Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2334
Peer-review started: November 20, 2020
First decision: December 21, 2020
Revised: January 4, 2021
Accepted: February 10, 2021
Article in press: February 10, 2021
Published online: April 6, 2021
Processing time: 129 Days and 12.4 Hours
Appendiceal tumors are rare lesions that may not be easily differentiated from primary ovarian lesions preoperatively, despite the use of advanced diagnostic methods by experienced clinicians.
A 59-year-old G2P2 woman, with chronic pelvic pain, underwent a pelvic ultrasound that revealed an adnexal mass measuring 58 mm × 34 mm × 36 mm, with irregular borders, heterogeneous echogenicity, no color Doppler vascularization and without acoustic shadowing. Normal ovarian tissue was visualized in contact with the lesion, and it was impossible to separate the lesion from the ovary by applying pressure with the ultrasound probe. Ascites, peritoneal metastases or other alterations were not observed. With the international ovarian tumor analysis ADNEX model, the lesion was classified as a malignant tumor (the risk of malignancy was 27.1%, corresponding to Ovarian-Adnexal Reporting Data System category 4). Magnetic resonance imaging confirmed the presence of a right adnexal mass, apparently an ovarian tumor measuring 65 mm × 35 mm, without signs of invasive or metastatic disease. During explorative laparotomy, normal morphology of the internal reproductive organs was noted. A solid mobile lesion involved the entire appendix. Appendectomy was performed. Inspection of the abdominal cavity revealed no signs of malignant dissemination. Histopathologically, the appendiceal lesion corresponded to a completely resected low-grade mucinous appendiceal neoplasm (LAMN).
The appropriate treatment and team of specialists who should provide health care to patients with seemingly adnexal lesions depend on the nature (benign vs malignant) and origin (gynecological vs nongynecological) of the lesion. Radiologists, gynecologists and other pelvic surgeons should be familiar with the imaging signs of LAMN whose clinical presentation is silent or nonspecific. The assistance of a consultant specializing in intestinal tumors is important support that gynecological surgeons can receive during the operation to offer the patient with intestinal pathology an optimal intervention.
Core Tip: Low-grade mucinous appendiceal neoplasm is one of the rarest intestinal tumors. Our case highlights how this neoplasm can mimic the behavior of a gynecological (adnexal) lesion in terms of clinical and imaging presentation, while the management and teams of professionals offering treatment significantly differ from those appropriate in the case of adnexal pathology.
- Citation: Borges AL, Reis-de-Carvalho C, Chorão M, Pereira H, Djokovic D. Low-grade mucinous appendiceal neoplasm mimicking an ovarian lesion: A case report and review of literature. World J Clin Cases 2021; 9(10): 2334-2343
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2334.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2334
A pelvic mass with adnexal topography may be a primary adnexal lesion or an ovarian metastasis, but also a primary tumor arising from the uterus, bladder or intestine[1]. Meticulous diagnostic procedures should provide a reliable estimate of the lesion’s nature (benign vs malignant) and its origin (gynecological vs nongyne-cological), to offer the patient adequate treatment without delay, avoiding unnecessary interventions and reducing the risk of iatrogenic morbidity. Appendiceal tumors are infrequent and, in certain cases, such as the one that we are presenting here, may not be differentiated from primary adnexal lesions despite the use of advanced diagnostic methods and preoperative assessment procedures[2].
A postmenopausal 59-year-old woman, G2P2, was admitted to our Gynecology Department due to ultrasound evidence of an adnexal mass of uncertain behavior in the context of chronic pelvic pain.
Over the past 2-3 mo, the patient experienced mild-to-moderate and persistent pain in the right lower quadrant, without irradiation, which worsened with somatic movements. There was no reference to any specific gastrointestinal, gynecological, urological or other symptom. A right adnexal solid lesion of 5 cm was found on transvaginal ultrasound, which was requested by the general practitioner who referred the patient to our tertiary referral hospital.
The patient's past medical history was unremarkable.
The patient's personal and family history was also unremarkable.
Pelvic examination revealed that the external genitalia, vagina and cervix were normal. During bimanual palpation, a 5-6 cm, hard, painful and mobile mass was detected in the right ovarian fossa.
There was no hematological or biochemical alteration. The levels of tumor biomarkers, including CA-125 (6.7 U/mL), were normal.
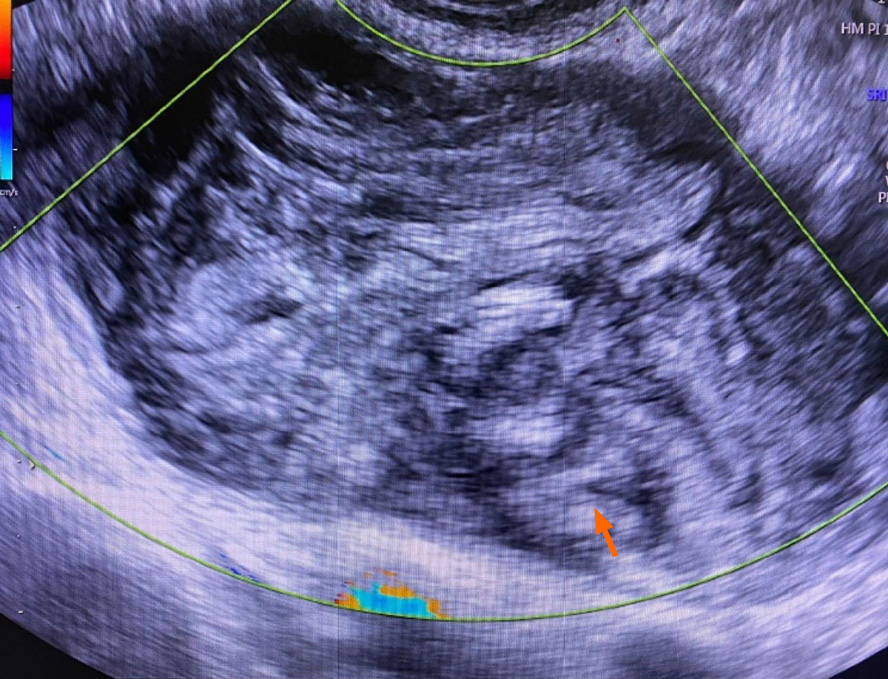
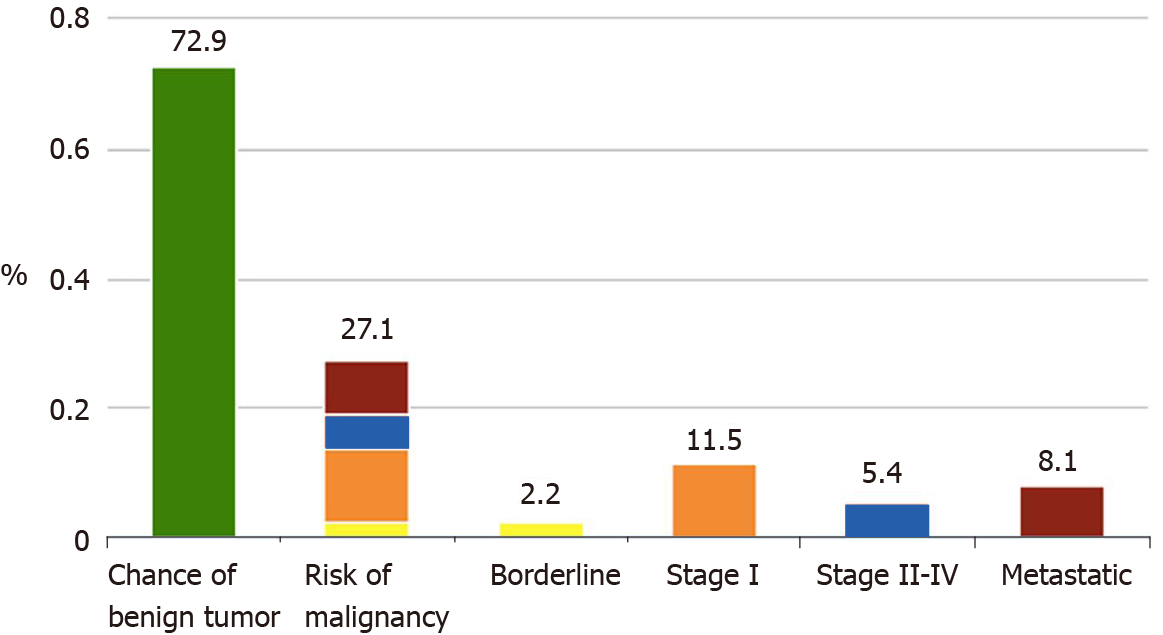
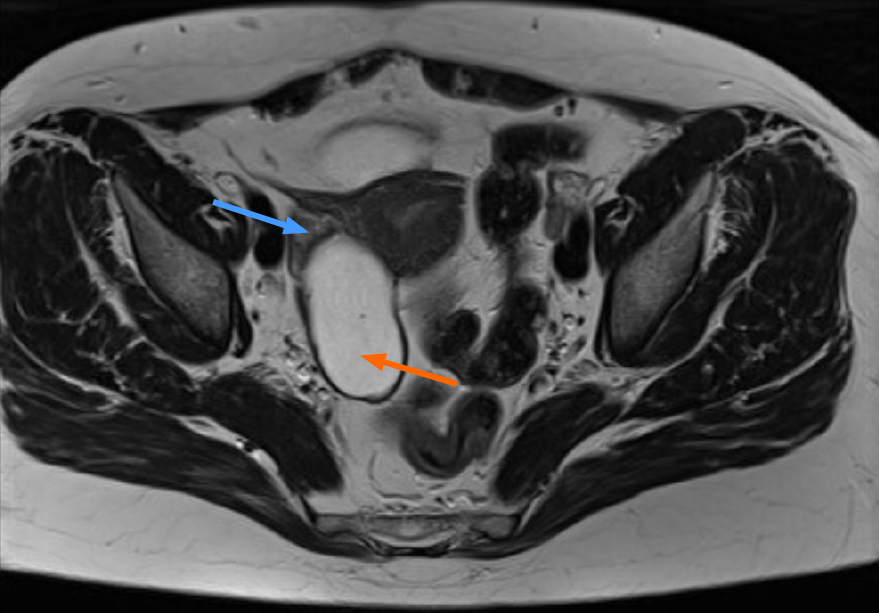
Transvaginal ultrasound revealed a solid lesion measuring 58 mm × 34 mm × 36 mm, in close contact with the normal tissue of the right ovary, with irregular borders, heterogeneous echogenicity, no vascularization visualized by the use of color Doppler (color score 1) and without acoustic shadowing (Figure 1). Ascites, peritoneal metastases or other alterations were not observed. Using the international ovarian tumor analysis (IOTA) ADNEX model[3] and the recommended cutoff of 10%, the lesion was classified as a malignant tumor (Figure 2). The determined risk of malignancy was 27.1%, which corresponded to the Ovarian-Adnexal Reporting Data System 4 risk category (i.e., intermediate risk)[4]. Pelvic magnetic resonance imaging (MRI) showed a tumor apparently originating from the right ovary and measuring 65 mm × 35 mm, while no signs of invasive disease were noted (Figure 3). In both imaging techniques, continuity between the tumor and gastrointestinal tract was not observed or documented.
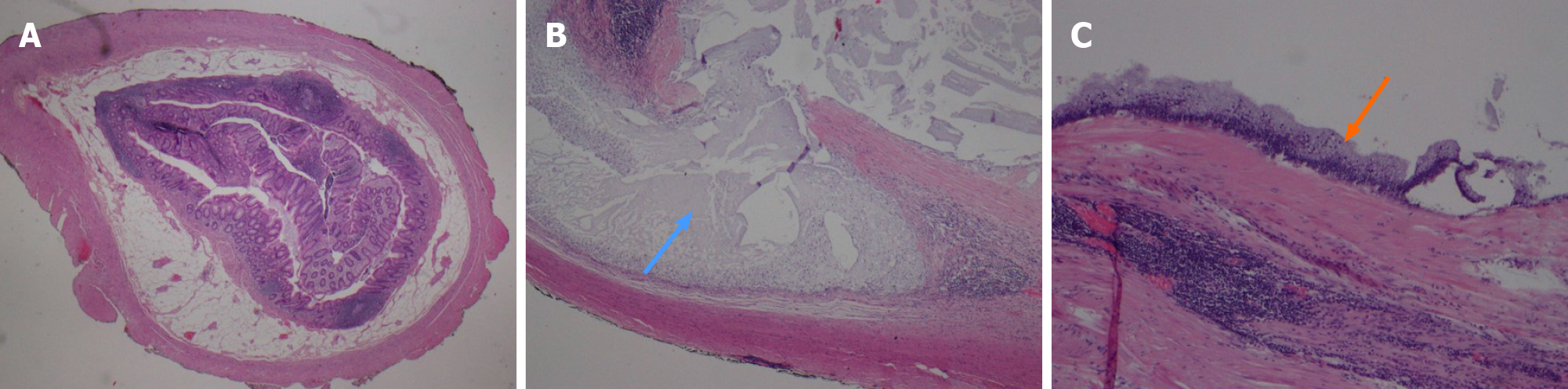
The patient underwent an exploratory laparotomy. Normal uterus, fallopian tubes and ovaries were visualized. We found a solid and mobile lesion originating in the appendix (Figure 4). Inspection of the abdominal cavity revealed no signs of malignant dissemination. The lesion histological diagnosis was low-grade mucinous appendiceal neoplasm (LAMN) (Figure 5).
Appendectomy was performed. In accordance with the orientation provided by the general surgery consultant, who was invited to the operative theatre, no other intervention was performed.
The patient had an uneventful postoperative clinical course and was discharged from the hospital on the third postoperative day. Currently, six months after surgery, the patient remains asymptomatic.
Pelvic tumors represent one of the most frequent reasons for referral to gynecology departments. The management strategies are guided by the degree of clinical imaging-based suspicion of malignancy, as well as symptoms; the patient's age; and her desire for fertility preservation. To promote survival and/or quality of life, an adequate characterization and clinical contextualization of the observed lesions must be carried out in order to refer the patients with a malignant neoplasm for treatment by gynecological oncologists or other specialists in their respective subspecialized units to avoid unnecessary surgery in patients with functional adnexal formations and benign adnexal lesions. The case presented in this study highlights how the preoperative assessment of a patient can be challenging and how gynecologists, despite a detailed and dedicated preoperative evaluation of the patient, can face nongynecological lesions during surgery.
Instead of an expected solid ovarian lesion, our patient had a LAMN, which accounts for 1% of gastrointestinal neoplasms[5]. It is a low-grade dysplastic epithelial lesion that, by definition, lacks infiltrative invasion, which would be termed mucinous adenocarcinoma[6]. The PubMed search that we conducted on January 1, 2021, identified 23 reports resembling our case (Table 1). A large case series indicated that the median age at LAMN diagnosis is 61 years, which is close to the age of our patient[7]. In terms of sex, the literature reports a higher prevalence in females (the female/male ratio varies from 7:1[8] to 1.4:1[9]). Similarly, ovarian carcinoma occurs at the median age of 63 years[10]. Regarding clinical presentation, ovarian cancer typically produces symptoms, including nonspecific pelvic/abdominal pain, bloating, urinary urgency or frequency, in the late and advanced stages[11,12]. In the same manner, appendiceal mucocele that mimics an adnexal mass most commonly presents with pelvic/abdominal pain[13]. The complications of LAMN include intussusception, volvulus, small bowel or ureteral obstruction, rupture and mucinous ascites, namely, pseudomyxoma peritonei. The ovarian etiology assumption by routine and epidemiological/clinical overlap can easily lead to an erroneous diagnosis. Preoperatively, LAMN is commonly misdiagnosed as acute appendicitis or an adnexal mass[14], as occurred in our patient. Differential diagnosis may also include mucinous adenocarcinoma of the appendix and a high-grade appendiceal mucinous neoplasm, a pelvic foreign body and a subserous uterine fibroid. The literature consistently reinforces the idea that the presence of a right-sided adnexal mass should allow for the possibility of an appendiceal neoplasm[15,16]. Interestingly, cases of left-sided appendiceal neoplasms mimicking an adnexal mass have recently been reported[17,18].
| Case | Age | Cardinal symptom | Clinical context | Imaging modality | Tumor marker | Presumed diagnosis | Treatment | Appendix: Histopathology |
| 1[24] | 32 | Abdominal pain | Acute abdomen (38 wk pregnancy) | US (cystic mass 32 mm × 35 mm × 59 mm) | N/A | Right ovarian torsion | Laparotomy: Appendectomy C-Section | Mucocele (torsion) |
| 2[25] | 49 | Pelvic pain | Chronic pain (1 yr) | US (heterogenous mass 70 mm × 35 mm × 40 mm). MRI (cystic mass 70 mm × 63 mm × 29 mm) | CEA 10.5 μg/L (↑). CA125 normal | Right adnexal mass of paraovarian origin | Laparoscopy: Appendectomy. Peritoneal washing | LAMN. Peritoneal citology: Negative |
| 3[2] | 81 | Abdominal pain | Chronic pain (several months) | US (heterogenous cystic mass 110 mm × 90 mm). MRI (heterogenous cystic mass 120 mm × 100 mm) | CA125 13.18 U/mL. CA19.9 20.8 U/mL. CEA 1.76 ng/mL. CA15.3 6.7 U/mL | Right adnexal mass | Laparotomy: Appendectomy and a right hemicolectomy with ileo-transverse anastomosis. Total abdominal hysterectomy and bilateral salpingo-oophorectomy due to pelvic organ prolapse | Appendiceal mucinous neoplasm with low malignancy potential |
| 4[17] | 61 | Incidental imaging finding | Preventive gynecological check-up | US (heterogenous solid mass 104 mm × 40 mm) | CA19.9 40 U/mL (↑). CA125 9 U/mL. CA15.3 13 U/mL. AFP 2 ng/mL | Left adnexal mass | Laparotomy: Appendectomy. Excisional biopsy of the omentum | LAMN |
| 5[26] | 41 | Pelvic pain | Chronic pain | US (cystic mass 60 mm × 28 mm). MRI (70 mm × 40 mm × 30 mm) | CEA and CA19.9 normal | Right adnexal mass | Laparoscopy converted to laparotomy: Right hemicolectomy with side to side ileocolic stapler anastomosis | LAMN |
| 6[27] | 15 | Abdominal pain | Acute abdomen | US; CT (no precise description reported) | N/A | Right ovarian torsion | Laparoscopy: Appendectomy | Mucocele |
| 7[28] | 46 | Incidental pelvic examination finding | Preventive gynecological check-up | US (cystic mass 115 mm × 40 mm) | N/A | Right adnexal mass (hydro-pyosalpinx, tubo-ovarian abscess or ovarian cyst) | Laparotomy: Appendectomy | Mucocele |
| 8[15] | 71 | Pelvic pain | Acute pain | US (cystic mass 50 mm × 70 mm). MRI (cystic mass 40 mm × 80 mm) | CA125 9.1 U/mL. CA19.9 5.09 U/mL. AFP 2.4 ng/mL. β-hCG 0.01 mIU/mL | Righ adnexal mass | Laparotomy: Appendectomy. Total abdominal hysterectomy and bilateral salpingo-oophorectomy due to pelvic organ prolapse | Mucocele |
| 9[29] | 80 | Abdominal pain | Chronic pain (several months) | US (mixed echogenic mass 61 mm × 43 mm × 51 mm). CT (calcified cyst 70 mm × 60 mm × 50 mm) | CA125 normal | Righ adnexal mass (ovarian cyst) | Laparotomy: Appendectomy | Mucinous cystadenoma |
| 10[30] | 61 | Pelvic pain | Chronic pain (several months) | US (cystic mass). CT (homogenous mass 110 mm × 35 mm) | Normal (not specified) | Right adnexal mass (ovarian cyst or hydrosalpynx) | Laparoscopy: Appendectomy | LAMN |
| 11[31] | 26 | Pelvic pain | Chronic pain | US (cystic mass 30 mm × 30 mm) | N/A | Right adnexal mass (ovarian cyst) | Laparoscopy: Appendectomy | Mucinous cystadenoma with mild-moderate dysplasia |
| 12[16] | 70 | Incidental pelvic examination finding | Preventive gynecological check-up | US (solid mass 60 mm × 60 mm × 40 mm) | CA125 120 mg/dL (↑). CEA normal | Right adnexal mass | Laparotomy: Appendectomy. Total abdominal hysterectomy and bilateral salpingo-oophorectomy. | Mucinous cystadenoma |
| 13[32] | 68 | Incidental pelvic examination finding | Abnormal uterine bleeding | US (cystic mass 39 mm) | N/A | Right adnexal mass (ovarian cyst) | Laparoscopy: Appendectomy | Mucocele |
| 14[18] | 50 | Pelvic pain | - | US (tubular mass 96 mm × 40 mm × 33 mm). MRI (no precise description reported) | N/A | Left adnexal mass (hydrosalpynx) | Robotic: Appendectomy Right hemicolectomy | Low grade mucinous adenocarcinoma |
| 15[33] | 42 | Incidental imaging finding | 1st trimester bleeding | US (cystic mass 120 mm × 108 mm × 58 mm) | CA125 16 U/mL | Right adnexal mass (ovarian cyst) | Laparotomy: Appendectomy | Mucocele |
| 16[34] | 31 | Pelvic pain | Fever | US; MRI (no precise description reported) | CA125 12.2 U/mL. CEA 5.2 U/mL. CA19.9 0.8 ng/mL | Right adnexal mass (hydrosalpynx) | Laparotomy: Appendectomy | Mucocele |
| 17[35] | 79 | Incidental imaging finding | Preventive gynecological check-up | US (uniloculated mass, characterizedby dishomogeneous content, distal shadowing 59 mm × 43 mm × 40 mm). MRI (cystic mass 80 mm) | CEA 1.26 ng/mL. CA125 8.1 U/mL. CA19.9 3.44 U/mL. CA15.3 14.1 U/mL | Right adnexal mass (ovarian cyst) | Laparoscopy: Appendectomy | Mucocele |
| 18[36] | 80 | Pelvic pain | Chronic pain | US (cystic/solid mass 83 mm × 65 mm × 64 mm). CT (cystic mass 100 mm × 80 mm) | CEA 54.2 ng/mL | Right adnexal mass | Laparotomy: Appendectomy. Omentectomy, total abdominal hysterectomy, and bilateral salpingo-oophorectomy | LAMN |
| 19[37] | 83 | Incidental imaging finding | Preventive gynecological check-up | US (cystic/solid mass 87 mm). MRI (cystic mass 90 mm) | CEA 5.3 ng/mL (↑). CA15.3 31.4 U/mL | Right adnexal mass | Laparotomy: Appendectomy | LAMN |
| 20[38] | 78 | Asymptomatic | Known adnexal mass on ultrasound follow-up | US (cystic mass 58 mm × 42 mm × 35 mm). MRI (bilocular cystic mass 41 mm × 19 mm) | CEA, CA125 and CA19.9 normal | Right adnexal mass | Laparotomy: Appendectomy. Total abdominal hysterectomy and bilateral salpingo-oophorectomy due to pelvic organ prolapse. | Mucinous cystadenoma |
| 21[39] | 28 | Pelvic pain | Acute abdomen | CT (cystic mass 33 mm × 50 mm) | N/A | Right adnexal mass (ovarin cyst rupture) | Laparoscopy: Appendectomy | Mucocele (torsion: Hemorrhagic transmural necrosis) |
| 22[40] | 36 | Pelvic pain | - | US (cystic complex mass) | CEA ↑; CA19.9 ↑ | Right adnexal mass | Laparotomy: Appendectomy | Mucinous cystadenoma |
| 23[41] | 75 | Asymptomatic | Adnexal mass on ultrasound (investigation due to CEA↑) | US. CT (cystic mass 90 mm) | CEA 17.7 ng/mL (↑). CA125 and CA19.9 normal | Right adnexal mass (ovarian malignancy) | Laparotomy: Appendectomy | Mucinous cystadenoma |
Imaging modalities for diagnosis include ultrasound, computed tomography (CT) and MRI. Regarding the ultrasound imaging features, it has been described that an appendiceal mucocele (the LAMN includes lesions that were described previously as mucoceles) should be suspected when a cystic mass with concentric echogenic layers (the “onion skin” sign) and a normal ovary are detected in the right lower quadrant[19]. In parallel, the possibility of separating a lesion from the ovary by applying pressure with the ultrasound probe (“split” sign) also indicates its nonovarian origin[20]. In our patient, we observed the “onion skin” sign (Figure 1) but not the “split” sign. The IOTA models have been externally validated and found to be valuable tools for discriminating between benign and malignant ovarian tumors (1); however, they should not be used if nonadnexal lesions with adnexal topography are suspected. We used the IOTA ADNEX model because it seemed a lesion originating from the ovarian parenchyma. The obtained output could not properly assist us. The literature suggest that CT scan are superior to ultrasound evaluations in diagnosing LAMN[21], namely, to distinguish LAMN from acute appendicitis. Nevertheless, CT is diagnostic in less than 50% of cases[22]. We used MRI to complement the ultrasound assessment, and the MRI findings were consistent with a primary ovarian lesion.
Once the appendiceal lesion was confirmed during the explorative intervention, the assistance of a surgeon specializing in intestinal pathology was of fundamental importance to provide an appropriate treatment to the patient. In accordance with the Clinical Practice Guidelines of the American Society of Colon and Rectal Surgeons[23], LAMNs with negative margins and no evidence of perforation or peritoneal involvement are safely treated with appendectomy alone.
The spectrum of lesions that have adnexal topography is wide, and in addition to diverse adnexal lesions, it includes uterine, bladder and intestinal pathology. LAMN should be suspected when a right adnexal mass with concentric echogenic layers separable from normal ovarian tissue is observed. Despite meticulous preoperative examination, when unexpectedly nongynecological lesions are identified, intraoperative cooperation between gynecologists and other specialists is crucial to offer adequate intervention to the patient. Registering such cases and reviewing the preoperative imaging findings may increase preoperative diagnostic sensitivity and specificity and therefore should not be omitted.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Iizuka M S-Editor: Fan JR L-Editor: A P-Editor: Liu JH
| 1. | Sørensen SS, Mosgaard BJ. Combination of cancer antigen 125 and carcinoembryonic antigen can improve ovarian cancer diagnosis. Dan Med Bull. 2011;58:A4331. [PubMed] |
| 2. | Akman L, Hursitoglu BS, Hortu İ, Sezer T, Oztekin K, Avsargil BD. Large mucinous neoplasm of the appendix mimicking adnexal mass in a postmenopausal woman. Int J Surg Case Rep. 2014;5:1265-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Van Calster B, Van Hoorde K, Valentin L, Testa AC, Fischerova D, Van Holsbeke C, Savelli L, Franchi D, Epstein E, Kaijser J, Van Belle V, Czekierdowski A, Guerriero S, Fruscio R, Lanzani C, Scala F, Bourne T, Timmerman D; International Ovarian Tumour Analysis Group. Evaluating the risk of ovarian cancer before surgery using the ADNEX model to differentiate between benign, borderline, early and advanced stage invasive, and secondary metastatic tumours: prospective multicentre diagnostic study. BMJ. 2014;349:g5920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 299] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 4. | Andreotti RF, Timmerman D, Strachowski LM, Froyman W, Benacerraf BR, Bennett GL, Bourne T, Brown DL, Coleman BG, Frates MC, Goldstein SR, Hamper UM, Horrow MM, Hernanz-Schulman M, Reinhold C, Rose SL, Whitcomb BP, Wolfman WL, Glanc P. O-RADS US risk stratification and management system: A consensus guideline from the ACR ovarian-adnexal reporting and data system committee. Radiology. 2020;294:168-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 245] [Article Influence: 40.8] [Reference Citation Analysis (2)] |
| 5. | Ramaswamy V. Pathology of mucinous appendiceal tumors and pseudomyxoma peritonei. Indian J Surg Oncol. 2016;7:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 6. | Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, Taflampas P, Chapman S, Moran BJ; Peritoneal Surface Oncology Group International. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: The results of the peritoneal surface oncology group international (PSOGI) modified Delphi process. Am J Surg Pathol. 2016;40:14-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 496] [Article Influence: 55.1] [Reference Citation Analysis (0)] |
| 7. | Zhang W, Tan C, Xu M, Wu X. Appendiceal mucinous neoplasm mimics ovarian tumors: Challenges for preoperative and intraoperative diagnosis and clinical implication. Eur J Surg Oncol. 2019;45:2120-2125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Landen S, Bertrand C, Maddern GJ, Herman D, Pourbaix A, de Neve A, Schmitz A. Appendiceal mucoceles and pseudomyxoma peritonei. Surg Gynecol Obstet. 1992;175:401-404. [PubMed] |
| 9. | Yu XR, Mao J, Tang W, Meng XY, Tian Y, Du ZL. Low-grade appendiceal mucinous neoplasms confined to the appendix: clinical manifestations and CT findings. J Investig Med. 2020;68:75-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014;384:1376-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1177] [Cited by in RCA: 1430] [Article Influence: 130.0] [Reference Citation Analysis (0)] |
| 11. | Goff BA, Mandel LS, Melancon CH, Muntz HG. Frequency of symptoms of ovarian cancer in women presenting to primary care clinics. JAMA. 2004;291:2705-2712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 264] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 12. | Goff BA, Mandel LS, Drescher CW, Urban N, Gough S, Schurman KM, Patras J, Mahony BS, Andersen MR. Development of an ovarian cancer symptom index: possibilities for earlier detection. Cancer. 2007;109:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 250] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 13. | Cubro H, Cengic V, Burina N, Kravic Z, Beciragic E, Vranic S. Mucocele of the appendix presenting as an exacerbated chronic tubo-ovarian abscess: A case report and comprehensive review of the literature. Medicine (Baltimore). 2019;98:e17149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Padmanaban V, Morano WF, Gleeson E, Aggarwal A, Mapow BL, Stein DE, Bowne WB. Incidentally discovered low-grade appendiceal mucinous neoplasm: a precursor to pseudomyxoma peritonei. Clin Case Rep. 2016;4:1112-1116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Balci O, Ozdemir S, Mahmoud AS. Appendiceal mucocele mimicking a cystic right adnexal mass. Taiwan J Obstet Gynecol. 2009;48:412-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Dragoumis K, Mikos T, Zafrakas M, Assimakopoulos E, Venizelos I, Demertzidis H, Bontis J. Mucocele of the vermiform appendix with sonographic appearance of an adnexal mass. Gynecol Obstet Invest. 2005;59:162-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Aleter A, El Ansari W. Incidental appendiceal mucinous neoplasm mimicking a left adnexal mass: A case report. Int J Surg Case Rep. 2020;74:132-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Hajiran A, Baker K, Jain P, Hashmi M. Case of an appendiceal mucinous adenocarcinoma presenting as a left adnexal mass. Int J Surg Case Rep. 2014;5:172-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Caspi B, Cassif E, Auslender R, Herman A, Hagay Z, Appelman Z. The onion skin sign: a specific sonographic marker of appendiceal mucocele. J Ultrasound Med. 2004;23:117-21; quiz 122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Testa AC, Van Holsbeke C, Mascilini F, Timmerman D. Dynamic and interactive gynecological ultrasound examination. Ultrasound Obstet Gynecol. 2009;34:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Xiao J, Li P, Liu W. Analysis of Clinical characteristics of low-grade appendiceal mucinous neoplasm (LAMN): A retrospective cohort study of 51 LAMN patients. J Invest Surg. 2020: 1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Nutu OA, Marcacuzco Quinto AA, Manrique Municio A, Justo Alonso I, Calvo Pulido J, García-Conde M, Cambra Molero F, Jiménez Romero LC. Mucinous appendiceal neoplasms: Incidence, diagnosis and surgical treatment. Cir Esp. 2017;95:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Glasgow SC, Gaertner W, Stewart D, Davids J, Alavi K, Paquette IM, Steele SR, Feingold DL. The American society of colon and rectal surgeons, clinical practice guidelines for the management of appendiceal neoplasms. Dis Colon Rectum. 2019;62:1425-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 24. | Abu Zidan FM, al-Hilaly MA, al-Atrabi N. Torsion of a mucocele of the appendix in a pregnant woman. Acta Obstet Gynecol Scand. 1992;71:140-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Ahmed N, Vimplis S, Deo N. A mucocele of the appendix seen as an adnexal mass on ultrasound scan. J Obstet Gynaecol. 2017;37:116-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Alghamdi AO, Aldossary MY, Alsawidan M, AlBahar S. Low grade appendiceal mucinous neoplasm mimicking an ovarian cyst: A case report. Int J Surg Case Rep. 2020;70:145-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Arrington D, Jewett B, Sterner S, Caplan M, Thacker P. Incidental mucocele of the appendix in a 15-year-old girl. Pediatr Emerg Care. 2014;30:555-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Bahia JO, Wilson MH. Mucocele of the appendix presenting as an adnexal mass. J Clin Ultrasound. 1989;17:62-66. [PubMed] [DOI] [Full Text] |
| 29. | Bartlett C, Manoharan M, Jackson A. Mucocele of the appendix - a diagnostic dilemma: a case report. J Med Case Rep. 2007;1:183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Cristian DA, Grama FA, Becheanu G, Pop A, Popa I, Şurlin V, Stănilescu S, Bratu AM, Burcoş T. Low-grade appendiceal mucinous neoplasm mimicking an adnexal mass. Rom J Morphol Embryol. 2015;56:837-842. [PubMed] |
| 31. | Demirci RK, Habibi M, Karakaş BR, Buluş H, Akkoca M, Öner OZ. Appendix mucocele mimicking a complex ovarian cyst. Ulus Cerrahi Derg. 2015;31:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Gortchev G, Tomov S, Dimitrov D, Nanev V, Betova T. Appendiceal mucocele presenting as a right adnexal mass: a case report. Obstet Gynecol Int. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Kalu E, Croucher C. Appendiceal mucocele: a rare differential diagnosis of a cystic right adnexal mass. Arch Gynecol Obstet. 2005;271:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Kanasugi T, Kikuchi A, Omi H, Ikeda M, Fukushima A, Sugiyama T. Appendiceal mucocele and peritoneal inclusion cyst mimicking right adnexal masses: a diagnostic challenge in gynecologic practice. J Med Ultrason (2001). 2013;40:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 35. | Paladino E, Bellantone M, Conway F, Sesti F, Piccione E, Pietropolli A. Large mucocele of the appendix at laparoscopy presenting as an adnexal mass in a postmenopausal woman: a case report. Case Rep Obstet Gynecol. 2014;2014:486078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Panagopoulos P, Tsokaki T, Misiakos E, Domi V, Christodoulaki C, Sioutis D, Papantoniou N. Low-Grade appendiceal mucinous neoplasm presenting as an adnexal mass. Case Rep Obstet Gynecol. 2017;2017:7165321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Pantiora EV, Massaras D, Koutalas J, Bagiasta A, Kontis EA, Fragulidis GP. Low-grade appendiceal mucinous neoplasm presenting as adnexal mass: A case report. Cureus. 2018;10:e3568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Papoutsis D, Protopappas A, Belitsos P, Sotiropoulou M, Antonakou A, Loutradis D, Antsaklis A. Mucocele of the vermiform appendix misdiagnosed as an adnexal mass on transvaginal sonography. J Clin Ultrasound. 2012;40:522-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Rudloff U, Malhotra S. Volvulus of an appendiceal mucocele: report of a case. Surg Today. 2007;37:514-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Scaffa C, Di Bella O, Tartaglia E, Rotondi M, Lup F, Messalli EM. Surgical approach to appendiceal mucocele mimicking an adnexal complex mass: case report. Eur J Gynaecol Oncol. 2007;28:503-505. [PubMed] |
| 41. | Shimizu T, Shimizu M, Kawaguchi K, Yomura W, Ihara Y, Matsumoto T. Mucinous cystadenoma of the appendix with raised serum carcinoembryonic antigen concentration: clinical and pathological features. J Clin Pathol. 1997;50:613-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |