Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3063
Peer-review started: October 19, 2020
First decision: January 17, 2021
Revised: January 27, 2021
Accepted: March 19, 2021
Article in press: March 19, 2021
Published online: May 6, 2021
Processing time: 185 Days and 3.4 Hours
Intracortical chondroma of the metacarpal bone which could be painful is an extremely rare condition and previously only one case has been reported. Due to the similar physical features and appearance on clinical imaging, it is difficult to differentiate between intracortical chondroma and osteoid osteoma. Therefore, pathological examination is usually required to establish a definite diagnosis, which is often carried out only after tumor removal. In this study, we describe a case of intracortical chondroma which developed in the metacarpal bone and demonstrate the utility of magnetic resonance imaging (MRI).
We present a case of a 40-year-old man with intracortical chondroma of the metacarpal bone who was strongly suspected of having a tumor, and it was confirmed using contrast-enhanced MRI and successfully treated with curettage. MRI performed before tumor removal revealed signal intensity similar to that of the nidus of an osteoid osteoma. However, no abnormal intensity was observed in the bone or soft tissues surrounding the tumor. Such abnormalities on images would indicate the presence of soft-tissue inflammation, which are characteristics of osteoid osteoma. Furthermore, contrast-enhanced imaging revealed no increased enhancement of the areas surrounding the tumor. This is the first report to describe the contrast-enhanced MRI features of intracortical chondroma. This may serve as a guide for clinicians when intracortical chondroma is suspected.
The contrast-enhanced MRI was useful for the differential diagnosis of intracortical chondroma.
Core Tip: In the present report, we described a case of intracortical chondroma with pain which developed in the metacarpal bone. Our findings highlight the utility of magnetic resonance imaging for the differential diagnosis of intracortical chondroma. To the best of our knowledge, this is the first report to describe the contrast-enhanced magnetic resonance imaging features of intracortical chondroma. This may serve as a guide for clinicians when intracortical chondroma is suspected.
- Citation: Yoshida Y, Anazawa U, Watanabe I, Hotta H, Aoyama R, Suzuki S, Nagura T. Intracortical chondroma of the metacarpal bone: A case report. World J Clin Cases 2021; 9(13): 3063-3069
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3063.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3063
Chondroma is a type of benign bone tumor composed of hyaline cartilage. Chondroma arising in the bone cortex is called intracortical chondroma, which is an extremely rare condition. This disorder demonstrates lucent lesion with surrounding sclerosis and is usually painful[1-8]. The radiographical and clinical features of intracortical chondroma resemble those of cortical osteoid osteoma. Osteoid osteoma is usually painful and represents approximately 5% of all primary bone tumors[6]. The painful and intracortical lucent lesions of intracortical chondroma appear almost identical to the nidus of osteoid osteoma in both clinical and imaging examinations, making the two conditions hard to differentiate[3,5]. To the best of our knowledge, there have been no case reports detailing the features of magnetic resonance imaging (MRI) studies, including contrast-enhanced imaging, in the context of intracortical chondroma. In the present report, we describe a case of intracortical chondroma which developed in the metacarpal bone and demonstrate the utility of MRI. As we present important information related to the differential diagnosis of intracortical chondroma, our findings highlight the situations in which intracortical chondroma should be considered and may serve as a guide for clinical assessment in such cases.
An otherwise healthy 40-year-old man presented with the primary complaint of pain in the left hand that persisted for 2 mo. The pain started intermittently without any injury and was most severe at night. He visited a local clinic, where he underwent plain radiography which revealed a tumor in the second metacarpal bone, and the patient was referred to our hospital.
He visited a local clinic, where he underwent plain radiography which revealed a tumor in the second metacarpal bone, and the patient was referred to our hospital.
He had no significant medical history.
He was healthy without a personal or family history of tumors.
Physical examination revealed stiffness and tenderness over the dorsum of the second metacarpal bone.
Measurements of routine laboratory examinations, including routine blood tests, routine urine tests, and blood biochemistry, were within normal levels. Blood biochemistry results demonstrated no obvious abnormalities.
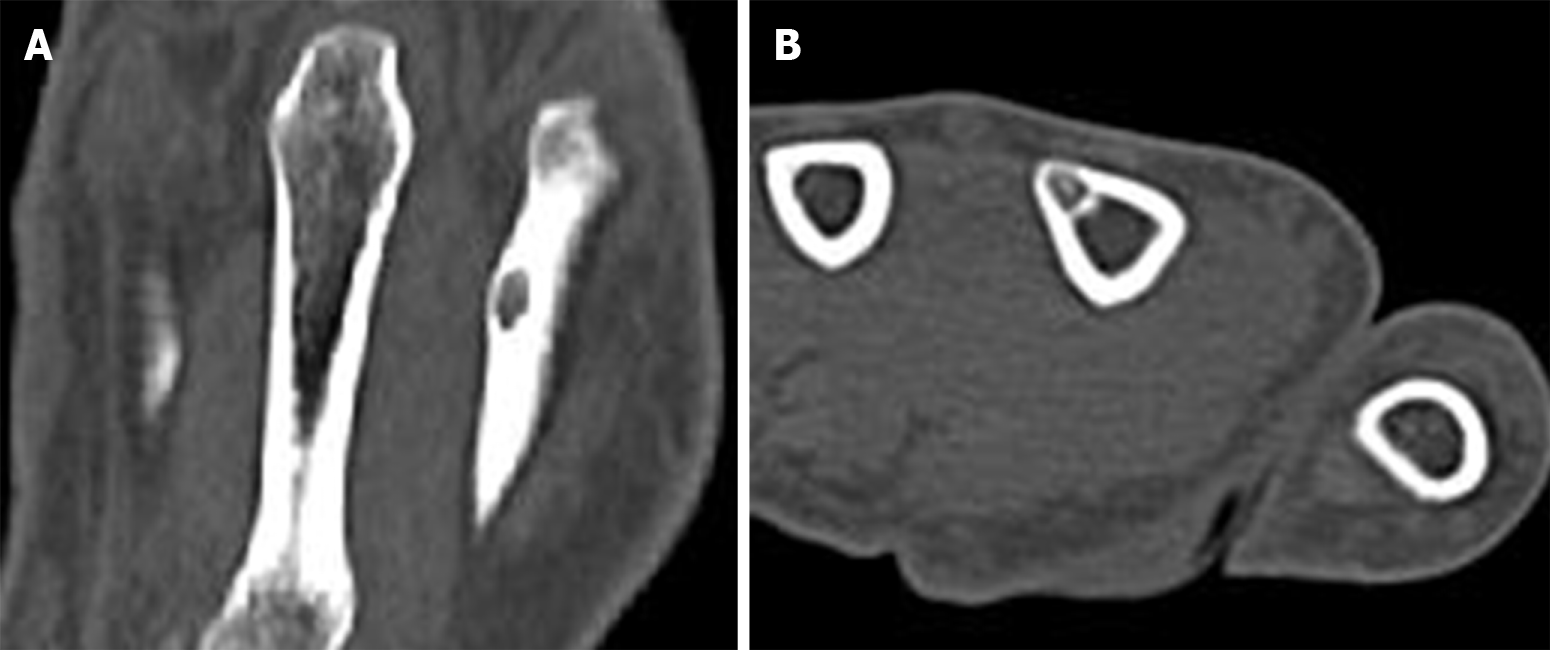
Plain radiography results revealed cortical expansion and well-demarcated lucency in the shaft of the second metacarpal bone (Figure 1). Plain computed tomography (CT) results revealed a 4 mm lucency with surrounding sclerosis and central calcification in the cortical bone on the ulnar side of the second metacarpal bone (Figure 2). No pathological fractures were observed.
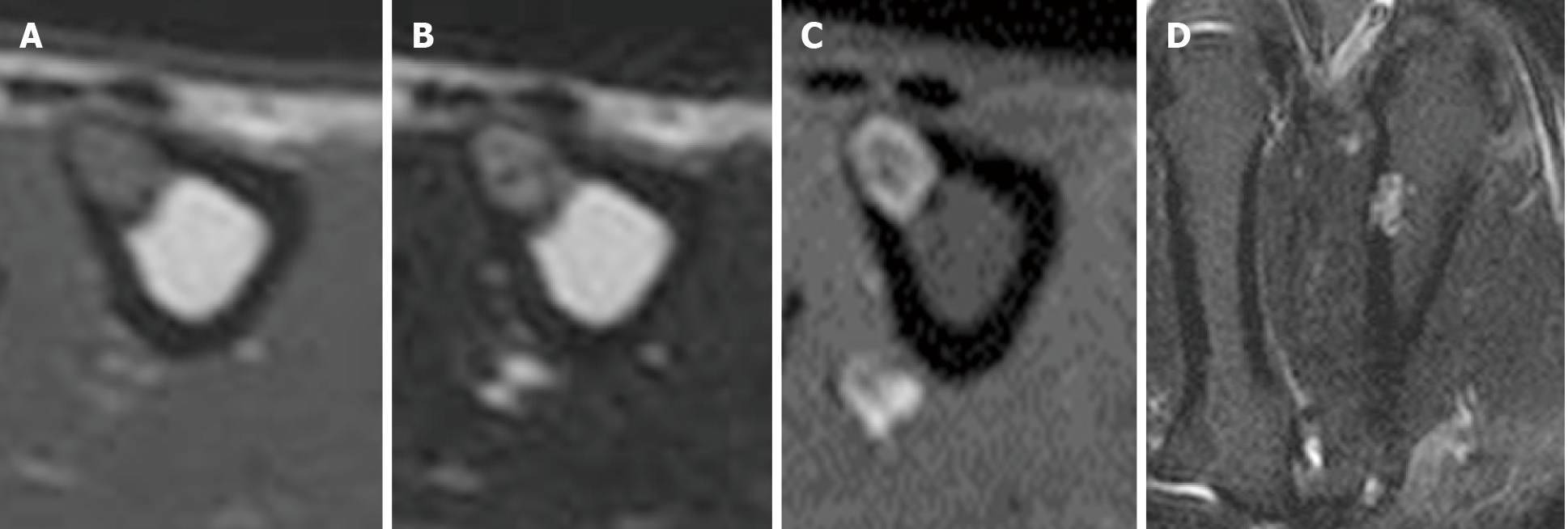
The tumor exhibited a distinct margin on MRI (Figure 3) with low signal intensity on T1-weighted images and high signal intensity on T2-weighted and short tau inversion recovery images. Axial contrast-enhanced images revealed only the tumor margin to be enhanced. No abnormal intensity was detected in the bone marrow or soft tissues around the lesion.
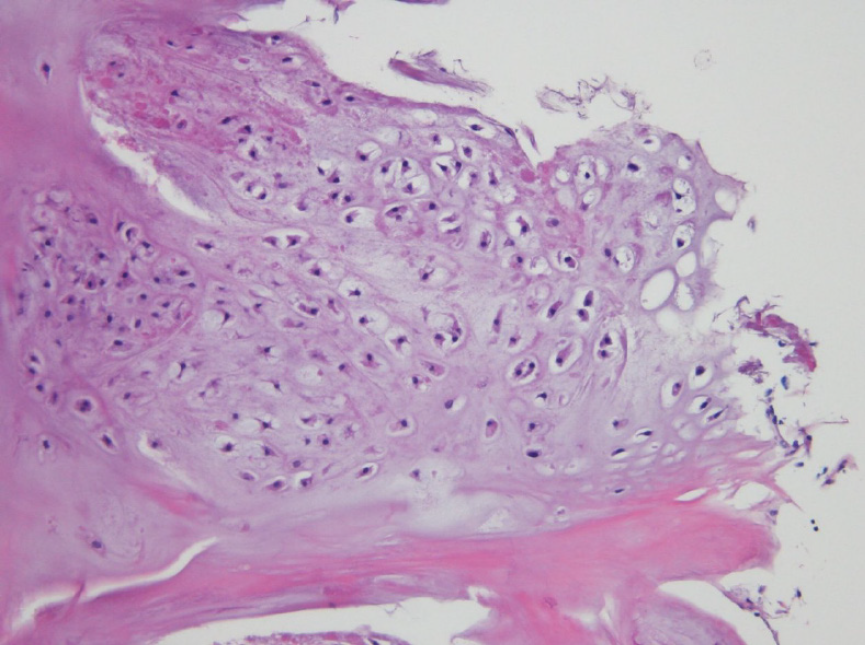
Results of the histopathological analysis revealed multinucleated chondrocytes with minimal atypia, which is consistent with the characteristics of chondroma. The site of tumor development was within the cortical bone; hence, the condition was determined to be intracortical chondroma (Figure 4). The final diagnosis of the presented case is intracortical chondroma of the metacarpal bone.
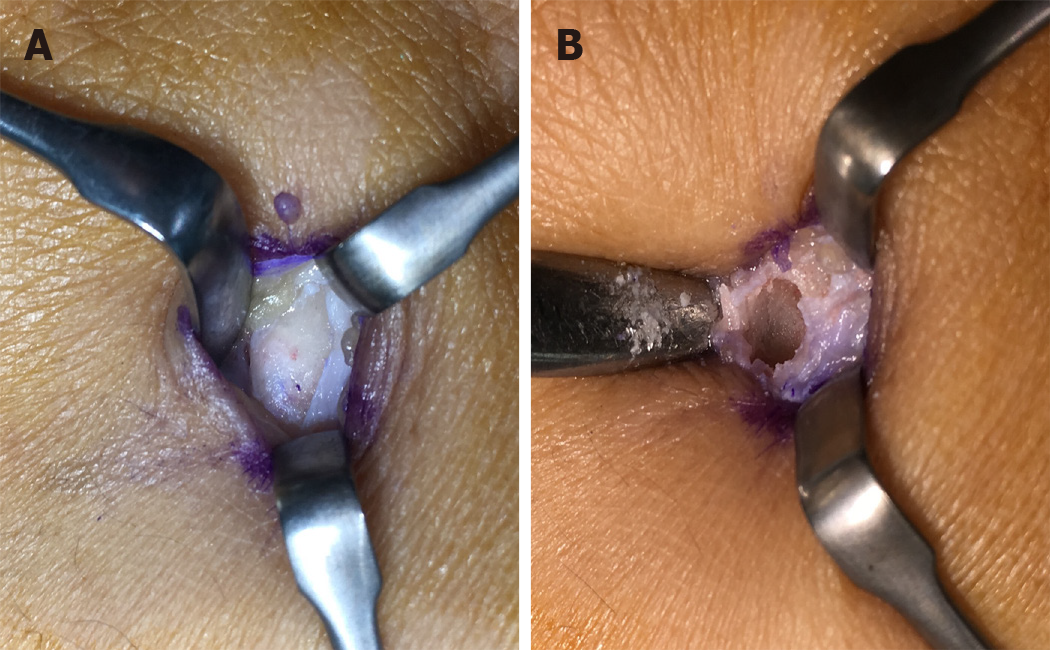
We suspect benign intracortical lesions according to these MRI features. Administration of non-steroidal anti-inflammatory drugs (NSAIDs) did not completely control the local pain; therefore, curettage of the lesion was performed (Figure 5).
The pain subsided following curettage, and in the 1 year since surgery, the patient has experienced a favorable course with no recurrence (Figure 6).
When a patient presents with a solitary painful tumor of the cortical bone, the possibility of chondrosarcoma, chondroma, and osteoid osteoma must be considered. In the present case report, radiographic findings did not reveal endosteal scalloping or destruction of the cortical bone suggesting chondrosarcoma. Conversely, MRI demonstrated well-demarcated lucency without reactive signal change around the lesion, meaning that osteoid osteoma could be ruled out as the reactive signal change is a typical feature of osteoid osteoma.
Chondroma is classified according to the location as enchondroma (arising in the medullary cavity), periosteal chondroma (arising in the periosteum), or intracortical chondroma (arising in the bone cortex), with most cases of chondroma being categorized as enchondroma. Periosteal and intracortical chondromas commonly develop in the long bones of relatively young patients and are accompanied by pain.
Intracortical chondroma was first reported by Abdelwahab et al[1] in 1990. To the best of our knowledge, only 10 cases of intracortical chondroma have been reported in the literature[1-8] (Table 1). The average age of onset was 20 years (range, 5-45 years), and the sites of tumor development were over the shaft to the shaft ends in the tibia of four patients, femur of three, humerus of two, and metacarpal bone of only one patient.
| Ref. | Age (yr) | Sex | Symptoms of pain | Analgesic effect of NSAIDs | Location | Tumor size (mm) | Radiology findings | Treatment | Recurrence | ||
| Lucency with surrounding sclerosis | Cortical thickening | Calcification | |||||||||
| Abdelwahab et al[1] | 22 | Male | + | NR | Femur | 20 | + | − | − | En bloc excision | − |
| Horikiri et al[2] | 21 | Male | + | NR | Metacarpal | 12 | + | − | − | En bloc excision and iliac bone graft | − |
| Ramnath et al[3] | 5 | Female | + | + | Tibia | 5 | + | + | − | CT-guided biopsy followed by radiofrequency ablation. After recurrence, en bloc excision | + 6 mo after radiofrequency ablation |
| Ramnath et al[3] | 7 | Male | + | + | Femur | 3 | + | − | − | CT-guided biopsy followed by radiofrequency ablation | − |
| Lui et al[4] | 7 | Male | + | NR | Tibia | 10 | + | + | − | En bloc excision | − |
| Jones et al[5] | 31 | Female | + | NR | Humerus | 8 | + | + | − | Excisional biopsy | − |
| Jones et al[5] | 41 | Male | − | NR | Femur | 10 | + | - | − | Excisional biopsy | − |
| Choi et al[6] | 12 | Male | + | − | Tibia | 5 | + | + | − | Excisional biopsy | − |
| Chou et al[7] | 7 | Female | + | NR | Humerus | 8 | + | − | − | Excisional biopsy | − |
| Rudman et al[8] | 45 | Female | − | NR | Tibia | 10 | + | − | + | En bloc excision | − |
| Present case | 40 | Male | + | − | Metacarpal | 4 | + | − | + | Curettage | − |
Removal of the tumor resulted in good outcomes with no recurrence for all but one patient in these previous studies. This one patient had undergone CT-guided tumor resection.
When the present case is included, pain symptoms were present in 9 of the 11 published cases. Pain relief was only achieved through the administration of NSAIDs in two cases. Osteoid osteoma is characterized by the efficacy of NSAIDs for pain relief and conservative treatment could be chosen[9]; therefore, this factor may be helpful for clinically distinguishing intracortical chondroma from osteoid osteoma. However, not all patients improve, and pain relief is achieved in 70% of osteoid osteoma patients[10] and both intracortical chondroma and osteoid osteoma are generally treated by complete resection with curettage.
In all cases, plain radiography and CT imaging revealed a lucency with surrounding sclerosis. Four cases showed the expansion of the cortical bone with cortical thickening around the tumor, which is often observed in the osteoid osteoma[3-6]. The present case as well as the one previous case showed central calcification-like osteoid osteoma[8]. These findings of clinical presentation and plain radiography and CT imaging highlight the importance of distinguishing intracortical chondroma from osteoid osteoma. Previous studies have supported the difficulty of this owing to the similar clinical and imaging findings, and it has been suggested that pathological examination is required to make a definitive diagnosis[1].
On MRI scans, osteoid osteoma is identified by an abnormal intensity of the tumor and reactive signal change around, the tumor and enhancement of intensity is a characteristic feature of osteoid osteoma owing to the presence of soft-tissue swelling and inflammation[10,11]. There is only one report in the literature on intracortical chordoma that included MRI findings. They reported the MRI fast-spin-echo sequence (TR3616, TE 28) coronal images of intracortical chondroma, revealing high signal intensity and circular lesions[5].
In the present report, we demonstrated a thin peripheral enhancement of the tumor, which some enchondromas might show[10], and the lack of signal change around the tumor on T1- or T2-weighted or enhanced images. Since imaging findings of intracortical chondroma and osteoid osteoma are similar, these findings demonstrate the notable differences and support the utility of MRI for differential diagnosis (Table 2). To the best of our knowledge, there have been no studies on intracortical chondroma demonstrating the features of signal intensity of both the tumor and the surrounding area by contrast-enhanced MRI; further studies are required into this analysis. Although clinical analyses and radiographic and CT imaging features appear to indicate osteoid osteoma in the bone cortex, on MRI, no signal change in the area surrounding the tumor would suggest intracortical chondroma.
| Symptoms of pain | Analgesic effect of NSAIDs | Radiology findings | Contrast-enhanced magnetic resonance imaging | |||
| Lucency with surrounding sclerosis | Cortica; thickening | Calcification | ||||
| Intracortical chordoma | + | (-)-(+) | + | (-)-(+) | (-)-(+) | Only the tumor margin is enhanced |
| Osteoid osteoma | + | + | + | + | + | Signal intensity of both the tumor and the surrounding area |
MRI was useful for the differential diagnosis of intracortical chondroma. To the best of our knowledge, this is the first report to describe the contrast-enhanced MRI features of intracortical enchondroma. This may serve as a guide for clinicians when intracortical chondroma is suspected.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen Z, Liu PC, Xiao EH S-Editor: Zhang L L-Editor: A P-Editor: Ma YJ
| 1. | Abdelwahab IF, Hermann G, Lewis MM, Klein MJ. Case report 588: Intracortical chondroma of the left femur. Skeletal Radiol. 1990;19:59-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Horikiri K, Asato H, Oshiro W, Kanaya F. A rare case of intracortical chondroma of metacarpal. Orthop Traumatol. 2001;50:210-214. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Ramnath RR, Rosenthal DI, Cates J, Gebhardt M, Quinn RH. Intracortical chondroma simulating osteoid osteoma treated by radiofrequency. Skeletal Radiol. 2002;31:597-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Lui PC, Lau PP, Fan YS, Choi ST, Mak KH, Tam KF, Tse GM. Intracortical chondroma in a 7-year-old boy and literature review. Pathology. 2006;38:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Jones KB, Buckwalter JA, Frassica FJ, McCarthy EF. Intracortical chondroma: a report of two cases. Skeletal Radiol. 2006;35:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Choi E, Wert M, Guerrieri C, Tucci J. A pathologic fracture of an intracortical chondroma masking as an osteoid osteoma. Orthopedics. 2010;33:845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Chou YH, Hsieh MS, Huang CC, Wu K, Wu CT. Intracortical chondroma of the humerus in a child. Pathology. 2013;45:624-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Rudman DP, Damron TA, Vermont A, Mathur S. Intracortical chondroma. Skeletal Radiol. 1998;27:581-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Goto T, Shinoda Y, Okuma T, Ogura K, Tsuda Y, Yamakawa K, Hozumi T. Administration of nonsteroidal anti-inflammatory drugs accelerates spontaneous healing of osteoid osteoma. Arch Orthop Trauma Surg. 2011;131:619-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Meyers SP. MRI of Bone and Soft Tissue Tumors and Tumorlike Lesions. Differential Diagnosis and Atlas. Rodiology. 2009;250: e16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | von Kalle T, Langendörfer M, Fernandez FF, Winkler P. Combined dynamic contrast-enhancement and serial 3D-subtraction analysis in magnetic resonance imaging of osteoid osteomas. Eur Radiol. 2009;19:2508-2517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |