Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2446
Peer-review started: December 25, 2020
First decision: January 17, 2021
Revised: January 25, 2021
Accepted: February 25, 2021
Article in press: February 25, 2021
Published online: April 16, 2021
Processing time: 98 Days and 3.3 Hours
Colonoscopy within 24 h of hospital admission for colonic diverticular bleeding (CDB) is recommended. However, little is known about rates of rebleeding within 30 d. We posited that a group of patients who underwent contrast-enhanced computed tomography (CT) within 4 h of the last hematochezia and colonoscopy within 24 h would experience fewer incidences of rebleeding.
To evaluate the outcomes of early colonoscopy for CDB among different groups of patients.
Data from 182 patients with CDB who underwent contrast-enhanced CT and colonoscopy between January 2011 and December 2018 at the study site were retrospectively reviewed. Patients were divided into groups based on the timing of the CT imaging, within or at 4 h were defined as urgent CTs (n = 100) and those performed after 4 h were defined as elective CTs (n = 82). Main outcomes included rebleeding within 30 d and the identification of stigmata of recent hemorrhage (SRH) (i.e., active bleeding, non-bleeding visible vessels, or adherent clots).
In total, 182 patients (126 men and 56 women) with median ages of 68.6 (range, 37-92) and 73.7 (range, 48-93) years, respectively, underwent CT imaging and colonoscopy within 24 h of the last hematochezia. Patients for whom CT was performed within 4 h of the last hematochezia were included in the urgent CT group (n = 100) and patients for whom CT was performed after 4 h were included in the elective CT group (n = 82). SRH were identified in 35.0% (35/100) of the urgent CT cases and 7.3% (6/82) of the elective CT cases (P < 0.01). Among all patients with extravasation-positive images on CT, SRH was identified in 31 out of 47 patients (66.0%) in the urgent CT group and 4 out of 20 patients (20.0%) in the elective CT group (P < 0.01). Furthermore, rates of rebleeding within 30 d were significantly improved in the urgent CT and extravasation-positive cases (P < 0.05). Results from the evaluation of early colonoscopy did not show a difference in the ability to detect SRH identification or rebleeding rates. Only cases by urgent CT reduced risk of rebleeding due to the evidence of active bleeding on the image.
To improve rates of rebleeding, colonoscopy is recommended within 24 h in patients with extravasation-positive CT images within 4 h of the last hema-tochezia. Otherwise, elective colonoscopy can be performed.
Core Tip: While colonoscopy within 24 h of hospital admission for colonic diverticular bleeding (CDB) is recommended, there is no evidence of improved rates of rebleeding within 30 d. This study aimed to evaluate outcomes of early colonoscopy for CDB. Results indicate that rebleeding significantly improved in patients with extravasation-positive computed tomography images taken within 4 h of the last hematochezia (P < 0.05). Clinicians are advised to utilize contrast-enhanced computed tomography within 4 h of active CDB to detect extravasation-positive cases. For these patients, colonoscopy is recommended within 24 h to reduce the risk of rebleeding.
- Citation: Ochi M, Kamoshida T, Hamano Y, Ohkawara A, Ohkawara H, Kakinoki N, Yamaguchi Y, Hirai S, Yanaka A. Early colonoscopy and urgent contrast enhanced computed tomography for colonic diverticular bleeding reduces risk of rebleeding. World J Clin Cases 2021; 9(11): 2446-2457
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2446.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2446
Causes of lower gastrointestinal bleeding (LGIB) include colonic polyps, diverticular disease, hemorrhoids, inflammatory bowel disease, and ischemic colitis. Colonic diverticular bleeding (CDB) accounts for approximately 40.0% of LGIB cases[1-3]. CDB stops spontaneously in approximately 75.0% of cases, whereas bleeding persists in approximately 25.0% of cases, requiring interventions such as blood transfusions and hemostatic treatments[1-4]. Colonoscopy is one of the best methods for diagnosing CDB, leading to shortened hospital stays and reduced rates of rebleeding and surgery[3-6].
Stigmata of recent hemorrhage (SRH) are important endoscopic findings for diagnosing CDB. If patients with SRH receive conservative treatment without endoscopic hemostatic interventions, the rebleeding rate within 30 d may be as high as 60.0%, but endoscopic hemostatic interventions significantly reduce these rates[3,7]. Therefore, it is important to establish an effective examination method for identifying SRH to reduce the risk of early rebleeding.
Recent studies have demonstrated the effectiveness of computed tomography (CT) before colonoscopy. For example, compared with colonoscopy alone, contrast-enhanced CT before colonoscopy was shown to improve the identification of SRH[8], and early contrast-enhanced CT, rather than elective CT before colonoscopy, improved the specificity of SRH identification[9]. Previous studies suggest that colonoscopy should be performed within 24 h of hospital admission to increase the effectiveness of diagnosis and treatment[5,10-13]. However, none of these studies showed an improvement in rates of rebleeding within 30 d. Therefore, it is not clear whether a full inspection colonoscopy within 24 h is necessary to improve rates of rebleeding within 30 d. This study aimed to evaluate the outcomes of early colonoscopy within 24 h by using CT findings for CDB.
This was a retrospective cohort study of patients admitted from January 2011 to December 2018 to an emergency hospital in a moderately populated (approximately 300000 people) area of Japan. Patients with LGIB were transported by ambulance or arrived in the emergency room via personal transportation and were first examined by emergency doctors who are on call 24 h/d. The doctors searched for the source of the LGIB by CT immediately after checking vital signs and performing blood tests. Patients with unstable hemodynamics (blood pressure less than 90 mmHg or hemoglobin level less than 7 g/dL) were treated with fluid or blood transfusion before CT. The indication for blood transfusion was a hemoglobin level less than 7 g/dL, and blood transfusion was performed until the level exceeded 7 g/dL. CT was performed after confirming that the hemoglobin level exceeded 7 g/dL or that the blood pressure was more than 90 mmHg. According to the institutional protocol, the consulting gastroenterologist performed colonoscopy to identify the source of bleeding.
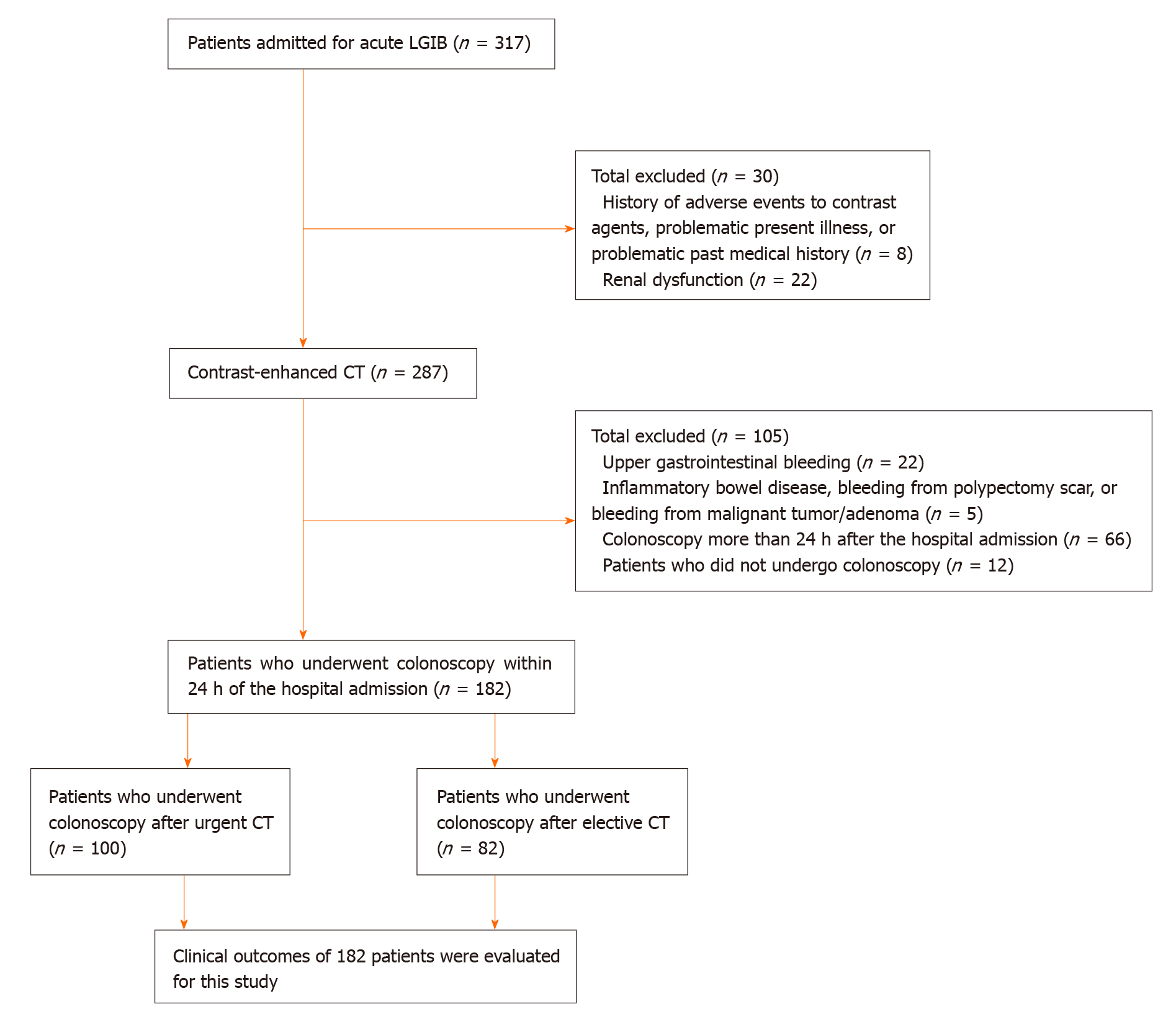
After a review of the medical charts, 182 patients, including 126 men and 56 women with median ages of 69 (range, 37-92) and 72 (range, 48-93) years, respectively, who underwent CT imaging and colonoscopy within 24 h of the last hematochezia, were included in the study. The last hematochezia was defined as the last LGIB excreted before the emergency room examination (time based on reports by paramedics). Patients were excluded according to the study criteria of (1) history of adverse events during examinations using contrast agents; (2) history of bronchial asthma, urticaria, atopic dermatitis, or severe thyroid disease; (3) use of a biguanide diabetes drug or beta-blocker; (4) current or possible pregnancy; (5) estimated glomerular filtration rate of < 45 mL/min per 1.73 m2; (6) diagnosis of upper gastrointestinal (GI) or small bowel bleeding based on upper GI endoscopy or capsule endoscopy; (7) diagnosis of ulcerative colitis or Crohn’s disease or diagnosis of bleeding from a polypectomy scar; (8) diagnosis of bleeding from a malignant tumor or adenoma; (9) colonoscopy more than 24 h from the last hematochezia; and (10) failure to undergo colonoscopy. Figure 1 shows the study flowchart for patients.
This study received approval from Hitachi General Hospital’s institutional review board (No. 2019-20) and was conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained in the form of an opt-out option on the website (http://www.hitachi.co.jp/hospital/hitachi/infor/opto-out/index.html). This study was registered with the University Hospital Medical Information Network (UMIN ID: 000037591).
Patients were examined for the source of bleeding in the lower GI tract using 64-channel multi-detector row CT scanners (Scenaria SE 128, Hitachi Ltd., Tokyo, Japan). Contrast-enhanced CT examinations were performed according to a protocol created by an experienced radiologist.
A nonionic water-soluble iodine-containing contrast medium [Omnipaque (iohexol) 300, GE Healthcare Japan, Tokyo, Japan] (80-100 mL) was injected intravenously at 2-3 mL/s. Two-phase imaging was performed with an arterial-dominant phase and a parenchymal phase. The imaging range was from the diaphragm to the pelvic floor, using both horizontal and coronal slices. All CT examinations were performed using an exposure time per rotation of 0.35 s, 512 × 512 matrix, 64 mm × 0.625 mm collimation, 120 kV, pitch factor 0.83 (collimation beam width = 40 mm), and a 350-mm field of view. The radiation dose was set by using the CT auto exposure control. All images were reconstructed using a standard reconstruction algorithm. Detection of the bleeding source was defined as the appearance of contrast medium extravasation into the intestinal lumen, which was determined by experienced radiologists who were blinded to the study hypothesis.
After patients were examined, CTs were performed to investigate the cause of the LGIB. Next, a total colonoscopy was performed within 24 h of hospital admission. For the procedure, 1-2 L polyethylene glycol was administered orally to the patients for bowel preparation. Total colonoscopy was performed after bowel preparation.
CDB diagnoses were classified as definitive or presumptive. After eliminating diseases such as colon cancer, ischemic enteritis, post-polypectomy bleeding, and bleeding from hemorrhoids, definitive CDB was visually confirmed based on the presence of diverticula with SRH, such as active bleeding, non-bleeding visible vessels, or adherent clots, on colonoscopy[7]. Presumptive CDB was defined as the presence of colonic diverticula with no evidence of bleeding and no other major colonic lesions confirmed by colonoscopy, gastroscopy, or capsule endoscopy[3,7].
In our study, all patients in the urgent and elective CT groups received endoscopic intervention after the identification of SRH. Hemostasis for CDB was performed with monotherapy using endoscopic clipping (EC). Transcatheter arterial embolization or surgery was performed if hemostasis with EC did not stop the bleeding or if endoscopic hemostasis was difficult.
Categorical variables are summarized as number (%) and continuous variables as mean or median ± SD. Differences between groups were examined with the chi-square and Mann-Whitney U tests. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software version 22 (IBM Corp., Armonk, NY, United States). The statistical methods of this study were reviewed by Ochi M from the Department of Gastroenterology, Hitachi General Hospital, Japan.
The 182 patients with CDB who underwent contrast-enhanced CT before colonoscopy were hospitalized and treated. The mean time from the last hematochezia episode to CT was 4.0 ± 2.8 h. CTs performed within or at 4 h were defined as urgent CTs (n = 100) and those performed after 4 h were defined as elective CTs (n = 82). The mean time from contrast-enhanced CT to colonoscopy for all patients was 11.4 ± 8.3 h, and for the urgent and elective CT groups, they were 8.3 ± 7.8 h and 15.1 ± 8.5 h, respectively. No statistically significant differences were found between the groups in terms of sex, medical history, medication history, physical findings, or blood test results (Table 1).
| Total | Urgent CT | Elective CT | P value | |
| n = 182 | n = 100 | n = 82 | ||
| Number of men, n (%) | 126 (69.2) | 71 (71.0) | 55 (67.1) | 0.65 |
| Median age, yr, mean ± SD | 71 ± 12.4 | 69 ± 13.3 | 72 ± 11.0 | 0.34 |
| BMI, kg/m2, mean ± SD | 23.5 ± 3.5 | 23.8 ± 3.5 | 23.1 ± 3.5 | 0.15 |
| Pulse rate, beat/min, mean ± SD | 81.3 ± 15.9 | 80.9 ± 15.9 | 81.8 ± 15.8 | 0.77 |
| Systolic blood pressure, mmHg, mean ± SD | 133.2 ± 24.8 | 132.8 ± 24.7 | 133.1 ± 25.1 | 0.74 |
| Hypertension, % | 58.6 | 55.9 | 59.0 | 0.72 |
| Diabetes mellitus, % | 15.5 | 18.6 | 13.3 | 0.44 |
| Cerebrovascular disease, % | 17.7 | 19.6 | 14.5 | 0.38 |
| Ischemic heart disease, % | 18.8 | 14.7 | 24.7 | 0.15 |
| History of CDB, % | 36.5 | 41.2 | 28.9 | 0.10 |
| Bowel preparation1, % | 57.1 | 51.0 | 64.6 | 0.09 |
| Low-dose aspirin (≤ 100 mg/d), % | 20.4 | 19.6 | 20.5 | 0.99 |
| Non-aspirin antiplatelets, % | 16.0 | 13.7 | 18.1 | 0.54 |
| Anticoagulants, % | 9.4 | 8.8 | 9.6 | 0.99 |
| NSAIDs, % | 16.6 | 19.6 | 12 | 0.24 |
| Syncope, % | 8.8 | 11.8 | 6.0 | 0.27 |
| Abdominal pain, % | 3.9 | 4.9 | 2.4 | 0.62 |
| Hemoglobin, g/dL, mean ± SD | 11.4 ± 2.4 | 11.5 ± 2.4 | 11.3 ± 2.4 | 0.38 |
| Platelet, count/mm3, mean ± SD | 20.3 ± 5.5 | 20.4 ± 5.8 | 19.9 ± 5.3 | 0.54 |
| Cr, mg/dL, mean ± SD | 1.1 ± 1.1 | 1.2 ± 1.3 | 1.0 ± 0.7 | 0.24 |
Extravasation-positive images were observed on contrast-enhanced CT in 47 of 100 patients (47.0%) who underwent examination within 4 h and in 20 of 82 patients (24.4%) who underwent examination after 4 h (P < 0.01). Overall, SRH was identified in 35 out of 100 patients (35.0%) in the urgent CT group and 6 out of 82 patients (7.3%) in the elective CT group (P < 0.01). Further, SRH was identified as active bleeding in 26 out of 100 patients (26.0%) in the urgent CT group and 4 out of 82 patients (4.9%) in the elective CT group (P < 0.01). Active bleeding constituted approximately 75% of the overall SRH (26/35 cases) (Table 2).
| Total | Urgent CT | Elective CT | P value | |
| n = 182 | n = 100 | n = 82 | ||
| Extravasation-positive rate, n (%) | 67 (36.8) | 47 (47.0) | 20 (24.4) | < 0.01 |
| SRH identification, n (%) | 41 (22.5) | 35 (35.0) | 6 (7.3) | < 0.01 |
| Active bleeding | 30 (16.5) | 26 (26.0) | 4 (4.9) | < 0.01 |
| Adherent clot | 7 (3.8) | 6 (6.0) | 1 (1.2) | 0.06 |
| Non-bleeding visible vessel | 4 (2.2) | 3 (3.0) | 1 (1.2) | 0.32 |
| Hospitalization length of stay, d, mean ± SD | 7.4 ± 5.3 | 7.1 ± 4.1 | 7.7 ± 6.3 | 0.40 |
| Need for interventional radiology, n (%) | 4 (2.2) | 1 (1.0) | 3 (3.7) | 0.48 |
| Need for surgery, n (%) | 4 (2.2) | 0 (0.0) | 4 (4.9) | 0.08 |
| Blood transfusion, n (%) | 40 (22.0) | 24 (24.0) | 16 (19.5) | 0.61 |
| Amount of transfusion, units, mean ± SD | 1.1 ± 2.7 | 1.2 ± 2.6 | 1.0 ± 2.8 | 0.46 |
| Blood transfusion after SRH, n (%) | 17 (9.3) | 13 (13.0) | 4 (4.9) | 0.11 |
| Contrast media-related adverse events | ||||
| Nausea, vomiting n (%) | 1 (0.6) | 1 (1.0) | 0 | |
| Urticaria and skin rash, n (%) | 0 | 0 | 0 | |
| Pruritus, n (%) | 1 (0.6) | 0 | 1 (1.2) | |
| Erythema, n (%) | 0 | 0 | 0 | |
| Laryngeal edema, n (%) | 0 | 0 | 0 | |
| Sneezing, n (%) | 0 | 0 | 0 | |
| Coughing, n (%) | 0 | 0 | 0 | |
| Contrast media-related severe adverse events | ||||
| Dyspnea, n (%) | 0 | 0 | 0 | |
| Sudden drop in blood pressure, n (%) | 0 | 0 | 0 | |
| Loss of consciousness, n (%) | 0 | 0 | 0 | |
| Cardiac arrest, n (%) | 0 | 0 | 0 |
Statistically significant differences between the groups were not observed for length of hospitalization, rate of red cell concentrate transfusion, amount of transfusion, history of blood transfusion after SRH identification, or adverse events during contrast-enhanced CT. The overall incidence of adverse events during CT was 1.1% with no severe adverse events (Table 2).
For the outcomes of SRH identification and rebleeding according to timing of CT and the contrast-enhanced CT findings, the only statistically significant differences between the urgent CT group (≤ 4 h) and the extravasation-positive cases were observed for SRH identification and rebleeding within 30 d (P < 0.05) (Tables 3-6). In addition, there was no difference in the ability to identify SRH or rates of rebleeding according to the timing of the colonoscopy (within 12 h and more than 12 h) (Tables 3-6).
| Rate of SRH identification by contrast-enhanced CT findings (%) | ||||||
| Extravasation-positive cases | Extravasation-negative cases | |||||
| Time from last hematochezia to colonoscopy within 12 h | Time from last hematochezia to colonoscopy after 12 h | P value | Time from last hematochezia to colonoscopy within 12 h | Time from last hematochezia to colonoscopy after 12 h | P value | |
| Urgent CT group (≤ 4 h) | 61.8 (21/34) | 76.9 (10/13) | 0.52 | 8.7 (2/23) | 6.7 (2/30) | 1.00 |
| Elective CT group (> 4 h) | 18.2 (2/11) | 22.2 (2/9) | NA | 4.5 (1/24) | 2.6 (1/38) | 1.00 |
| P value | 0.03 | NA | 0.97 | 0.83 | ||
| Rate of SRH identification by contrast-enhanced CT findings (%) | |||
| Extravasation-positive cases | Extravasation-negative cases | ||
| Time from last hematochezia to colonoscopy within 24 h | Time from last hematochezia to colonoscopy within 24 h | P value | |
| Urgent CT group (≤ 4 h) | 66.0 (31/47) | 7.5 (4/53) | < 0.01 |
| Elective CT group (> 4 h) | 20.0 (4/20) | 3.2 (2/62) | 0.31 |
| P value | < 0.01 | 0.54 | |
| Rate of rebleeding within 30 d by contrast-enhanced CT findings (%) | ||||||
| Extravasation-positive cases | Extravasation-negative cases | |||||
| Time from last hematochezia to colonoscopy within 12 h | Time from last hematochezia to colonoscopy after 12 h | P value | Time from last hematochezia to colonoscopy within 12 h | Time from last hematochezia to colonoscopy after 12 h | P value | |
| Urgent CT group (≤ 4 h) | 5.9 (2/34) | 7.7 (1/13) | 1.00 | 30.4 (7/23) | 33.3 (10/30) | 1.00 |
| Elective CT group (> 4 h) | 36.4 (4/11) | 22.2 (2/9) | NA | 16.7 (4/24) | 21.1 (8/38) | 0.92 |
| P value | 0.04 | NA | 0.44 | 0.39 | ||
| Rate of rebleeding within 30 d by contrast-enhanced CT findings (%) | |||
| Extravasation-positive cases | Extravasation-negative cases | ||
| Time from last hematochezia to colonoscopy within 24 h | Time from last hematochezia to colonoscopy within 24 h | P value | |
| Urgent CT group (≤ 4 h) | 6.4 (3/47) | 32.1 (17/53) | < 0.01 |
| Elective CT group (> 4 h) | 30.0 (6/20) | 19.4 (12/62) | 0.49 |
| P value | 0.03 | 0.18 | |
Among all patients with extravasation-positive images on CT, SRH was identified in 31 out of 47 patients (66.0%) in the urgent CT group and 4 out of 20 patients (20.0%) in the elective CT group (P < 0.01). Active bleeding was detected in 22 out of 47 patients (46.8%) in the urgent CT group and 2 out of 20 patients (10.0%) in the elective CT group (P < 0.01) (Table 7).
| SRH identification rate (%) | |||||||
| Extravasation-positive cases | Extravasation-negative cases | ||||||
| All SRH | Active bleeding of SRH | Adherent clot of SRH | NBVV of SRH | ||||
| All CDB | 52.2 (35/67) | 35.8 (24/67) | 10.4 (7/67) | 6.0 (4/67) | 5.2 (6/115) | ||
| Urgent CT group (≤ 4 h) | 66.0 (31/47) | 46.8 (22/47) | 12.8 (6/47) | 4.5 (3/47) | 7.5 (4/53) | ||
| Elective CT group (> 4 h) | 20.0 (4/20) | 10.0 (2/20) | 5.0 (1/20) | 5.0 (1/20) | 3.2 (2/62) | ||
| P value | < 0.01 | < 0.01 | 0.45 | 0.83 | 0.54 | ||
| Concordance rate of extravasation-positive site to SRH identification site (%) | |||||||
| All SRH | Active bleeding of SRH | Adherent clot of SRH | NBVV of SRH | ||||
| All CDB | 91.4 (32/35) | 91.7 (22/24) | 85.7 (6/7) | 100 (4/4) | |||
| Urgent CT group (≤ 4 h) | 90.3 (28/31) | 90.9 (20/22) | 83.3 (5/6) | 100 (3/3) | |||
| Elective CT group (> 4 h) | 100 (4/4) | 100 (2/2) | 100 (1/1) | 100 (1/1) | |||
The concordance rate of extravasation-positive images to the identification of the active bleeding site was 20 out of 22 patients (90.9%) in the urgent CT group and 2 out of 2 patients (100%) in the elective CT group (Table 7).
Table 8 shows the accuracy of contrast-enhanced CT findings for predicting SRH by colonoscopy. Results in Table 8 were calculated based on the relationship between SRH and contrast-enhanced CT findings (Table 9).
| Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio | |
| All CDB | 85.4 (70.8-94.4) | 77.3 (69.5-83.9) | 3.69 (2.66-5.13) | 0.20 (0.10-0.41) |
| Urgent CT group ≤ 4 h | 88.6 (73.3-96.8) | 75.4 (63.1-85.2) | 3.50 (2.26-5.41) | 0.17 (0.07-0.40) |
| Elective CT group > 4 h | 66.7 (22.3-95.7) | 78.9 (68.1-87.5) | 3.00 (1.49-6.03) | 0.46 (0.17-1.24) |
| All cases | Urgent CT group (≤ 4 h) | Elective CT group (> 4 h) | ||||
| Extravasation-positive | Extravasation-negative | Extravasation-positive | Extravasation-negative | Extravasation-positive | Extravasation-negative | |
| SRH-positive | 35 | 6 | 31 | 4 | 4 | 2 |
| SRH-negative | 32 | 109 | 16 | 49 | 16 | 60 |
| SRH identification rate (%) | 52.2 (35/67) | 5.2 (6/115) | 66.0 (31/47) | 7.5 (4/53) | 20.0 (4/20) | 3.2 (2/62) |
| P value | < 0.01 | |||||
Contrast-enhanced CT for diagnosis of CDB had 85.4% sensitivity and 77.3% specificity for all cases. In the urgent CT group, the sensitivity was 88.6% and the specificity was 75.4%. In the elective CT group, the sensitivity was 66.7% and the specificity was 78.9%. In the urgent CT group, the positive likelihood ratio for identifying SRH was 3.50 and the negative likelihood ratio was 0.17. In the elective CT group, the positive likelihood ratio was 3.00 and the negative likelihood ratio was 0.46.
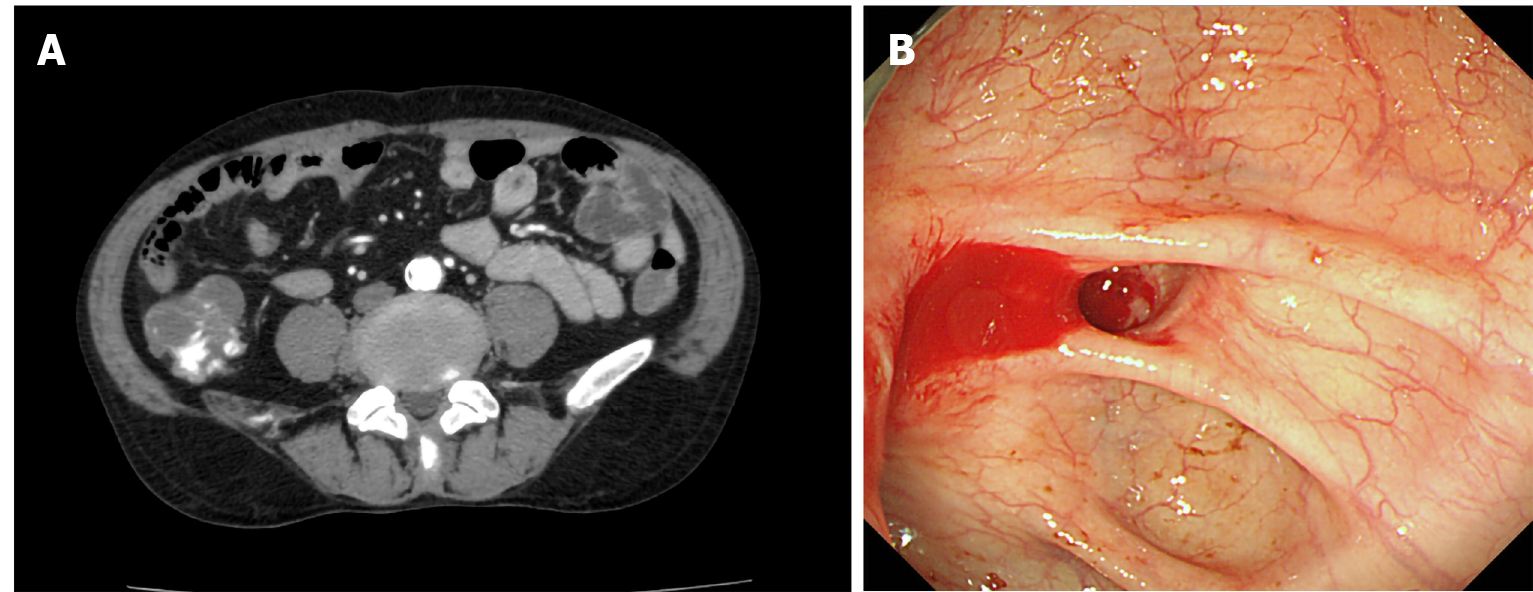
The present results show that extravasation-positive images in the cases of urgent CTs before colonoscopy were consistent with the endoscopic findings of active bleeding. Furthermore, most of the active bleeding sites were detected in the extravasation-positive CT images taken within 4 h, but the number of active bleeding sites decreased dramatically when the CT was performed more than 4 h from the last incidence of hematochezia. With urgent CT, there were significantly more extravasation-positive images because active bleeding is more frequent during this 4-h timeframe (Figure 2). Importantly, the results indicate that the occurrence of rebleeding within 30 d significantly improved in patients who underwent urgent CT (≤ 4 h) with extravasation-positive images.
These results raise the possibility that active bleeding, accounting for approximately 75% of all the cases, temporarily ceases before colonoscopy. This phenomenon may lead to a misdiagnosis of hemostasis, thus complicating treatment aimed to reduce rebleeding. While the effectiveness of early colonoscopy (≤ 24 h after hospital admission) has been reported in many studies, improved rates of rebleeding within 30 d has not been shown[10,11,14-16]. For example, a recent multicenter randomized controlled study did not report significant differences in SRH and rebleeding within 30 d between early colonoscopy (≤ 24 h) and elective (> 24 h) groups[17]. These results may have been due to the temporal nature of the active bleeding site.
Since the interval from last hematochezia to colonoscopy may affect the outcomes of SRH identification or rebleeding, we also evaluated the optimal timing of colonoscopy. However, the ability to detect SRH or rebleeding did not change in the present study according to colonoscopy timing. The patients were transported to the hospital after hematochezia where they underwent vital sign monitoring and blood tests. Patients with unstable hemodynamics were treated with fluids and/or blood transfusion. In addition, patients underwent bowel preparation before colonoscopy. Because colonoscopy can only be performed after testing and treatment to stabilize the patient, it was difficult to perform colonoscopy before active bleeding temporarily ceased (≤ 4 h). Thus, in our study, colonoscopy within 4 h of the last hematochezia was performed in only a small number of cases (18/182 cases).
Urgent CT can show active bleeding as an extravasation-positive image before it temporarily ceases, substantially narrowing the search area for SRH during colonoscopy. Furthermore, SRH can be easily identified during colonoscopy because active bleeding sites are visually distinguishable from the rest of the colon. Previous studies reported that CDB patients who received conservative treatment without colonoscopy intervention had a high rate of rebleeding within 30 d of 53%-66%, and that endoscopic hemostasis reduced the rebleeding rate[3,7]. These studies suggested that CDB patients with SRH who received conservative treatment relapsed over time. In our study, the rebleeding rate decreased because lesions with a risk of rebleeding were identified as SRH and hemostasis treatment was performed using colonoscopy. Thus, extravasation-positive images from urgent CT may contribute to lowered rates of rebleeding within 30 d and higher rates of SRH identification under limited conditions.
In previous studies, contrast-enhanced CT before colonoscopy, defined as CT within 4 h after hospital admission, had a high specificity (89.5%) and a high positive likelihood ratio (6.15) for the identification of CDB[9]. In our study, contrast-enhanced CT before colonoscopy defined as CT within 4 h of the last hematochezia, was highly sensitive (88.6%) and had a low negative likelihood ratio (0.17). Thus, CT performed within 4 h after the last hematochezia was an effective screening for SRH active bleeding.
Our hospital uses nonionic contrast media as contrast agents in contrast-enhanced CT. Nonionic contrast media have been associated with significantly fewer adverse events than ionic contrast media[18]. The reported adverse events with nonionic contrast media are extremely low, with the incidence of overall adverse events at 1.03% and incidence of severe adverse events at 0.01%[19], similar to the findings in the present study (1.1% and 0%, respectively). Therefore, we posit that contrast-enhanced CT before colonoscopy has an acceptably low rate of associated adverse events.
Our study had several advantages. For example, the study size was large and due to the single-center study design, the doctors followed the same system-wide protocols, reducing the variation between patient interventions, including the process of consultation with a gastroenterologist, CT, and colonoscopy within 24 h. Nevertheless, our study also had some limitations to consider. First, because this was a single-center study, there is the possibility of selection bias; however, we imposed strict exclusion criteria to minimize the possible effects. Second, many of the patients in the elective CT group were admitted to the hospital at night, and colonoscopies are performed during the day. Therefore, there was a higher chance for spontaneous resolution of the bleeding in these cases, making it more difficult to identify the bleeding site during colonoscopy. Third, because this was a retrospective analysis, a prospective analysis needs to be performed in the future to confirm a lowered risk of rebleeding with urgent CT in patients with extravasation-positive images.
We propose a new method of diagnosis and treatment of CDB using contrast-enhanced CT as a screening tool. To improve SRH and rebleeding within 30 d, colonoscopy should be performed within 24 h only if extravasation-positive images from contrast-enhanced CT occur within 4 h of the last hematochezia. In other cases, colonoscopy may be electively performed.
There is little evidence regarding lowered rates of rebleeding within 30 d after early colonoscopy for colonic diverticular bleeding (CDB).
We posited that contrast-enhanced computed tomography (CT) before colonoscopy for CDB reduces risk of rebleeding.
We evaluated the outcomes of early colonoscopy (within 24 h of hospital admission) by timing of contrast-enhanced CT for CDB.
This study included patients with CDB who underwent contrast-enhanced CT and colonoscopy between January 2011 and December 2018. Patients were divided into groups based on the timing of the CT imaging (urgent CT vs elective CT). Main outcomes included rebleeding within 30 d and the identification of stigmata of recent hemorrhage (SRH).
In total, 182 patients [urgent CT (n = 100) vs elective CT (n = 82)] with CDB underwent CT imaging and colonoscopy within 24 h of the last hematochezia. Among all patients with extravasation-positive images on CT, SRH was identified in 31 out of 47 patients (66.0%) in the urgent CT group and 4 out of 20 patients (20.0%) in the elective CT group (P < 0.01). The rates of rebleeding within 30 d were significantly lower in patients with extravasation-positive images among the urgent CT group (P < 0.05). Secondary analysis to determine the optimal timing for colonoscopy (within 12 h or more than 12 h), showed no difference in the ability to identify SRH or reduce rebleeding rates.
To improve SRH and rebleeding within 30 d, colonoscopy should be performed within 24 h if contrast-enhanced CT images taken within 4 h of the last hematochezia are extravasation-positive. In other cases, colonoscopy may be electively performed.
A prospective analysis is needed to add to the evidence for a lowered risk of rebleeding among urgent CT cases with extravasation-positive images.
We thank Mizutani S, MD (Department of Gastroenterology, Hitachi General Hospital) for help with data collection.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garg R S-Editor: Gao CC L-Editor: A P-Editor: Ma YJ
| 1. | Bloomfeld RS, Rockey DC, Shetzline MA. Endoscopic therapy of acute diverticular hemorrhage. Am J Gastroenterol. 2001;96:2367-2372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 97] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92:419-424. [PubMed] |
| 3. | Jensen DM, Machicado GA, Jutabha R, Kovacs TO. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med. 2000;342:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 423] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 4. | McGuire HH Jr. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 197] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 5. | Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol. 2016;111:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 299] [Article Influence: 33.2] [Reference Citation Analysis (2)] |
| 6. | Strate LL, Syngal S. Timing of colonoscopy: impact on length of hospital stay in patients with acute lower intestinal bleeding. Am J Gastroenterol. 2003;98:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Jensen DM, Ohning GV, Kovacs TO, Jutabha R, Ghassemi K, Dulai GS, Machicado GA. Natural history of definitive diverticular hemorrhage based on stigmata of recent hemorrhage and colonoscopic Doppler blood flow monitoring for risk stratification and definitive hemostasis. Gastrointest Endosc. 2016;83:416-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Nagata N, Niikura R, Aoki T, Moriyasu S, Sakurai T, Shimbo T, Shinozaki M, Sekine K, Okubo H, Watanabe K, Yokoi C, Yanase M, Akiyama J, Uemura N. Role of urgent contrast-enhanced multidetector computed tomography for acute lower gastrointestinal bleeding in patients undergoing early colonoscopy. J Gastroenterol. 2015;50:1162-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Umezawa S, Nagata N, Arimoto J, Uchiyama S, Higurashi T, Nakano K, Ishii N, Sakurai T, Moriyasu S, Takeda Y, Nagase H, Komatsu H, Nakajima A, Mizuki A. Contrast-enhanced CT for Colonic Diverticular Bleeding before Colonoscopy: A Prospective Multicenter Study. Radiology. 2018;288:755-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Sengupta N, Tapper EB, Feuerstein JD. Early Versus Delayed Colonoscopy in Hospitalized Patients With Lower Gastrointestinal Bleeding: A Meta-Analysis. J Clin Gastroenterol. 2017;51:352-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 11. | Seth A, Khan MA, Nollan R, Gupta D, Kamal S, Singh U, Kamal F, Howden CW. Does Urgent Colonoscopy Improve Outcomes in the Management of Lower Gastrointestinal Bleeding? Am J Med Sci. 2017;353:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | ASGE Standards of Practice Committee, Pasha SF, Shergill A, Acosta RD, Chandrasekhara V, Chathadi KV, Early D, Evans JA, Fisher D, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Saltzman JR, Cash BD. The role of endoscopy in the patient with lower GI bleeding. Gastrointest Endosc. 2014;79:875-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 13. | Nagata N, Ishii N, Manabe N, Tomizawa K, Urita Y, Funabiki T, Fujimori S, Kaise M. Guidelines for Colonic Diverticular Bleeding and Colonic Diverticulitis: Japan Gastroenterological Association. Digestion. 2019;99 Suppl 1:1-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 129] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 14. | Kouanda AM, Somsouk M, Sewell JL, Day LW. Urgent colonoscopy in patients with lower GI bleeding: a systematic review and meta-analysis. Gastrointest Endosc 2017; 86: 107-117. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol. 2010;105:2636-41; quiz 2642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 16. | Green BT, Rockey DC, Portwood G, Tarnasky PR, Guarisco S, Branch MS, Leung J, Jowell P. Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage: a randomized controlled trial. Am J Gastroenterol. 2005;100:2395-2402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 17. | Niikura R, Nagata N, Yamada A, Honda T, Hasatani K, Ishii N, Shiratori Y, Doyama H, Nishida T, Sumiyoshi T, Fujita T, Kiyotoki S, Yada T, Yamamoto K, Shinozaki T, Takata M, Mikami T, Mabe K, Hara K, Fujishiro M, Koike K. Efficacy and Safety of Early vs Elective Colonoscopy for Acute Lower Gastrointestinal Bleeding. Gastroenterology 2020; 158: 168-175. e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 18. | Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990;175:621-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1072] [Cited by in RCA: 911] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 19. | Suh YJ, Yoon SH, Hong H, Hahn S, Kang DY, Kang HR, Choi YH, Lee W. Acute Adverse Reactions to Nonionic Iodinated Contrast Media: A Meta-Analysis. Invest Radiol. 2019;54:589-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |