Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2524
Peer-review started: September 4, 2020
First decision: December 21, 2020
Revised: January 4, 2021
Accepted: February 10, 2021
Article in press: February 10, 2021
Published online: April 16, 2021
Processing time: 206 Days and 5.2 Hours
Giant cell tumor (GCT) is a benign lesion and rarely involves the patella. This disease is characterized by a relatively high recurrence rate after primary treatment. En bloc resection has been a predominant option for recurrent GCT. However, total patellectomy can lead to disruption of the knee. Therefore, exploration of functional reconstruction of the extensor mechanism is worthwhile.
A 54-year-old woman presented with right knee pain and swelling, and was diagnosed as having a GCT in the patella following curettage and autograft. Medical imaging revealed a lytic and expanded lesion involving the whole patella with focal cortical breaches and pathological fracture. Based on the combination of histological, radiological, and clinical features, a diagnosis of recurrent GCT in the patella was made (Campanacci grade III). After a multidisciplinary team discussion, three-dimensional (3D)-printed custom-made patellar endoprosthesis was performed following en bloc resection for reconstructing the extensor mechanism. The patient was followed for 35 mo postoperatively. No evidence of local recurrence, pulmonary metastasis, or osteoarthritis of the right knee was observed. The active flexion arc was 0°-120°, and no extension lag was detected. A favorable patellar tracking and height (Insall-Salvati ratio 0.93) were detected by radiography.
We depict a case of a GCT at the right patella, which was successfully treated by patellectomy and 3D-printed custom-made endoprosthetic replacement. The patella normal reconstruction, the precise-fit articular design, and gastrocnemius flap augmentation could lead to satisfactory knee function and a low rate of complications in the short-term follow-up.
Core Tip: The history of allogenic patellectomy has been a predominant option for recurrent giant cell tumor of the patella for decades. Although many reconstructive methods were reported following patellectomy, much needs to be researched for better knee function and fewer complications. Our study is a pioneering case using three-dimensional-printed custom-made patella, which could be able to minimize complications and improve knee function. What’s more, a review of the previous relevant research and the potential future avenues of research related to the novel introduction of reconstructive methods following patellectomy cases was performed.
- Citation: Wang J, Zhou Y, Wang YT, Min L, Zhang YQ, Lu MX, Tang F, Luo Y, Zhang YH, Zhang XL, Tu CQ. Three-dimensional-printed custom-made patellar endoprosthesis for recurrent giant cell tumor of the patella: A case report and review of the literature. World J Clin Cases 2021; 9(11): 2524-2532
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2524.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2524
Giant cell tumor of bone (GCTB) is a benign lesion with local aggressive nature and a relatively high recurrence rate after primary treatment[1]. The majority of GCTBs are located in the epiphyseal regions of long bones, with the sacrum or spine being the second most common site, while rarely involving the patella[1-3]. Generally, intralesional curettage and cementation are suitable for patients with Campanacci grade I or II GCTBs[1]. As for Campanacci grade III or recurrent GCTBs, en bloc resection has been a predominant option to reduce the incidence of recurrence[4,5]. However, the patella is a crucial component of the extensor mechanism. Total patellectomy without following proper reconstruction can lead to disruption of the knee joint. Therefore, exploration of functional reconstruction of the extensor mechanism is worthwhile.
Several methods for the reconstruction of extensor mechanisms have been applied, such as end-to-end suture of the quadriceps tendon and patellar tendon[6], allografting[5,7-9], and autografting[10-12]. Although these procedures have been reported to lead to reasonable functional outcomes, each has its corresponding disadvantages, such as donor site morbidity, extensor lag, disease transmission, and graft rejection. We proposed the introduction of three-dimensional (3D)-printed custom-made patellar endoprosthesis that can reconnect the quadriceps tendon and patellar tendon properly, and therefore restore acceptable postoperative lower-limb function. To our best knowledge, no study has been performed on this subject. The present paper describes detailed endoprosthesis design and surgical techniques in total patellar replacement for a patient with a recurrent Campanacci III GCTB.
In October 2017, a 54-year-old woman presented with a 4-mo history of progressive right knee pain and swelling.
No other health conditions were reported.
One year before visiting our outpatient department, the patient had been diagnosed as having Campanacci grade I GCTB of the patella at another institution. The curettage of the lesion and iliac autografting were performed, and the pain was relieved. During her visit to our department, the physical examination revealed mild swelling and slight tenderness in the anterior aspect of the right knee.
The patient’s father had hypertension.
The Visual Analog Scale (VAS)[13] score was 6. The affected knee flexion arc was 20°-80°, and 20° of extension lag was found. Meanwhile, the strength of an active knee extension was 3 of 5 in the muscle manual test. The Musculoskeletal Tumor Society (MSTS-93) scale[14] score was 13. No osteoarthritis occurred.
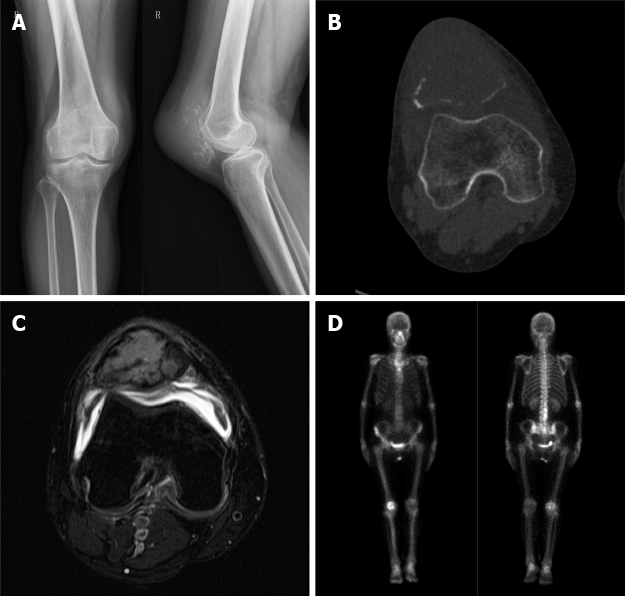
The patient has an AB blood type. Routine blood count and coagulation profile for the patient were within normal limits.
Plain radiograph revealed a lytic and expanded lesion involving the whole patella with focal cortical breaches and pathological fracture (Figure 1A). Computed tomography (CT) delineated the lesion (Figure 1B). The lesion on magnetic resonance imaging (MRI) was T2-hyperintense with small multiple fluid pockets (Figure 1C). There were areas with hemorrhagic component and cortical breach. Technetium-99m hydroxy methylene diphosphonate bone scintigraphy revealed a thin-rimmed doughnut pattern (Figure 1D). Chest CT detected no pulmonary metastasis.
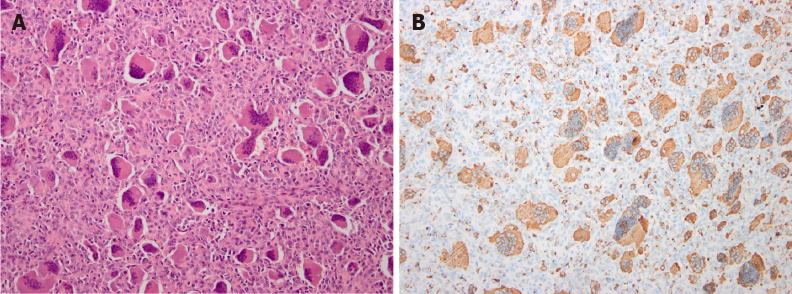
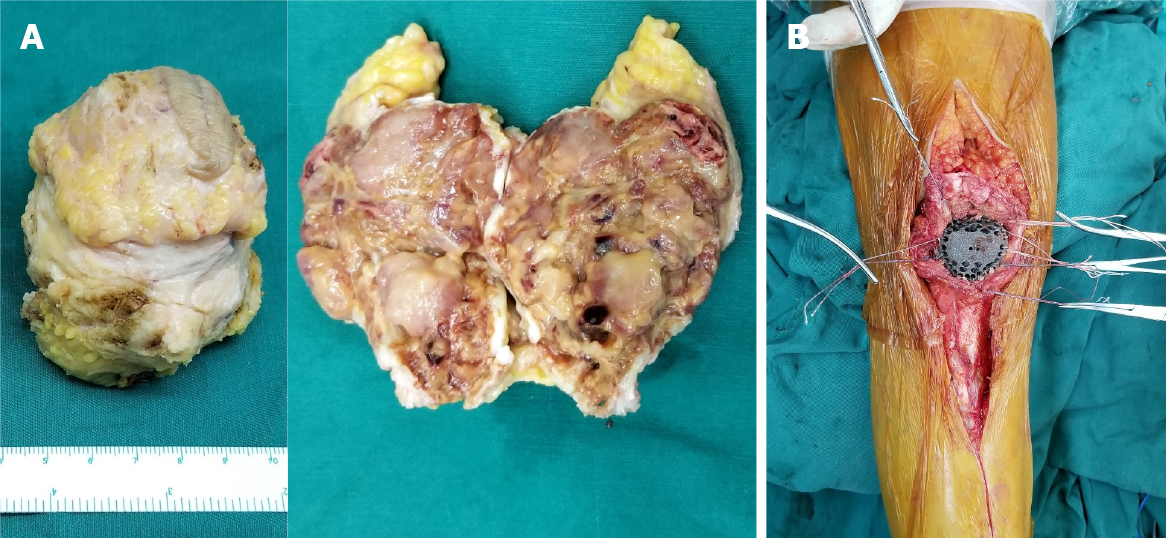
A biopsy confirmed the diagnose of Campanacci grade III GCTB with aneurysmal bone cyst (Figure 2)[1].
After a multidisciplinary team discussion, patellectomy was made. To reconstruct the extensor mechanism, reconstruction with 3D-printed custom-made patellar endoprosthesis was performed following en bloc resection.
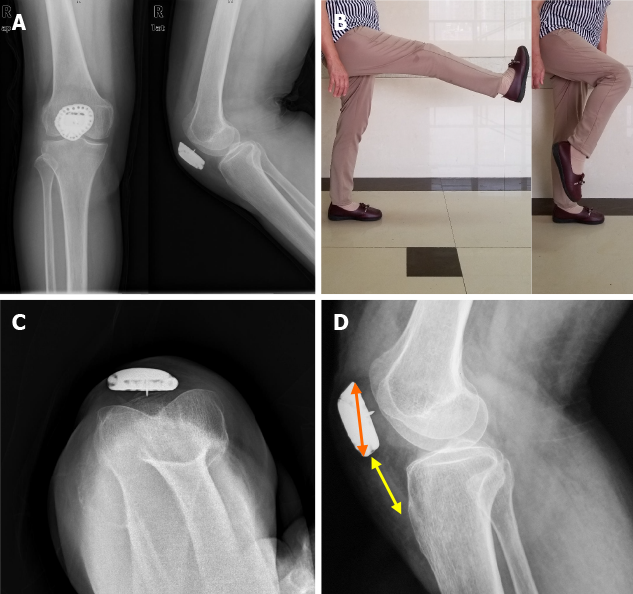
Postoperatively, the affected knee was immobilized in a plaster splint for 4 wk, and then passive extension and flexion were undertaken for 2 wk. After that, active extension and flexion were encouraged. The patient was allowed toe-touch weight-bearing within 6 wk and partial weight-bearing at 6-12 wk postoperatively. At the 35-mo follow-up, no evidence of local recurrence or pulmonary metastasis was observed. The patellofemoral joint showed no osteoarthritis on plain radiographs (Figure 3A). The active flexion arc was 0°-120° (Figure 3B), and no extension lag was detected. Meanwhile, the strength of the active extension was 5 of 5 in the muscle manual test—the postoperative MSTS-93 score 29. The VAS score was 0. A favorable patellar tracking was detected by patellar axial radiography (Figure 3C). The Insall-Salvati ratio (ISR)[15] was 0.93 (3.81/4.09) (Figure 3D). The reconstruction with 3D-printed custom-made patellar endoprosthesis after total patellectomy can reconnect the quadriceps tendon and patellar tendon properly, restoring acceptable postoperative lower-limb function.
To date, total patellectomies have been reported in treating Campanacci grade III GCTB or malignant neoplasms arising from the patella[5,6,8,10,16]. To repair the consequent defect in the extensor mechanism, several reconstruction methods including end-to-end suture of the quadriceps tendon and patellar tendon[6], allografting[5,7,8], and autografting[10,11] have been proposed. Still, each of them has its demerits (Table 1)[5,6,17-19].
| Ref. | No. of patients | Ennecking stage | Follow-up (yr) | Reconstruction | Clinical outcomes | Complications |
| Mercuri et al[17] | 4 | 3 | Average 18.5 | Not mentioned | All had full motion; no instability; no limping | One local recurrence underwent amputation |
| Agarwal et al[18] | 9 | 3 | Average 5.3 | Five had free fascia lata strip graft | Extensor lag of 10°-20°; average active ROM 80° | Benign pulmonary metastasis |
| Malhotra et al[5] | 1 | 3 | 3 | Patella bone tendon allograft | Knee ROM 80°; no extensor lag; no pain | - |
| Görmeli et al[19] | 1 | 3 | 1 | Achilles allograft | ROM 110º flexion; strength loss 51.1% in extensor and 21.1% in flexor | - |
| Tripathy et al[6] | 1 | 3 | 2 | End-to-end repair of quadriceps to the patellar tendon | ROM 130º; normal gait | No local recurrence or distant metastasis |
The end-to-end suture of the quadriceps tendon and patellar tendon leads to the shortage of extensor mechanism and limits the range of motion (ROM) of the knee. The autografting utilizing tendon grafts lengthens the extensor mechanism. Nevertheless, the donor site morbidities and insufficient mechanical property still limit its application. Allografting with the patella and its apparatus was reported with acceptable function. However, disease transmission and graft rejection are not uncommon. Additionally, the difficulty in vascularization of the patellar allograft can imperil the allograft's long-term durability[20]. So far, there has been no unanimous view on the prior therapeutic method among them, and the new approach is under exploration. With the advent of computer-aided design techniques and the improvement of 3D printing technology, reconstructing complex bone defects with custom-made endoprosthesis has become feasible[21,22]. Therefore, we performed a reconstruction using a 3D-printed custom-made patellar endoprosthesis for a defect in the extensor mechanism following total patellectomy. We found that the postoperative function was satisfactory with no incidence of complications.
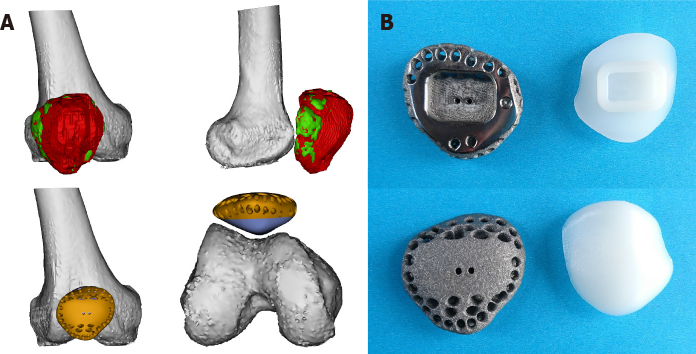
The endoprosthesis was designed by our clinical team and fabricated by Chunli Co., Ltd. (Tongzhou, Beijing, China). Building virtual 3D models of the affected patella, distal femur, proximal tibia, and contralateral patella was the first step, importing 3D-CT data into Mimics V22.0 software (Materialise Corp., Leuven, Belgium). The mirror model of the normal contralateral patella was generated as the endoprosthesis prototype, and we measured the largest transverse diameter, suprainferior diameter, and patella height of the unaffected patella. The location of the prototype was determined as the natural location of the patella at full knee extension. After that, we adjusted the prototype's orientation to conform to the right track of endoprosthesis along the trochlear groove. The articular surface was then modified according to the cartilage model built from the MRI data (Figure 4A). The endoprosthesis was composed of a metal component and an ultrahigh-molecular-weight polyethylene (Orthoplastics Ltd., Lancashire, United Kingdom) component. To assemble the two parts tightly, a specialized polyethylene lock structure was embedded into the metal component. The design of a 2-mm-extended margin of the endoprosthesis enables flexible adjustment of peri-patellar soft tissue tension. Finally, suture holes were distributed along the margin of the endoprosthesis to secure the extensor mechanism and retinaculum. The ultrahigh-molecular-weight polyethylene component was manufactured by computerized numerical control engraving technology. The metal component was fabricated by electron beam melting technology (ARCAM Q10 plus, Mölndal, Sweden) (Figure 4B).
During the surgery, the patellectomy was performed first (Figure 5A). Then, we assembled the two components of the patellar endoprosthesis after ensuring the feasibility of suturing the retinaculum to the endoprosthesis with appropriate tension. The intraoperative soft tissue reconstruction is as important as the endoprosthesis feature design because this procedure also determines patellar tracking and the tension of the extensor mechanism. The patella height was confirmed by the ISR. The patella tracking was checked by the ‘no thumb technique’ with flexing the knee joint from 30° to 90°[23]. The endoprosthesis was then stabilized at the natural location at full knee extension. The Number 5 EthibondTM (Ethicon Inc, Somerville NJ, United States) sutures were woven into the suture holes and retinaculum but without knotting till all the sutures were placed. Thereafter, the distal edge was fixed tightly at the priority, followed by the proximal edge. We then secured the medial and lateral edges to patella retinacula simultaneously to counterbalance peri-patellar tension. After obtaining a considerable prosthetic height and tracking, all the sutures were knotted simultaneously. The 3D-printed custom-made endoprosthesis fit the defect in the extensor mechanism and was secured by nonabsorbable sutures (Figure 5B). However, the maximal forces across the quadriceps tendon have been recorded at 3200 N, whereas those across the patellar ligament are 2800 N[24]. To strengthen the fixation, we specified the suture holes with a thickened and rounded bridge to enhance the durability. The inverting suture was performed to protect the sliding between superficial and deep fascia surrounding the endoprosthesis. Finally, the rotation of gastrocnemius myocutaneous flap enabled early soft tissue coverage and augmented the extensor mechanism[25].
The natural location of the patella is associated with a reasonable function. The patella is an essential component of the extensor mechanism to improve quadriceps efficiency by increasing the extensor mechanism's lever arm so that the last 15° from flexion to the full extension can be obtained more efficiently[26]. Hence, the deficiency of the patella and lengthened extensor mechanism can cause extensor lag and jeopardize postoperative function[27]. In our application, the anatomical feature of the endoprosthesis, the preservation of quadriceps tendon and patellar tendon, the right location and well retinaculum reconstruction enabled by extended 2-mm-surrounding-edge, and the confirmation of the full extension of the knee joint during suture procedure allow for reconstructing the patella in situ to maximize the mechanical properties of the extensor mechanism. As a result, the extensor lag of 0°, the ROM of 120°, and the MSTS score of 29 are acceptable[28].
The specially modified articular surface of the patella reduces the degeneration of the patellofemoral joint. During flexion to full extension of the knee joint, the compression force on the patellofemoral joint is tremendous[26]. Previously, Berkmortel et al[29] demonstrated that only the material with modulus below approximately 300 MPa significantly reduced cartilage contact stresses to more desirable levels. At present, only several materials fulfill this demand, and their long-term fatigue performances are not fully addressed. As a result, with the ability to reduce endoprosthesis weight and the possibility for strength and wear properties, ultrahigh-molecular-weight polyethylene was applied in our endoprosthesis and covered all the articular surfaces[30,31]. Meanwhile, the modification of the articular surface integrated the cartilage and obtained a reasonable matching degree to the articular surface of the femoral trochlear to enlarge the contact area so that the contact stress can be minimized, providing a preliminary basement for good tracking of the patellar endoprosthesis[26,31]. Consequently, no wound complication occurred, and the patient acquired full strength of active knee extension.
This study had several limitations. First, the patella tendon reconstruction was not included in our procedure, which might lead to more incredible difficulty. In that situation, autografting with tendons would be added. Second, the follow-up duration was short, and unknown drawbacks might occur in the long term. We will need to follow this patient over a longer period to see whether the generally good results that we observed will endure over time, especially the integration between the endoprosthesis and the host tendon. Third, although ultrahigh-molecular-weight polyethylene was applied in our endoprosthesis design, it still had relatively high modulus compared to cartilage. Therefore, investigating novel materials in the articular surface to prevent cartilage degeneration is required in such hemiarthrop
The 3D-printed custom-made endoprosthetic replacement may be a feasible therapeutic option for the reconstruction following total patellectomy. The patella normal reconstruction, the precise-fit articular design, and the augmentation with gastrocnemius flap could lead to good knee function and a low complication rate. However, as we have presented only short-term follow-up outcomes, this technique's long-term efficacy regarding postoperative knee function and degeneration is yet to be clarified.
We are thankful to the nurse team from the Department of Orthopedics, West China Hospital for their support. We are thankful to the patient enrolled in this study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Borakati A, Paul S S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am. 1987;69:106-114. [PubMed] |
| 2. | Shibata T, Nishio J, Matsunaga T, Aoki M, Iwasaki H, Naito M. Giant cell tumor of the patella: An uncommon cause of anterior knee pain. Mol Clin Oncol. 2015;3:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Singh J, James SL, Kroon HM, Woertler K, Anderson SE, Jundt G, Davies AM. Tumour and tumour-like lesions of the patella--a multicentre experience. Eur Radiol. 2009;19:701-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Lu M, Min L, Xiao C, Li Y, Luo Y, Zhou Y, Zhang W, Tu C. Uncemented three-dimensional-printed prosthetic replacement for giant cell tumor of distal radius: a new design of prosthesis and surgical techniques. Cancer Manag Res. 2018;10:265-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Malhotra R, Sharma L, Kumar V, Nataraj AR. Giant cell tumor of the patella and its management using a patella, patellar tendon, and tibial tubercle allograft. Knee Surg Sports Traumatol Arthrosc. 2010;18:167-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Tripathy SK, Doki S, Behera G, Sable M. Giant Cell Tumor with Secondary Aneurysmal Bone Cyst of the Patella: A Case Report. Cureus. 2019;11:e5819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Müller DA, Beltrami G, Scoccianti G, Cuomo P, Totti F, Capanna R. Allograft Reconstruction of the Extensor Mechanism after Resection of Soft Tissue Sarcoma. Adv Orthop. 2018;2018:6275861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Alqasim E, Aljowder A, Alammari N, Joudeh AA. Total patellectomy with extensor mechanism reconstruction following pathological fracture due to patellar Ewing's sarcoma. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Burnett RS, Berger RA, Della Valle CJ, Sporer SM, Jacobs JJ, Paprosky WG, Rosenberg AG. Extensor mechanism allograft reconstruction after total knee arthroplasty. J Bone Joint Surg Am. 2005;87 Suppl 1:175-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Gomes AR, Campos FN, Becker NM, Tamanini JG. Aneurysmal Patellar Bone Cyst: Case Reportt. Rev Bras Ortop (Sao Paulo). 2019;54:609-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Valsalan RM, Zacharia B. Ewings sarcoma of patella: A rare entity treated with a novel technique of extensor mechanism reconstruction using tendoachilles auto graft. World J Orthop. 2015;6:744-749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Machens HG, Siemers F, Kaun M, Krapohl B, Reichert B, Russlies M, Krüger S, Stöckelhuber B, Mailänder P. Patellar tendon reconstruction using a free latissimus dorsi flap following resection of a prepatellar myxofibrosarcoma: case report. J Reconstr Microsurg. 2005;21:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Heller GZ, Manuguerra M, Chow R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. 2016;13:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 355] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 14. | Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993: 241-246. [PubMed] |
| 15. | Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1105] [Cited by in RCA: 995] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 16. | Çetinkaya M, Özer H, Selek HY, Erekul S. Total patellectomy for patellar aneurysmal bone cyst. Eklem Hastalik Cerrahisi. 2016;27:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Mercuri M, Casadei R. Patellar tumors. Clin Orthop Relat Res. 2001: 35-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Agarwal S, Jain UK, Chandra T, Bansal GJ, Mishra US. Giant-cell tumors of the patella. Orthopedics. 2002;25:749-751. [PubMed] |
| 19. | Görmeli G, Görmeli CA, Maraş Özdemir Z, Sevimli R, Akpolat N. [A patellar giant-cell tumor with soft tissue involvement: an alternative treatment method and review of the literature]. Eklem Hastalik Cerrahisi. 2015;26:110-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Imanishi J, Grinsell D, Choong PF. Bone-patellar tendon-bone allograft reconstruction for peri-patellar tendon sarcomas: case series. Springerplus. 2015;4:740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Wang J, Min L, Lu M, Zhang Y, Wang Y, Luo Y, Zhou Y, Duan H, Tu C. What are the Complications of Three-dimensionally Printed, Custom-made, Integrative Hemipelvic Endoprostheses in Patients with Primary Malignancies Involving the Acetabulum, and What is the Function of These Patients? Clin Orthop Relat Res. 2020;478:2487-2501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 22. | Wei R, Guo W, Ji T, Zhang Y, Liang H. One-step reconstruction with a 3D-printed, custom-made prosthesis after total en bloc sacrectomy: a technical note. Eur Spine J. 2017;26:1902-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 23. | Cho WS, Woo JH, Park HY, Youm YS, Kim BK. Should the 'no thumb technique' be the golden standard for evaluating patellar tracking in total knee arthroplasty? Knee. 2011;18:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715-724. [PubMed] |
| 25. | Cipriano CA, Dalton J, McDonald DJ. Does Patellar Tendon Repair With Gastrocnemius Flap Augmentation Effectively Restore Active Extension After Proximal Tibial Sarcoma Resection? Clin Orthop Relat Res. 2019;477:584-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Fox AJ, Wanivenhaus F, Rodeo SA. The basic science of the patella: structure, composition, and function. J Knee Surg. 2012;25:127-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 27. | Shimose S, Sugita T, Kubo T, Matsuo T, Ochi M. Reconstructed patellar tendon length after proximal tibia prosthetic replacement. Clin Orthop Relat Res. 2005;439:176-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture. 2000;12:143-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 265] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 29. | Berkmortel C, Langohr GDG, King G, Johnson J. Hemiarthroplasty implants should have very low stiffness to optimize cartilage contact stress. J Orthop Res. 2020;38:1719-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Gibon E, Mouton A, Passeron D, Le Strat V, Graff W, Marmor S. Doctor, what does my knee arthroplasty weigh? J Arthroplasty. 2014;29:2091-2094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Roussot MA, Haddad FS. The evolution of patellofemoral prosthetic design in total knee arthroplasty: how far have we come? EFORT Open Rev. 2019;4:503-512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |