Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2400
Peer-review started: December 18, 2020
First decision: January 7, 2021
Revised: January 16, 2021
Accepted: February 8, 2021
Article in press: February 8, 2021
Published online: April 6, 2021
Processing time: 101 Days and 23.7 Hours
Patients with intraductal papillary mucinous neoplasm (IPMN) have an increased risk of pancreatic and extrapancreatic malignancies. Lymphomas are rare extrapancreatic malignancies, and in situ collisions of early gastric cancer and diffuse large B-cell lymphoma (DLBCL) are even rarer. Here, we report the first case of pancreatic cancer comorbid with in situ collision of extrapancreatic malignancies (early gastric cancer and DLBCL) in a follow-up IPMN patient. Furthermore, we have made innovations in the treatment of such cases.
An 81-year-old Japanese female diagnosed with IPMN developed elevated carbohydrate antigen (CA) 19-9 levels during follow-up. Because her CA19-9 levels continued to rise, endoscopic ultrasound (EUS) was performed and revealed a suspicious lesion at the pancreatic tail. However, lesions in the pancreas were not found by computed tomography, magnetic resonance imaging, or endoscopic retrograde cholangiopancreatography. To make an exact patho-logical diagnosis, EUS-guided fine needle aspiration was performed. To our supprise, early gastric cancer was found in preoperative gastroscopy. The gastric cancer was completely resected through endoscopic submucosal dissection before postoperative pathology identified early adenocarcinoma collided with DLBCL. Subsequent EUS-guided fine needle aspiration provided pathological support for the pancreatic cancer diagnosis, and then laparoscopic distal pancreatectomy and splenectomy were performed. CA19-9 levels returned to normal postoperatively.
Endoscopic submucosal dissection is appropriate for submucosal lymphomas in patients intoleratant of chemotherapy. EUS can detect small IPMN-related pancreatic tumors.
Core Tip: Since intraductal papillary mucinous neoplasm (IPMN) was defined as an independent disease, its unique characteristics have led to many detailed studies. In particular, IPMN-associated pancreatic cancer and extrapancreatic malignancy are focused on. These cases should be managed timely and optimally to improve outcomes and extend patients’ lives. Diffuse large B-cell lymphoma can appear together with early gastric cancer in IPMN and is usually difficult to diagnose before surgery. We recommend endoscopic submucosal dissection for early gastric cancer with local lymphoma, especially for patients who have concerns about undergoing chemotherapy. We believe that endoscopic ultrasound is superior to computed tomography and magnetic resonance imaging for the follow-up of IPMN to diagnose pancreatic cancer.
- Citation: Ma YH, Yamaguchi T, Yasumura T, Kuno T, Kobayashi S, Yoshida T, Ishida T, Ishida Y, Takaoka S, Fan JL, Enomoto N. Pancreatic cancer secondary to intraductal papillary mucinous neoplasm with collision between gastric cancer and B-cell lymphoma: A case report. World J Clin Cases 2021; 9(10): 2400-2408
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2400.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2400
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas was first described in the 1980s[1] and was regarded as a unique clinicopathological entity by the World Health Organization in the 1990s[2]. IPMN is associated with a high incidence of pancreatic cancer and the presence of extrapancreatic malignancies. Extrapancreatic malignancies typically occur before IPMN, are more common among patients with IPMN than in healthy individuals, and show increased incidence with age[3-5]. Extrapancreatic malignancies in IPMN are common in the gastrointestinal tract, lung, prostate, and breast. Although they can also occur in the ovaries, esophagus, liver, kidney, and thyroid[3,6], lymphomas are rare in IPMN[3,7].
Here, we report a follow-up of an IPMN patient who showed elevated carbohydrate antigen (CA) 19-9 and was found to have pancreatic cancer with in situ collision of early gastric cancer and diffuse large B-cell lymphoma (DLBCL).
Timeline: The timeline of diagnosis and treatment after admission is shown in Table 1.
| Time | Events |
| October 11, 2015 | Patient diagnosed with intraductal papillary mucinous neoplasm |
| November 13, 2017 | Patient diagnosed with CA19-9 increased |
| April 16, 2018 | Patient’s EUS examination was revealed a mass in the tail of the pancreas |
| June 1, 2018 | Patient diagnosed with early gastric cancer |
| July 26, 2018 | Patient was treated with endoscopic submucosal dissection |
| July 31, 2018 | ESD resected specimen, pathological diagnosis of submucosal diffuse large B cell lymphoma |
| February 15, 2019 | Patients underwent EUS-FNA were diagnosed with pancreatic cancer |
| March 7, 2019 | Patient underwent surgery for pancreatic cancer |
| June 5, 2019 | CA19-9 returned to normal |
An 81-year-old Japanese woman had been diagnosed with a branch-duct disease IPMN lesion in the pancreas by abdominal computed tomography (CT) in 2015. In March 2017, an abdominal CT examination had showed no significant change in IPMN, but in November 2017, blood examinations found elevated CA19-9 (87 U/mL).
In March 2018, the patient was transferred to our hospital for further examination. CT and magnetic resonance imaging (MRI) found the known branch-duct disease IPMN lesion (12 mm) and confirmed localized pancreatitis in the tail of the pancreas and mild pancreatic duct dilatation (2.2 mm). In April 2018, endoscopic ultrasound (EUS) (UE260 Ultrasonic gastrovideoscope; Olympus, Tokyo, Japan) revealed a hypoechoic tumor (approximately 7 mm) and local atrophy in the tail of the pancreas. There were no changes in the lesions or other suspicious lesions on CT and MRI scans performed in May 2018.
After admission, the patient’s temperature was 36.4 °C, heart rate was 72 beats per minute, respiratory rate was 16 breaths per minute, blood pressure was 112/60 mmHg, and oxygen saturation in room air was 98%. The physical examination did not reveal any abnormal findings.
The patient was admitted to our hospital for EUS-guided fine needle aspiration (EUS-FNA) for the pancreatic tail tumor. Gastroscopy revealed a suspicious 10 mm lesion in the greater curvature of the gastric antrum, which was confirmed as early gastric cancer (Tub1, 10 mm, M, UL-) by magnifying endoscopy with narrow band imaging and EUS, and as group V adenocarcinoma by pathological biopsy [negative for Helicobacter pylori (HP) antibody]. Thus, it met the indications of endoscopic submucosal dissection (ESD). Colonoscopy revealed no positive findings. Although pancreatic EUS confirmed a 7 mm pancreatic tail tumor, FNA could not be performed despite contrast-enhanced EUS because of its small size and poor reproducibility. Endoscopic retrograde cholangiopancreatography was performed, and the pancreatic juice was collected four times for cytological examination.
The patient was diagnosed with class III cellular atypia. CA19-9 levels continued to increase. Based on the American College of Gastroenterology clinical guidelines[8], we suggested surgical treatment, and her family supported the decision. The patient refused pancreatic surgery but agreed to gastric ESD. In February 2019, we attempted EUS-FNA again, as the lesion had enlarged (15 mm). We were able to successfully obtain a pathological diagnosis following puncture, from which the subsequent ex vivo examinations indicated adenocarcinoma class V.
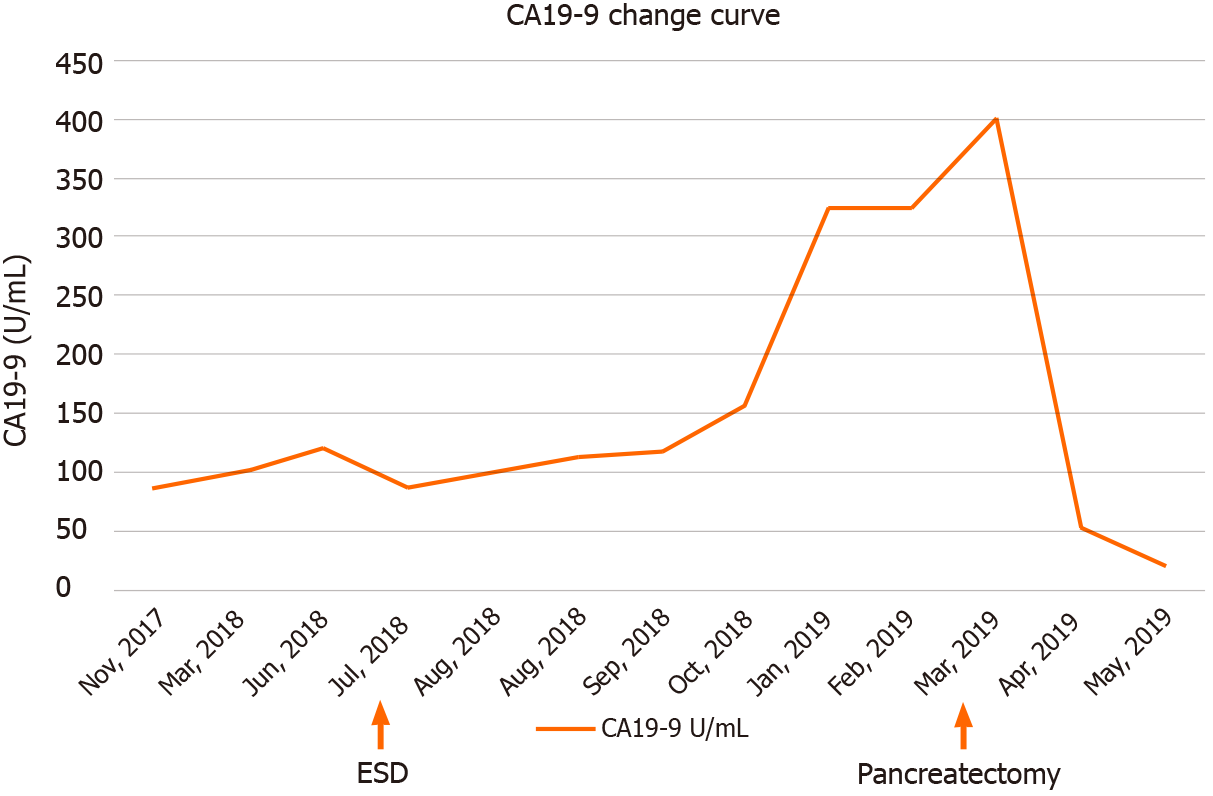
Blood test data on admission are shown in Table 2. The CA19-9 levels before and after treatment are shown in Figure 1.
| Value | Unit | Reference | |
| Blood count | |||
| White blood cells | 3.45 | 103/μL | 3.30-8.60 |
| Red blood cells | 3.54 | 106/μL | 3.86-4.92 |
| Hemoglobin | 11.2 | g/dL | 11.6-14.8 |
| Platelet | 283 | 103/μL | 158-348 |
| Blood coagulation | |||
| Prothrombin time | 11.8 | s | 10-13 |
| International normalized ratio | 1.03 | 0.91-1.14 | |
| Activated partial thromboplastin time | 38.9 | s | 27.0-39.5 |
| Fibrinogen | 327 | mg/dL | 183-349 |
| Biochemical test | |||
| Total protein | 6.6 | g/dL | 6.6-8.1 |
| Albumin | 4.0 | g/dL | 4.1-5.1 |
| Aotal bilirubin | 0.6 | mg/dL | 0.4-1.2 |
| Alkaline phosphatase | 210 | U/L | 106-322 |
| Glutamide transpeptidase | 15 | U/L | 9-32 |
| Lactic dehydrogenase | 214 | U/L | 124-222 |
| Asparatetransaminase | 253 | U/L | 13-30 |
| Alanine aminotransferase | 16 | U/L | 7-30 |
| Blood urea nitrogen | 22.0 | mg/dL | 8-20 |
| Creatinine | 0.80 | mg/dL | 0.46-0.79 |
| C-reactive protein | 0.34 | mg/dL | 0.00-0.14 |
| Natrium | 141 | mmol/L | 138-145 |
| Potassium | 4.12 | mmol/L | 3.6-4.8 |
| Lipase | 60.3 | U/L | 7.1-60 |
| Amylase | 152 | U/L | 44-132 |
| Triglyceride | 48 | mg/dL | 30-149 |
| Blood helicobacter pylori | |||
| Helicobacter pylori | < 3 | U/m | l0-10 |
| Tumor marker | |||
| Carcinoembryonic antigen | 4.5 | ng/mL | 0.0-5.0 |
| Carbohydrate antigen19-9 | 87.95 | U/mL | 0.00-37 |
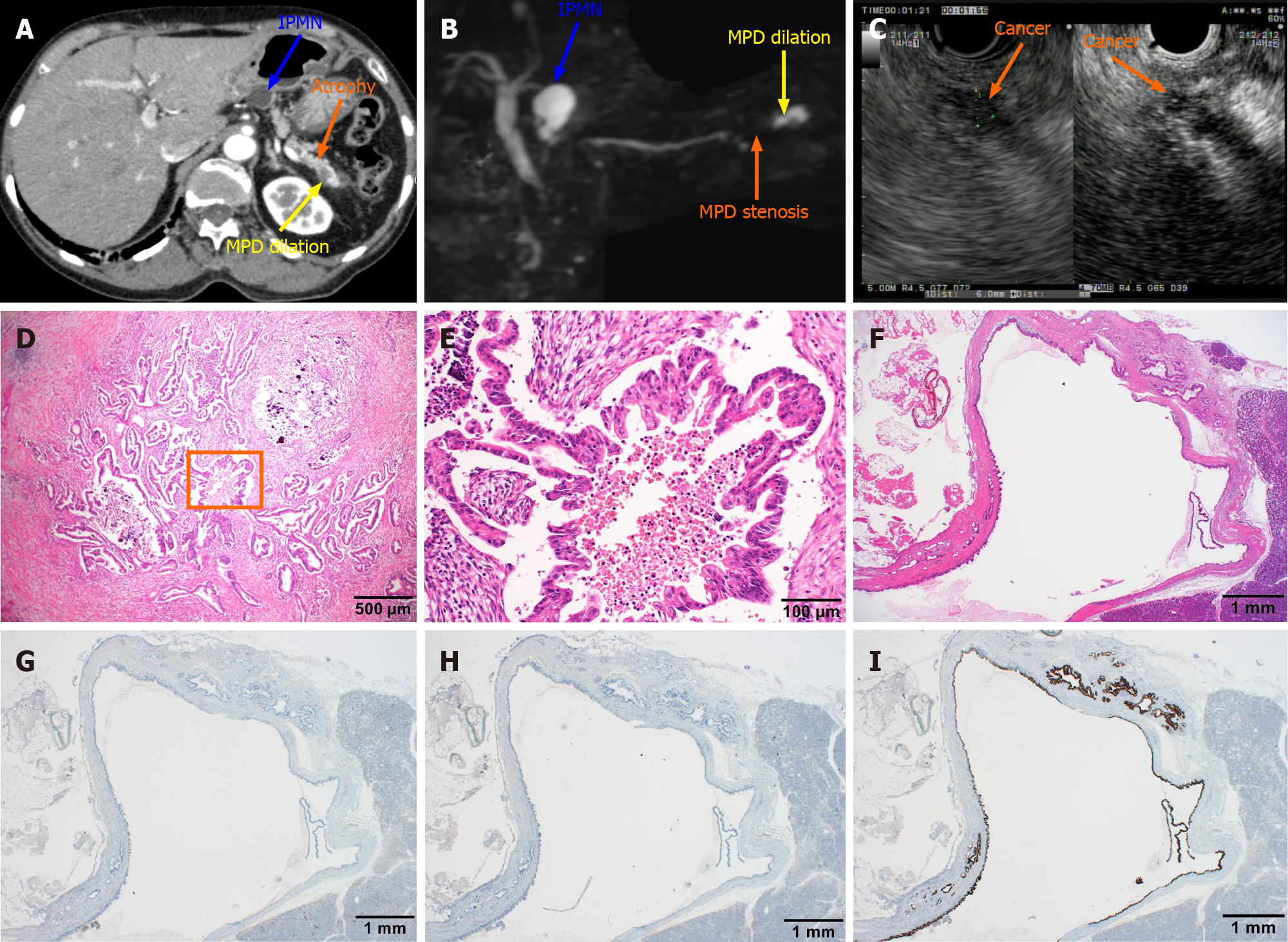
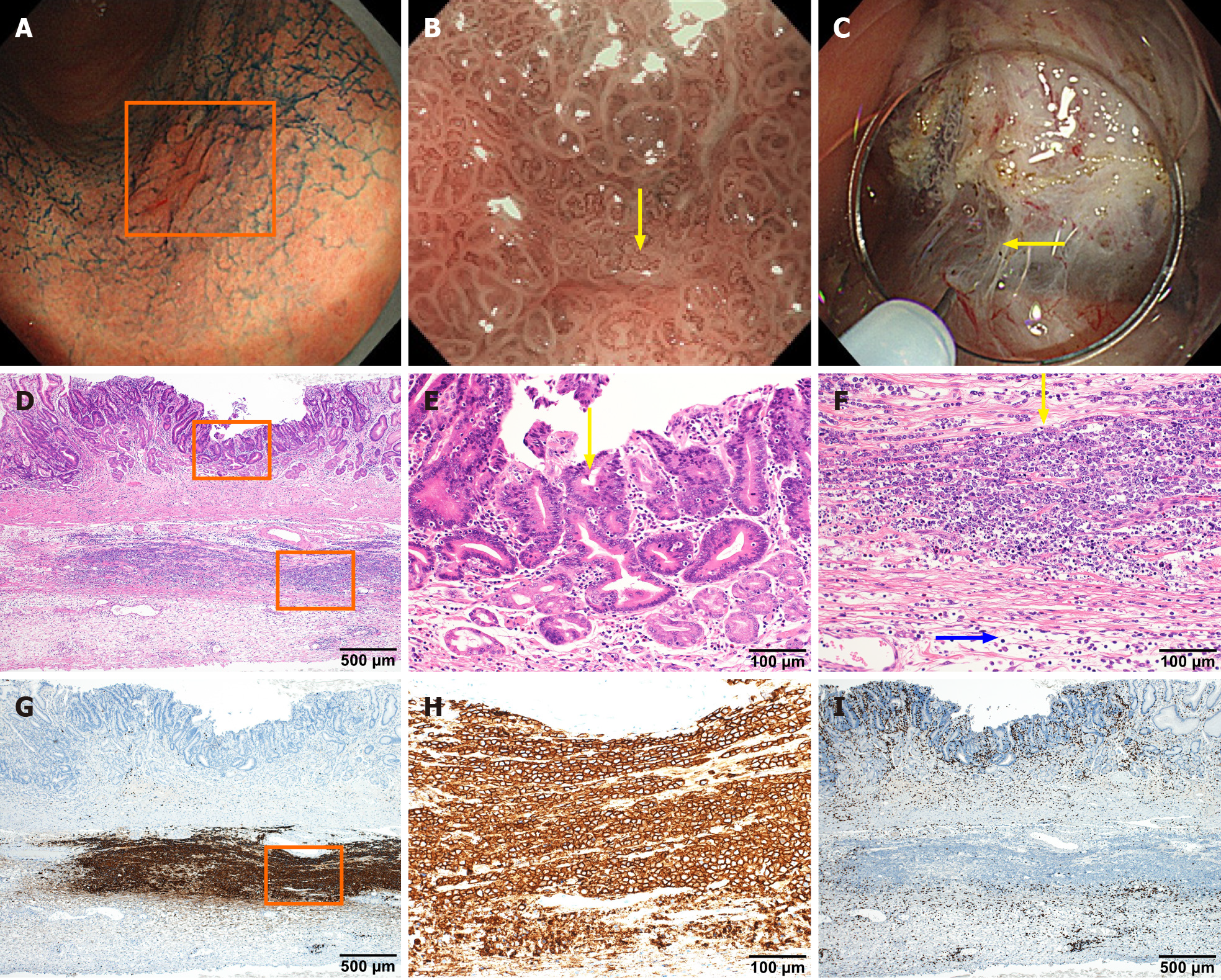
The imaging comparison, pathology, and immunostaining of pancreatic cancer and IPMN are shown in Figure 2. The endoscopic images, pathological examination, and immunostaining of early gastric cancer are shown in Figure 3.
IPMN-synchronized pancreatic cancer with extrapancreatic early gastric cancer and gastric DLBCL.
ESD was performed in July 2018. Intraoperatively, submucosal fibrosis was obvious. The surgeon preferred the submucosal layer to be dissected close to the muscularis propria. Postoperative pathology tests showed well-to-moderately differentiated tubular adenocarcinoma and DLBCL (positive staining of CD20). The ESD samples were further examined by Epstein-Barr encoding region-in situ hybridization, and the result was negative. The patient refused chemotherapy for DLBCL but continued follow-up. At 4 wk post-ESD, the wound developed into a healing ulcer, as observed under gastroscopy, and we collected six biopsies of the surface of the artificial ulcer during the healing stage. Despite the presence of CD20-positive lymphocytes, no large, atypical lymphocyte proliferation was found.
In March 2019, the patient acquiesced to and underwent distal pancreatectomy under laparoscopy for the body and tail tumor. The preoperative CA19-9 level was 400.1 U/mL, and CT and MRI showed no local or distal metastases. The original operation was a pancreatic body and tail resection and splenectomy. Part of the pancreas was removed from 1 cm of the left side of the portal vein. Intraoperative pathology testing confirmed pancreatic cancer, but the broken end was positive. Consequently, another 2 cm of the pancreatic tissue was resected. Further pathological examination, performed intraoperatively, confirmed the new specimens to be pancreatic intraepithelial neoplasia-2 grade and p53-negative. No continuity existed between the main lesion of the pancreatic cancer and IPMN. Postoperative pathological diagnosis included the following: (1) Invasive ductal carcinoma, well > moderate, nodular type; 15 mm × 10 mm; and (2) Intraductal papillary mucinous adenoma, gastric type. Immunostaining results were mucin (MUC) 1(-), MUC2(-), and MUC5AC(+) (Table 3). CA19-9 levels returned to normal 2 mo postoperatively.
Characteristics of IPMN combined with intrapancreatic and extrapancreatic malignant tumor are shown in Table 3.
| Size | Clinical type | Pathologic types | Immunohistochemical | |
| IPMN | 15 mm × 12 mm | BD-IPMN | Gastric type | MUC1(-), MUC2(-), MUC5AC(+) |
| PC | 15 mm × 10 mm | Nodular type | Invasive ductal carcinoma | P53(-) |
| EGC | 15 mm × 11 mm | 0-IIc | Moderately differentiated tubular adenocarcinoma | |
| LM | DLBCL | Diffuse Large B-cell lymphoma | CD20(+), CD(+), EBER-ISH(-) |
CA19-9 levels were normal by 2 mo postoperative. After 18 mo of follow-up, in the absence of chemotherapy, the patient had a good prognosis with no clinical symptoms.
We present herein the case of a patient with IPMN who, at follow-up, showed elevated CA19-9 levels and was found to have pancreatic cancer and in situ collision of early gastric cancer with DLBCL. DLBCL is not generally considered a common extrapancreatic malignant tumor in IPMN[7], much less IPMN combined with two kinds of extrapancreatic malignant tumors, in situ collision of DLBCL, and gastric cancer. Although this patient did not undergo chemotherapy for lymphoma, her prognosis was good, providing an instructive example for aged patients who cannot tolerate chemotherapy.
At the 2-year follow-up visit, initial, routine examinations revealed pancreatic cancer due to elevated CA19-9 levels. EUS indicated a suspicious lesion (size < 1 cm), while CT, MRI, and endoscopic retrograde cholangiopancreatography failed to detect it. Thus, during follow-up of IPMN patients, despite guidelines[8] recommending CT and MRI, EUS is necessary for the earlier detection of small IPMN-related pancreatic tumors, especially when continuous elevations in CA19-9 levels suggest invasive cancer[9]. Therefore, EUS can facilitate early diagnosis and improve prognosis. This patient underwent a 16-mo diagnostic process from the initial detection of increased CA19-9 levels to surgery, and the CA19-9 level increased from 87 to 400.1 U/mL during this period. Finally, EUS-FNA provided diagnostic confirmation because pathology is the gold standard. Timely pathological evaluation during the operation for the nature of the resection margin laid the foundation for the successful outcome.
In invasive pancreatic cancer, a low-echo mass with irregular contour can be seen on EUS, with uneven internal echo and a dilated pancreatic duct in the tail of the pancreas, and cystic lesions can be seen in branched IPMN using EUS, with uniform internal echo and sometimes intramural nodules, which need to be differentiated from mucous thromboembolism. Gastric DLBCL is often accompanied by ulcer formation; morphology similar to early gastric cancer is rare, while most is similar to advanced gastric cancer. Ulcer demarcation line is clear, with smooth uplift of the ulcer boundary.
Pathological analysis is essential to detect these malignant tumors. At high magnification, the pancreatic carcinoma cells show papillary hyperplasia with central necrosis in pancreas biopsy (Figure 2D and E). The histological features of IPMN were also found in pancreatic tissue sections. The cystic lesion is composed of dilated ducts, and the cystic surface is lined with a layer of columnar epithelial cells with basal nuclei showing minimal atypia (Figure 2F). Sequence sections were immunohistochemically stained with antibodies to MUC1 (G), MUC2 (H), and MUC5AC (I), but only MIC5AC was positive (Figure 2G-I).
Histological examination of resected gastric specimen revealed atypical epithelial cells with large nuclei and tubular or papillary proliferation without submucosal invasion (Figure 3D and E). Based on these pathohistological features, the lesion was diagnosed as early gastric adenocarcinoma. Beneath the gastric carcinoma, there was diffuse infiltration of atypical lymphoid cells in the muscular propria (Figure 3D and F). Atypical lymphoid cells (yellow arrow) were large in size compared to normal lymphocytes (red arrow) (Figure 3F). Regarding immunohistochemical staining analysis, brown staining showed that abnormal lymphoid cells positively stained for CD20 (Figure 3G and H) but were negative for CD3 (Figure 3I), suggesting that they are of B-cell origin. Based on these results, she was diagnosed with diffuse large B-cell lymphoma.
HP and Epstein-Barr virus infections are known to play important roles in the synchronous or asynchronous occurrence of primary gastric lymphoma and gastric adenocarcinoma. However, lymphoma-associated HP antibody and Epstein-Barr encoding region-in situ hybridization test results were negative. Some studies[10,11] have shown that HP is highly associated with both synchronous and asynchronous occurrence of mucosa-associated lymphoid tissue lymphoma and gastric adeno-carcinoma; however, the role of Epstein-Barr virus in association with the two malignancies is still debated. Hamaloglu et al[10] found that early gastric cancer is more common (62.5%) in intragastric collision between lymphoma and adenocarcinoma, and most mucosa-associated lymphoid tissue lymphomas (72%-86%) are HP-positive. However, studies involving collisions between primary gastric DLBCL and gastric adenocarcinoma are rare, and few studies have reported HP negativity in patients with collision of primary gastric DLBCL and gastric adenocarcinoma. This suggests that HP is not the main factor in the occurrence of primary gastric DLBCL and gastric adenocarcinoma.
MUC1 expression is associated with tumor progression and lymph node metastases. MUC2 positivity suggests a co-existence of IPMN and gastrointestinal tumors. MUC5AC is expressed in most IPMN patients and is associated with a more favorable prognosis. Immunostaining after pancreatic cancer and IPMN surgery revealed MUC1(-), MUC2(-), and MUC5AC(+) in this patient, who had a comorbid gastrointestinal malignancy and in situ collision between two extrapancreatic malignancies. IPMN combined with pancreatic cancer is more likely to occur in patients with a family history of pancreatic cancer. The breast cancer gene mutation of these patients is also common in extrapancreatic malignant tumors, such as breast cancer, ovarian cancer, and prostate cancer[11]. Three kinds of malignant tumors in one IPMN patient suggest that there may be some relationship between them. Lymphomas are typically larger than adenocarcinomas, suggesting that lymphomas may occur earlier than adenocarcinoma and increase the risk of gastric cancer[11]. Here, we could not verify whether DLBCL occurred before gastric adenocarcinoma. Future studies should investigate the pathogenetic connection between IPMN and the synch-ronous/metachronous occurrence of intra/extrapancreatic malignancies and their interaction.
For this IPMN patient with three different malignancies, choosing the best treatment approach was difficult. We first resected the whole mucosa and submucosa by ESD to confirm the presence of gastric cancer, and during ESD, both the gastric adeno-carcinoma and DLBCL were fully removed. Our patient refused standard DLBCL treatment with chemotherapy; however, there was no recurrence during follow-up, suggesting a good prognosis. Therefore, ESD is a good option for submucosal lymphomas in older patients who cannot tolerate chemotherapy.
The good prognosis and quality of life provided by successful ESD permitted subsequent pancreatic cancer resection. Because of its minimal invasiveness, laparoscopic pancreatectomy was selected, and intraoperative pathologic evaluation of the resection margin was important for its success. In addition, we suggest that during IPMN follow-up, EUS is necessary for earlier detection of small IPMN-related pancreatic tumors.
We thank Dr. Yu-Hui Wang (Health Science Center, Peking University, Beijing, China) for critical reading of the manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Esmaieel S, Wang XB S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | Ohashi K, Murakami Y, Muruayama M. Four cases of "mucin-producing" cancer of the pancreas on specific findings of the papilla of Vater. Prog Dig Endosc. 1982;20:348-352. |
| 2. | Kloppel G, Solcia E, Sobin LH, Longnecker DS, Capella C. Histological typing of tumours of the exocrine pancreas. World Health Organization international classification of tumors. 2nd ed. Berlin: Springer, 1996: 11-20. [DOI] [Full Text] |
| 3. | Benarroch-Gampel J, Riall TS. Extrapancreatic malignancies and intraductal papillary mucinous neoplasms of the pancreas. World J Gastrointest Surg. 2010;2:363-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Panic N, Macchini F, Solito S, Boccia S, Leoncini E, Larghi A, Berretti D, Pevere S, Vadala S, Marino M, Zilli M, Bulajic M. Prevalence of Extrapancreatic Malignancies Among Patients With Intraductal Papillary Mucinous Neoplasms of the Pancreas. Pancreas. 2018;47:721-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Yoon WJ, Ryu JK, Lee JK, Woo SM, Lee SH, Park JK, Kim YT, Yoon YB. Extrapancreatic malignancies in patients with intraductal papillary mucinous neoplasm of the pancreas: prevalence, associated factors, and comparison with patients with other pancreatic cystic neoplasms. Ann Surg Oncol. 2008;15:3193-3198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Oh SJ, Lee SJ, Lee HY, Paik YH, Lee DK, Lee KS, Chung JB, Yu JS, Yoon DS. [Extrapancreatic tumors in intraductal papillary mucinous neoplasm of the pancreas]. Korean J Gastroenterol. 2009;54:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Choi MG, Kim SW, Han SS, Jang JY, Park YH. High incidence of extrapancreatic neoplasms in patients with intraductal papillary mucinous neoplasms. Arch Surg. 2006;141:51-6; discussion 56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts. Am J Gastroenterol. 2018;113:464-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 423] [Article Influence: 60.4] [Reference Citation Analysis (1)] |
| 9. | Fritz S, Hackert T, Hinz U, Hartwig W, Büchler MW, Werner J. Role of serum carbohydrate antigen 19-9 and carcinoembryonic antigen in distinguishing between benign and invasive intraductal papillary mucinous neoplasm of the pancreas. Br J Surg. 2011;98:104-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Hamaloglu E, Topaloglu S, Ozdemir A, Ozenc A. Synchronous and metachronous occurrence of gastric adenocarcinoma and gastric lymphoma: A review of the literature. World J Gastroenterol. 2006;12:3564-3574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991;338:1175-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1293] [Cited by in RCA: 1201] [Article Influence: 35.3] [Reference Citation Analysis (0)] |