Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3120
Peer-review started: November 24, 2020
First decision: January 24, 2021
Revised: February 4, 2021
Accepted: March 3, 2021
Article in press: March 3, 2021
Published online: May 6, 2021
Processing time: 143 Days and 9.1 Hours
We report a case of Intracardiac, pulmonary, and intravenous cement embolism after cement-augmented pedicle screw instrumentation in treating spondylolisthesis underlying osteoporotic bone, which was successfully managed by conservative treatment. We describe the treatment and outcome of the patient, hoping to shed light on the management of bone cement embolism.
A 67-year-old female suffered from progressive low back pain and numbness in lower extremities for 30 years. She was diagnosed with L4 and L5 spon
Intracardiac, pulmonary cement embolism after cement-augmented pedicle screw instrumentation is extremely rare. Careful clinical and radiographic evaluation is required in multiple sites of bone cement embolism. Conservative treatment may be a primary consideration in scattered emboli without life-threatening conditions, but a clinical decision should be made on an individualized basis.
Core Tip: Intracardiac and pulmonary cement embolism event after cement-augmented pedicle screw instrumentation is an extremely rare complication in orthopedics surgery. In our case, the patient developed no symptoms except for rapid decrease in oxygen saturation to 70%. The case presents evidence for treating cement embolism cases without severe life-threatening complications, which include close monitoring, oxygen inhalation, anti-coagulation, and antibiotic therapy. This case improves our understanding of bone cement embolism and informs optimization of the duration and type of anticoagulant drugs to be used when the complication occurs.
- Citation: Liang TZ, Zhu HP, Gao B, Peng Y, Gao WJ. Intracardiac, pulmonary cement embolism in a 67-year-old female after cement-augmented pedicle screw instrumentation: A case report and review of literature. World J Clin Cases 2021; 9(13): 3120-3129
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3120.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3120
Currently, pedicle screw instrumentation is a common and necessary approach in spinal surgery. With a surge in the aging population, degenerative lumbar disease and osteoporosis have become increasingly common. When dealing with osteoporotic patients, the strength of internal fixation is reduced, thus leading to increased intraoperative bleeding and higher postoperative revision rate and failure rate. A study performed by Wang et al[1] showed that osteoporosis is a risk factor for longer instrumented posterior spinal fusion. Longer instrumented extending to the adjacent segment may lead to several complications such as proximal junctional kyphosis that undermine the effectiveness of surgery[1,2]. To enhance the anchoring strength, several techniques have been used, including bicortical screws, tricortical screws, expandable screws, iliac screws, and iliosacral screws[3,4]. While it is not recommended to extend the extra fixation segment, the strength of bicortical or tricortical screws are also limited and may lead to internal fixation failure in an osteoporotic patients[5].
Cement-augmented pedicle screw instrumentation (CAPSI), first reported in the 1970s, has been widely applied in spinal surgeries for osteoporotic patients[6]. Generally, the indications for CAPSI include osteoporotic spine and revision surgeries[7,8]. Bone cement augmentation has complications of leakage into the intraspinal space and venous system and may lead to neurological deficits, pulmonary cement embolism (PCE), or intracardiac cement embolism (ICE)[9,10]. Compared to vertebroplasty, only a few studies focused on embolism events caused by CAPSI[11]. PCE and ICE caused by cement leakage into the venous system after CAPSI have been rarely reported. However, the incidence of cement embolism is increasing, and the treatment of severe multiple organ embolism remains controversial. It is estimated that the risk of all cement leakage was around 21.8%, while the incidence for symptomatic pulmonary embolism was between 0.2%-1.4%[12]. In this article, a case of conservative treatment for intracardiac and pulmonary cement embolism after CAPSI and a 30-mo uneventful outcome status is reported.
Low back pain for 30 years, worsening with numbness of both lower limbs for 3 mo.
A 67-year-old woman initially presented with the symptoms of chronic low back pain for 30 years. The patient received pain relief treatment, but she was not examined systematically because of poor compliance. The pain was then exacerbated and was accompanied by numbness in the lateral thigh of both sides for 3 mo. Therefore, the patient came to our hospital for a comprehensive examination.
The patient was diagnosed with hypertension for 10 years. The highest blood pressure level was around 150/90 mmHg. The patient did not have dizziness, vertigo, or blurred vision. She began to take metoprolol 47.5 mg once a day and yielded a good control of blood pressure level. The patient had no record of vascular diseases or embolism.
Her family members had no records of thrombotic disease.
A physical examination revealed a step sign on the L5 and S1 spinous process with tenderness on the paraspinal muscles of L4-S1. The Laseque sign was negative for both limbs of the patient. Sciatica was not induced by bilateral femoral nerve stretching test of both lower limbs. No obvious scoliosis and kyphosis were observed in the patient.
Prothrombin and partial thromboplastin times were normal, and D-dimers were slightly increased at 632 ng/mL. The blood analysis showed a hemoglobin level of 133 g/L, a platelet count of 247 ×109/L, and a white count of 5.77 × 109/L, which were all within the normal range. Three days after the surgery when the drop of oxygen saturation occurred, blood analysis revealed a leukocytosis 14.27 × 109/L, with predominant neutrophils (91.6%) with decreased hemoglobin at 96 g/L and normal platelet count. D-dimers were significantly increased at 7669 ng/mL (referenced range: 68-494 ng/mL). Creatine kinase was increased slightly at 219 U/L (referenced range < 190 U/L). Arterial blood gas revealed an elevated pH 7.479 and reduced oxygen partial pressure at 58.6 mmHg. The blood biochemistries, electrocardiogram, and urine analysis were normal.
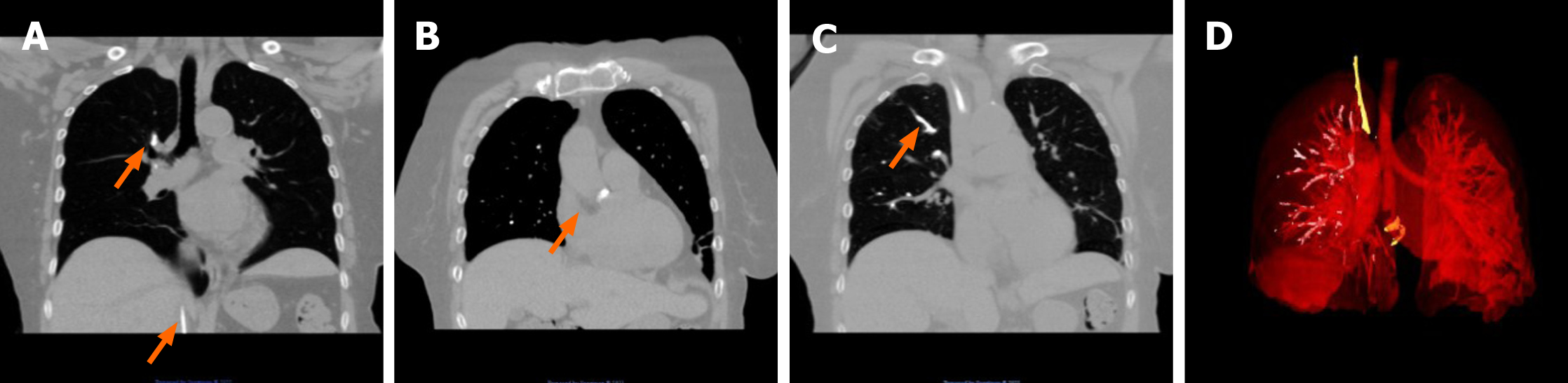
The T-value measured by dual-energy X-ray absorptiometry was -3.21 SD, which indicated osteoporosis of the lumbar spine. The average Hounsfield unit value of the L4 vertebrae was 98.82, while the average Hounsfield unit value of the L5 vertebrae was 98.77 (Supplementary Figure 1). A preoperative radiograph and computed tomography (CT) scan showed L4 and L5 isthmic spondylolisthesis. The magnetic resonance imaging scan indicated anterior L4 spondylolisthesis complicated with spinal canal stenosis of the L4-S1 segment. Bilateral nerve root was compressed significantly. After surgery, chest CT was performed to evaluate the severity of embolism. Multiple columnar high-density shadows in pulmonary arteries of multiple segments of right pulmonary arteries, anteromedial basal segment, and basal lateral segment of left lower lobe and azygos vein were observed.
The patient was anesthetized and placed in a prone position. Under fluoroscopic guidance, 6.5 mm fenestrated pedicle screws were inserted in L4 and L5, and regular pedicle screws were inserted in S1. For cement augmentation, 2 mL of high-viscosity polymethyl methacrylate bone cement was injected into each pedicle screw gently 4 min after mixture without application of high-pressure injection system. An L4 and L5 Laminectomy and decompression were performed, and the nerve roots were released. A standard posterior lumbar interbody fusion was performed of the L4/5 and L5/S1 segments.
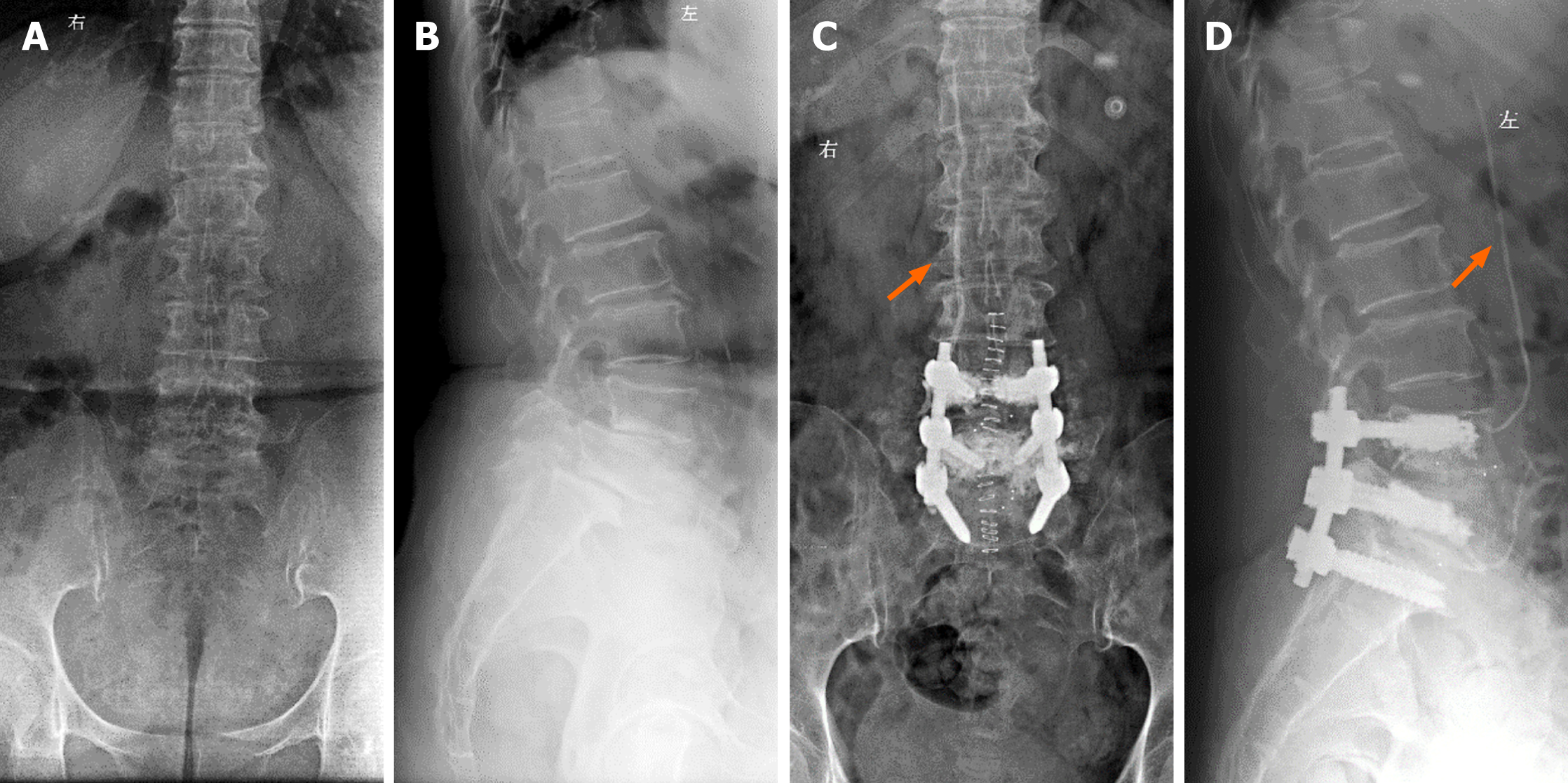
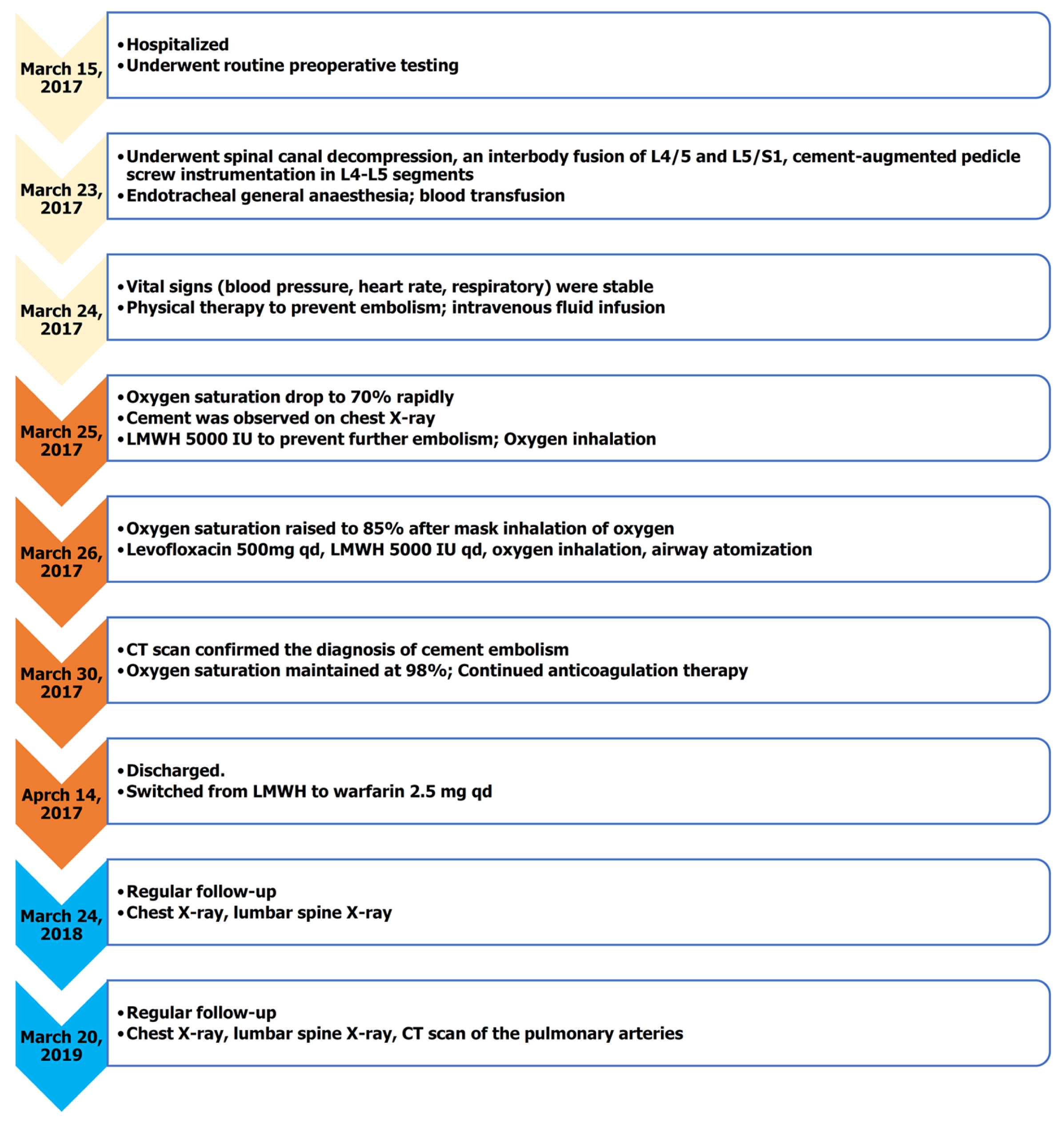
The patient’s condition was stable after surgery. The low back pain and numbness in the lower extremities were relieved immediately. Her oxygen saturation maintained at 99%. However, on the third day after surgery, the patient presented with a sudden decrease in oxygen saturation to 70%. X-ray of lumbar vertebrae showed leakage of cement from the venous system (Figure 1). The patient did not have cough, hemoptysis, or shortness of breath, and there were no signs of chest pain or palpitation. The oxygen saturation raised to 85% after low-flow oxygen inhalation. A blood gas analysis revealed a pH = 7.479, partial pressure of carbon dioxide = 41.0 mmHg, and oxygen partial pressure = 58.6 mmHg. Blood D-dimer was raised from 631 ng/mL 1 d preoperative to 7669 ng/mL 3 d postoperative. Spirometry revealed small airway dysfunction without diffusion impairment. The pulmonary function test showed that the diffusion function was normal, but small airway dysfunction existed. Chest CT confirmed the presence of multiple columnar high-density shadows in the pulmonary arteries of multiple segments of right pulmonary arteries, anteromedial basal segment, and basal lateral segment of left lower lobe and azygos vein (Figure 2). The bone cement embolism was located within the right and left lower lobe of the lung. The CT scan also revealed exudation and inflammation of both lungs. The electrocardiograph was normal, and the molecular markers of myocardial infarction including creatine kinase (219 U/L), lactate dehydrogenase (293 U/L), and myoglobin (78.4 ug/L) were slightly elevated. The Pulmonary Embolism Severity Index and simple Pulmonary Embolism Severity Index score for the patient were 20 and 1, respectively. Because the patient exhibited no significant hemodynamic disorder or signs of cardiac failure, she was treated with continuous low-flow oxygen inhalation and 5000 IU/d low molecular weight heparin. Blood oxygen was restored in 2 h. The patient developed the symptoms of fever and her white blood cell count elevated to 12.4 × 109/L. Meanwhile, plain radiography indicated diffuse exudation in the lungs.
The final diagnosis of the presented case is intracardiac, pulmonary, and venous bone cement embolism after cement-augmented pedicle screw instrumentation.
To treat plausible infection, 500 mg/d of levofloxacin was used. After the commencement of cement embolism, the patient was nursed sitting up regularly and was atomized to clear airway secretions twice daily. The patient developed no further embolism, and blood oxygen was maintained above 98%. Therefore, the patient was discharged 3 wk after surgery. The patient was treated with low molecular weight heparin 5000 IU/d for 1 mo and was switched to 2.5 mg/d of warfarin for 6 mo after discharge. The coagulation function was closely monitored by international normalized ratio during warfarin administration.
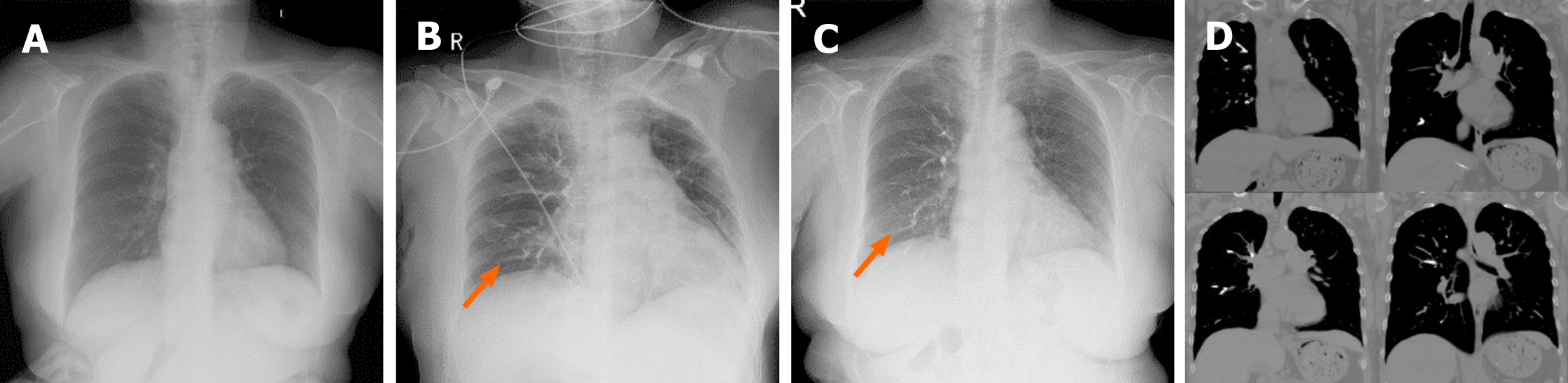
Regular tests and serial cardiac and pulmonary assessments were carried out and revealed no signs of an exacerbation. She did not report further discomfort in the 30-mo follow-up (Figure 3).
In the case we presented, the patient was diagnosed with L4-L5 isthmic spo
Bone cement leakage is a common complication of a bone cement-augmented pedicle screw. Two major complications underlying CAPSI are PCE and perivertebral cement leakage (PCL). It is estimated that the risk of PCE in an augmented pedicle screw insertion is approximately 1.5%-7.9%[14]. Janssen et al[11] reported the risk of cardiac cement embolism following percutaneous vertebroplasty was approximately 3.9%. Approximately 71% of patients with underlying CAPSI may develop cement leakage, but most of them were asymptomatic. In a study conducted by Ulusoy et al[15], the distribution of intravenous leakage locations in PCL-positive cases was 10.8% in both the azygos vein and inferior vena cava. In PCE-positive patients, emboli in segmentary and subsegmental arteries were detected in 52% of patients, while 48% had emboli detected in the lobar and main pulmonary arteries[15]. In this case, the intracardiac, pulmonary, and vein cement embolism were all developed following CAPSI procedure.
Very few studies have focused on the risk factors of an embolism following CAPSI. Known risk factors for PCE include thoracic spine instrumentation, spinal metastases, more instrumented levels, and more total cement volume[16]. Risk factors of symptomatic PCE include more than 10 instrumented levels, previous card
Most cardiopulmonary cement embolisms are asymptomatic, but in some cases, cement embolisms can lead to severe clinical outcomes[18,19]. More devastating clinical outcomes may occur when PCL enters the lumbar venous plexus, azygos vein, inferior vena cava, the right heart, and eventually the pulmonary arteries[20-26]. Symptoms such as dyspnea, oxygen desaturation, tachypnea, or cardiopulmonary arrest seem to begin a few days or immediately after surgery (Figure 4 and Table 1). Life-threatening conditions including acute respiratory distress, pericardial effusion, and fatal cardiac perforation may occur[15,27,28]. Most PCE and ICE patients develop symptoms during hospitalization[29], but in some cases, it may take more than 5 years before the symptoms emerge[30].
| Date | Oxygen saturation | Platelets, 109/L | WBC, 109/L | Hemoglobin, g/L | D-dimer, ng/mL | Clinical intervention |
| March 13, 2017 | 99% | 172 | 6.75 | 121 | 631 | Admission |
| March 23, 2017 | 99% | - | - | - | - | Lumbar surgery |
| March 24, 2017 | 99% | 158 | 14.27 | 96 | 7698.90 | Vital signs monitering |
| March 25, 2017 | 70% | 113 | 12.4 | 84 | Pulmonary expert consultation | |
| March 26, 2017 | 85% | 121 | 8.90 | 85 | 5667 | Levofloxacin 500 mg qd+ LMWH 5000 IU qd |
| April 1, 2017 | 98% | - | - | - | - | Levofloxacin 500 mg qd+ LMWH 5000 IU qd |
| April 14, 2017 | 98% | - | - | - | 4638 | Discharged |
Many studies have reported removing the central embolism caused by large emboli through surgery. Open surgery may be considered when the patient develops life threating conditions such as progressive dyspnea, chest pain, hemodynamic disruption, cardiac perforation, or tamponade[31]. After careful evaluation of the location and the shape of the cement emboli, percutaneous retrieval is an approach that is considered to extract the embolus. There is a viable algorithm and indication of reverting to surgery in treating symptomatic central bone cement embolization. After careful evaluation of clinical presentation, cement size and location, and vital signs, the decision of interventional radiology or either open/minimal invasive cardiac surgery can be made[9]. Sometimes, the embolus may be difficult to extract, and forced removal may cause extra damage. In this case, the symptomatic cardiopulmonary embolism was treated using conservative treatments under close monitoring. It is not practical to remove all the sparse and fragile emboli through catheter-based retrieval. Therefore, in the case of mild clinical manifestation with stable hemodynamic status, conservative treatment including anticoagulation, continuous low-flow oxygen inhalation, and antibiotics can be an option. Some preventive measures have been used to avoid embolic complications of CAPSI (Table 2).
| Ref. | Sex | Age | Vertebrae augmented | Time of embolism detected Post-op | Clinical presentation | Treatment | Outcome |
| Rasch et al[20], 2010 | M | 55 | L3/4 | 2 d | Tachycardia, dyspnea and oxygen desaturation | Pulmonary arteriotomy and cement removement | Discharged without severe complication |
| Tang et al[21], 2020 | F | 73 | L3-L5 | 6 d | Dyspnea, blood oxygen desaturation | Oxygen inhalation and anticoagulation treatment | Uneventful recovery in 2 yr follow-up |
| Akinola et al[22], 2010 | M | 76 | L3-L5 | Immediate | No symptoms | Anticoagulation treatment for 6 mo | Uneventful recovery in 6 mo follow-up |
| Zheng et al[23], 2013 | F | 47 | T1-T4, T9 | 1 h | Dyspnea, low blood pressure, unconsciousness | NA | Death |
| Rahimizadeh et al[24], 2020 | F | NA (middle aged) | L3 | 1 d | Cardiopulmonary arrest | Resuscitation, anticoagulation treatment | Uneventful recovery in 12 mo follow-up |
| Röllinghoff et al[25], 2010 | F | 69 | T8-L1 | NA | No symptoms | NA | Uneventful recovery in 18 mo follow-up |
| Tonolini et al[26], 2012 | F | 75 | L1/L3 | Immediate | Dyspnea with tachypnea and bilateral hypoventilation | Anticoagulation treatment | Discharged without severe complication |
Baroud et al[32] suggested the use of high-viscosity bone cement and longer mixing time, while lower injection pressure and intermittent injections have also been recommended[33]. Close monitoring under consecutive fluoroscopy can detect early leakages.
Spine surgeons should pay more attention to the occurrence of cement embolism when treating an osteoporotic or metastatic spine tumor through CAPSI. In this case, the patient developed intracardiac, pulmonary, and intravenous embolism without significant clinical symptoms. The leakage may be caused by the injection of bone cement into paravertebral veins. The patient was treated with continuous low-flow oxygen inhalation, anticoagulation, and antibiotics, and the prognosis was acceptable in a 30-mo follow-up. When making clinical decisions, conservative treatment may be considered in patients without significant symptoms and when the embolus is small. Despite the rare complications, CAPSI is generally a reliable and safe surgical procedure. Nevertheless, more studies are needed to establish a decision-making algorithm regarding CAPSI related embolism events.
The authors would like to thank the patient for their involvement in the present study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saha S, Wood AM S-Editor: Zhang L L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Wang H, Ma L, Yang D, Wang T, Yang S, Wang Y, Wang Q, Zhang F, Ding W. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine (Baltimore). 2016;95:e4443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Hyun SJ, Kim YJ, Rhim SC. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016;16:1095-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 114] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 3. | Zhuang XM, Yu BS, Zheng ZM, Zhang JF, Lu WW. Effect of the degree of osteoporosis on the biomechanical anchoring strength of the sacral pedicle screws: an in vitro comparison between unaugmented bicortical screws and polymethylmethacrylate augmented unicortical screws. Spine (Phila Pa 1976). 2010;35:E925-E931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Weng F, Wang J, Yang L, Zeng J, Chu Y, Tian Z. Application value of expansive pedicle screw in the lumbar short-segment fixation and fusion for osteoporosis patients. Exp Ther Med. 2018;16:665-670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Guo HZ, Tang YC, Li YX, Yuan K, Guo DQ, Mo GY, Luo PJ, Zhou TP, Zhang SC, Liang. The Effect and Safety of Polymethylmethacrylate-Augmented Sacral Pedicle Screws Applied in Osteoporotic Spine with Lumbosacral Degenerative Disease: A 2-Year Follow-up of 25 Patients. World Neurosurg. 2019;121:e404-e410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, Spencer CW. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;99-112. [PubMed] |
| 7. | Hoppe S, Keel MJ. Pedicle screw augmentation in osteoporotic spine: indications, limitations and technical aspects. Eur J Trauma Emerg Surg. 2017;43:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Liu D, Sheng J, Wu HH, Kang X, Xie QY, Luo Y, Zhou JJ, Zheng W. Biomechanical study of injectable hollow pedicle screws for PMMA augmentation in severely osteoporotic lumbar vertebrae: effect of PMMA distribution and volume on screw stability. J Neurosurg Spine. 2018;29:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Sidhu GS, Kepler CK, Savage KE, Eachus B, Albert TJ, Vaccaro AR. Neurological deficit due to cement extravasation following a vertebral augmentation procedure. J Neurosurg Spine. 2013;19:61-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | D'Errico S, Niballi S, Bonuccelli D. Fatal cardiac perforation and pulmonary embolism of leaked cement after percutaneous vertebroplasty. J Forensic Leg Med. 2019;63:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Janssen I, Ryang YM, Gempt J, Bette S, Gerhardt J, Kirschke JS, Meyer B. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017;17:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 12. | Zhang J, Wang G, Zhang N. A Meta-Analysis Of Complications Associated With The Use Of Cement-Augmented Pedicle Screws In Osteoporosis Of Spine. Orthop Traumatol Surg Res. 2020;102791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC. Laminectomy plus Fusion vs Laminectomy Alone for Lumbar Spondylolisthesis. N Engl J Med. 2016;374:1424-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 461] [Cited by in RCA: 583] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 14. | Singh V, Mahajan R, Das K, Chhabra HS, Rustagi T. Surgical Trend Analysis for Use of Cement Augmented Pedicle Screws in Osteoporosis of Spine: A Systematic Review (2000-2017). Global Spine J. 2019;9:783-795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Ulusoy OL, Kahraman S, Karalok I, Kaya E, Enercan M, Sever C, Abay B, Karadereler S, Hamzaoglu A. Pulmonary cement embolism following cement-augmented fenestrated pedicle screw fixation in adult spinal deformity patients with severe osteoporosis (analysis of 2978 fenestrated screws). Eur Spine J. 2018;27:2348-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Hsieh MK, Kao FC, Chiu PY, Chen LH, Yu CW, Niu CC, Lai PL, Tsai TT. Risk factors of neurological deficit and pulmonary cement embolism after percutaneous vertebroplasty. J Orthop Surg Res. 2019;14:406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Corcos G, Dbjay J, Mastier C, Leon S, Auperin A, De Baere T, Deschamps F. Cement leakage in percutaneous vertebroplasty for spinal metastases: a retrospective evaluation of incidence and risk factors. Spine (Phila Pa 1976). 2014;39:E332-E338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Chang CY, Huang SF. Asymptomatic pulmonary cement embolism. CMAJ. 2017;189:E543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Pannirselvam V, Hee HT. Asymptomatic cement embolism in the right atrium after vertebroplasty using high-viscosity cement: a case report. J Orthop Surg (Hong Kong). 2014;22:244-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Rasch A, Sindermann J, Scheld HH, Hoffmeier A. Pulmonary Palacos embolism: a case report. Thorac Cardiovasc Surg. 2010;58:437-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Tang YC, Guo HZ, Guo DQ, Luo PJ, Li YX, Mo GY, Ma YH, Peng JC, Liang, Zhang SC. Effect and potential risks of using multilevel cement-augmented pedicle screw fixation in osteoporotic spine with lumbar degenerative disease. BMC Musculoskelet Disord. 2020;21:274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Akinola B, Lutchman L, Barker P, Rai A. Pulmonary cement embolism during cement augmentation of pedicle screw fixation: a case report. J Orthop Surg (Hong Kong). 2010;18:364-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Zheng N, Liang M, Zhang HD, Zhu SH, Yang TT, Zhuo L, Wang GF, Liu HX, Liu L. Fatal extensive bone cement embolism: histological findings confirmed by Fourier transform infrared spectroscopy. Forensic Sci Int. 2013;229:e23-e25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Rahimizadeh A, Hassani V, Soufiani H, Rahimizadeh A, Karimi M, Asgari N. Symptomatic pulmonary cement embolism after pedicle screw polymethylmethacrylate cement augmentation: A case report and review. Surg Neurol Int. 2020;11:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Röllinghoff M, Siewe J, Eysel P, Delank KS. Pulmonary cement embolism after augmentation of pedicle screws with bone cement. Acta Orthop Belg. 2010;76:269-273. [PubMed] |
| 26. | Tonolini M, Bianco R. Pulmonary cement embolism after pedicle screw vertebral stabilization. J Emerg Trauma Shock. 2012;5:272-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Andrä M, Baumer H, Mittergradnegger F, Laschitz M, Petek T, Wandschneider W. Life-Threatening Cardiac Perforation After Posterior Spondylodesis. Ann Thorac Surg. 2017;104:e355-e357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Gosev I, Nascimben L, Huang PH, Mauri L, Steigner M, Mizuguchi A, Shah AM, Aranki SF. Right ventricular perforation and pulmonary embolism with polymethylmethacrylate cement after percutaneous kyphoplasty. Circulation. 2013;127:1251-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Kim SY, Seo JB, Do KH, Lee JS, Song KS, Lim TH. Cardiac perforation caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJR Am J Roentgenol. 2005;185:1245-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Lim KJ, Yoon SZ, Jeon YS, Bahk JH, Kim CS, Lee JH, Ha JW. An intraatrial thrombus and pulmonary thromboembolism as a late complication of percutaneous vertebroplasty. Anesth Analg. 2007;104:924-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Tran I, Gerckens U, Remig J, Zintl G, Textor J. First report of a life-threatening cardiac complication after percutaneous balloon kyphoplasty. Spine (Phila Pa 1976). 2013;38:E316-E318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Baroud G, Crookshank M, Bohner M. High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine (Phila Pa 1976). 2006;31:2562-2568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 150] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 33. | Krueger A, Bliemel C, Zettl R, Ruchholtz S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009;18:1257-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 220] [Article Influence: 13.8] [Reference Citation Analysis (0)] |