solitary kidney: experience with 400 cases. J Urol. 2006;175:1630-3; discussion 1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 124] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, Marechal JM, Klotz L, Skinner E, Keane T, Claessens I, Sylvester R; European Organization for Research and Treatment of Cancer (EORTC); National Cancer Institute of Canada Clinical Trials Group (NCIC CTG); Southwest Oncology Group (SWOG); Eastern Cooperative Oncology Group (ECOG). A prospective randomized EORTC intergroup phase 3 study comparing the complications of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2007;51:1606-1615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 291] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 12. | Lesage K, Joniau S, Fransis K, Van Poppel H. Comparison between open partial and radical nephrectomy for renal tumours: perioperative outcome and health-related quality of life. Eur Urol. 2007;51:614-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Spana G, Haber GP, Dulabon LM, Petros F, Rogers CG, Bhayani SB, Stifelman MD, Kaouk JH. Complications after robotic partial nephrectomy at centers of excellence: multi-institutional analysis of 450 cases. J Urol. 2011;186:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Potretzke AM, Knight BA, Zargar H, Kaouk JH, Barod R, Rogers CG, Mass A, Stifelman MD, Johnson MH, Allaf ME, Sherburne Figenshau R, Bhayani SB. Urinary fistula after robot-assisted partial nephrectomy: a multicentre analysis of 1 791 patients. BJU Int. 2016;117:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Li HZ, Ma X, Zhang J, Zhang X, Wang BJ, Shi TP, Chen GF, Dong J, Ai X, Yan YJ, Wu Z, Hu DL. Retroperitoneal laparoscopic upper-pole nephroureterectomy for duplex kidney anomalies in adult patients. Urology. 2011;77:1122-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Titton RL, Gervais DA, Hahn PF, Harisinghani MG, Arellano RS, Mueller PR. Urine leaks and urinomas: diagnosis and imaging-guided intervention. Radiographics. 2003;23:1133-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 159] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 17. | Meeks JJ, Zhao LC, Navai N, Perry KT Jr, Nadler RB, Smith ND. Risk factors and management of urine leaks after partial nephrectomy. J Urol. 2008;180:2375-2378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Erlich T, Abu-Ghanem Y, Ramon J, Mor Y, Rosenzweig B, Dotan Z. Postoperative Urinary Leakage Following Partial Nephrectomy for Renal Mass: Risk Factors and a Proposed Algorithm for the Diagnosis and Management. Scand J Surg. 2017;106:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Li SX, Dagrosa LM, Pais VM Jr. Management of Urinoma Formation After Laparoscopic Cryoablation of Renal Cyst. J Endourol Case Rep. 2017;3:10-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Stefani P, Selli C, Nicita G, Lapini A, Dami A. Treatment of urinary fistulas after resection of horseshoe kidneys by selective arterial embolization. Cardiovasc Intervent Radiol. 1989;12:18-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Mitty HA, Dan SJ, Goldman HJ, Glickman SI. Urinary fistulas after partial nephrectomy: treatment by segmental renal embolization. AJR Am J Roentgenol. 1983;141:101-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Ogawa H, Yajima I, Hori N, Ishii Y, Gomi T. [Transcatheter arterial embolization for severely dysfunctioning kidney]. Nihon Jinzo Gakkai Shi. 1993;35:1073-1079. [PubMed] |
| 23. | Wang DS, Bird VG, Cooper CS, Austin JC, Winfield HN. Laparoscopic upper pole heminephrectomy for ectopic ureter: initial experience. Can J Urol. 2004;11:2141-2145. [PubMed] |
| 24. | Nohara T, Matsuyama S, Kawaguchi S, Miyagi T, Seto C, Mochizuki K. Usefulness of selective renal artery embolization for urinary fistula following partial nephrectomy: Two case reports. Mol Clin Oncol. 2016;5:158-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Yamamoto T, Kinoshita H, Ikeda J, Sugi M, Matsuda T. Refractory urinary fistula with infundibular stenosis after partial nephrectomy. Int J Urol. 2015;22:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Davarpanah AH, Pahade JK, Cornfeld D, Ghita M, Kulkarni S, Israel GM. CT angiography in potential living kidney donors: 80 kVp vs 120 kVp. AJR Am J Roentgenol. 2013;201:W753-W760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Kapoor A, Kapoor A, Mahajan G, Singh A, Sarin P. Multispiral computed tomographic angiography of renal arteries of live potential renal donors: a review of 118 cases. Transplantation. 2004;77:1535-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Fernández-Alvarez V, Suárez C, de Bree R, Nixon IJ, Mäkitie AA, Rinaldo A, Downer J, Ferlito A. Management of extracranial arteriovenous malformations of the head and neck. Auris Nasus Larynx. 2020;47:181-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | Huang N, Yang WZ, Jiang N, Zheng QB, Huang JY, Shen Q. Application of Guglielmi detachable coils in embolization of iatrogenic renal hemorrhage. Ann Vasc Surg. 2013;27:1081-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Nouri YM, Chu HH, Shin JH, Tsauo J, Kim CS, Hong BS, Kim JW, Kim JH. Percutaneous Obliteration of Urinary Leakage after Partial Nephrectomy Using N-Butyl-Cyanoacrylate Obliteration of the Urinoma with or without Coil Embolization of the Fistula Tract. J Vasc Interv Radiol. 2019;30:2002-2008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Muto G, D'Urso L, Castelli E, Formiconi A, Bardari F. Cyanoacrylic glue: a minimally invasive nonsurgical first line approach for the treatment of some urinary fistulas. J Urol. 2005;174:2239-2243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Okada T, Kono Y, Matsumoto K, Utsunomiya N, Tsunemori H, Kawakita M. [Percutaneous Fibrin Glue Injection for Persistent Urinary Leakage after Partial Nephrectomy : A Case Report]. Hinyokika Kiyo. 2017;63:107-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 33. | Aning JJ, Stott MA, Watkinson AF. Glue ablation of a late-presentation urinary fistula after partial nephrectomy. Br J Radiol. 2009;82:e246-e248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | French DB, Marcovich R. Fibrin sealant for retrograde ureteroscopic closure of urine leak after partial nephrectomy. Urology 2006; 67: 1085.e1-1085. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Aslan G, Men S, Gülcü A, Kefi A, Esen A. Percutaneous embolization of persistent urinary fistula after partial nephrectomy using N-butyl-2-cyanoacrylate. Int J Urol. 2005;12:838-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Tekin MI, Peşkircioğlu L, Boyvat F, Ozkardes H. Practical approach to terminate urinary extravasation: percutaneous fistula tract embolization with N-butyl cyanoacrylate in a case with partial nephrectomy. Tech Urol. 2001;7:67-69. [PubMed] |
| 37. | Selli C, De Maria M, Manica M, Turri FM, Manassero F. Minimally invasive treatment of urinary fistulas using N-butyl-2-cyanoacrylate: a valid first line option. BMC Urol. 2013;13:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |