Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3157
Peer-review started: November 30, 2020
First decision: December 24, 2020
Revised: January 12, 2021
Accepted: February 12, 2021
Article in press: February 12, 2021
Published online: May 6, 2021
Processing time: 143 Days and 5.9 Hours
Subclavian vein stenosis or occlusion may be caused by a transvenous pacemaker, which makes the reimplantation of a new pacemaker lead difficult. Transvenous pacemaker lead implantation-related subclavian vein occlusion may present difficulty with regard to cardiac resynchronization therapy (CRT) upgrade.
We report the case of a 46-year-old man who was admitted with total subclavian vein occlusion caused by a permanent pacemaker that had been implanted 2 years previously. We successfully treated this patient with an upgrade to a CRT pacemaker by utilizing transferable interventional coronary and radiological techniques. The patient recovered uneventfully during the follow-up period.
CRT upgrade is still a viable technique for the treatment of subclavian vein obstruction caused by previous pacemaker implantation.
Core Tip: Subclavian vein stenosis or occlusion may be caused by a transvenous pacemaker, which makes the reimplantation of a new pacemaker lead difficult. Transvenous pacemaker lead implantation-related subclavian vein obstruction may present difficulty with regard to cardiac resynchronization therapy (CRT) upgrade. We successfully treated a patient who was admitted with total subclavian vein occlusion caused by a permanent pacemaker that had been implanted 2 years previously, with an upgrade to a CRT pacemaker by utilizing transferable interventional coronary and radiological techniques.
- Citation: Zhong JY, Zheng XW, Li HD, Jiang LF. Successful upgrade to cardiac resynchronization therapy for cardiac implantation-associated left subclavian vein occlusion: A case report. World J Clin Cases 2021; 9(13): 3157-3162
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3157.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3157
Implantation of pacemakers is a widely adopted treatment for cardiac arrhythmia. However, pacemaker implantation is associated with some complications including heart failure, lead dislodgment, lead failure, pericarditis, infection, skin erosion, hematoma, venous thrombosis, and malfunction[1]. While rare, these complications may occur long after the implantation procedure[2]. In particular, the etiology of 15%-45% of cases of venous thrombosis is attributed to implantation of a transvenous pacemaker, depending on the study cohorts[3,4]. One form of venous thrombosis, subclavian vein obstruction, can cause difficulty in the re-implantation of new pacemaker leads, when needed to upgrade a transvenous pacemaker to a cardiac resynchronization therapy (CRT)-P or CRT-D. We report a patient who developed total subclavian vein occlusion caused by a permanent pacemaker that had been implanted 2 years previously. We successfully treated this patient with a CRT-P through transferable interventional coronary and radiological techniques.
The 46-year-old man presented with dyspnea on exertion upon admission.
The patient who had congestive heart failure was diagnosed with high-degree atrioventricular blockage after treatment of a permanent pacemaker in DDD mode (Medtronic) on January 1, 2018.
He started having dyspnea on exertion from time to time about 6 mo ago.
He denied any family diseases.
The patient’s blood pressure was 86/60 mmHg, and his heart rate was 60 bpm with right ventricular pacing.
The patient had an elevated level of N terminal pro brain natriuretic peptide of 1653 pg/mL, indicating heart failure, which was classified as class II–III according to the New York Heart Association (NYHA) Classification of Heart Failure.
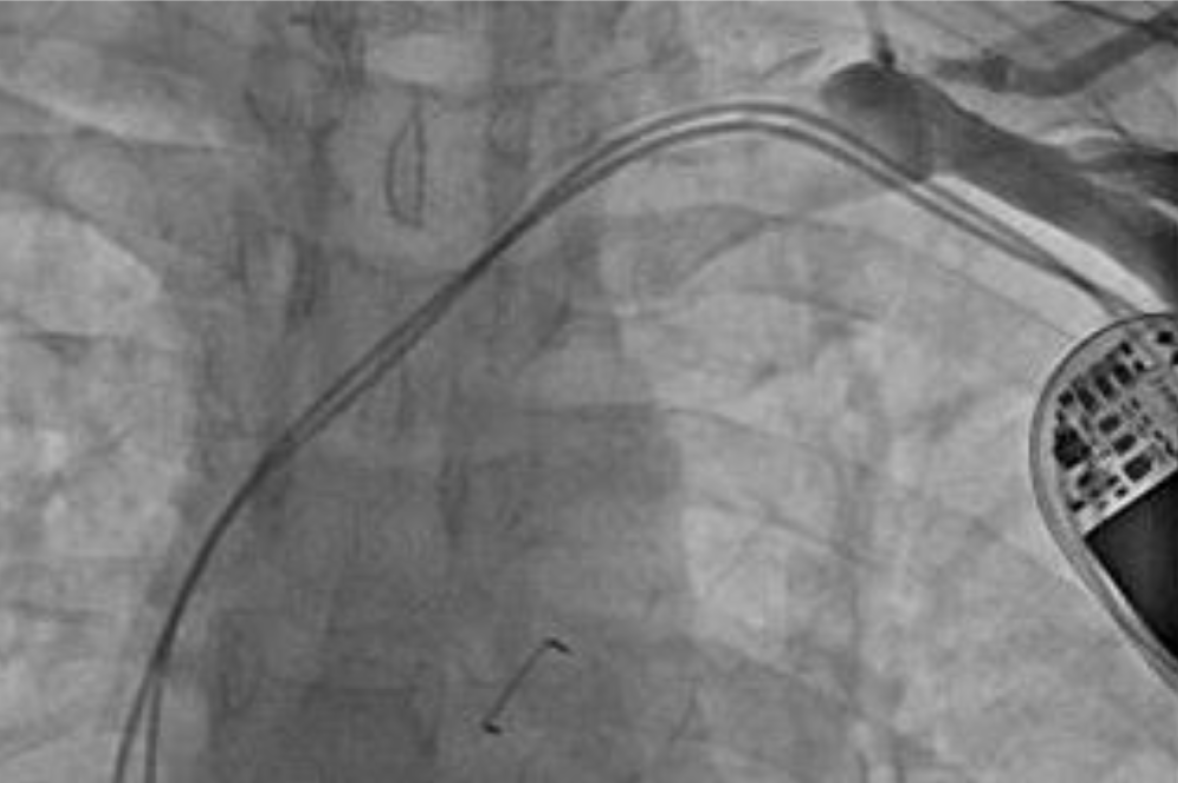
Echocardiography showed impaired left ventricular (LV) systolic motion with a LV ejection fraction of 33%, a ventricular septum thickness of 4 mm (indicating atrophy), and a LV diameter of 69 mm (indicating LV dilation). The left atrium was also dilated with severe mitral regurgitation and mild tricuspid regurgitation. The patient also had moderate pulmonary hypertension. The ventricular pacing rhythm with QRS duration > 170 ms was recorded in the 12-lead electrocardiogram. The patient was diagnosed with complete obstruction of the left subclavian vein due to two leads previously implanted as revealed by venography (Figure 1).
The patient was previously given diuretics, vasodilators, sacubitril-valsartan sodium tablets, β-blockers, and spironolactone for treatment of heart failure, following the current heart failure treatment guidelines.
As coronary angiography showed no coronary disease, and no tachycardia or atrial fibrillation were observed by Holter monitoring, we proposed a CRT-P upgrade for treatment of heart failure.
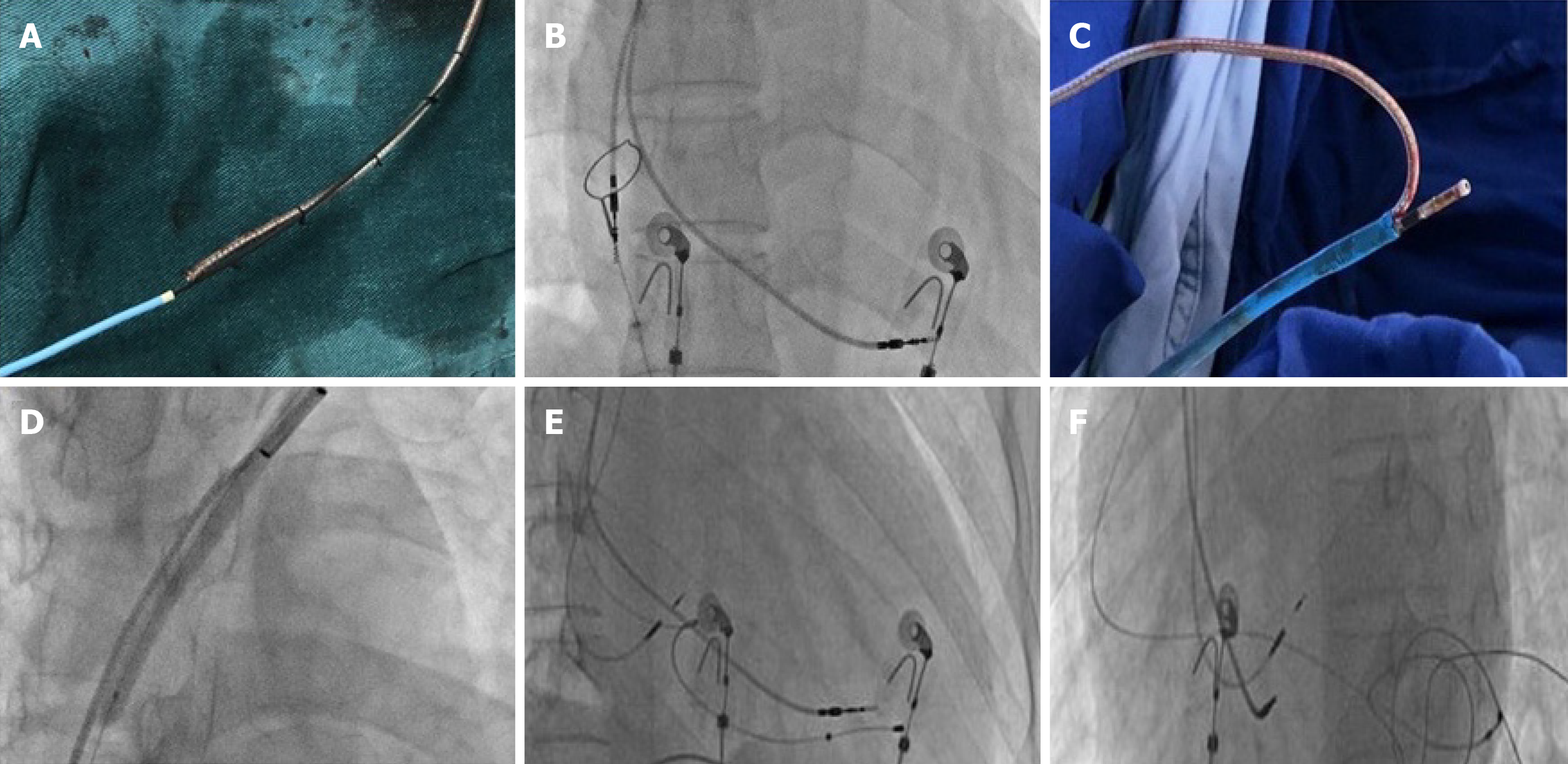
A 0.035-in Terumo wire (Terumo Corporation, Tokyo, Japan) was introduced via a left subclavian puncture, but we could not advance the wire through the occluded region, even after switching to a Radifocus guidewire (Terumo Corporation) and a 0.018-in V-18 control wire (Boston Scientific Corporation, Boston, MA, United States). We then decided to re-canalize the left subclavian vein through femoral vein access. The atrial lead was gently pulled back with a counterclockwise rotation and stabilized in the right atrium without any anchoring forces. Proximally cut lead portions and the Radifocus guidewire tip were bundled together with a suture firmly 6 times (Figure 2A). An 8 French sheath was inserted into the right femoral vein, and a goose-neck snare was advanced to the lower edge of the right atrium (Figure 2B). The atrial lead tip was then snared and pulled into the 8 French femoral vein sheath for final retrieval (Figure 2C). Following the atrial lead body, the Radifocus guidewire passed the lesion. A Finecross catheter was then advanced over the wire, and the Radifocus guidewire was replaced by a 0.018-in V-18 control wire to provide additional support for balloon inflation. Next, we performed balloon venoplasty in the left subclavian vein using a balloon of 4.0 mm × 60 mm (Bantam, Wexford, Ireland) and a balloon of 8.0 mm × 80 mm (Abbott, Santa Clara, CA, United States) (Figure 2D). With the 9 French short sheath supports, we used a stiffer guidewire (Terumo Corporation) simultaneously to deliver an 8 French long sheath past the obstruction. Following that, the LV lead (Medtronic, Inc. Minneapolis, MN, United States) was implanted successfully. Before the LV lead implantation procedure, we attempted to insert the selected secure lead (model 3830, Medtronic, Inc.) into the left bundle branch area to narrow the QRS duration. Unfortunately, the condition of the lead was unstable, and all parameters were abnormal. We then implanted the selected secure lead (model 3830, Medtronic, Inc.) in the right atrium. The rest of the procedure was completed without any difficulty, and the time of pacemaker implantation was 240 min (Figure 2E and F).
The leads were stable with normal parameters and a narrow QRS during a routine follow-up visit. Fortunately, visible blood flow was observed on enhanced computed tomography. The cardiac function in this patient was NYHA functional class I.
Subclavian vein stenosis/occlusion is a known complication associated with implantation of a transvenous pacemaker[3]. In the present case, the patient developed subclavian vein obstruction likely due to endothelial disruption resulting from mechanical stress of the leads, which ultimately led to fibrosis and narrowing of the lumen. The management of pacemaker lead-induced subclavian vein obstruction includes medical, interventional, or surgical interventions. Surgical intervention has been the first-line treatment for patients with subclavian vein obstruction. However, in the past 20 years, endovascular reconstruction, which can minimize the risk of bleeding, has become more popular[5].
In this patient, venography demonstrated total subclavian vein occlusion. Interventional procedures such as angioplasty and stenting were the primary choices for this patient. If visible blood flowed back to the right atrium, the passage of wires to the stenotic lesion would be recommended. Also, retrograde angioplasty from the femoral vein to pass the obstruction may be an option. Another choice could be to use a laser sheath as a lead extraction tool, as described by Pecha et al[6] and Hasumi et al[7] However, a laser sheath is not enough in the vast majority of hospitals in China. For this patient, we finally fixed a Radifocus guidewire tip and proximally cut the lead portions instead of using a bulldog lead extender to pass the lesion and perform venoplasty.
Previously, Leacche et al[8] reported that lead extraction alone could cause thrombosis and thus believed that it carried a high risk for subsequent re-occlusion with a low likelihood of sustaining patency. In another study performed with a cohort of 28 patients who received treatment for pacemaker-related superior vena cava syndrome, the primary patency rates were 18% and 9% at 6 and 12 mo, respectively[9]. The Heart Rhythm Society recommends that the entrapment of the pacemaker leads should be avoided prior to stent deployment[10]. Previous studies reported that diagnosis of occlusive lesions with magnetic resonance angiography was accurate, which could be used to evaluate the outcome of patients with atherosclerosis and embolus[11]. For this patient, the concern was that the pressure posed by the metallic stent on the wires could lead to malfunction of the pacemaker. Thus, instead of using stenting to remove the subclavian vein obstruction caused by the previously implanted leads, we used the CRT-P technique. We observed that the patient recovered uneventfully at least during the follow-up period. In consideration of the previous right ventricle lead, enhanced computed tomography was selected to evaluate the degree of subclavian vein stenosis, and visible blood flow was observed.
This preliminary experience is limited to one case and difficult to generalize. The relatively short follow-up period cannot prejudge long-term outcomes in this patient.
This report demonstrates that CRT upgrade is still a viable technique for the treatment of subclavian vein obstruction caused by previous pacemaker implantation if appropriate additional technologies such as transferable interventional coronary and radiological techniques are available.
We appreciate the following authors’ help on this study: Ye HH, Chen GF, Wu H, Peng XH, Shen JB, Zhuo SS, and Wang DJ.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaypakli O S-Editor: Zhang H L-Editor: Webster JR P-Editor: Wang LL
| 1. | Kirkfeldt RE, Johansen JB, Nohr EA, Jørgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186-1194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 487] [Cited by in RCA: 643] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 2. | Laurent G, Ricolfi F, Wolf JÉ. Venous stenting as a treatment for pacemaker-induced superior vena cava syndrome. Arch Cardiovasc Dis. 2013;106:624-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Spittell PC, Hayes DL. Venous complications after insertion of a transvenous pacemaker. Mayo Clin Proc. 1992;67:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 129] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Worley SJ. Implant venoplasty: dilation of subclavian and coronary veins to facilitate device implantation: indications, frequency, methods, and complications. J Cardiovasc Electrophysiol. 2008;19:1004-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Madkaiker AN, Krishna N, Jose R, Balasubramoniam KR, Murukan P, Baquero L, Varma PK. Superior Vena Cava Syndrome Caused by Pacemaker Leads. Ann Thorac Surg. 2016;101:2358-2361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Pecha S, Burger H, Castro L, Gosau N, Atlihan G, Willems S, Reichenspurner H, Hakmi S. The Bridge Occlusion Balloon for Venous Angioplasty in Superior Vena Cava Occlusion. Braz J Cardiovasc Surg. 2019;34:368-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Hasumi E, Fujiu K, Kojima T, Kinoshita O, Nawata K, Yamauchi H, Ono M, Komuro I. Novel extraction technique of retained pacemaker and defibrillator lead during heart transplantation. PLoS One. 2018;13:e0203172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Leacche M, Katsnelson Y, Arshad H, Mihaljevic T, Rawn JD, Sweeney MO, Byrne JG. Delayed presentation of totally avulsed right superior vena cava after extraction of permanent pacemaker lead. Pacing Clin Electrophysiol. 2004;27:262-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Asif A, Salman L, Carrillo RG, Garisto JD, Lopera G, Barakat U, Lenz O, Yevzlin A, Agarwal A, Gadalean F, Sachdeva B, Vachharajani TJ, Wu S, Maya ID, Abreo K. Patency rates for angioplasty in the treatment of pacemaker-induced central venous stenosis in hemodialysis patients: results of a multi-center study. Semin Dial. 2009;22:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, Epstein LM, Friedman RA, Kennergren CE, Mitkowski P, Schaerf RH, Wazni OM; Heart Rhythm Society; American Heart Association. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: this document was endorsed by the American Heart Association (AHA). Heart Rhythm. 2009;6:1085-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 744] [Cited by in RCA: 792] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 11. | Razek AA, Saad E, Soliman N, Elatta HA. Assessment of vascular disorders of the upper extremity with contrast-enhanced magnetic resonance angiography: pictorial review. Jpn J Radiol. 2010;28:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |