Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2386
Peer-review started: December 5, 2020
First decision: January 7, 2021
Revised: January 21, 2021
Accepted: February 1, 2021
Article in press: February 1, 2021
Published online: April 6, 2021
Processing time: 109 Days and 21 Hours
Transcrestal sinus floor elevation (TSFE) has been widely used in the oral clinic when the residual bone height (RBH) exceeds 5 mm. However, when there is insufficient RBH in the posterior maxilla, two-stage TSFE may be an option.
This article introduces the concept of two-stage TSFE. Six patients had osseointegration failure after TSFE. For the first-stage surgery, we restricted the vertical bone augmentation as much as possible. At the second-stage surgery, the increased RBH was 3.28 ± 1.55 mm, which was beneficial for surgery. Five implants functioned successfully on schedule, but one implant failed again during the healing period. A third surgery was performed, and the implant functioned successfully.
When RBH was less than 5 mm, two or more procedures of TSFE might result in a higher RBH.
Core Tip: When the residual bone height is less than 5 mm, two-stage transcrestal sinus floor elevation is a safe technology, which might be an excellent option to embed standard-length implants. Two-stage transcrestal sinus floor elevation could obtain more maxillary sinus membrane elevation height, especially in difficult and complicated cases.
- Citation: Lin ZZ, Xu DQ, Ye ZY, Wang GG, Ding X. Two-stage transcrestal sinus floor elevation-insight into replantation: Six case reports. World J Clin Cases 2021; 9(10): 2386-2393
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2386.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2386
Two decades ago, we could not place implants in an atrophic posterior maxilla due to limited residual bone height (RBH). As a solution to this problem, transcrestal sinus floor elevation (TSFE) has been widely used in the oral clinic, and has been proven to be an effective method for atrophic posterior maxilla[1]. Compared with lateral sinus floor elevation, TSFE is time-saving and economical, and patients experience less trauma after TSFE. Patients may suffer more complications after lateral sinus floor elevation[2]. For doctors, it is easier to master TSFE with the application of new techniques. Nevertheless, if the RBH is less than 5 mm, short implants combined with TSFE is an option to solve this problem[3]. Short implants may be prone to mechanical complications in the long term, and conventional implants are more common in oral clinics. Although TSFE combined with conventional implants could also be applied to a severely atrophic posterior maxilla[4], a higher implant protrusion length might increase the risk of perforation. Therefore, we introduced the concept of two-stage TSFE, which has seldom been mentioned in previous studies[5]. In our research, the implants combined with TSFE, showed adverse events, and another operation was required. The purpose of our study was to introduce the concept of two-stage TSFE.
Six patients (including four men and two women) ranging in age from 25 to 67 years consulted The First Affiliated Hospital of Wenzhou Medical University for prosthetic rehabilitation (Table 1).
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |
| Gender | Woman | Man | Man | Man | Man | Woman |
| Age (yr) | 25 | 54 | 29 | 63 | 46 | 67 |
| Position | 16 | 16 | 26 | 26 | 16 | 26 |
| Smoking | No | Yes | No | Yes | No | No |
| Diabetes | No | No | No | No | No | No |
| First-stage surgery | ||||||
| Bone substitute | Yes, bio-oss | Yes, bio-oss | No | Yes, bio-oss | No | Yes, bio-oss |
| Perforation | No | No | No | No | No | No |
| RBH (mm) | 5.22 | 4.43 | 3.35 | 4.56 | 6.10 | 5.22 |
| Implant (mm) | 4.8 × 10; Straumann | 4.8 × 8; Straumann | 4.8 × 8; Straumann | 4.8 × 10; Straumann | 4.3 × 10; Nobel | 4.8 × 10; Straumann |
| Stability (N·cm) | ≥ 25 | 25 | 15 | ≥ 25 | 15 | 25-35 |
| Failure time | 1 mo | 2 mo | 1 yr | 1 mo | 7 mo | 1 mo |
| Second-stage surgery | ||||||
| Bone substitute | No | No | No | No | No | Yes, bio-oss |
| Perforation | No | No | No | No | No | No |
| RBH (mm) | 11.47 | 8.02 | 6.18 | 7.04 | 8.06 | 9.80 |
| Implant (mm) | 4.8 × 10; Straumann | 4.8 × 10; Straumann | 4.8 × 10; Straumann | 4.8 × 10; Straumann | 4.1 × 10; Straumann | 4.8 × 12; Straumann |
| Stability (N·cm) | 15 | 15 | 15 | ≥ 25 | ≥ 25 | 15 |
| Loading time | 2.5 yr | 2.5 yr | 0 | 2.5 yr | 2.5 yr | 2.5 yr |
| Third-stage surgery | ||||||
| Bone substitute | No | |||||
| Perforation | No | |||||
| RBH (mm) | 6.49 | |||||
| Implant (mm) | 5.0 × 10; Nobel | |||||
| Stability (N·cm) | 25 | |||||
These six patients lost teeth in the posterior maxilla and there was insufficient RBH in the posterior maxilla.
Two patients were smokers, and none had uncontrolled systemic diseases.
Blood analysis of the six patients was performed before surgery, and all results were normal.
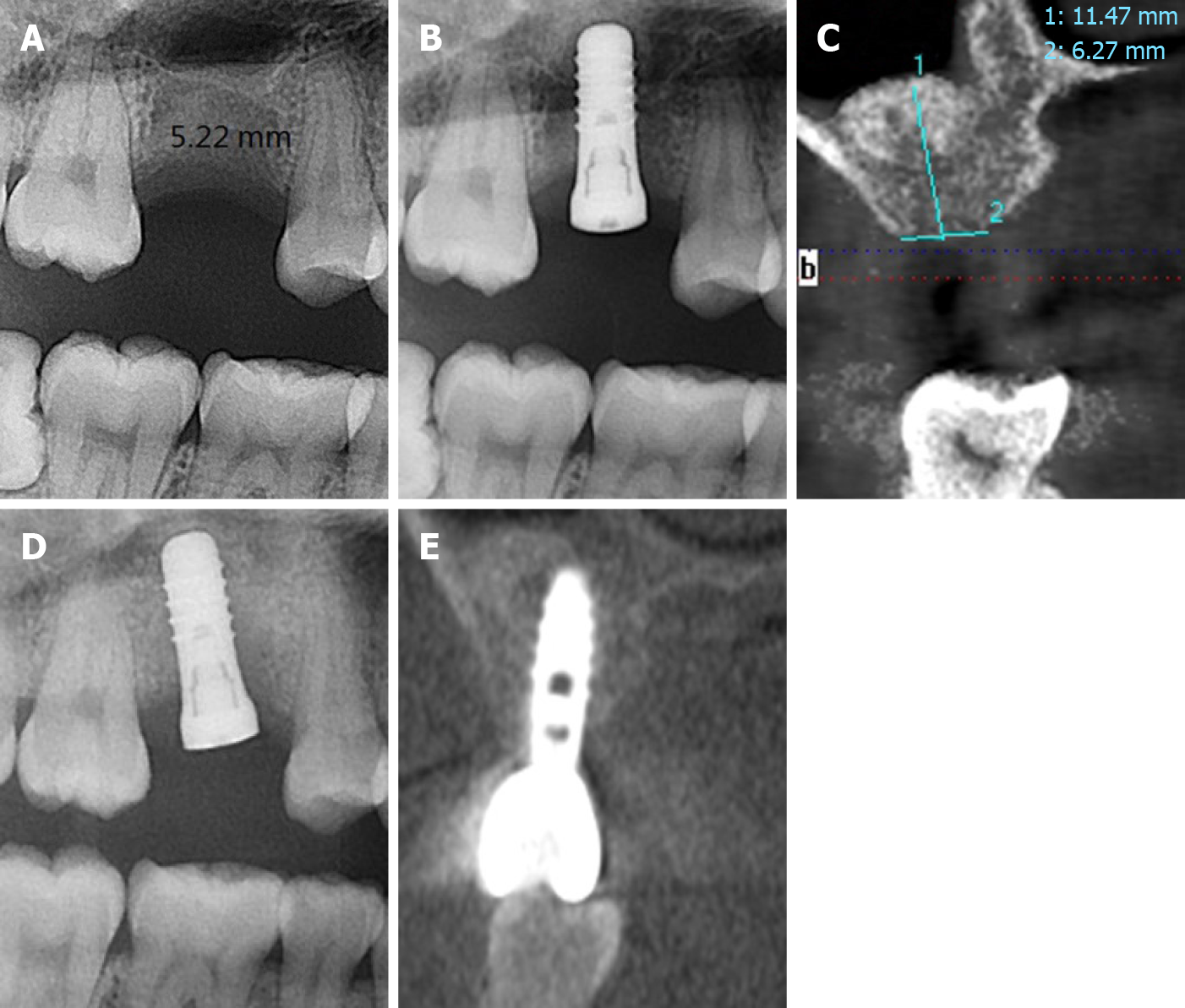
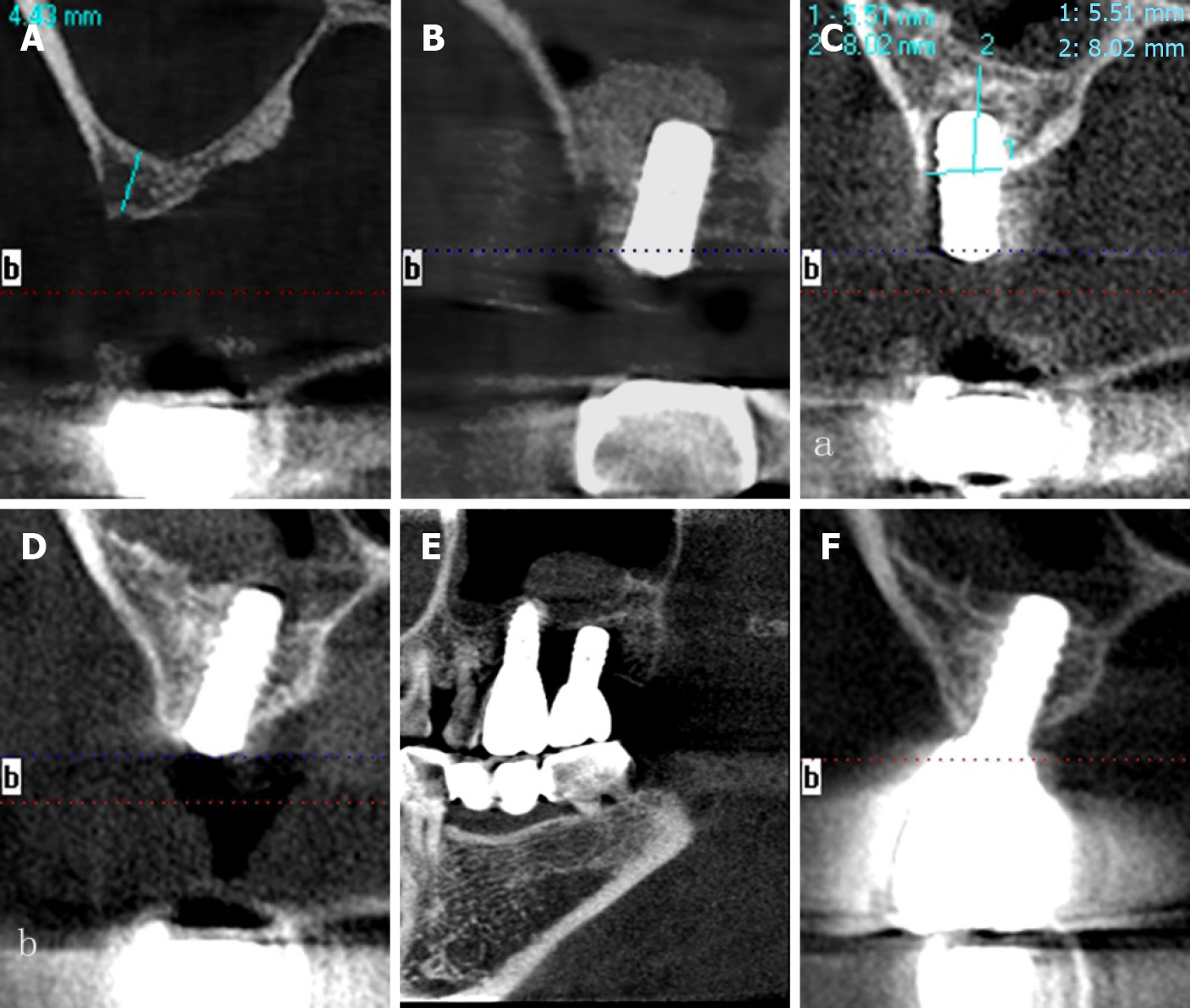
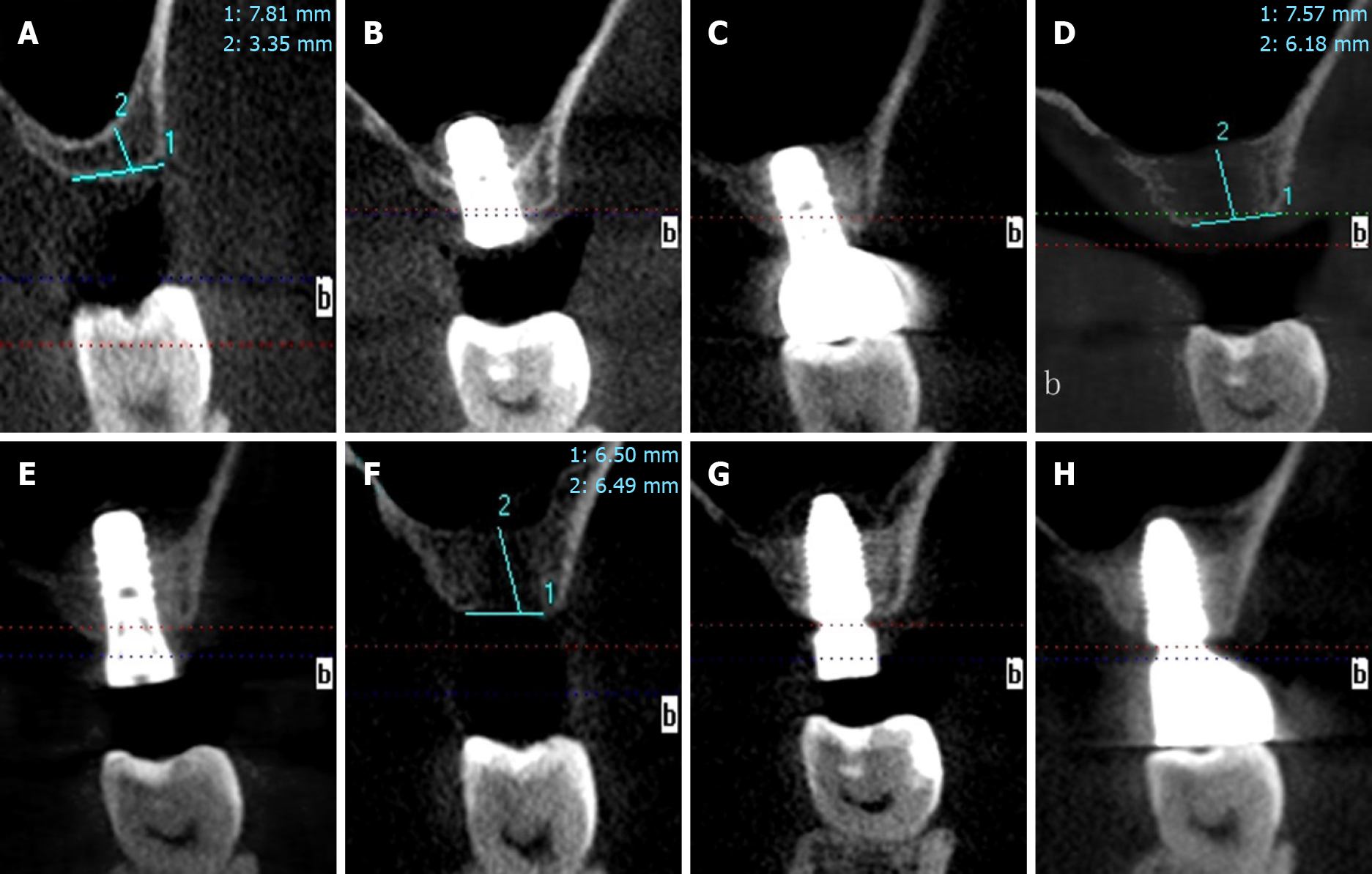
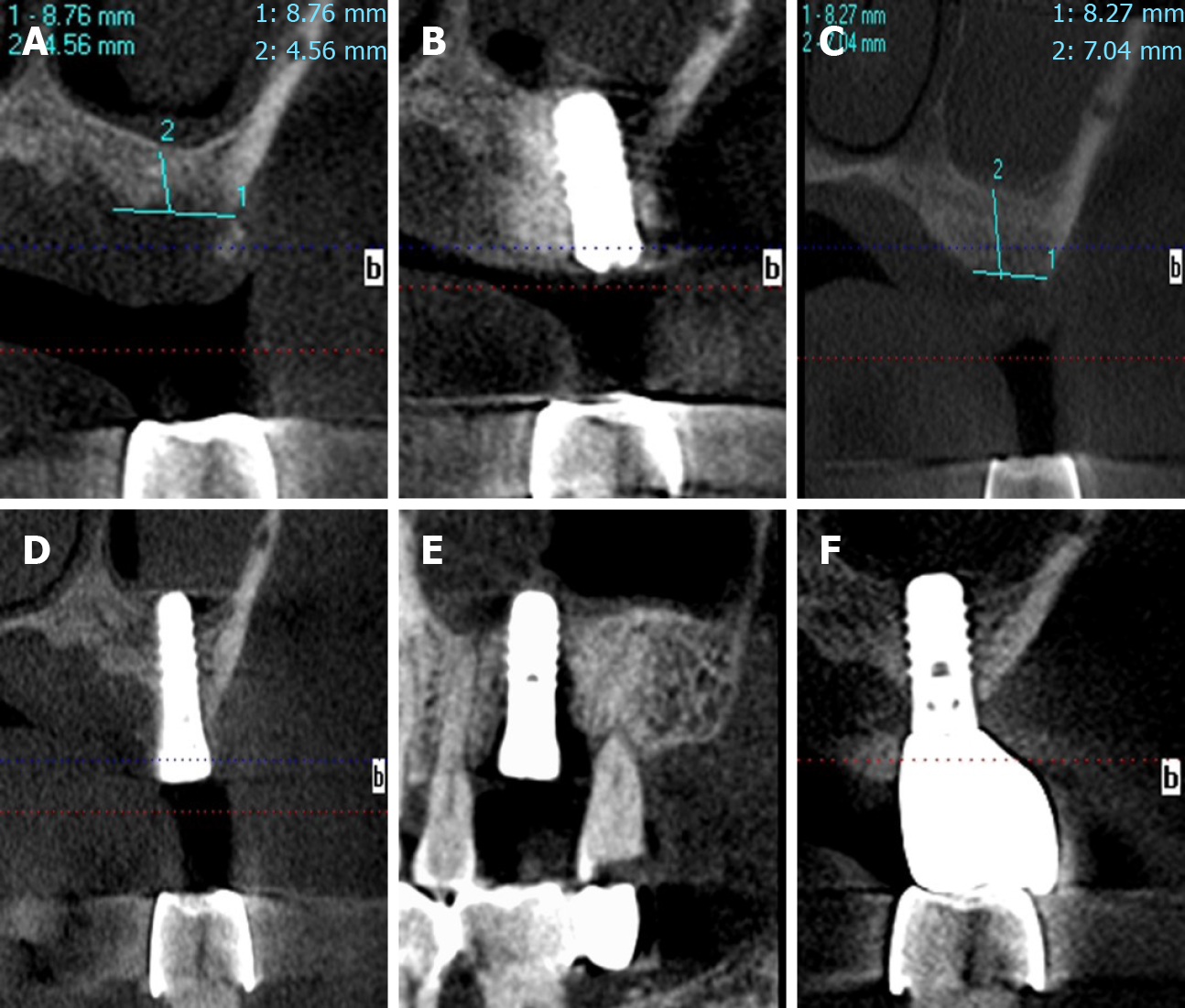
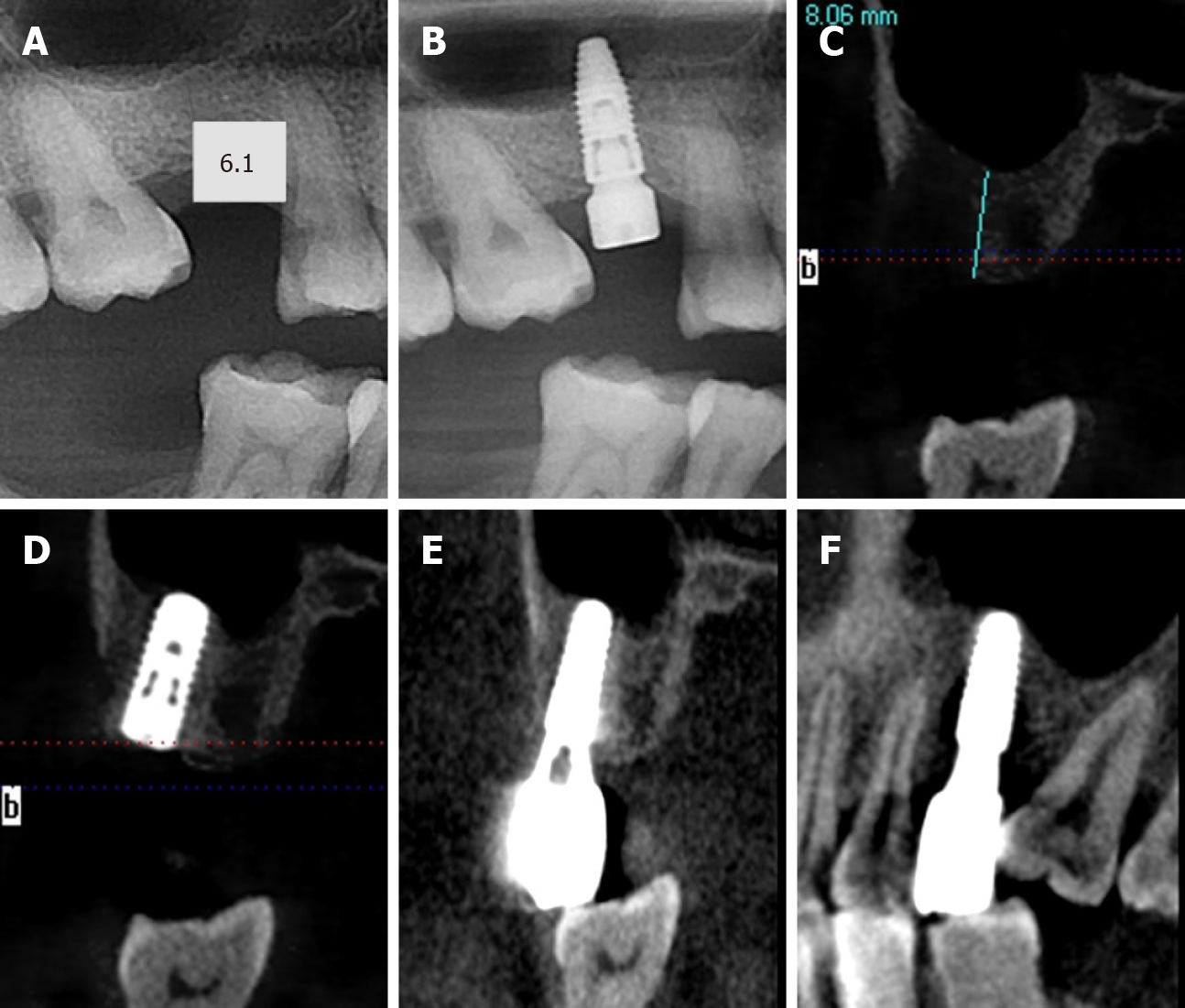
Radiographic and clinical examinations were performed before surgery. Figures 1-5 show that there was insufficient RBH in the posterior maxilla. Interestingly, the RBH in the second surgery was relatively higher than that in the first surgery.
Maxillary dentition defect (insufficient residual bone height in the posterior maxilla).
Two-stage TSFE followed by simultaneous implant placement.
This study followed the Declaration of Helsinki protocols. The RBH in all patients was insufficient, and therefore, TSFE was essential to place a regular implant (implant length = 10 mm). During the operation, TSFE and implants were performed simultaneously. In four cases, we chose 10 mm-long implants, and 8 mm-long implants were used in the other two cases. After the surgery, the patients were prescribed antibiotics and chlorhexidine. We told the patients not to inhale forcefully through the nose and not to swim for a week.
Unfortunately, these six implants were found to be mobile during the healing period or at the 1-year follow-up. Therefore, the failed teeth were extracted.
Another surgery was performed again immediately or after a sufficient healing period, and five of the six implants functioned on schedule (Figures 1-5). We placed five 10 mm-long implants and one 12 mm-long implant in the second-stage surgery. Nevertheless, one implant failed again, and a third surgery was performed. The 10 mm-long implant functioned on schedule after the third surgery.
Table 1 summarizes the main details of the six patients. No perforations occurred in the first-stage and second-stage surgery. In addition, bone material was utilized in four cases. The mean RBH before the first-stage surgery was 4.81 ± 0.93 mm, and the mean RBH before the second-stage surgery was 8.43 ± 1.92 mm. The mean RBH before the second-stage surgery was significantly higher than that before the first-stage surgery (P < 0.05). Functional restoration of five of the six implants was successful. One implant required a third surgery and functioned successfully. Three implants have been loaded for 2.5 years, and the other two implants had been loaded for 1.5 years. These patients were satisfied with implant restoration.
In this study, implants combined with TSFE in the first-stage surgery showed osseointegration failure and the patients were willing to undergo further surgery. The RBH before the second-stage surgery was relatively higher than that before the first operation, which was beneficial for surgery. Five of the implants were successfully loaded. We learned from this procedure that doctors should not consider osseointegration failure of TSFE as negative. Instead, doctors must communicate with patients. If patients would like to undergo further surgery, doctors should be confident about surgery, due to the possibility of a higher RBH.
Knowledge was obtained from the six failed cases of osseointegration, which indicated that two or three TSFE procedures could increase the RBH. We called this procedure “two-stage TSFE or progressive TSFE”, which has rarely been mentioned in previous studies. Therefore, the concept of two-stage TSFE was introduced. Trombelli et al[6] (2015) introduced the concept of “incremental TSFE”, they performed TSFE with graft material in the first stage surgery. Several months later, TSFE was repeated at the molar sites, and conventional implants were simultaneously placed in the sites. This protocol was safe and minimally invasive, decreasing the risk of membrane laceration. Although vertical augmentation greater than 6 mm could also lead to excellent clinical performance with the development of technology[7], the implant protrusion length should be restricted owing to the lower incidence of complications.
The principle of our study was similar to that of the above study[6]. It was accidentally found that the RBH at the sites had increased after osseointegration failure. In the first-stage surgery, we chose a conservative approach as much as possible, and the membrane had the capability of osteogenesis. As a result, the RBH before the second-stage surgery was higher than that before the first-stage surgery.
We should restrict the implant protrusion length in the TSFE (≤ 5 mm), which is a disadvantage of this procedure. The implant protrusion length can exceed 5 mm in the lateral sinus floor elevation, which is considered an advantage of this procedure. However, TSFE is time-saving and less traumatic. Therefore, TSFE has been widely used in oral clinics.
It is known that TSFE has a certain failure rate[8]. Patients may feel disappointed if they encounter osseointegration failure, and they may be afraid of undergoing further surgery. However, osseointegration failure does not mean that the sites cannot be implanted. Above all, we need to respect the opinion of the patients. After a detailed clinical and radiographic assessment, we performed TSFE again and embedded another longer implant, and the clinical performance of the replantation was satisfactory.
Consequently, we concluded that a two-stage TSFE protocol can be selected to embed a standard-length implant if the RBH is less than 5 mm, as the two-stage TSFE could obtain more maxillary sinus membrane elevation height. In the first-stage surgery, the graft materials can be placed after TSFE, which contributed to the second-stage surgery. The latter avoids the relatively complicated operation of lateral window sinus elevation surgery. When the residual bone height is less than 5 mm, two-stage TSFE might be a safe and good choice, and is suitable for general dentistry. The lateral window sinus elevation would cause unnecessary damage to patients and more complications. Nevertheless, the sample size in this study was limited; therefore, studies with a larger sample size are required in the future.
In summary, two-stage transcrestal sinus floor elevation might be an excellent option to embed standard-length implants when the residual bone height is less than 5 mm. In addition, there were limited cases and follow-up time in this study, failure of TSFE should be treated positively, and osseointegration failure could provide a better bone volume, which was beneficial in our implantation.
Manuscript source: Unsolicited manuscript
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH S-Editor: Zhang H L-Editor: Webster JR P-Editor: Liu JH
| 1. | El Hage M, Nurdin N, Abi Najm S, Bischof M, Nedir R. Osteotome Sinus Floor Elevation Without Grafting: A 10-Year Study of Cone Beam Computerized Tomography vs Periapical Radiography. Int J Periodontics Restorative Dent. 2019;39:e89-e97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Stacchi C, Andolsek F, Berton F, Perinetti G, Navarra CO, Di Lenarda R. Intraoperative Complications During Sinus Floor Elevation with Lateral Approach: A Systematic Review. Int J Oral Maxillofac Implants. 2017;32:e107-e118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 3. | Pjetursson BE, Rast C, Brägger U, Schmidlin K, Zwahlen M, Lang NP. Maxillary sinus floor elevation using the (transalveolar) osteotome technique with or without grafting material. Part I: Implant survival and patients' perception. Clin Oral Implants Res. 2009;20:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Chaushu L, Chaushu G, Better H, Naishlos S, Kolerman R, Aragoneses JM, Calvo-Guirado JL, Nissan J. Sinus Augmentation with Simultaneous, Non-Submerged, Implant Placement Using a Minimally Invasive Hydraulic Technique. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Franceschetti G, Farina R, Stacchi C, Di Lenarda R, Di Raimondo R, Trombelli L. Radiographic outcomes of transcrestal sinus floor elevation performed with a minimally invasive technique in smoker and non-smoker patients. Clin Oral Implants Res. 2014;25:493-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Trombelli L, Franceschetti G, Trisi P, Farina R. Incremental, transcrestal sinus floor elevation with a minimally invasive technique in the rehabilitation of severe maxillary atrophy. Clinical and histological findings from a proof-of-concept case series. J Oral MaxillofacSurg. 2015;73:861-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Better H, Chaushu L, Nissan J, Xavier S, Tallarico M, Chaushu G. The Feasibility of Flapless Approach to Sinus Augmentation Using an Implant Device Designed According to Residual Alveolar Ridge Height. Int J Periodontics Restorative Dent. 2018;38:601-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Călin C, Petre A, Drafta S. Osteotome-mediated sinus floor elevation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014;29:558-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |