Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2320
Peer-review started: October 16, 2020
First decision: December 21, 2020
Revised: December 28, 2020
Accepted: January 25, 2021
Article in press: January 25, 2021
Published online: April 6, 2021
Processing time: 164 Days and 17.9 Hours
Pulsatile tinnitus (PT) is a potentially disabling symptom that has received increasing attention. Multiple causes of PT have been confirmed by targeted treatment. However, dynamic changes of related structures in PT patients with multiple causes after stenting for ipsilateral transverse sinus stenosis (TSS) have not been previously reported. We report such a case and present postoperative computed tomography venography (CTV) follow-up findings to demonstrate the decreased sigmoid sinus diverticulum and bone remodeling.
A 45-year-old man suffered from left-sided PT for 15 years that was occasionally accompanied by headache and dizziness. Pre-operative CTV revealed left-sided sigmoid sinus wall anomalies (SSWAs), TSS, outflow dominance, large posterior condylar emissary vein, and an empty sella turcica. A cerebrospinal fluid pressure of 270 mmH2O was further detected. The sound disappeared immediately after stenting for ipsilateral TSS, with no recurrence during 2 years of follow-up. After the procedure, the patient underwent four consecutive CTV examinations. The diverticulum decreased 6 mo after the procedure with new bone remodeling. The density of the remodeled bone was further increased 1 year later, and a hardened edge was formed 2 years later.
PT associated with SSWAs, TSS, and idiopathic intracranial hypertension can be cured by stenting for TSS alone. And bone remodeling around SSWAs is a more significant finding.
Core Tip: Pulsatile tinnitus is a potential disease that has attracted considerable attention recently. Multiple causes of pulsatile tinnitus have been identified by targeted treatment. However, the dynamic CT changes of related structures after stenting for transverse sinus stenosis have never been reported. In this case, four postoperative computed tomography venography examinations were performed to demonstrate the dynamic changes in the sigmoid sinus wall anomalies and transverse sinus stenosis. Stenting relieved transverse sinus stenosis, reduced intracranial pressure, and eliminated tinnitus. A decreased sigmoid sinus diverticulum and bone remodeling represent more significant findings.
- Citation: Qiu XY, Zhao PF, Ding HY, Li XS, Lv H, Yang ZH, Gong SS, Jin L, Wang ZC. Bone remodeling in sigmoid sinus diverticulum after stenting for transverse sinus stenosis in pulsatile tinnitus: A case report. World J Clin Cases 2021; 9(10): 2320-2325
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2320.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2320
Pulsatile tinnitus (PT) is the self-perception of a pulse-synchronous, vascular sound in the ear and is a potentially disabling symptom. The long-term existence of this symptom seriously affects the patient's mood and leads to both functional and structural brain changes[1]. Multiple causes have been confirmed, including sigmoid sinus wall anomalies (SSWAs; including dehiscence and diverticulum)[2], transverse sinus stenosis (TSS)[3], and idiopathic intracranial hypertension (IIH)[4], which are some of the most common venous causes. SSWA is the most common finding after a comprehensive radiologic examination[5], and is widely treated by trans-temporal sinus wall reconstruction[2]. Patients with SSWAs typically report accompanying TSS[2,6,7]. Stenting for TSS is occasionally used for venous PT or IIH patients[8]. However, previous studies of PT with TSS or IIH have rarely mentioned the co-occurrence of an SSWA. Furthermore, to our knowledge, computed tomography venography (CTV) follow-up findings after stenting for TSS in PT patients remain lacking.
Herein, we report a PT patient with SSWAs, bilateral TSS, and IIH who underwent stenting for ipsilateral TSS. The sound disappeared immediately after the procedure, with no recurrence during 2 years of follow-up. Four postoperative CTV examinations were performed to demonstrate dynamic changes in the SSWAs and TSS.
A 45-year-old man suffered from left-sided PT that was occasionally accompanied by headache and dizziness. The sound was pulse-synchronous with the heartbeat, which was more obvious at rest and could be diminished with compression of the ipsilateral jugular vein area.
The symptoms lasted 15 years and worsened in the last 2 years. There was no previous history of ear lesion or hearing loss.
The patient underwent surgeries for nasal septal reconstruction and intraocular lens implantation 9 years prior.
The family history was unremarkable.
Otoscopic examination revealed no abnormalities in either ear. Pure tone audiometry showed slightly conductive hearing loss in the left ear (29 dB for air conduction and 19 dB for bone conduction). The acoustic impedance was type A. No hearing abnormalities were present in the right ear.
All indicators of laboratory examination were within the normal range.
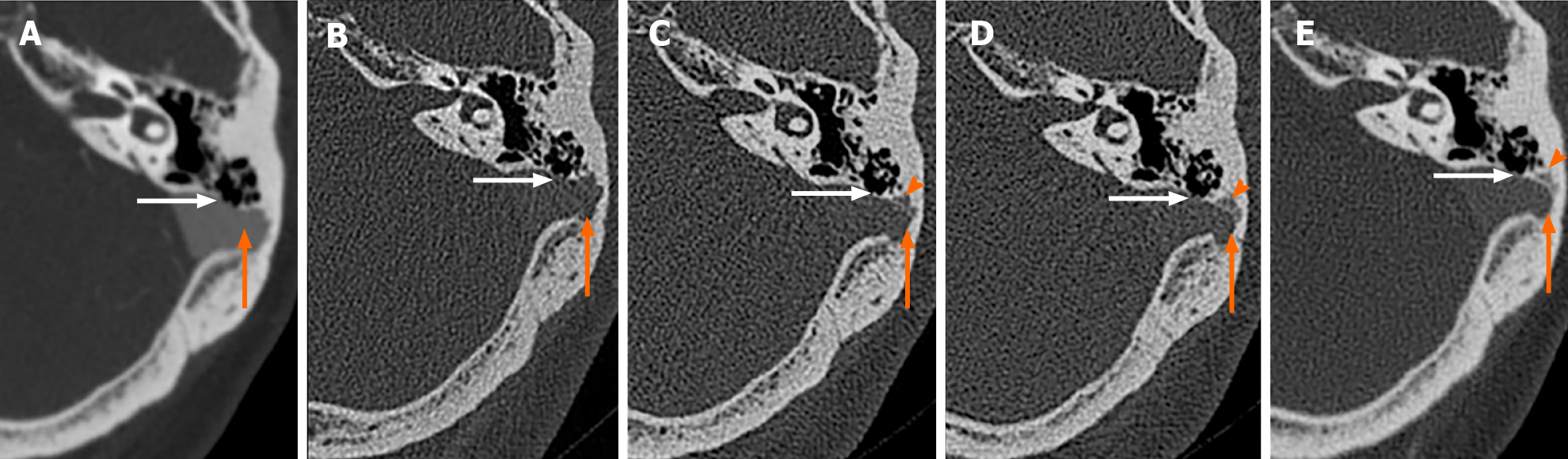
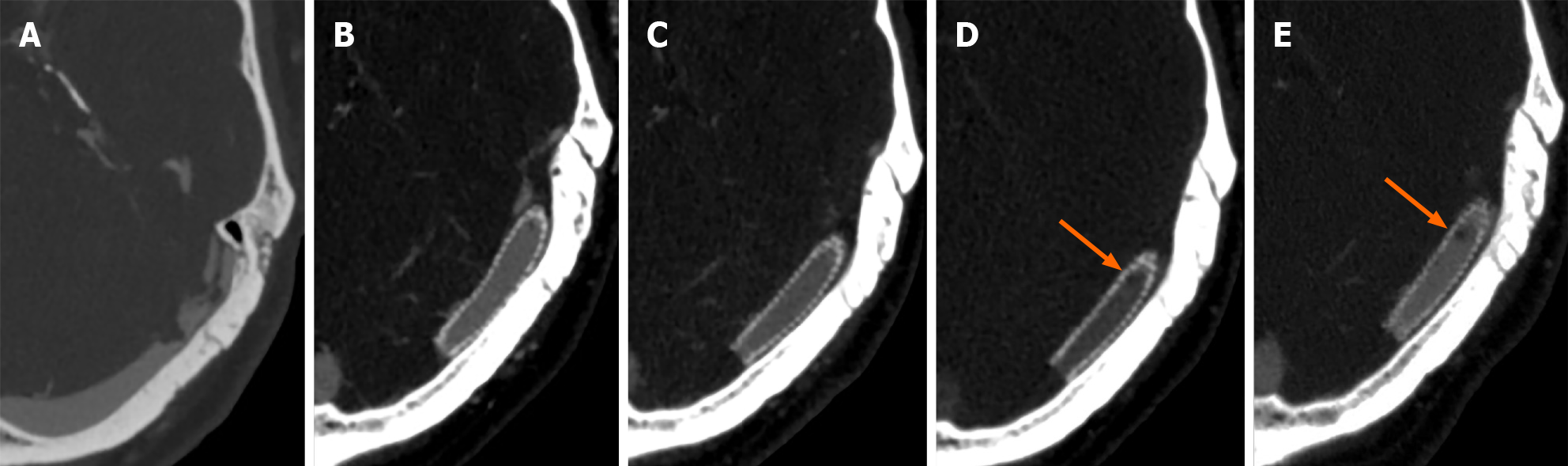
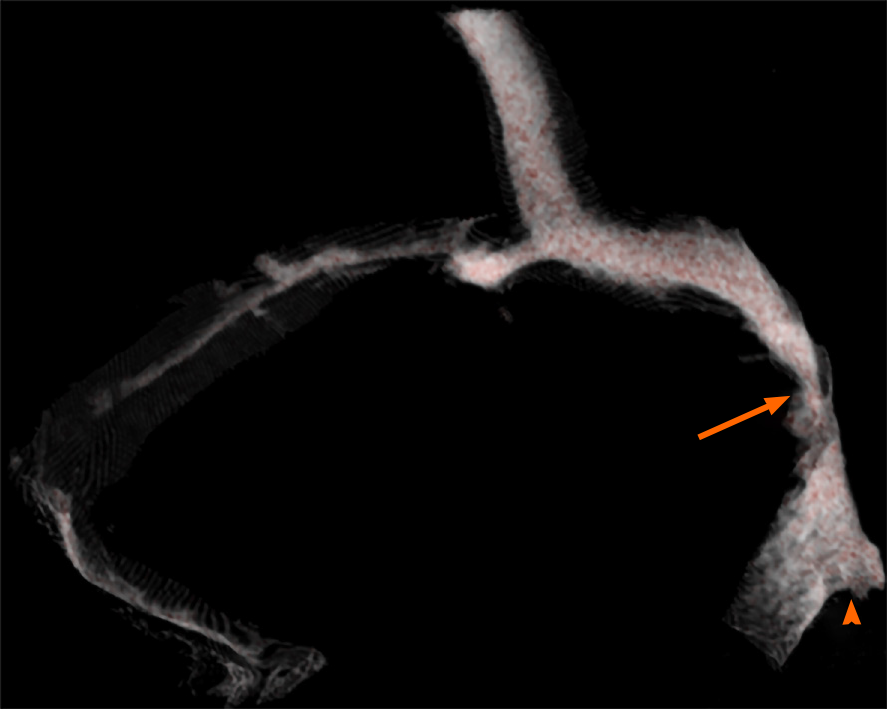
Pre-operative CTV revealed focal bulging of the left sigmoid sinus; a focal defect of the bony wall around the adjacent sigmoid sinus (Figure 1A); severe ipsilateral TSS (Figure 2A); contralateral transverse sinus dysplasia and ipsilateral outflow dominance (Figure 3); a left-sided, large, posterior condylar emissary vein (PCEV); and an empty sella turcica. Digital subtraction angiography was performed to exclude arteriovenous malformations or tumors with abundant vascularity.
Lumbar puncture indicated a cerebrospinal fluid pressure of 270 mmH2O, and IIH was further diagnosed according to the existing criteria.
CTV revealed left sigmoid sinus dehiscence and diverticulum, severe ipsilateral TSS, contralateral transverse sinus dysplasia, ipsilateral outflow dominance, a left-sided, large PCEV, and an empty sella turcica.
Responsible lesions should be identified. Then, the patient should undergo treatment by stenting for left TSS and long-term anticoagulant therapy.
Other vascular diseases should be excluded based on digital subtraction angiography. Then, the decision regarding stenting should be made.
PT with multiple causes, including left SSWAs, TSS, outflow dominance, large PCEV, contralateral transverse sinus dysplasia, and empty sella turcica.
Stenting for TSS was successfully performed to re-expand the left TSS by an interventional doctor with 25 years of experience. And long-term anticoagulant therapy was required.
The sound disappeared immediately after the procedure. The patient was discharged 7 d later, with no adverse reactions.
Postoperative CTV examinations were performed 2 d, 6 mo, 1 year, and 2 years later. CTV performed on the second day after stenting for TSS revealed that the TSS was well dilated (Figure 2B). The results showed that the diverticulum was decreased 4 mo after the procedure with new bone remodeling (Figure 1C). The density of the remodeled bone was further increased 1 year later (Figure 1D), and a hardened edge was formed 2 years later (Figure 1E). In addition, the TSS was well expanded by the stent, and there were no changes in the extent of sigmoid sinus dehiscence (Figure 1A-E). Due to the discontinuation of anticoagulants, suspicious thrombosis formed in the stent after 1 year and enlarged after 2 years.
This case showed that PT with SSWAs can be completely eliminated using stenting for the stenosis, suggesting that abnormal hemodynamics may be a further underlying cause for PT compared with SSWAs. We report for the first time that bone remodeling occurred in the diverticulum after stenting. This finding suggests that SSWAs may be the result of abnormal hemodynamics associated with TSS based on further evidence.
TSS is closely related to increased pressure gradients and jet-like blood flow formation[2,6,9]. The long-term impact of jet-like fast flow toward the sigmoid sinus may result in the formation of SSWAs and transmission of the sound[10]. Thus, the role of stenting for TSS is to reduce the trans-stenotic pressure gradient and blood flow velocity to eliminate jet-like fast flow and relevant sound[3].
IIH has been recognized as one of the most common causes of PT; however, the mechanism by which IIH generates PT remains unclear. We hypothesize that TSS and the relevant hemodynamic changes might be closely associated with the occurrence of PT in IIH patients[11].
Bone remodeling around the sigmoid sinus after TSS stenting in PT or IIH patients has not been reported. The bony wall at the portion of the diverticulum gradually ossified after stenting, forming a hardened edge after 2 years, suggesting that the diverticulum was reversible. This phenomenon may be partly associated with hemodynamic changes in the diverticulum after stenting, supporting the above hypothesis that diverticula may develop from the forceful impact of the blood flow on the anterolateral sinus wall.
Trans-temporal sinus wall reconstruction seeks to rebuild the bony barrier to hinder the sound-originating vibration of the sigmoid sinus wall, whereas stenting for TSS is performed to relieve the relevant pressure gradient and “jet-flow”. Both procedures may eliminate PT, and stenting seems to be the better choice as the abnormal hemodynamics associated with TSS still exist after surgical reconstruction. However, this patient was found to have suspected thrombosis in the stent after withdrawal of anticoagulants. Therefore, if stenting is indicated for relief of both PT and elevated intracranial pressure, stenting is probably the better option, and possible complications need to be considered when discussing treatment options[12].
This case implies that PT associated with SSWAs, TSS, and IIH can be cured by stenting for TSS alone. After stenting, bone remodeling may occur in the diverticulum. The results may help to improve the understanding of physiological changes in PT and may influence the choice of treatment in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ocak E S-Editor: Liu M L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Zheng W, Peng Z, Pengfei Z, Jing L, Heyu D, Hongxia Y, Yawen L, Zhengyu Z, Shusheng G, Zhenghan Y, Han L, Zhenchang W. Long-term reactions to pulsatile tinnitus are marked by weakened short-range functional connectivity within a brain network in the right temporal lobe. J Magn Reson Imaging. 2019;49:1629-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Eisenman DJ, Raghavan P, Hertzano R, Morales R. Evaluation and treatment of pulsatile tinnitus associated with sigmoid sinus wall anomalies. Laryngoscope. 2018;128 Suppl 2:S1-S13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 3. | Han Y, Yang Q, Yang Z, Xia J, Su T, Yu J, Jin L, Qiao A. Computational Fluid Dynamics Simulation of Hemodynamic Alterations in Sigmoid Sinus Diverticulum and Ipsilateral Upstream Sinus Stenosis After Stent Implantation in Patients with Pulsatile Tinnitus. World Neurosurg. 2017;106:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Guo P, Sun W, Shi S, Wang W. Patients with pulse-synchronous tinnitus should be suspected to have elevated cerebrospinal fluid pressure. J Int Med Res. 2019;47:4104-4113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Dong C, Zhao PF, Yang JG, Liu ZH, Wang ZC. Incidence of vascular anomalies and variants associated with unilateral venous pulsatile tinnitus in 242 patients based on dual-phase contrast-enhanced computed tomography. Chin Med J (Engl). 2015;128:581-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Zhao P, Lv H, Dong C, Niu Y, Xian J, Wang Z. CT evaluation of sigmoid plate dehiscence causing pulsatile tinnitus. Eur Radiol. 2016;26:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Hewes D, Morales R, Raghavan P, Eisenman DJ. Pattern and severity of transverse sinus stenosis in patients with pulsatile tinnitus associated with sigmoid sinus wall anomalies. Laryngoscope. 2020;130:1028-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Lenck S, Labeyrie MA, Vallee F, Saint-Maurice JP, Guillonnet A, Bernat AL, Vironneau P, Houdart E. Stent Placement for Disabling Pulsatile Tinnitus Caused by a Lateral Sinus Stenosis: A Retrospective Study. Oper Neurosurg (Hagerstown). 2017;13:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Li Y, Chen H, He L, Cao X, Wang X, Chen S, Li R, Yuan C. Hemodynamic assessments of venous pulsatile tinnitus using 4D-flow MRI. Neurology. 2018;91:e586-e593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Tian S, Fan X, Wang Y, Liu Z, Wang L. An in vitro experimental study on the relationship between pulsatile tinnitus and the dehiscence/thinness of sigmoid sinus cortical plate. J Biomech. 2019;84:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Dinkin M, Oliveira C. Men Are from Mars, Idiopathic Intracranial Hypertension Is from Venous: The Role of Venous Sinus Stenosis and Stenting in Idiopathic Intracranial Hypertension. Semin Neurol. 2019;39:692-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Shields LBE, Shields CB, Yao TL, Plato BM, Zhang YP, Dashti SR. Endovascular Treatment for Venous Sinus Stenosis in Idiopathic Intracranial Hypertension: An Observational Study of Clinical Indications, Surgical Technique, and Long-Term Outcomes. World Neurosurg. 2019;121:e165-e171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |