Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2380
Peer-review started: December 10, 2020
First decision: January 17, 2021
Revised: January 18, 2021
Accepted: January 27, 2021
Article in press: January 27, 2021
Published online: April 6, 2021
Processing time: 109 Days and 6.5 Hours
Solitary bone plasmacytoma (SBP) of the upper cervical spine is a rare diagnosis. The exact role of surgery for SBP remains unclear.
We present the first case of SBP of the C2. A 69-year-old Chinese woman presented with severe neck pain and limitation of rotative activity for 2 mo. She underwent anterior one-stage debridement combined with cement augmentation in the C2 to reconstruct stability of the spine. The patient did not receive postoperative radiotherapy. She now remains disease free with no neck pain or neurological deficit after follow-up of 3 years.
Anterior one-stage debridement combined with cement augmentation of the upper cervical spine may be an alternative treatment for SBP.
Core Tip: We present a case of solitary bone plasmacytoma on the C2 with follow-up of 3 years. The patient underwent anterior one-stage debridement combined with cement augmentation. The results of this case provide a choice for surgical treatment of solitary bone plasmacytoma. They also show that radical surgery without radiotherapy is a rational choice for treating solitary bone plasmacytoma with spinal instability.
- Citation: Li RJ, Li XF, Jiang WM. Solitary bone plasmacytoma of the upper cervical spine: A case report . World J Clin Cases 2021; 9(10): 2380-2385
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2380.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2380
Multiple myeloma (MM) presents as a malignant tumor with abnormal proliferation of plasma cells with major clinical manifestations of anemia, bone pain, hypercalcemia and renal insufficiency. When myeloma cells infiltrate the bone marrow, the balance of bone resorption and destruction is destroyed. It commonly affects the spine, presenting as either a solitary plasmacytoma or part of a systemic disease. The level of the cervical spine is the location of 10%-17% of neoplastic disease of the vertebral column, including MM[1]. Solitary bone plasmacytoma (SBP) is defined as a localized tumor in the bone comprised by a single clone of plasma cells. The diagnosis of SBP is currently based on histopathological examination through tissue biopsy and radiological confirmation[2]. SBP is a rare diagnosis for which the primary treatment is local radiotherapy. The exact role of surgery for SBP remains unclear[3-5]. Although MM is a common disease when compared to other plasma cell neoplasms, SBP in the vertebral body is a rare condition with little published literature[3]. Meanwhile, the upper cervical spine (C1/2) has a unique function and biomechanical and anatomical characteristics. Lesions in this region mainly present with pain from instability rather than neurological deficit from cord compression.
Here, we report a 69-year-old woman with SBP of the upper cervical spine to improve our understanding of the clinical manifestations and to report successful radical surgery of SBP.
A 69-year-old Chinese woman presented with severe neck pain and limitation of rotative activity for 2 mo.
The patient noticed intermittent neck discomfort 10 years ago, which improved after rest and became aggravated after activity. Two months ago, the neck pain aggravated suddenly.
The patient complained about neck discomfort for > 10 years but did not go to the hospital or take any medication. There was no significant change in body weight for 10 years.
She denied any personal or family history of other diseases.
Physical examination revealed localized tenderness on the cervical spine. The strength of both upper limbs was normal, while the sensation of both hands decreased. No sensory loss of the lower extremities was noted, and muscular tension was normal. Pathological signs were negative, and no hyperactivity of tendon reflex was found. The spinal instability neoplastic score was 8.
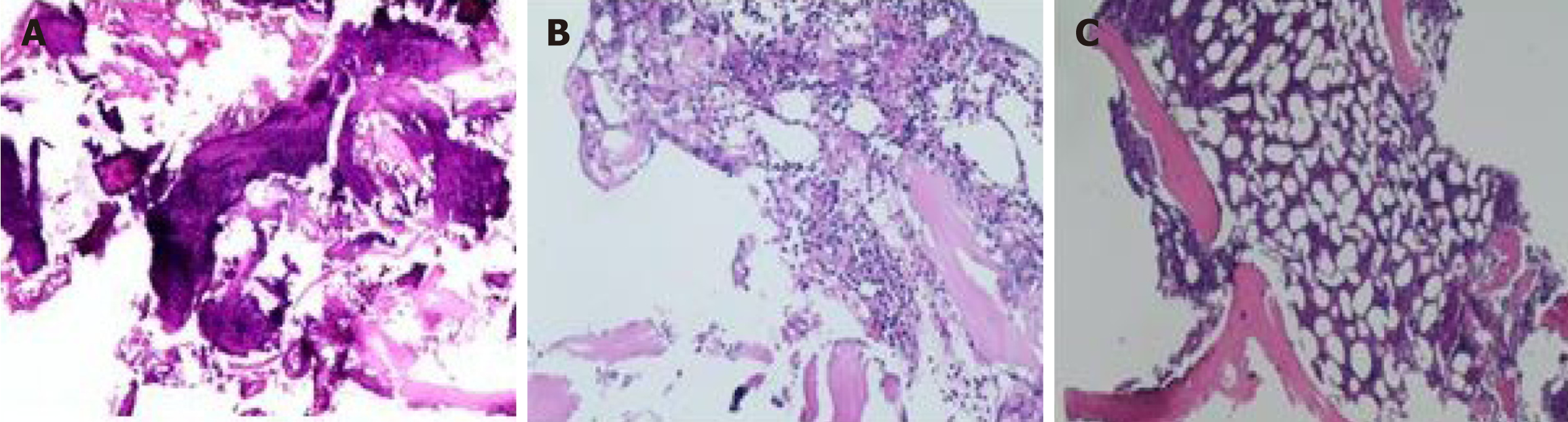
Hemoglobin, calcium and creatinine were normal. C2 biopsy showed multilobe mature plasma cells with no histopathology. No tumor cells were found in the bone marrow 1 year postoperatively (Figure 1).
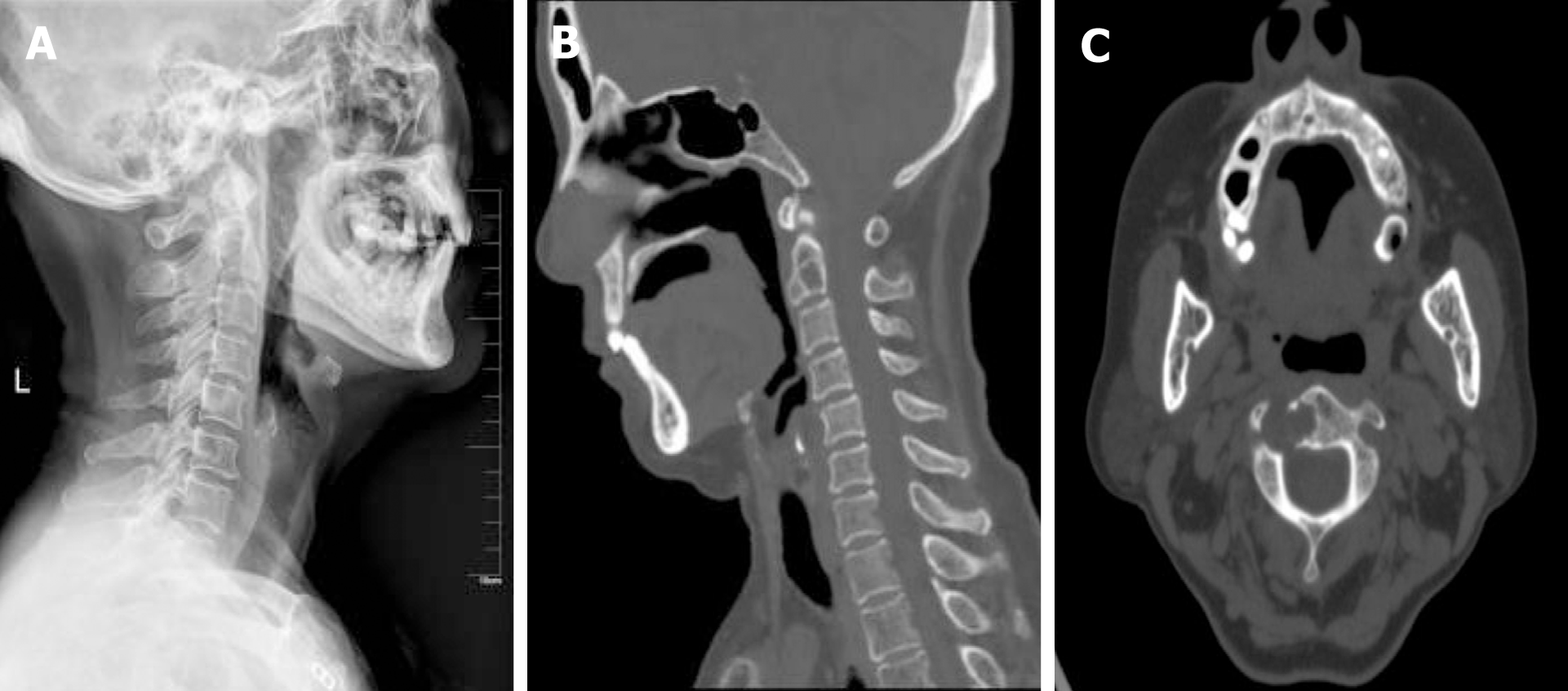
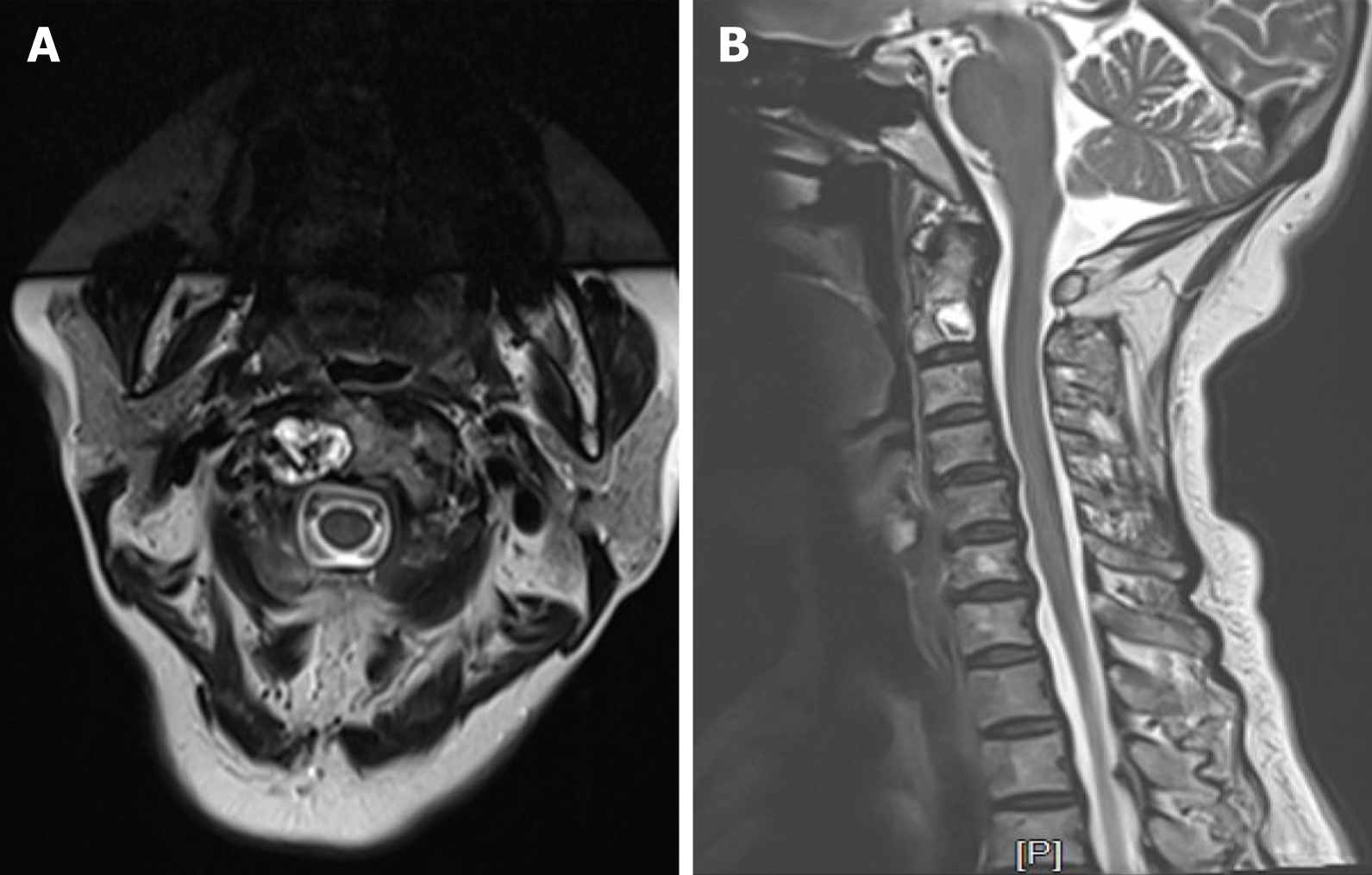
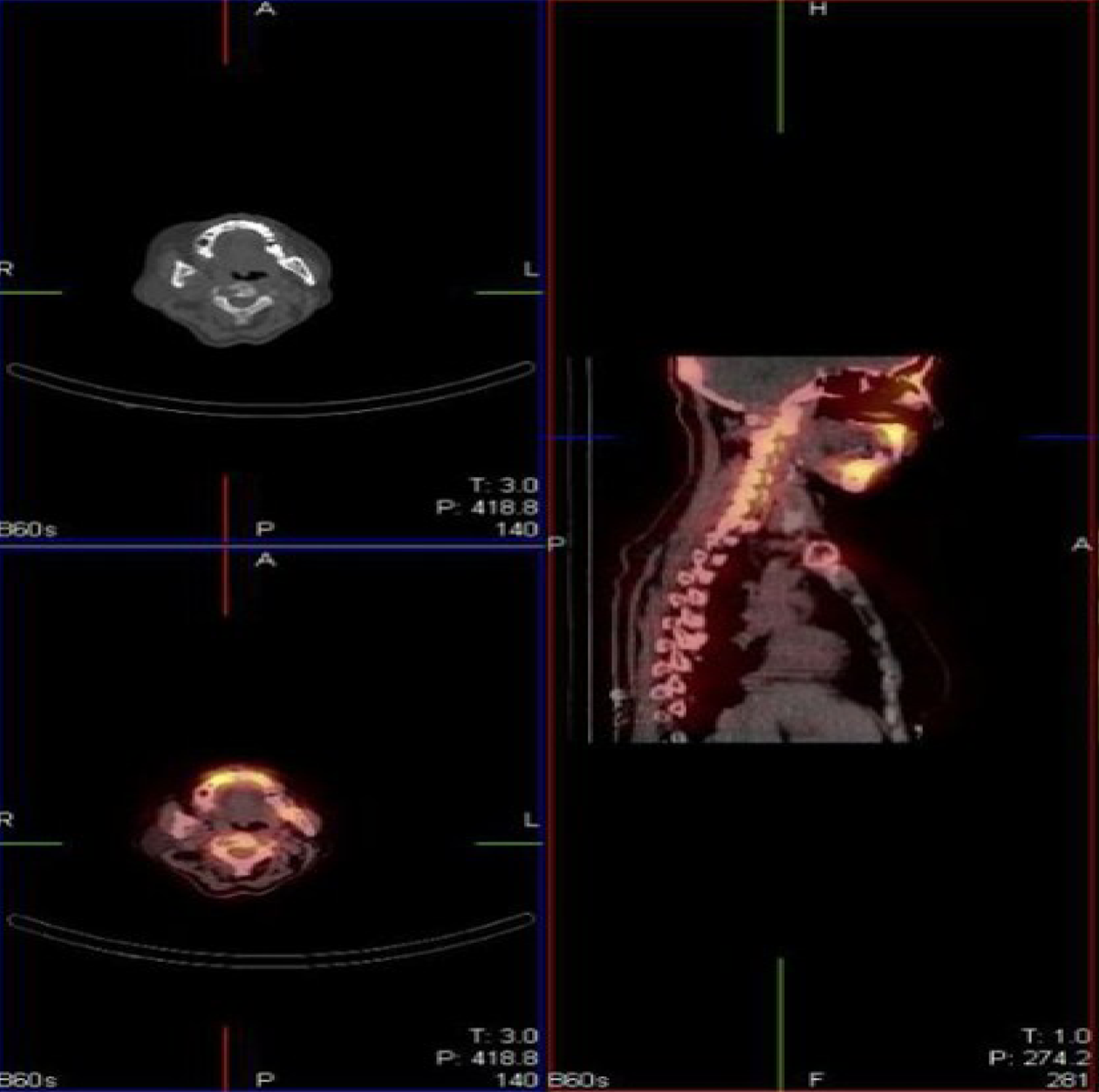
X-rays showed mild cervical kyphosis and cystic lesions in (CK1) C2. Computed tomography (CT) reconstruction revealed bone destruction in the pedicle of C2 with absence of the posterior wall. Magnetic resonance imaging showed a high signal mass on the right side of the C2 with clear margin. No lymph node metastasis was found in the magnetic resonance imaging. Cervical disc herniation could be found in C4-6, while no garrulous blade or swollen discs were observed toward the spinal cord in C2 (Figure 2 and 3). Single photon emission CT/CT showed high bright signal intensity in C2 and the teeth (Figure 4).
According to clinical symptoms, imaging findings and postoperative biopsy, SBP was diagnosed.
CT revealed severe bone destruction in the (CK1) C2, causing instability of the cervical spine. The patient was asked to wear a neck brace and forbidden to get out of bed. She underwent anterior one-stage debridement combined with cement augmentation in C2 to reconstruct stability of the spine. Methylprednisolone was given intravenously in the first 3 d after surgery, and dexamethasone was used in the last 4 d. The patient was reviewed in the hematology department every 6 mo. This patient did not receive postoperative radiotherapy.
The cervical activity of the patient was restored to normal, and neck pain was significantly relieved. Postoperative X-rays and CT showed that the bone cement filled well, and no leakage occurred during the 3 years of follow up (Figure 5). X-rays showed good stability, and the patient remained disease free with no neurological deficit at 3 years postoperatively. The serum markers of MM were normal at the 3-year follow-up.
In patients with plasma cell dysplasia, SBP is a rare condition with a cumulative incidence of 5%[6]. As long as there is initial bone involvement, it can still be classified as SBP, even if soft tissue extension occurs[7]. SBP can be diagnosed by biopsy demonstrating monoclonal plasma cell infiltration of a single lesion. The median age at diagnosis of SBP is 10 years younger than that of MM[3]. To date, the treatment choices of tumors in the upper cervical spine are controversial, especially in terms of the surgical approaches, extent and reconstruction. The most common symptom may be pain, but other neurological symptoms may be caused by nerve compression[8-10].
Molloy et al[4] reported that treatment of SBP involving the spine is medical, including radiotherapy, chemotherapy or both modalities. However, instability is the main reason for pain, which can only be relieved completely by surgery. Yang et al[11] recommended aggressive resection of upper cervical spine tumor to reduce mortality. Huang et al[12] reported four cases of cervical SBP that showed unsatisfactory outcomes after surgical treatment due to spinal instability and neurological deficits in the cervical spine. They demonstrated that the vertebral body was reconstructed by a titanium mesh cage filled with iliac crest combined with an anterior titanium plate for lesions in the (CK1) C2. Von der Hoeh et al[3] reported that surgery combined with radiotherapy are necessary because of spinal instability in SBP. They demonstrated that total spondylectomy and postoperative radiotherapy minimized the risk of local recurrence and reduced the risk of conversion to MM. Molloy et al[4] argued that spinal stability was not an issue in SBP because the vertebral body had compensated for the osteolytic defects by thickening its cortices. Some researchers[13-15] believe that the posterior approach is preferred for this region, and lesions of C1 or C2 are needed to be fused into the occiput for the spinal stability (CK2)[3].
To date, the recommended treatment of SBP is local radiotherapy without surgery. However, CT reconstruction revealed bone destruction in the C2 (CK4) with absence of the posterior wall and involvement of the pedicle (CK5), and adjuvant therapy cannot maintain the spinal stability. Once neck trauma occurs, it can easily lead to cervical cord compression. Generally speaking, adjuvant therapy such as radiotherapy should be carried out after surgery rather than before. Von der Hoeh et al[3] reported a similar case in 2014 with the diagnosis of SBP with a 1 year history of low back pain. He chose to perform a total spondylectomy in the lumbar spine. Postoperative local radiotherapy was performed with the rationale of improving the prognosis regarding local recurrence and decreasing the risk of progression to MM. After 4 years of follow-up, laboratory and imaging diagnostics showed no pathologic recurrence. In the present case, the spinal instability neoplastic score was 8, and surgical intervention is recommended when the score ranges from 7 to 18[16]. The patient underwent anterior one-stage debridement combined with cement augmentation, with the advantages of less trauma and blood loss. A definitive surgical excision alone was considered because of the small size of the tumor and a clear margin. In addition, no lymph node metastases were found in the magnetic resonance imaging.
Meanwhile, the patient’s own decision was necessary for the choice of treatment. After the surgery, the shape of the vertebral body and immediate spinal stability were restored by filling with bone cement. Temperature elevation caused by bone cement played a role in the destruction of tumor cells[17]. It can be seen that no leakage of bone cement occurred, and the shape of the C2 was maintained. Normal laboratory examinations indicated no pathological recurrence or progression to MM. This case provides evidence that surgical treatment of SBP can be successful and shows that radical surgery without radiotherapy is a rational choice for treating SBP with spinal instability. However, follow-up of 3 years is limited and further follow-up is needed.
Anterior one-stage debridement combined with cement augmentation without radiotherapy of the upper cervical spine may be an alternative choice for treatment of SBP.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Decker S S-Editor: Fan JR L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Cawley DT, Butler JS, Benton A, Altaf F, Rezajooi K, Kyriakou C, Selvadurai S, Molloy S. Managing the cervical spine in multiple myeloma patients. Hematol Oncol. 2019;37:129-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, Samson D; Working Group of the UK Myeloma Forum; British Committee for Standards in Haematology; British Society for Haematology. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol (R Coll Radiol). 2004;16:405-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 118] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | von der Hoeh NH, Tschoeke SK, Gulow J, Voelker A, Siebolts U, Heyde CE. Total spondylectomy for solitary bone plasmacytoma of the lumbar spine in a young woman: a case report and review of literature. Eur Spine J. 2014;23:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Molloy S, Kyriakou C. Expert's comment concerning Grand Rounds case entitled "total spondylectomy for solitary bone plasmacytoma of the lumbar spine in a young woman. A case report and review of the literature" (by N. von der Hoeh, S.K. Tschoeke, J. Gulow, A. Voelker, U. Siebolts and C.-E. Heyde). Eur Spine J. 2014;23:40-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1662] [Cited by in RCA: 1510] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 6. | Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992-2004. Br J Haematol. 2009;144:86-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 179] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 7. | Pham A, Mahindra A. Solitary Plasmacytoma: a Review of Diagnosis and Management. Curr Hematol Malig Rep. 2019;14:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 8. | Phillips E, Levine AM. Metastatic lesions of the upper cervical spine. Spine (Phila Pa 1976). 1989;14:1071-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Nakamura M, Toyama Y, Suzuki N, Fujimura Y. Metastases to the upper cervical spine. J Spinal Disord. 1996;9:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, Grejs A, Harms J, Kawahara N, Mazel C, Melcher R, Tomita K. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? J Neurosurg Spine. 2008;8:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 218] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 11. | Yang J, Jia Q, Peng D, Wan W, Zhong N, Lou Y, Cai X, Wu Z, Zhao C, Yang X, Xiao J. Surgical treatment of upper cervical spine metastases: a retrospective study of 39 cases. World J Surg Oncol. 2017;15:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Huang W, Cao D, Ma J, Yang X, Xiao J, Zheng W, Feng D, Wu Z, Huang Q, Chen D, Jia L. Solitary plasmacytoma of cervical spine: treatment and prognosis in patients with neurological lesions and spinal instability. Spine (Phila Pa 1976). 2010;35:E278-E284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Rao G, Ha CS, Chakrabarti I, Feiz-Erfan I, Mendel E, Rhines LD. Multiple myeloma of the cervical spine: treatment strategies for pain and spinal instability. J Neurosurg Spine. 2006;5:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Ahmadi SA, Slotty PJ, Munoz-Bendix C, Steiger HJ, Cornelius JF. Early surgical occipitocervical stabilization for plasma cell neoplasms at the craniocervical junction: systematic review and proposal of a treatment algorithm. Spine J. 2016;16:91-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Delank KS, Wendtner C, Eich HT, Eysel P. The treatment of spinal metastases. Dtsch Arztebl Int. 2011;108:71-9; quiz 80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, Harrop JS, Fehlings MG, Boriani S, Chou D, Schmidt MH, Polly DW, Biagini R, Burch S, Dekutoski MB, Ganju A, Gerszten PC, Gokaslan ZL, Groff MW, Liebsch NJ, Mendel E, Okuno SH, Patel S, Rhines LD, Rose PS, Sciubba DM, Sundaresan N, Tomita K, Varga PP, Vialle LR, Vrionis FD, Yamada Y, Fourney DR. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35:E1221-E1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 996] [Cited by in RCA: 778] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 17. | Deramond H, Wright NT, Belkoff SM. Temperature elevation caused by bone cement polymerization during vertebroplasty. Bone. 1999;25:17S-21S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 216] [Article Influence: 8.3] [Reference Citation Analysis (0)] |