Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2555
Peer-review started: November 17, 2020
First decision: January 7, 2021
Revised: January 19, 2021
Accepted: February 10, 2021
Article in press: February 10, 2021
Published online: April 16, 2021
Processing time: 124 Days and 10.6 Hours
Multiple myeloma is a malignant hematological disease characterized by proliferation of monoclonal plasma cells mainly in the bone marrow. Extraosseous epidural plasmacytoma associated with myeloma arises from lymphoid tissue in the epidural space without focal vertebral involvement, and is rare.
A 52-year-old woman was diagnosed with kappa subtype nonsecretory multiple myeloma and presented with bilateral arm weakness 11 mo after completing multiple courses of chemotherapy. Spinal magnetic resonance imaging (MRI) showed a posterior C7–T3 epidural mass with spinal cord compression. After five courses of chemotherapy, follow-up MRI showed resolution of cord compression. A 54-year-old man presented with paraplegia 15 mo after a diagnosis of IgD kappa subtype multiple myeloma and completing multiple courses of chemotherapy. He underwent Th11 and L1 laminectomies for tumor resection because MRI showed an epidural mass causing cord compression. His-topathologic examination was consistent with IgD multiple myeloma. The patients have currently survived for 33 mo and 19 mo, respectively.
Isolated extraosseous epidural plasmacytoma associated with multiple myeloma without bony involvement is difficult to diagnose by imaging. Definitive diagnosis requires pathological and immunohistochemical examination.
Core Tip: Extraosseous epidural plasmacytoma associated with multiple myeloma is believed to arise from lymphoid tissue in the epidural space. Patients with these lesions can present with normal or diffuse vertebral bone marrow patterns on magnetic resonance imaging. Chemotherapy and laminectomy should be considered for treatment.
- Citation: Cui JF, Sun LL, Liu H, Gao CP. Extraosseous spinal epidural plasmocytoma associated with multiple myeloma: Two case reports. World J Clin Cases 2021; 9(11): 2555-2561
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2555.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2555
Multiple myeloma is a hematogenous disorder characterized by the proliferation of small monoclonal plasma cells. Symptoms develop because of anemia, immunosuppression, renal failure, hypercalcemia, osteolytic bone lesions, and pathologic fractures. Despite therapeutic advances, the 5-year survival rate remains just under 50%[1]. On magnetic resonance imaging (MRI), myeloma involves the bone marrow in either a focal pattern characterized by nodular marrow lesions, or a diffuse pattern characterized by widespread homogeneous alteration of marrow signal intensity. Although myeloma typically breaks through the cortex to extend into the surrounding tissue, epidural extraosseous plasmacytoma with intact adjacent bone is uncommon.
We present two patients with multiple myeloma, who developed epidural plasmocytoma causing spinal cord compression. To the best of our knowledge, these patients represent the 7th and 8th reported cases of spinal epidural extraosseous plasmacytoma associated with myeloma. We also review the current literature.
Case 1: A 52-year-old woman presented with mild bilateral arm weakness.
Case 2: A 53-year-old man was admitted to the hospital because of progressively worsening intractable thoracolumbar spine pain that limited his activities and rendered him unable to lie flat. Associated symptoms included bilateral lower extremity numbness and dysuria.
Case 1: Eleven months earlier, the patient was diagnosed with kappa subtype nonsecretory multiple myeloma and treated with seven courses of vincristine, adriamycin, and dexamethasone, and one course of vincristine, adriamycin, cyclophosphamide, and dexamethasone. MRI at the time of initial diagnosis showed diffuse osteolytic lesions in the thoracic and lumbar vertebrae.
Case 2: Fifteen months earlier, the patient was diagnosed with IgD kappa type multiple myeloma and treated with chemotherapy, including four courses of bortezomib, doxorubicin, and dexamethasone, and eight courses of vincristine, doxorubicin, and dexamethasone. Computed tomography (CT) at the time of initial diagnosis showed multiple osteolytic lesions involving the vertebral bodies, sternum, and bilateral ribs.
Case 1: The patient exhibited neurologic deficits in both upper extremities.
Case 2: Neurologic examination showed sensory loss below the level of L1, complete paraplegia in both lower extremities, and absence of patellar reflexes bilaterally.
Case 1: At the time of myeloma diagnosis, laboratory data showed normocytic normochromic anemia. Blood urea nitrogen was 34 mg/dL, calcium was 13.5 mg/dL, total protein was 6.8 g/dL, and albumin was 3.6 g/dL. A peripheral blood smear showed no evidence of rouleaux. β2-microglobulin was elevated at 4500 μg/L (normal range, 600-2000 μg/L). Immunofixation of the serum and urine using monoclonal antisera against IgG, IgA, IgM, and λ was also negative. No monoclonal gammopathy was found in the serum or urine. Bone marrow biopsy showed marked plasmacytosis, with 45%-60% infiltration and osteoclastic invasion of the bone. Immunoperoxidase staining of the bone marrow aspirate was positive for intracytoplasmic light chain, consistent with nonsecretory multiple myeloma.
Case 2: Laboratory studies at the time of the myeloma diagnosis showed an elevation in the erythrocyte sedimentation rate to 92 mm/h, a C-reactive protein level of 5.12 mg/L, and normochromic normocytic aplastic anemia (hemoglobin, 104 g/L), with normal leukocyte and platelet counts. Bence-Jones protein was not detected. Bone marrow aspirated from the sternum showed 32% malignant plasma cells; presence of IgD and λ chains in the tumor cells was confirmed by immunohistochemistry.
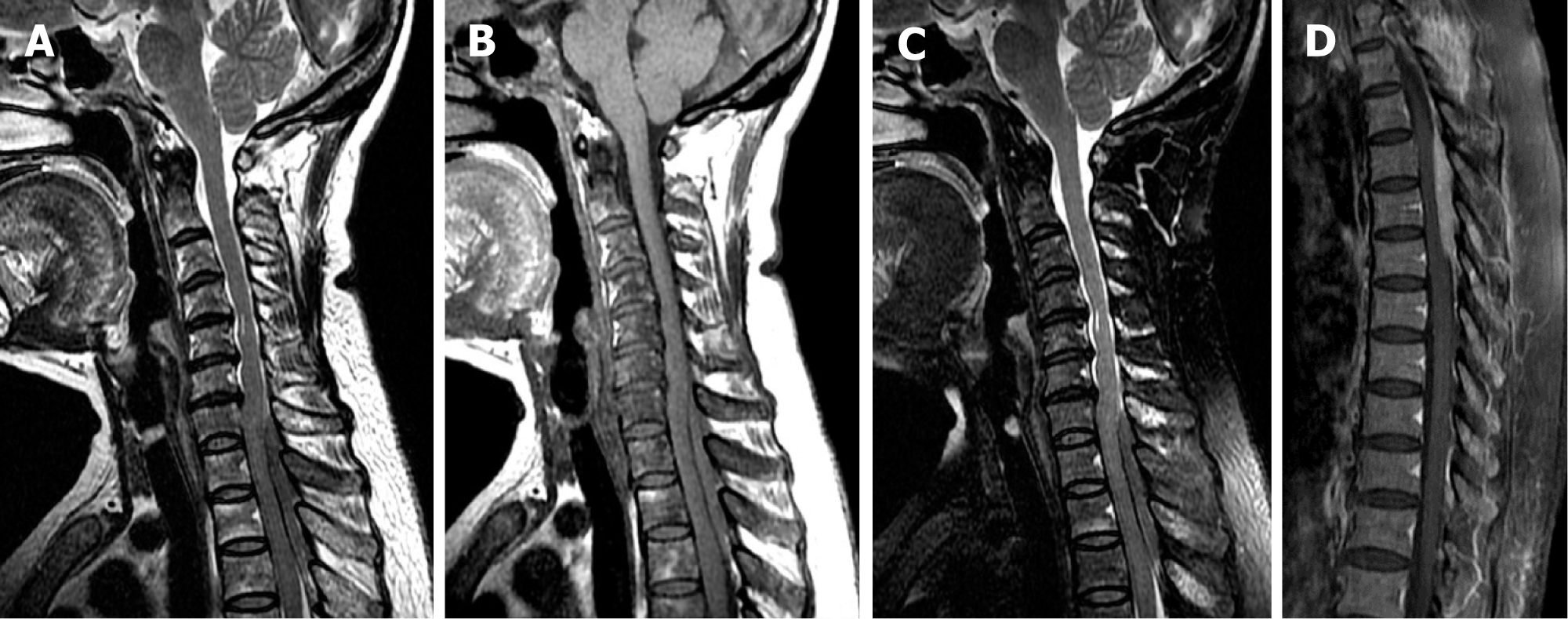
Case 1: The patient underwent spinal MRI to evaluate her arm weakness, which showed a posterior epidural mass extending from C7 to T3, measuring 61 mm × 5 mm in the sagittal plane. The mass compressed the spinal cord and appeared isointense on both T1-weighted imaging (T1WI) and T2-weighted imaging (T2WI). On contrasted T1WI, the mass showed moderate and homogenous enhancement (Figure 1).
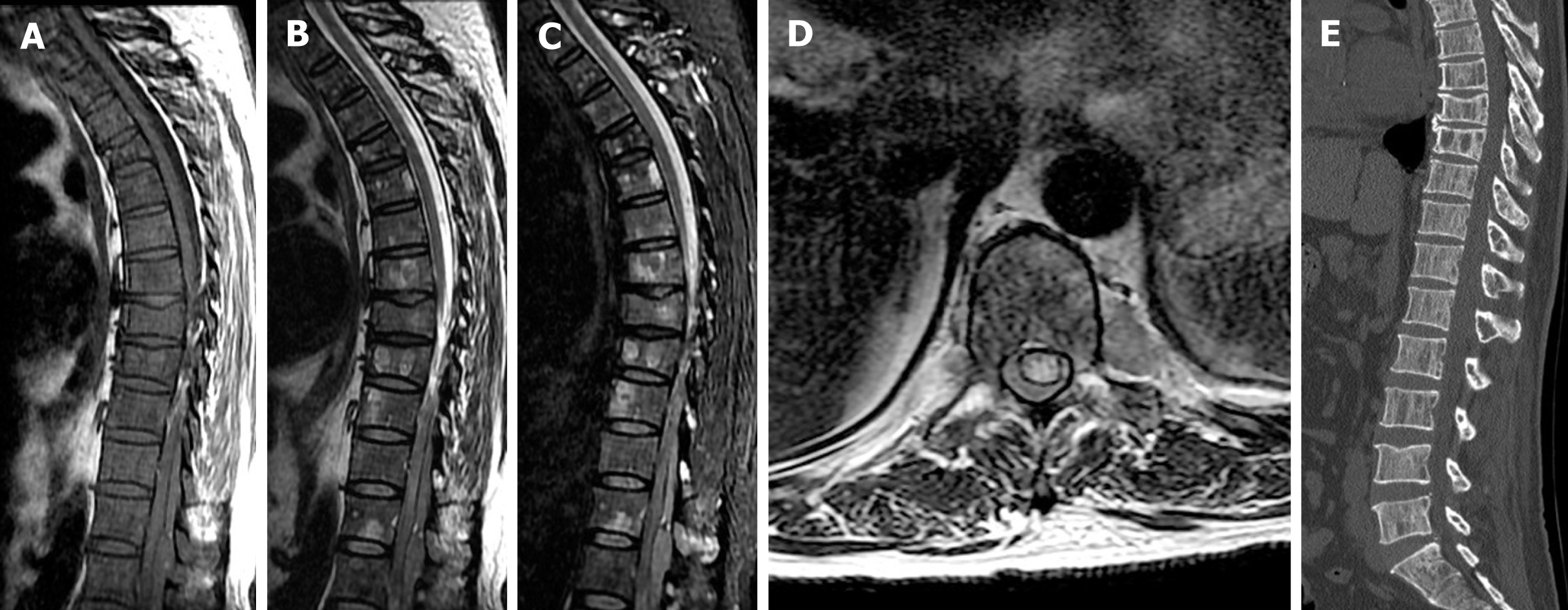
Case 2: Spinal MRI showed a posterior epidural mass extending from the Th11 to L1 Levels. The mass was isointense to the paravertebral muscles on T1WI and T2WI. On CT with sagittal reconstructions, the vertebral cortical margins were clearly defined and no communication was noted between the epidural mass and posterior vertebral elements. Multiple osteolytic lesions of the vertebrae appeared as multiple patchy areas of high signal intensity on T2WI and low density on CT (Figure 2). Vertebral body collapse without spinal canal narrowing was noted at Th8 and Th9.
Cases 1 and 2: The patients were diagnosed with extraosseous spinal epidural plasmacytoma associated with multiple myeloma.
Case 1: As there was no indication for surgical resection, five courses of chemotherapy with vincristine, adriamycin, and dexamethasone were administered.
Case 2: Decompressive laminectomies were performed from Th11 to L1 and the soft tissue mass coating the dura was easily and completely removed.
Case 1: Follow-up MRI showed a marked reduction of the epidural mass and resolution of spinal cord compression (Figure 3). The patient’s neurologic deficits significantly improved and she is currently alive 42 mo after diagnosis.
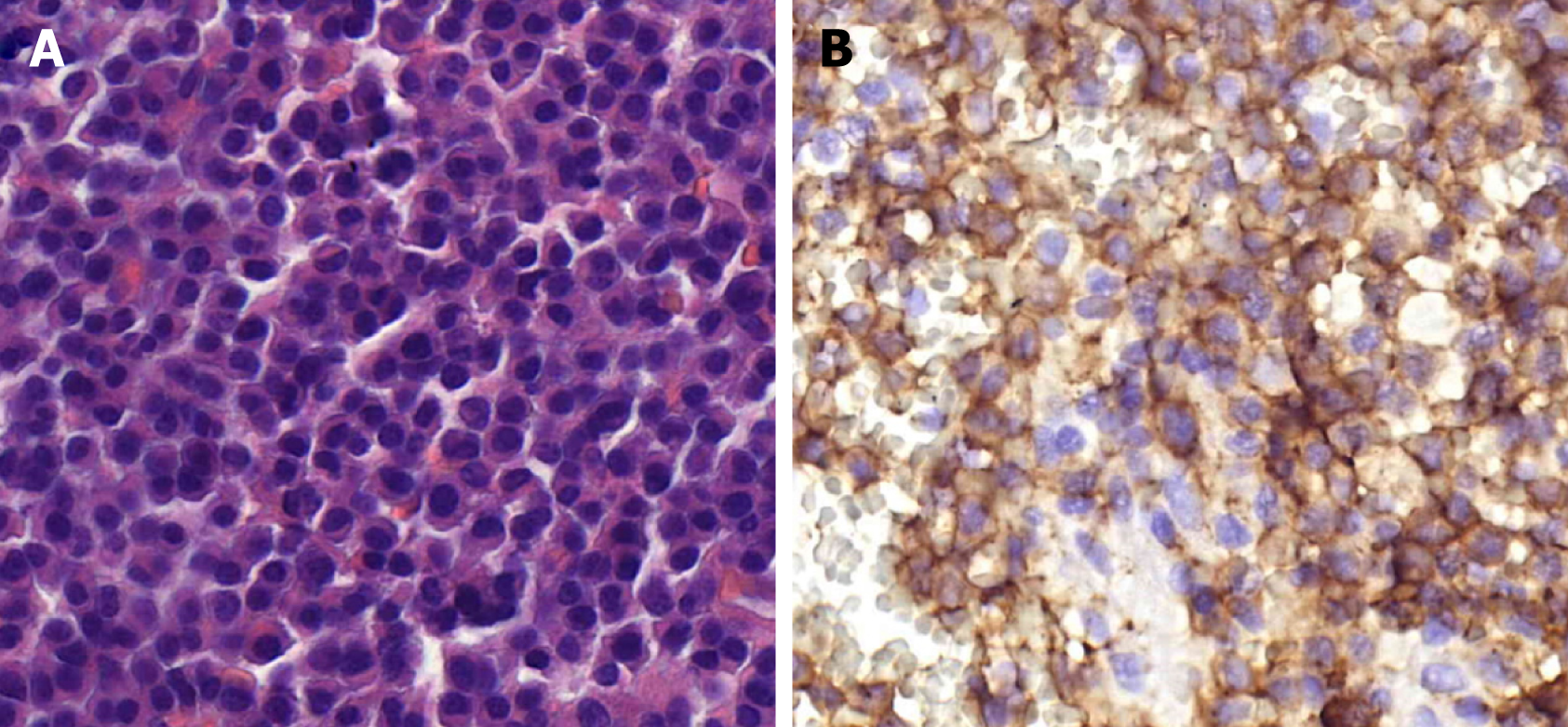
Case 2: Immunohistochemical studies of the soft tissue mass were consistent with kappa subtype myeloma (Figure 4). The patient is currently alive 19 mo after diagnosis.
Multiple myeloma is a cancer of clonal plasma cells characterized by infiltration of the bone marrow that causes anemia, painful lytic bone disease, and hypercalcemia and kidney damage due to accumulation of monoclonal immunoglobulins[2]. The disease involves the bone marrow, can break through the cortex, and most commonly occurs in the spine. Myeloma may exhibit several patterns in the bone marrow of the spine on MRI[3]. The focal pattern is characterized by nodular marrow lesions against a background of normal-appearing marrow, while the diffuse pattern is characterized by widespread homogeneously altered marrow signal intensity. However, the bone marrow may also appear completely normal[2].
Extraosseous multiple myeloma is uncommon, comprising < 5% of all plasma cell neoplasms, and it has a particular predilection for the mucosa of the upper respiratory and gastrointestinal tracts[4]. Extraosseous epidural plasmacytoma associated with myeloma is believed to arise from lymphoid tissue in the epidural space[5]. Extension of paraspinal lymph nodes through vertebral foramina is another possibility[6]. Regardless, MRI is the best radiologic modality to detect epidural masses in affected patients.
Extraosseous epidural plasmacytoma associated with myeloma was first described by Matsui et al[7] in 1992. Since then, a total of eight cases have been reported, including the two presented here (Table 1). These cases comprise four men and four women, with ages ranging from 40 to 85 years. The masses were located over the entire length of the spine, from the cervical vertebrae to the sacrum. In the patient reported by Matsui et al[7], the mass was located at L3 at the time of initial diagnosis and relapsed after 15 mo, extending epidurally from C7 to T4. Seven patients had epidural masses spanning multiple segments and one patient had a mass confined to the L3 segment. The mass spanning the largest number of segments extended from C7 to L2/3[3]. Furthermore, extraosseous epidural masses restricted to the spinal canal or extending to the vertebral foramina and paravertebral muscles occurred in three patients.
| No. | Age in yr | Sex | subtype | Symptom and sign | Treatment | Neurological improvement/survival | Ref. |
| 1 | 52 | M | IgD/λ | Back and leg pain with paresthesia of legs1; Back pain with paraparesis2 | Chemotherapy; Laminectomy | Improved with complete remission; Died of respiratory dysfunction/19 mo | Matsui et al[7], 1992 |
| 2 | 40 | F | IgA/λ | Back pain with paraparesis; Progressive paraplegia | Plasmapheresis; Radiotherapy, chemotherapy | No improvement/7 mo | Palmbach et al[3], 1996 |
| 3 | 85 | M | IgD/λ | Paraplegia, anesthesia below T6 | Chemotherapy | No improvement/> 12 mo | Watanabe et al[11], 2000 |
| 4 | 45 | F | IgG/λ | Low back pain, right L5, S1; Radioculopathy | Surgical resection; Chemotherapy | No improvement/> 5 mo | Hu et al[12], 2001 |
| 5 | 47 | M | IgG/λ | Back pain, paraplegia sensory disturbance below T8 | Chemotherapy; Radiotherapy | No improvement/> 6 mo | Okacha et al[6], 2008 |
| 6 | 60 | F | IgG/λ | Paraplegia, sensory disturbance below T8 | Laminectomy, local radiotherapy, chemotherapy | Improved/> 6 mo | Avadhani et al[13], 2010 |
| 7 | 53 | F | NSM/k | Numbness of bilateral lower extremities | Chemotherapy | Improved/> 42 mo3 | Present case |
| 8 | 53 | M | IgD/λ | Paraplegia | Chemotherapy, laminectomy | Improved/> 19 mo3 | Present case |
MRI clearly demonstrates epidural masses, while CT can be used to define the cortex of adjacent vertebrae. The reported imaging findings of epidural plasmacytoma associated with myeloma, including our two cases, are presented in Table 2. On T1WI, four of nine masses appeared isointense and one appeared hypointense; T1WI findings of the remaining four masses were not reported. In contrast, four masses were hyperintense and three were isointense on T2WI; T2WI findings of the remaining two masses were not reported. Among the four patients who underwent contrasted MRI, three had masses that enhanced while one did not. Four of the eight patients exhibited isolated epidural plasmacytoma with normal spinal bone marrow, while the remaining four showed vertebral infiltration with multiple osteolytic lesions.
| No. | Location | IF and paravertebral extension | T1WI | T2WI | Enhancement | Vertebrae infiltration |
| 1 | L3 posterior C7-T4 posterior1 | No | N/A | Hyperintense | / | L2-L3 |
| Yes | N/A | Hyperintense | / | N/A | ||
| 2 | C7-L2/3 posterior | Yes | Isointense | Hyperintense | / | Diffuse |
| 3 | C7-T2 posterior | No | Isointense | Isointense | No | No |
| 4 | L5-S1 N/A | N/A | N/A | N/A | N/A | No |
| 5 | T4-T6 posterior | Yes | Hypointense | Hyperintense | Moderate | No |
| 6 | T6-T7 posterior | No | N/A | N/A | Yes | No |
| 7 | C7-T3 posterior | No | Isointense | Isointense | Moderate | Diffuse |
| 8 | T12-L1 posterior | No | Isointense | Isointense | / | Diffuse |
There are no current guidelines for management of extraosseous epidural plasmacytoma associated with myeloma. All eight reported patients were treated with chemotherapy, including our two, and four showed improvement. Three patients underwent laminectomy because of paraplegia, and one patient underwent surgical resection. Survival in the six previously reported patients ranged from 6 to 19 mo. Both of our patients are currently alive; the survival from myeloma diagnosis to last follow-up was 42 mo and 19 mo, respectively. Furthermore, the patient described in case 1 has remained in remission for over 3 years and has experienced a significant decrease in epidural mass size, indicating a good chemotherapy response.
Multiple myeloma should be differentiated from other epidural neoplasms such as lymphoma, solitary amyloidoma, and metastases. Spinal epidural lymphoma without evidence of systemic involvement is uncommon. On MRI, the epidural mass appears isointense on T1WI and T2WI and poorly enhances on contrasted imaging[8]. Solitary amyloidoma of the spine is also rare and manifests as an epidural tumor with bony involvement that typically appears hypointense on T1WI and T2WI and brightly enhances on contrasted imaging[9]. Epidural metastases are difficult to distinguish on the basis of MRI signal intensity and morphology and require histopathological confirmation for further management[10].
In conclusion, although the presence of an extraosseous epidural mass with diffuse vertebral bone marrow infiltration can establish the diagnosis of multiple myeloma, establishing the diagnosis of an isolated epidural mass with normal vertebral bone marrow on MRI is difficult. However, patient age and laboratory findings may provide clues. Despite the poor prognosis, chemotherapy is indicated for all myeloma patients, and laminectomy is indicated in patients with paraplegia resulting from epidural spinal cord compression.
Manuscript source: Unsolicited manuscript
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Secer HI S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Kosmala A, Bley T, Petritsch B. Imaging of Multiple Myeloma. Rofo. 2019;191:805-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Lecouvet FE, Vande Berg BC, Michaux L, Malghem J, Maldague BE, Jamart J, Ferrant A, Michaux JL. Stage III multiple myeloma: clinical and prognostic value of spinal bone marrow MR imaging. Radiology. 1998;209:653-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 112] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Palmbach M, Hoffmann W, Grodd W, Postler E, Voigt K. Extraosseous, epidural tumour spread of multiple myeloma. Eur J Radiol. 1996;22:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Damaj G, Mohty M, Vey N, Dincan E, Bouabdallah R, Faucher C, Stoppa AM, Gastaut JA. Features of extramedullary and extraosseous multiple myeloma: a report of 19 patients from a single center. Eur J Haematol. 2004;73:402-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | George ED, Sadovsky R. Multiple myeloma: recognition and management. Am Fam Physician. 1999;59:1885-1894. [PubMed] |
| 6. | Okacha N, Chrif E, Brahim E, Ali A, Abderrahman E, Gazzaz M, Adil B, Bouchaib K, Mohamed B. Extraosseous epidural multiple myeloma presenting with thoracic spine compression. Joint Bone Spine. 2008;75:70-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Matsui H, Fujie H, Tsuji H. Extraosseous epidural tumor of immunoglobulin D myeloma. J Spinal Disord. 1992;5:366-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dho YS, Kim H, Wang KC, Kim SK, Lee JY, Shin HY, Park KD, Kang HJ, Kim IH, Park SH, Phi JH. Pediatric Spinal Epidural Lymphoma Presenting with Compressive Myelopathy: A Distinct Pattern of Disease Presentation. World Neurosurg. 2018;114:e689-e697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Smitherman AD, Fung KM, Glenn CA, Martin MD. Intradural, extramedullary amyloidoma involving cervical and thoracic spine. J Clin Neurosci. 2015;22:1052-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Kim HJ, Ryu KN, Choi WS, Choi BK, Choi JM, Yoon Y. Spinal involvement of hematopoietic malignancies and metastasis: differentiation using MR imaging. Clin Imaging. 1999;23:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Watanabe Y, Endou A, Ooi S, Matsushima E, Shimisu Y, Nakashima K. Extraosseous epidural IgD myeloma presenting with compression myelopathy. Psychiatry Clin Neurosci. 2000;54:665-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Hu KC, Lin J, Chuang YC, Cheng SJ, Chang KM. Multiple myeloma associated with extramedullary plasmacytoma causing nerve root compression: a case report. J Formos Med Assoc. 2001;100:277-280. [PubMed] |
| 13. | Avadhani A, Shetty AP, Rajasekaran S. Isolated extraosseous epidural myeloma presenting with thoracic compressive myelopathy. Spine J. 2010;10:e7-e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |