Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2352
Peer-review started: November 25, 2020
First decision: December 8, 2020
Revised: December 15, 2020
Accepted: December 28, 2020
Article in press: December 28, 2020
Published online: April 6, 2021
Processing time: 125 Days and 5 Hours
Primary intramedullary melanoma is a very rare tumor, most frequently occurring in the cervical and thoracic spinal cord.
We present a rare case in which the primary intramedullary melanoma was located in the lumbar spine. A 56-year-old man complained of progressive intermittent pain in the lumbar area. Thoracic magnetic resonance imaging showed a spinal intramedullary tumor between the L3 and S1 levels. The tumor was resected entirely, and the diagnosis of malignant melanoma was confirmed by histopathology.
Primary melanoma of the spinal cord, particularly intramedullary localization, has rarely been reported in the previous literature. We describe a primary malignant melanoma of the lumbar spinal cord and discuss the challenges associated with the diagnosis.
Core Tip: We report a primary malignant melanoma of the lumbar spinal cord and emphasize the diagnostic challenge.
- Citation: Sun LD, Chu X, Xu L, Fan XZ, Qian Y, Zuo DM. Primary intramedullary melanoma of lumbar spinal cord: A case report. World J Clin Cases 2021; 9(10): 2352-2356
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2352.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2352
Primary malignant melanoma of the central nervous system (CNS) accounts for about 1% of all melanoma cases[1]. Primary CNS melanoma localized to the spinal cord is extremely rare, and most frequently involves the thoracic spine and the cervical spine. The diagnosis of primary intramedullary melanoma was based on histological examination and the exclusion of other lesions outside of the CNS[2,3]. In this paper, we present the case of a 56-year-old male patient diagnosed with primary intramedullary melanoma of the lumbar spine that proceeded with surgical resection.
A 56-year-old man visited our hospital with radiating pain in the lower limbs for 2 wk.
The patient had been suffering from progressive intermittent pain in the lumbar area for approximately 3 years, and his pain was only partially relieved after bed rest. He then began to feel severe radiating pain in the left lower limb 2 wk before presentation.
The patient had mild kyphosis of the spine and intervertebral tenderness in the L4-L5 and L5-S1 disc spaces. Physical examination showed left hip tenderness and percussion pain. The muscles of the left lower limb were significantly atrophied relative to the right lower limb. Resultantly, the left lower limb was observed to be 3 cm shorter than the right one.
A Faber test of the left lower limb was positive. Straight leg elevation tests of both lower extremities were negative. Pain sensation and temperature sensation were normal in both lower limbs. Muscle tension in both lower extremities was also normal.
Dorsiflexion force of the left ankle joint was 3+, and plantar flexor muscle strength was level 3. The nail of the big toe was grade 0. Right ankle dorsiflexor force was 4, and plantar flexor force was 5. The anal sphincter contracted evenly and forcefully. Bilateral knee and Achilles tendon reflexes were normal. The physiological reflex was present, but the pathological reflex was not elicited.
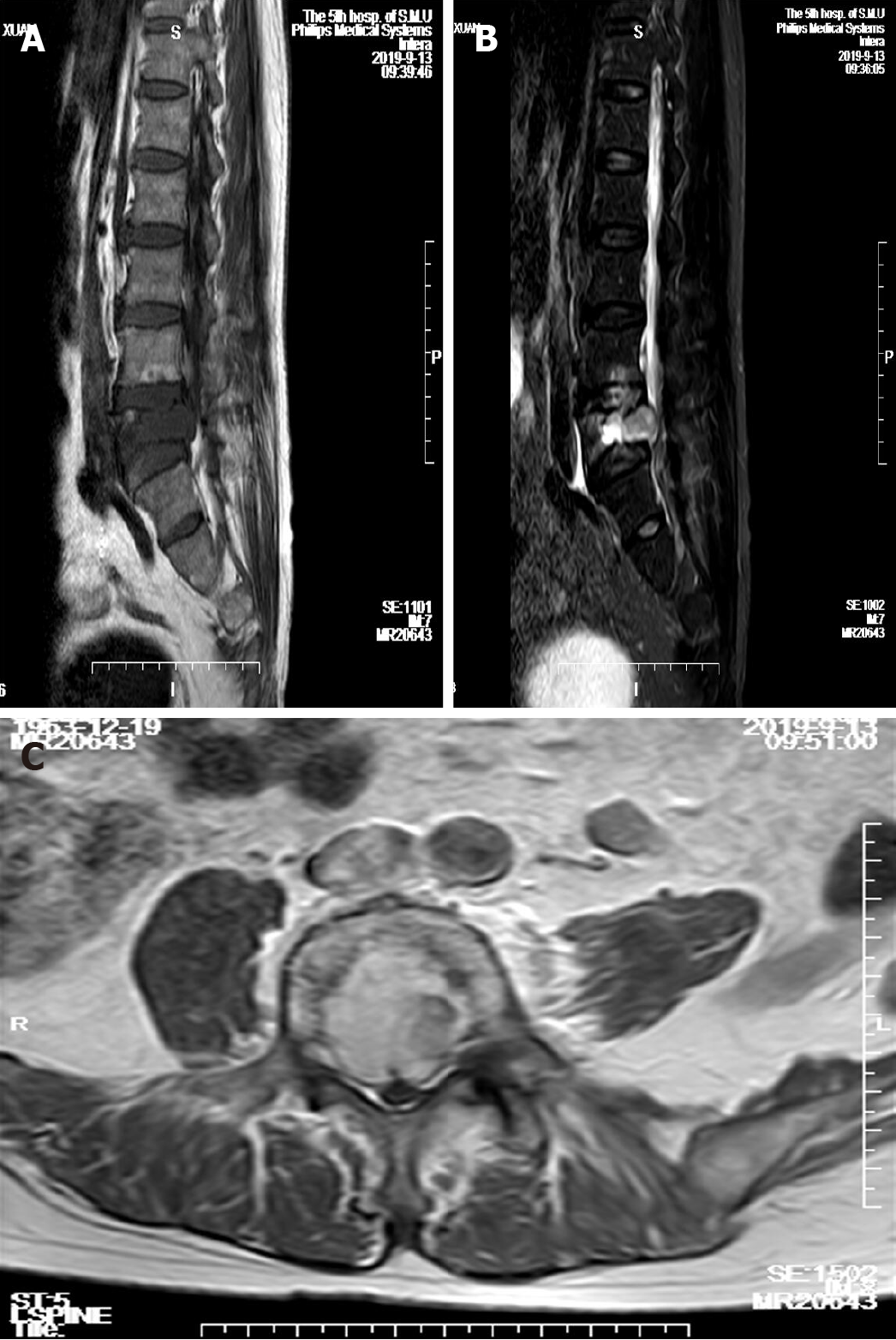
Magnetic resonance imaging (MRI) analysis of the lumbar spine exhibited an intramedullary mass between the L3 and S1 levels. An impressive Schmorl node was visible in the L4 vertebral body (Figure 1).
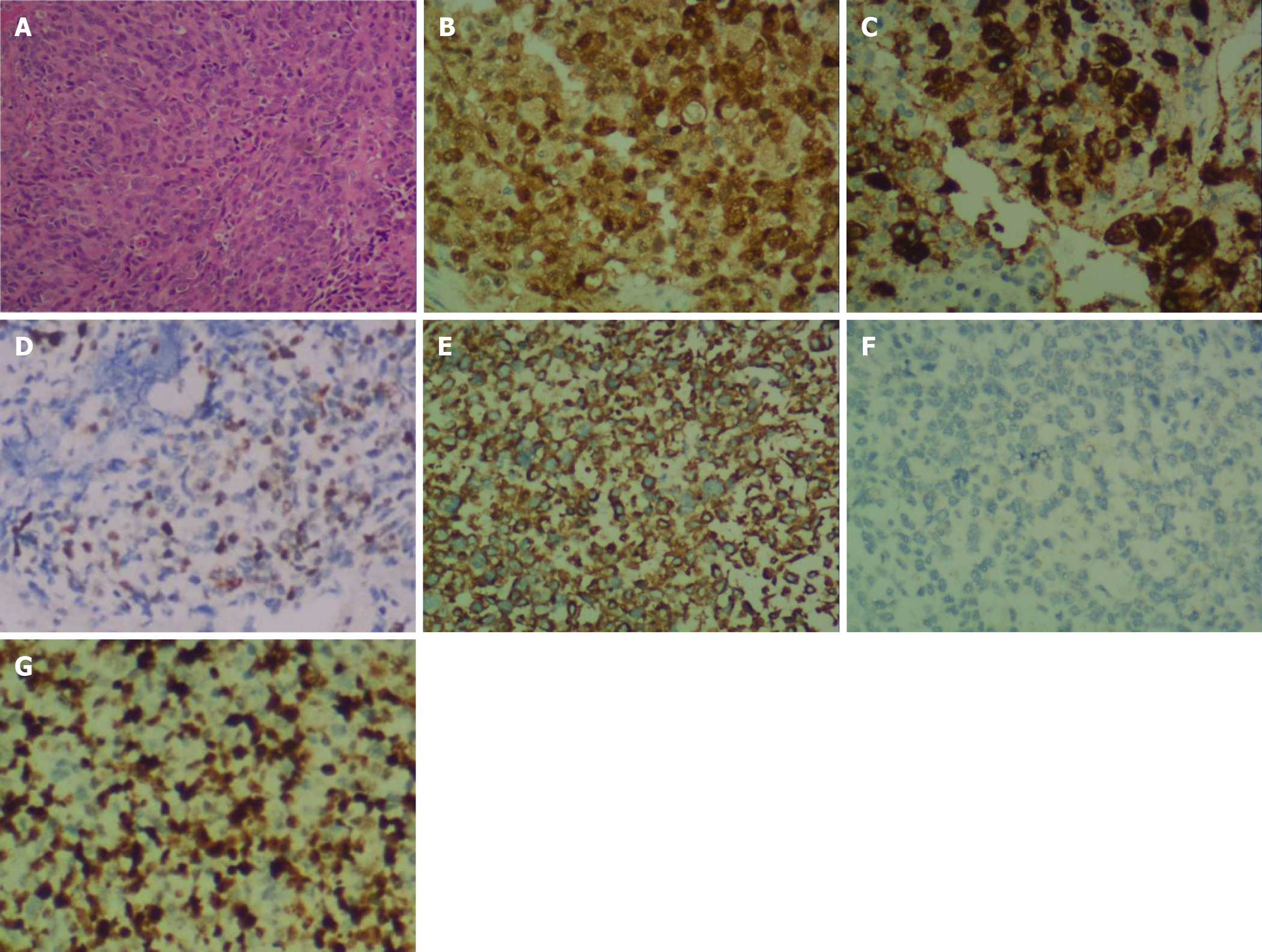
Histopathological examination of the specimen showed that the tissue was composed of most polygonal and some spindle tumor cells. The tumor cells were relatively uniform in size, with rich and transparent cytoplasm. The nuclei of most of the cells were either round or oval, and they had large nucleoli. The tumor cells displayed a high degree of mitotic activity, but no necrosis was seen (Figure 2A). The isolated tumor was also subjected to immunohistochemical examination, which revealed positive staining for S-100, homatropine methylbromide (HMB)-45, and p53, indicating an intramedullary malignant melanoma (Figure 2B-D). The tumor cells expressed vimentin and did not exhibit positivity for the epithelial marker cytokeratin, which indicates that the tumor had undergone the epithelial-to-mesenchymal transition process (Figure 2E and F). Additionally, immunostaining for Ki67 supported an appreciable proliferative activity, and the Ki67 proliferation index was about 10%-50% (Figure 2G).
The patient had no history or clinical manifestation of the primary cutaneous or ocular lesion. Based on the MRI analysis and histological examination, the final diagnosis was primary malignant intramedullary melanoma of the lumbar spinal cord.
The patient underwent L4-S1 discectomy with total resection of a dark reddish-brown ventrally exophytic intramedullary tumor. The tumor was exposed after the dura was widely opened. It was black and firm, and invaded the L5 spinal nerve root. Titanium mesh implantation and pedicle screw fixation were used for the treatment.
The patient refused the molecular targeted therapy based on the drug sensitivity test. Unfortunately, the patient passed away 6 mo after the surgery.
Our case presents a rare occurrence of primary intramedullary malignant melanoma in the lumbar spine manifested by pathological features and clinical behavior. Primary malignant melanoma of the spinal cord is common in the thoracic region and the cervical region.
Melanoma is an aggressive form of cancer that develops in the cells (melanocytes) that produce melanin and can show up anywhere on the skin[4]. Less common types may be found in other organs. Primary melanoma in the CNS arises from melanocytes that develop from their precursors. Hayward's classification of primary spinal cord melanoma relies on the absence of a melanoma outside of the spinal cord and histologic confirmation of melanoma[2]. Primary intramedullary melanoma shows either slow progression or rapid decline, and this lesion is distinct from meningeal melanocytoma and the frequent type of skin melanoma with metastases extending to the CNS.
Notably, surgical criteria are useful when distinguishing primary malignant melanoma from meningeal melanocytoma. At surgery, the adherence to nerve roots by the tumor is suggestive of primary spinal melanoma[5]. Additional chemotherapy and adjuvant radiotherapy may improve disease-free survival[3]. Accordingly, it was believed that our case was associated with a primary spinal cord melanoma.
So far, MRI analysis is the best imaging modality for diagnosing spinal cord tumors. Spinal cord melanoma often displays slightly greater signal intensity on the T1-weighted images than the otherwise healthy spinal cord. On the T2-weighted images, however, it can show the same or less signal intensity than the normal cord. The lesion usually shows mild and homogeneous enhancement following the intravenous administration of a gadolinium-based contrast agent. Here, the appearance of the lesion on MRI in our case was consistent with previously reported findings[6,7]. The final diagnosis should be based on histological and immunophenotyping examinations. Histopathologic features of malignant melanoma include the formation of tight nests surrounded by well-differentiated melanocytes, which produce pigmented melanin[8]. Immunohistochemically, S-100 and HMB-45 may contribute to the diagnosis of malignant melanoma[9].
The various differential diagnoses of primary intramedullary melanoma include metastatic carcinoma, epithelioid schwannoma, and meningeal melanocytoma. In the diagnosis of spinal cord melanoma, the distinction between primary intramedullary melanoma and metastatic melanoma is necessary. As mentioned in the Hayward criteria[2], histological confirmation and exclusion of melanoma outside the CNS (e.g., the skin, squamous mucosa, and the eyes) are required for the diagnosis of primary intramedullary melanoma. In contrast to melanomas, epithelioid schwannomas exhibit compactly interwoven fascicles of pigmented spindle cells with oval nuclei and low nuclear grade[10]. Meningeal melanocytoma is a rare pigmented CNS tumor that might be intradural or extradural and was frequently found in the posterior cranial fossa and spinal cord[11]. Histologically, the tumor cells are arranged in sheets, bundles, nests, and whorls surrounded by a network of reticulin fibers. Mitosis and necrosis are rarely seen in the meningeal melanocytomas.
We herein report a case of primary intramedullary melanoma of the lumbar spinal cord, which is a very rare disease, and surgical resection was applied to the patient after careful evaluation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saffar H S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Liubinas SV, Maartens N, Drummond KJ. Primary melanocytic neoplasms of the central nervous system. J Clin Neurosci. 2010;17:1227-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | Hayward RD. Malignant melanoma and the central nervous system. A guide for classification based on the clinical findings. J Neurol Neurosurg Psychiatry. 1976;39:526-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Sharma A, Sinha VD. Primary Spinal Cord Melanoma of Intradural Extramedullary Origin. J Neurosci Rural Pract. 2019;10:522-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Mirea MA, Eckensperger S, Hengstschläger M, Mikula M. Insights into Differentiation of Melanocytes from Human Stem Cells and Their Relevance for Melanoma Treatment. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Liu QY, Liu AM, Li HG, Guan YB. Primary spinal melanoma of extramedullary origin: a report of three cases and systematic review of the literature. Spinal Cord Ser Cases. 2015;1:15003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Yamasaki T, Kikuchi H, Yamashita J, Asato R, Fujita M. Primary spinal intramedullary malignant melanoma: case report. Neurosurgery. 1989;25:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Uematsu Y, Yukawa S, Yokote H, Itakura T, Hayashi S, Komai N. Meningeal melanocytoma: magnetic resonance imaging characteristics and pathological features. Case report. J Neurosurg. 1992;76:705-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Bastian BC. The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annu Rev Pathol. 2014;9:239-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 379] [Cited by in RCA: 334] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 9. | Xia J, Wang Y, Li F, Wang J, Mu Y, Mei X, Li X, Zhu W, Jin X, Yu K. Expression of microphthalmia transcription factor, S100 protein, and HMB-45 in malignant melanoma and pigmented nevi. Biomed Rep. 2016;5:327-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Hart J, Gardner JM, Edgar M, Weiss SW. Epithelioid Schwannomas: An Analysis of 58 Cases Including Atypical Variants. Am J Surg Pathol. 2016;40:704-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Shanthi V, Ramakrishna BA, Bheemaraju VV, Rao NM, Athota VR. Spinal meningeal melanocytoma: A rare meningeal tumor. Ann Indian Acad Neurol. 2010;13:308-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |