Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3130
Peer-review started: November 23, 2020
First decision: December 21, 2020
Revised: January 4, 2021
Accepted: March 3, 2021
Article in press: March 3, 2021
Published online: May 6, 2021
Processing time: 143 Days and 10.7 Hours
Acute urinary retention (AUR) is rare during pregnancy.
We report on three pregnant women with AUR between the 10th and 18th wk of gestation. Case 1 was first diagnosed as urinary tract infection and developed a urinary tract infection due to urinary retention caused by urethral obstruction. Case 2 had a history of previous abdominal surgery for pelvic tuberculosis, leading to severe adhesions and a persistent retroverted uterus. In case 3, healthcare providers focused on the patient’s gastrointestinal symptoms and did not investigate her inability to void. Case 1 required manual disimpaction of the uterus and the knee-chest position. The other cases required immediate catheterization. The condition resolved in cases 1 and 2; these patients had normal pregnancies. Case 3 had severe complications at the time of consultation, leading to an abortion.
Retroverted uterus is the most common cause of AUR. Prompt recognition and diagnosis are required. Clinicians should be aware of the risk factors, etiology, and clinical presentation of AUR in the first and second trimester of pregnancy.
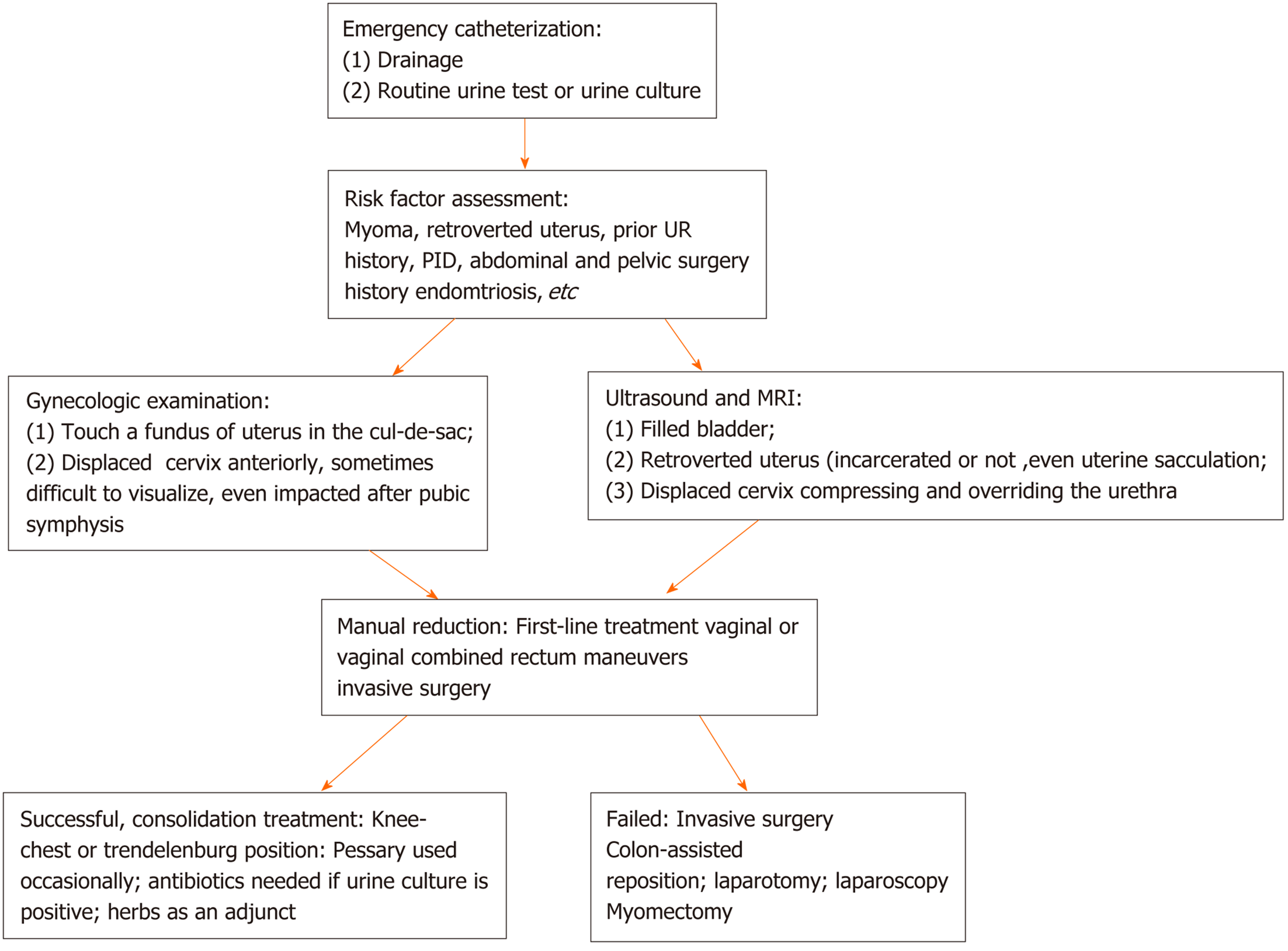
Core Tip: Acute urinary retention (AUR) during pregnancy can have a negative impact on maternal and fetal health. We propose a diagnostic and therapeutic algorithm for the management of AUR in the first and second trimester. A retroverted uterus is the most common cause of AUR. Clinical symptoms, physical examination, and imaging should be used for diagnosis of a retroverted gravid uterus and AUR. Treatment may include conservative measures and/or bladder decompression with an indwelling Foley catheter or manual reduction. Subsequently, the uterus should be kept anterior with a normal vesicourethral angle. Occasionally, a soft pessary or antibiotics may be used.
- Citation: Zhuang L, Wang XY, Sang Y, Xu J, He XL. Acute urinary retention in the first and second-trimester of pregnancy: Three case reports . World J Clin Cases 2021; 9(13): 3130-3139
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3130.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3130
Acute urinary retention (AUR) is rare during pregnancy, but it can be associated with maternal and fetal complications. As pregnancy progresses, anatomical and functional changes in the lower urinary tract can result in pathological conditions such as AUR, which manifests as a sudden inability to micturate with or without pain[1]. The risk of AUR in a healthy pregnant woman is 0.47%. AUR can occur at any gestational age but is most often observed between the 9th and 16th wk of gestation[2]. Risk factors include retroverted enlarged uterus, adenomyosis and myomas, cervical pregnancy, maternal anterior sacral meningocele, pelvic adhesions, congenital uterine anomalies, endometriosis, and uterine prolapse[3-9].
Pregnant women with AUR are treated in the emergency department, urology clinic, or obstetrics clinic. Prompt identification of underlying pathology is the key to successful management and avoidance of adverse outcomes such as renal failure, bladder or uterine rupture, colon necrosis, urinary tract infection, uterine sacculation, spontaneous abortion, or fetal death.
Here, we report on three pregnant women with AUR who presented to our institution between the 10th and 18th wk of gestation. We discuss the etiology of AUR during pregnancy based on a review of previously published literature (Table 1). The three cases were managed according to our clinical experience. Two of the cases required immediate catheterization, knee-chest position, and manual disimpaction of the uterus. The third case had severe complications at the time of consultation, which resulted in an abortion. This case series should raise awareness among clinicians of the risk factors, etiology, clinical presentation, diagnosis, and management of AUR in the first and second trimester of pregnancy.
| Case | Year | GA | MG | Risk Factors | Symptoms | Treatment and outcome |
| 1 | 2012 | G3P1 | 31 | None | Constipation, tenesmus, fatigue, vulva edema renal failure | Indwelling catheter; miscarriage |
| 2 | 2018 | G1P0 | 27 | IVF-ET, prior abdominal surgery for TB | Urinary retention | Intermittent; self-catheterization; herbs; normal pregnancy |
| 3 | 2018 | G2P0 | 31 | None | Urine frequency and urgency, urinary retention | Manual reduction, knee-chest position; herbs. Normal pregnancy |
Our research team conducted a search of the PubMed, Web of Science, and Science Direct databases using the following terms and combinations: “AUR in/ during/and/pregnancy”, “retroverted gravid uterus”, “incarcerated gravid uterus”, “uterine incarceration”, “impacted gravid uterus”, “urinary retention in pregnancy and infection”, and “urinary tract infection in pregnancy.” The search was limited to articles published in the English language. The initial search provided 30 articles, of which 12 were excluded because they were published before 1980 or were not full texts. Finally, 18 full text articles were reviewed; the majority of these were case reports (Table 2).
| Ref. | Year | Case | MA, G/P | Risk factor | Reason | GA in wk | Presentation | Treatment | Outcome |
| Goldberg et al[4] | 1981 | 1 | 29/G4P2 | None | Prolapsed, progressive protrusion of gravid cervix out of the vestibule | 10 | AUR | IDC; cystoscopy; pessary | No recurrence |
| Chauleur et al[7] | 2008 | 2 | 1st: 33, G2P0; 2nd: 41, G1P0 | Fibroid | Fibroid incarceration | 1st: 5; 2nd: 6 | 1st: AUR; 2nd: Frequent and urgent, small volume urination | Myomectomy | 1st: Miscarriage; 2nd: Normal pregnancy |
| Kubota et al[3] | 2012 | 1 | 31/not mentioned | Protrusion of the meninges | ASM | 28 | Dysuria | ISC | CS at 35 wk |
| Nelson et al[26] | 1986 | 1 | 30/G3P2 | Incarcerated uterus | 14 | Dysuria and abdominal pain | IDC MR | An uneventful pregnancy | |
| Yang et al[13] | 2004 | 5 | 31 (range, 25-37)/3 cases: G2P1; 2 cases: G1P0 | Not mentioned | Not mentioned | 11-14 | All AUR | Water-limiting before sleep, prone position for a while before urination, leaning forward when initiating voiding, avoiding any Valsalva | No voiding problems after 16th wk |
| Lam et al[27] | 2015 | 1 | 31/G5P1 | RUTI, laparoscopy for PID | Incarcerated uterus | 18 | Urinary frequency and urgency, dysuria | Antibiotics, IDC | An uncomplicated pregnancy |
| Heazell et al[8] | 2004 | 1 | 33/G3P2 | None | Cervical pregnancy | 8 | AUR, abdominal pain and vaginal bleeding | Emergency evacuation, laparotomy | Hysterectomy |
| Newell et al[15] | 2014 | 2 | 1st: 41/G1P0; 2nd: 33/G2P1 | None | Retroverted uterus with incarceration | 1st: 17; 2nd: 14 | 1st: UR and constipation; lower limb edema and hypertension. 2nd: UR | 1st: MR; 2nd: ISC | 1st: Fetal death after reduction; 2nd: An uncomplicated pregnancy |
| Slama et al[23] | 2015 | 3 | 1st: 37/G6P2; 2nd: 42/G5P3; 3rd: 22/G15P5 | None | Uterine incarceration | 1st: 13; 2nd: 13; 3rd: 21 | 1st: UR; 2nd: UR; 3rd: UR, nausea | 1st: ISC, Pessary; 2nd: ISC, Pessary; 3rd: Pessary | Symptoms alleviation |
| Inaba et al[25] | 2005 | 2 | 1st: 27/G1P0; 2nd: 32/G3P0 | 1st: Prolapse uterus IVF; 2nd: Endometriosis | Uterine incarceration | 1st: 11; 2nd: 14 | 1st: UR; 2nd: UR | 1st: KCP, MR; 2nd: MR many times | 1st: no recurrence; 2nd: not relieved, uterine rupture at 34 wk, CS |
| Danis et al[12] | 2015 | 1 | 25/G1P0 | None | Retroverted uterus without incarceration | 18 | UR | MR, colonoscopy-assisted rectosigmoid insufflation | An uneventful pregnancy |
| Kim et al[6] | 2018 | 2 | 1st: 34/multiparous; 2nd: 31/primigravid a | Adenomyosis and myoma | Incarceration of uterus | 1st: 7.2; 2nd: 6 | 1st: UR; 2nd: UR | 1st: MR, pessary; 2nd: IDC, MR | 1st: An uncompleted pregnancy; 2nd: A spontaneous abortion |
| Dierickx et al[21] | 2011 | 4 | 1st: 39/G1P0; 2nd: 29/G1P0; 3rd: 28/G3P2; 4th: 34/G2P1 | 1st: Endometriosis; 2nd: Deep sacral concavity with prominent promontorium; 3rd: None; 4th: None | Incarcerated uterus | 1st: 22; 2nd: 22, 25; 3rd: 15; 4th: 18 | 1st: UR and abdominal pain; 2nd: Dysuria and incomplete bladder emptying; 3rd: UR; 4th: Mictalgia | All sigmoidoscopy1st, 3rd, 4th: Successful; 2nd: 22 wk successful/25 wk not successful, laparotomy | 1st and 3st: Vaginal delivery at term; 2nd and 4th: CS at term |
| Yohannes et al[24] | 2002 | 1 | Not mentioned/G2P1 | None | Incarcerated uterus | 15 | UR and abdominal pain | IDC, MR, KCP | No urologic problem |
| Suzuki et al[28] | 2009 | 2 | 1st: 26/G1P0; 2nd: 26/G1P0 | None | Retroverted uterus | 1st: 12; 2nd: 12 | 1st: UR; 2nd: UR | Both: IDC, limiting fluid intake before sleep; prone position for a while before urination | |
| Smalbraak et al[5] | 1991 | 4 | 1st: 31/G2P1; 2nd: 28/G2P1; 3rd: 26/G2P0; 4th: 34/G2P1 | None | Retroverted uterus | 1st: 15; 2nd: 12, 25; 3rd: 16; 4th: 14 | 1st: UR and abdominal pain; 2nd: Abdominal pain and micturition; 3rd: Unpalpable uterine fundus; 4th: Micturition, abdominal pain | 1st: IDC MR; 2nd: None; 3rd: MR; 4th: Antibiotics | 1st: A normal pregnancy; 2nd: CS at term for breech presentation; 3st: CS at 32 wk |
| Martínez-Varea et al[22] | 2013 | 1 | 35/G7P1 | Uterine prolapse (grade 2) | Uterine prolapse | 14 + 3 | Hypogastric pain, unable to void urine | IDC, Arabin ceralage pessary | No urologic problem |
| Hamod et al[17] | 2002 | 1 | 27/G1P0 | Fundal fibroid | Incarcerated Uterus | 18 | Urinary frequency, passing small volumes of urine | ISC; antibiotics for fibroid degeneration | CS at 36 wk |
Case 1: A 31-year-old pregnant Chinese woman (gravida 2 para 0) at 13 + 5 wk of gestation presented with intermittent dysuria for 1 mo and vaginal bleeding for 3 d and was admitted to the Obstetrics Department on October 8, 2018.
Case 2: A 27-year-old pregnant Chinese nulligravida presented to the Obstetrics Department with intermittent urinary retention at 17 wk of gestation on December 26, 2018.
Case 3: A 31-year-old pregnant woman (gravida 3 para 1, abortion 1) at 14 + 5 wk of gestation presented with constipation and no bowel movements for 10 d and was admitted to the Obstetrics Department on February 8, 2011.
Case 1: The patient’s pregnancy was uneventful until 10 wk of gestation when she experienced frequent urination and urgency. The patient was diagnosed with cystitis but was not provided treatment at her local hospital. Subsequently, the patient experienced abdominal distension, urinary retention, and persistent dysuria. Ultrasound imaging indicated excessive residual urine. Catheterization for 5 d did not relieve the patient’s symptoms. The patient visited the Emergency Center at a local hospital, where color Doppler ultrasound showed no obvious urinary system abnormalities. Routine urinalysis was positive for occult blood (3+) and white blood cells (3+). The patient was diagnosed with urinary tract infection and urine retention. She was treated with an indwelling catheter and intravenous cephalosporin for 3 d but showed little improvement. At 13 wk of gestation the patient attended our obstetric clinic, and her AUR was managed with re-catheterization.
Case 2: The patient was admitted to the Emergency Department for abdominal pain and sudden dysuria at 13 wk of gestation. A Foley catheter was inserted, and 1.2 L of clear urine was promptly evacuated. Routine blood and urine tests were negative. Five days later, the patient was voiding normally, and she was discharged. Within 2 wk, the patient required intermittent catheterization.
Case 3: The patient experienced bloating, lower abdomen pain, and distension. Her symptoms had been accompanied by fatigue and vulval swelling for 2 d.
Case 1: The patient had an abortion 1 year ago.
Case 2: The patient was infertile due to pelvic tuberculosis (TB). The patient underwent laparoscopic surgery for adhesions 2 years ago and received one course of oral medication for TB. The patient became pregnant by in vitro fertilization.
Case 3: The patient delivered one baby 10 years ago and had an abortion 1 year ago.
Cases 1-3: The personal and family history of all patients was unremarkable.
Case 1: Gynecological examination showed a small amount of bloody vaginal discharge, the cervix was displaced superiorly, and a partially compressed urethra, but no urethral prolapse. Palpation by two fingers in the vagina revealed a large painless retroverted uterus with little mobility.
Case 2: Gynecological examination detected a retroverted uterus.
Case 3: Gynecological examination demonstrated bilateral swelling of the vulva and vulval edema that compressed the vaginal orifice such that it could only accommodate one finger, and a detailed gynecological examination was not possible.
Case 1: Routine urinalysis was positive for occult blood (2+) and white blood cells, (3+) and urine culture showed Enterococcus faecalis.
Case 2: Routine urinalysis was negative.
Case 3: Renal function tests showed uric acid, creatinine, and urea nitrogen levels were high enough to be diagnosed as acute renal failure.
Case 1: Ultrasound showed that the retroverted uterus obstructed the urethra (Figure 1).
Case 2: Ultrasonography detected a retroverted uterus.
Case 3: Ultrasound revealed a large cystic mass approximately 20.2 cm × 14.0 cm × 16.0 cm located in front of the uterus, the uterus was obviously compressed in the posterior part of the pelvis, bilateral ureteral dilatation and hydronephrosis, and a normal fetus.
Case 1: The patient was diagnosed with AUR and urinary tract infection during pregnancy.
Case 2: The patient was diagnosed with AUR during pregnancy.
Case 3: The patient was diagnosed with AUR and renal failure.
Case 1: The patient was placed in the lithotomy position for manual reduction of the uterus. The retroverted uterus was gently pushed using two fingers in the posterior fornix of the vagina, assisted by one finger in the rectum. The patient did not complain of any discomfort during this maneuver. She was treated with penicillin and advised to adopt the knee-chest prone position three times a day.
Case 2: The patient was advised to adopt the knee-chest prone position daily.
Case 3: The patient was unable to urinate after admission. The patient received an indwelling catheter, and a total of 5400 mL of light brown urine was evacuated during the next 9 h. Subsequent ultrasound showed no pelvic mass, which confirmed the diagnosis of urinary retention.
Case 1: The catheter was removed after 5 d, and the patient was able to void normally. Twelve days later, routine urinalysis and urine culture were unremarkable, and the patient was discharged. The patient was advised to adopt a knee-chest prone position, as before, three times a day until 20 wk of gestation. The patient’s symptoms did not recur, and she delivered a baby at 38 wk gestation.
Case 2: After 17 wk of gestation, the uterus was enlarged and had moved forward. The patient’s condition resolved spontaneously.
Case 3: On the 3rd d of admission, the patient defecated, and her renal function test was normal. After 10 d, the catheter was removed, but the patient had a miscarriage.
Our literature review identified 35 cases of AUR during the first and second trimesters of pregnancy. All cases occurred at 5-18 wk gestation, peaking at 11-14 wk, except one that occurred at 28 wk. There was no significant difference in the prevalence of AUR between primiparas and multiparas.
Retroversion of the uterus occurs in an estimated 11%-15% of women during pregnancy; of these, 1.4% experience AUR[10]. A retroverted uterus is the most common cause of AUR[11]. A retroverted gravid uterus displaces the cervix, compresses the lower bladder, and interferes with drainage to the urethra[12]. Yang and Huang[13] observed three women with a retroverted gravid uterus and found no limitation of urethral mobility during a Valsalva maneuver. They reported compression of the lower bladder with straining[13]. Typically, the uterus lifts out of the pelvis at the end of the first trimester. A retroverted gravid uterus may become incarcerated if the uterus becomes trapped between the sacral promontory and the pubic symphysis. Incarceration of a retroverted gravid uterus is a rare cause of AUR, occurring in 1 in 3000 pregnancies[14].
Healthcare providers may lack knowledge of the urogynecological complications that can occur during pregnancy and may not perform a pelvic examination in patients presenting with urinary retention. Published evidence suggests that the most common symptoms of retroverted gravid uterus in the second trimester are urinary retention, vaginal bleeding, abortion, dysuria, overflow incontinence, incomplete voiding, rectal pressure, tenesmus, and constipation[9]. However, other symptoms may be present. Newell et al[15] described delayed diagnosis of incarcerated uterus in two patients who presented with urinary retention in the second trimester. One patient suffered lower limb edema and severe hypertension, but abdominal ultrasound showed bilateral hydronephrosis as a result of obstruction secondary to uterine incarceration[15]. Hsu et al[16] reported a case of asymptomatic uterine incarceration at term[16]. In case 1 of the current case series, the patient was first diagnosed as urinary tract infection, which is the most common cause of dysuria in pregnancy. The patient developed a urinary tract infection due to urinary retention caused by urethral obstruction. Case 2 had a history of previous abdominal surgery for TB, which resulted in severe adhesions and a persistent retroverted uterus. In case 3, healthcare providers focused on the patient’s gastrointestinal symptoms and did not investigate her inability to void. In the first two cases, the cervix was tilted upward towards the upper part of the symphysis pubis, and the uterus was retroverted but not incarcerated. The uterus may move forward naturally during gestation. Thus, some cases may be safely managed with conservative treatment[17].
In addition to clinical symptoms and physical examination, imaging is a useful adjunct for diagnosis of a retroverted gravid uterus and AUR. While ultrasound is the first choice, the elongated cervix can be difficult to visualize behind the pubic symphysis, and a retroverted uterus can be misdiagnosed as ectopic pregnancy or placenta previa[18]. Magnetic resonance imaging (MRI) may be useful for complex cases. Dierickx et al[19] suggested that MRI was the imaging method of choice for posterior incarceration of the uterus and recommended MRI prior to manual or colonoscopy-assisted repositioning in order to exclude incarceration in the anterior direction[19].
Treatment of AUR due to retroverted uterus can include conservative measures and more invasive interventions. High risk patients should limit fluid intake before sleep, change from the supine to the prone position before getting up, lean forward when initiating voiding, avoid the Valsalva maneuver, use a Crede maneuver to initiate or maintain voiding, and adopt the knee-chest position[13]. Minimally invasive procedures include bladder decompression by insertion of an indwelling Foley catheter or manual reduction. Patterson et al[20] recommends placing a tenaculum on the posterior lip of the cervix while the patient is in Trendelenburg or the knee-chest position[20]. Case 1 was put in a lithotomy position, and gentle and sustained pressure from the clinician’s fingers was used to push the fundus of the uterus upward from the posterior fornix of the vagina. In this case, vaginal reduction was combined with rectal reduction. Manual reduction is not recommended after 20 wk of gestation, as it is associated with an increased risk of preterm labor. If manual reduction fails, invasive surgery, including colonoscopy-assisted repositioning and laparotomy or laparoscopy, may be considered. Myomectomy may be required if AUR results from a uterus incarcerated due to fibroid masses[7]. Close follow-up is important, especially for incarceration induced by endometriosis or severe adhesions, to avoid uterine sacculation.
Following a minimally invasive or invasive procedure, it is essential to keep the uterus in an anterior position and maintain a normal vesicourethral angle. Case 1 was advised to sleep in the prone position after manual reduction and adopt the knee-chest prone position twice a day until 20 wk of gestation. Occasionally, a soft pessary can be used[21,22]. Slama et al[23] used pessaries to alleviate successfully symptoms in 3 cases of urinary retention caused by uterine incarceration[23]. Yohannes et al[24] indicated that pessaries should not be used for impacted uterus as they are uncomfortable and cumbersome and restrict blood flow to the uterus[24]. Antibiotics should be considered where necessary.
In summary, AUR is a rare emergency occurring in the first and second trimester of pregnancy that requires prompt recognition and diagnosis[25]. Based on our clinical experience and current published literature, we propose the diagnostic and therapeutic algorithm shown in Figure 2. All patients should be treated individually.
The authors acknowledge Zhang L and Yue C, from the Department of Ultrasound, Hospital of Chengdu University of Traditional Chinese Medicine, for their support in imaging pictures.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sakly A S-Editor: Fan JR L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Choong S, Emberton M. Acute urinary retention. BJU Int. 2000;85:186-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Chen JS, Chen SC, Lu CL, Yang HY, Wang P, Huang LC, Liu FS. Acute Urinary Retention During Pregnancy--A Nationwide Population-Based Cohort Study in Taiwan. Medicine (Baltimore). 2016;95:e3265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kubota Y, Kojima Y, Kohri K. Maternal anterior sacral meningocele presenting as acute urinary retention in pregnancy. Int J Urol. 2012;19:279-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Goldberg KA, Kwart AM. Intermittent urinary retention in first trimester of pregnancy. Urology. 1981;17:270-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Smalbraak I, Bleker OP, Schutte MF, Treffers PE. Incarceration of the retroverted gravid uterus: a report of four cases. Eur J Obstet Gynecol Reprod Biol. 1991;39:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Kim HS, Park JE, Kim SY, Kim JE, Chae SH, Sohn IS, Hwang HS, Kwon HS. Incarceration of early gravid uterus with adenomyosis and myoma: report of two patients managed with uterine reduction. Obstet Gynecol Sci. 2018;61:621-625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 7. | Chauleur C, Vulliez L, Seffert P. Acute urine retention in early pregnancy resulting from fibroid incarceration: proposition for management. Fertil Steril 2008; 90: 1198.e7-1198. 10;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Heazell AE, Dwarakanath LS, Sundar K. An unusual cause of urinary retention in early pregnancy. Am J Obstet Gynecol. 2004;191:364-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Shnaekel KL, Wendel MP, Rabie NZ, Magann EF. Incarceration of the Gravid Uterus. Obstet Gynecol Surv. 2016;71:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Weekes AR, Atlay RD, Brown VA, Jordan EC, Murray SM. The retroverted gravid uterus and its effect on the outcome of pregnancy. Br Med J. 1976;1:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Jacobsson B, Wide-Swensson D. Incarceration of the retroverted gravid uterus--a review. Acta Obstet Gynecol Scand. 1999;78:665-668. [PubMed] |
| 12. | Danis RB, Brannon RK, Pereira N. Acute urinary retention due to a nonincarcerated retroverted gravid uterus. Int Urogynecol J. 2015;26:453-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Yang JM, Huang WC. Sonographic findings in acute urinary retention secondary to retroverted gravid uterus: pathophysiology and preventive measures. Ultrasound Obstet Gynecol. 2004;23:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | O'Connell MP, Ivory CM, Hunter RW. Incarcerated retroverted uterus--a non recurring complication of pregnancy. J Obstet Gynaecol. 1999;19:84-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Newell SD, Crofts JF, Grant SR. The incarcerated gravid uterus: complications and lessons learned. Obstet Gynecol. 2014;123:423-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Hsu PC, Yu MH, Wang CY, Wang YK, Wang CK, Su HY. Asymptomatic uterine incarceration at term: Successful management of a rare complication in pregnancy. Taiwan J Obstet Gynecol. 2018;57:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Hamod H, Chamberlain PF, Moore NR, Mackenzie IZ. Conservative treatment of an incarcerated gravid uterus. BJOG. 2002;109:1074-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Charova J, Yunus D, Sarkar PK. Incarcerated retroverted gravid uterus presenting as placenta praevia. J Obstet Gynaecol. 2008;28:537-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Dierickx I, Delens F, Backaert T, Pauwels W, Gyselaers W. Case report: incarceration of the gravid uterus: a radiologic and obstetric challenge. J Radiol Case Rep. 2014;8:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Patterson E, Herd AM. Incarceration of the uterus in pregnancy. Am J Emerg Med. 1997;15:49-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Dierickx I, Van Holsbeke C, Mesens T, Gevers A, Meylaerts L, Voets W, Beckers E, Gyselaers W. Colonoscopy-assisted reposition of the incarcerated uterus in mid-pregnancy: a report of four cases and a literature review. Eur J Obstet Gynecol Reprod Biol. 2011;158:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Martínez-Varea A, Nohales-Alfonso F, Diago Almela VJ, Perales-Marín A. Arabin cerclage pessary as a treatment of an acute urinary retention in a pregnant woman with uterine prolapse. Case Rep Obstet Gynecol. 2013;2013:161376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Slama R, Barry M, McManus K, Latham D, Berniard M. Uterine Incarceration: Rare Cause of Urinary Retention in Healthy Pregnant Patients. West J Emerg Med. 2015;16:790-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Yohannes P, Schaefer J. Urinary retention during the second trimester of pregnancy: a rare cause. Urology. 2002;59:946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Inaba F, Kawatu T, Masaoka K, Fukasawa I, Watanabe H, Inaba N. Incarceration of the retroverted gravid uterus: the key to successful treatment. Arch Gynecol Obstet. 2005;273:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Nelson MS. Acute urinary retention secondary to an incarcerated gravid uterus. Am J Emerg Med. 1986;4:231-232. [PubMed] |
| 27. | Lam K, Suen CF. Stranded under the Prom: impacted gravid uterus presenting as acute urinary retention. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Suzuki S, Ono S, Satomi M. Recurrence of urinary retention secondary to retroverted gravid uterus. N Am J Med Sci. 2009;1:54-57. [PubMed] |