Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2268
Peer-review started: August 23, 2020
First decision: December 21, 2020
Revised: January 1, 2021
Accepted: February 1, 2021
Article in press: February 1, 2021
Published online: April 6, 2021
Processing time: 218 Days and 17.9 Hours
Mechanical thrombectomy (MT) has been demonstrated to be useful for the treatment of ischemic stroke in patients with large vessel occlusions. However, recanalization by MT is not recommended for distal vessels such as second-order branches of the middle cerebral artery and posterior inferior cerebellar artery (PICA). Because of the small size and tortuosity of these arteries, the risks of using the available endovascular devices outweigh the benefits of treatment. However, MT appears to be effective in patients with primary distal vessel occlusion in eloquent areas, those with a high National Institutes of Health Stroke Scale score, and those ineligible for recombinant tissue plasminogen activator therapy. Here, we report the use of MT for treating acute occlusion of the PICA using a direct-aspiration first-pass technique (ADAPT).
In this case, the patient received acute occlusion of the PICA with ADAPT when right internal carotid artery stenting was performed.
With the introduction of advanced endovascular devices, MT may now be a feasible treatment for acute occlusion of the PICA.
Core Tip: Mechanical thrombectomy, such as a direct-aspiration first-pass technique, can be performed in a cautiously selective manner in patients with occlusion of a posterior circulation branch with a smaller size and tortuosity, such as the posterior inferior cerebellar artery, and obtain a good clinical outcome.
- Citation: Zhang HB, Wang P, Wang Y, Wang JH, Li Z, Li R. Mechanical thrombectomy for acute occlusion of the posterior inferior cerebellar artery: A case report. World J Clin Cases 2021; 9(10): 2268-2273
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2268.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2268
Ischemic stroke continues to be a leading cause of death and disability worldwide. Various guidelines recommend endovascular treatment, in addition to intravenous thrombolysis, for acute cerebral infarctions with large vessel occlusion. Mechanical thrombectomy (MT) has been demonstrated to be useful for the treatment of ischemic stroke in patients with large vessel occlusions[1-3]. However, for acute cerebral infarctions caused by occlusion of the branches involved in posterior circulation, such as the posterior inferior cerebellar artery (PICA), the anterior inferior cerebellar artery, and the posterior cerebral artery, the best treatment currently available is intravenous thrombolysis. Nevertheless, with the development of interventional materials, MT devices have improved, and guide wires and catheters have become more flexible, making it safer to reach the diseased area. Thus, MT is now more widely used in neurovascular interventions, such as the treatment of occlusion of the M2 and M3 segments of the middle artery[4,5]. Here, we report a case of acute occlusion of the PICA with successful recanalization using a direct-aspiration first-pass technique (ADAPT).
A 72-year-old man presented with acute-onset left upper limb weakness and numbness that had persisted for 3 h.
The patient had a history of smoking (50 packs/year) and alcohol consumption.
No past illness.
No personal and family history.
The initial National Institutes of Health Stroke Scale (NIHSS) score was 3 because alalia and grade 3 weakness and numbness in the left upper limb were present.
The patient’s blood glucose level was 5.7 mmol/L.
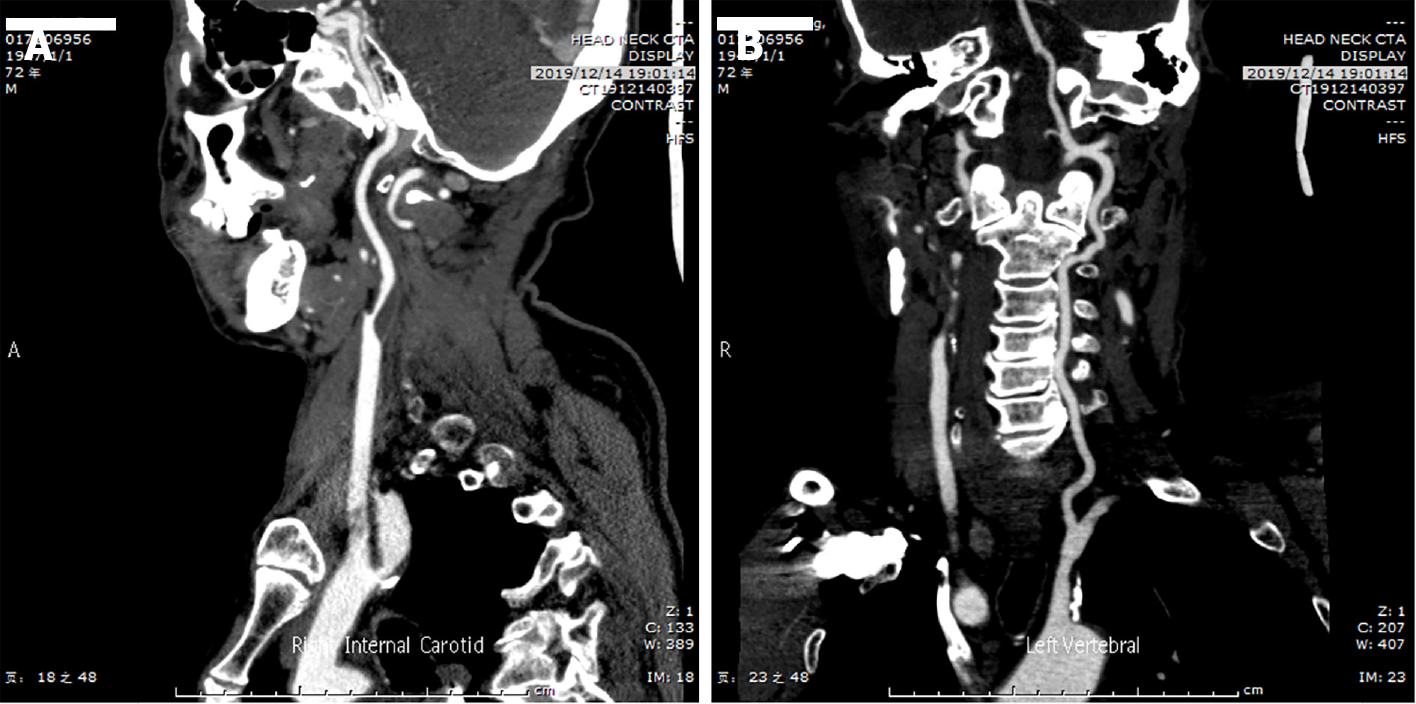
Brain computed tomography (CT) and electrocardiography findings were normal. CT angiography showed a soft plaque in the initial portion of the right internal carotid artery, with 80% stenosis, and a mixed plaque in the left subclavian artery (Figure 1).
The patient was diagnosed with acute ischemic stroke.
After intravenous thrombolysis was performed, CT angiography showed a soft plaque in the initial portion of the right internal carotid artery, with 80% stenosis, and a mixed plaque in the left subclavian artery (Figure 1). Fortunately, the patient's symptoms were completely relieved.
Twenty-four hours after intravenous thrombolysis, the patient had no signs of hemorrhage on a brain CT scan, and his NIHSS score was 0. A right internal carotid artery stent (XACT 6-8-40, Abbott, United States) was placed after aspirin (100 mg/d) and clopidogrel (75 mg/d) had been administered for > 5 d. During the procedure, the patient complained of dizziness, nausea, and profuse sweating, with blood pressure of 209/108 mmHg and a heart rate of 115 beats/min, indicating cerebral hyperperfusion syndrome. Urapidil was administered intravenously (12.5 mg) to achieve a systolic blood pressure of 90-120 mmHg, but the patient's symptoms were not relieved even after 10 min.
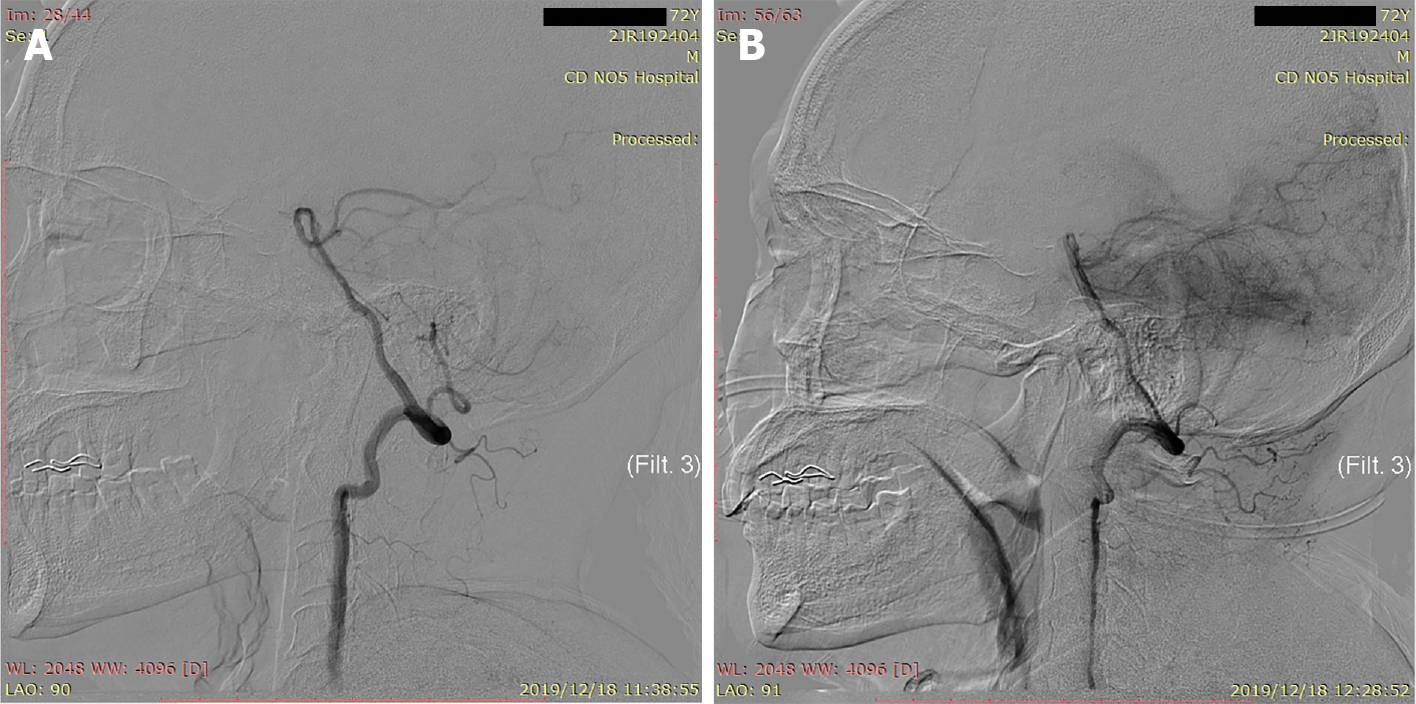
Considering the patient's dizziness and nausea, we immediately performed bilateral vertebral and basilar artery angiography, revealing occlusion of the left PICA (Figure 2). Given that the patient had no history of atrial fibrillation, we believed that the embolus had arisen from the left subclavian artery. We decided to perform intra-arterial thrombectomy for left PICA occlusion. Under general anesthesia, the V2 section of the left vertebral artery was accessed using a 6 F guide catheter (Boston Scientific, United States) through an 8 F common femoral artery sheath. The left PICA stroke was accessed using a 3MAX suction catheter (Penumbra, United States) over a 0.36 mm microwire (Synchro-14, Stryker, United States) using ADAPT. Intermittent staccato movement of blood in the pump tubing without free flow strongly suggested engagement and partial engulfment of the thrombus in the 3MAX tip. During this phase, a 50-mL syringe was connected to a three-way tap with the proximal 3MAX catheter to increase the extra suction force as slow traction was then applied to the 3MAX, especially at the tortuous part of the vertebral artery. A dark red embolus was observed at the tip of the suction catheter, indicating complete recanalization of the occluded PICA after 40 min. We refer to this treatment technique as enhanced mini-ADAPT.
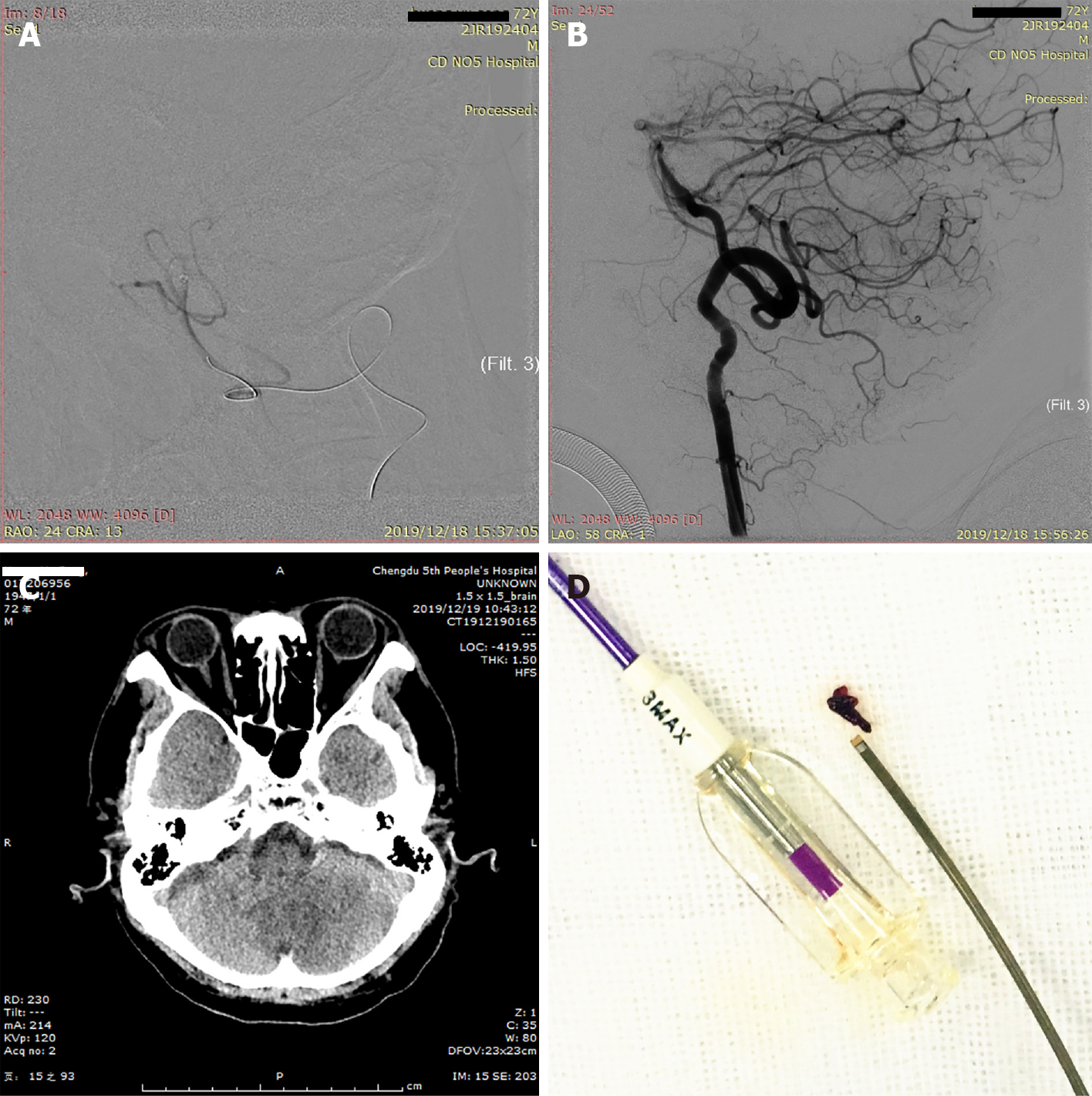
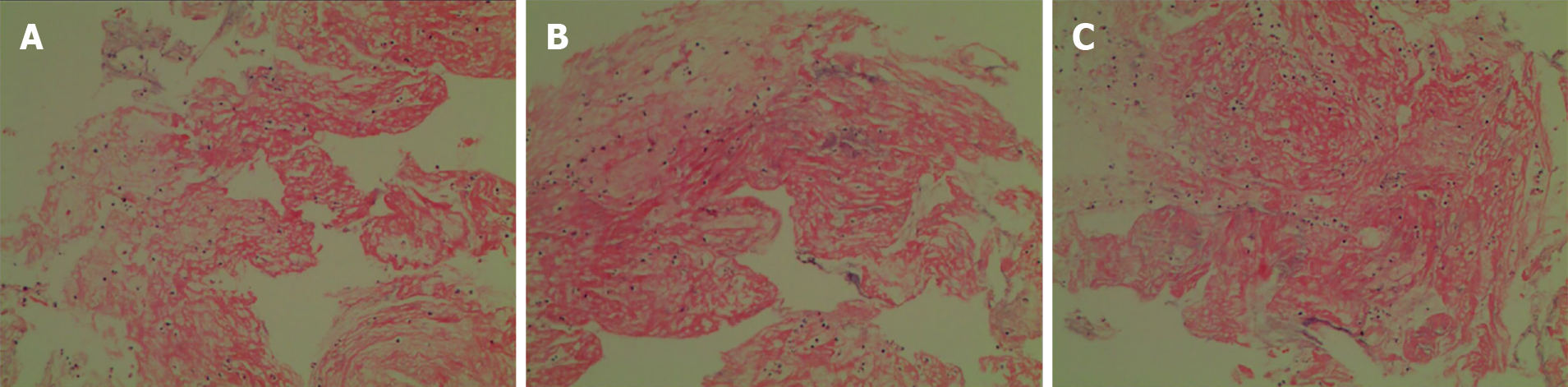
At the end of the procedure, the revascularization result was graded 3 according to the Thrombolysis in Cerebral Infarction (TICI) score classification. Noncontrast CT on the first day after surgery showed a low-density focus in the left cerebellum. The aspirated thrombus is shown in Figure 3. The patient recovered fully without any neurological deficits except for vertigo on day 1 after MT. Pathological results suggested fibrinous exudate with inflammatory cell infiltration (Figure 4).
In this case, nonoperative lateral arterial embolism occurred during the operation because the source of the embolus was the artery plaque of the left subclavian artery. According to Alakbarzade et al[6], the incidence of arterial thromboembolism during digital subtraction angiography is approximately 0.34%-1%[6-8]. Occlusion of the distal artery in an eloquent territory can result in severe symptoms, as evidenced by a high NIHSS score. The PICA is the largest and longest branch of the intracranial branch of the vertebrobasilar artery system. It mainly supplies the medulla oblongata, fourth ventricle, choroid plexus, and cerebellum and has complex, tortuous, and varied regional blood supply patterns. Its occlusion can lead to lateral medulla oblongata infarctions on the dorsal side of the inferior olive, causing ischemic damage; occlusion of the dominant side of the PICA can result in large-scale cerebellar hemisphere infarction. Secondary cerebral edema compresses the median foramen, lateral foramen, and fourth ventricle, causing obstructive hydrocephalus. There were two reasons for performing MT in this scenario. First, the patient had severe vertigo, nausea, and vomiting, and the risk of severe Wallenberg syndrome was extremely high. Second, the patient had undergone carotid artery stenting and required postoperative antiplatelet therapy. If cerebellar infarction, cerebral edema, and obstructive hydrocephalus occurred, decompressive craniectomy would increase the risk of thrombosis in the stent. Several reports[9,10] have shown that it is safe and feasible to use stent-assisted embolization for posterior inferior cerebellar aneurysms. The PICA is divided into four segments, and the patient's PICA was occluded at the end of the first segment. Before the MT operation, we measured the diameter of the first and second segments of the PICA, which we found to be 1.42-1.5 mm. Therefore, it was ensured that the microcatheter would safely reach the PICA occlusion site for the operation. The 3MAX system is a suction catheter from Penumbra that consists of a 3.8 F distal outer diameter catheter and a continuous suction pump. It can be used to quickly restore blood flow after small blood vessel occlusion. 3MAX has a soft tip; the inner diameter of the distal catheter is 0.89 mm, the inner diameter of the proximal catheter is 1.09 mm, and the working length is 153 cm. Owing to this design, the tip of the catheter produces the best suction force for thrombi that are occluding small blood vessels. According to Altenbernd et al[11] , 3MAX is safe and effective for M2 and M3 thrombus aspiration; the recanalization rate 2b-3 is 100%, the level 3 rate is 77.4%, the 90-d functional independence rate is 96.8% and the intracranial symptomatic hemorrhage rate is 0. 3MAX is softer than the tip of a microcatheter. It has a stronger attractive force and can effectively latch onto the thrombus. Therefore, in this case, we used 3MAX instead of a microcatheter.
In cases where posterior circulation branch vessels, such as the PICA, are occluded, aspiration with 3MAX could be a safe and feasible treatment. However, to achieve a good and successful outcome, the advantages and disadvantages should be carefully weighed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Adams JD, Ahuja CK S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Li X
| 1. | Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4460] [Cited by in RCA: 4868] [Article Influence: 486.8] [Reference Citation Analysis (0)] |
| 2. | Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3948] [Cited by in RCA: 4280] [Article Influence: 428.0] [Reference Citation Analysis (0)] |
| 3. | Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4180] [Cited by in RCA: 4542] [Article Influence: 454.2] [Reference Citation Analysis (0)] |
| 4. | Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, Sheth SA. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg. 2018;10:620-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 130] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 5. | Chen CJ, Wang C, Buell TJ, Ding D, Raper DM, Ironside N, Paisan GM, Starke RM, Southerland AM, Liu K, Worrall BB. Endovascular Mechanical Thrombectomy for Acute Middle Cerebral Artery M2 Segment Occlusion: A Systematic Review. World Neurosurg. 2017;107:684-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Alakbarzade V, Pereira AC. Cerebral catheter angiography and its complications. Pract Neurol. 2018;18:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Dawkins AA, Evans AL, Wattam J, Romanowski CA, Connolly DJ, Hodgson TJ, Coley SC. Complications of cerebral angiography: a prospective analysis of 2,924 consecutive procedures. Neuroradiology. 2007;49:753-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Choudhri O, Schoen M, Mantha A, Feroze A, Ali R, Lawton MT, Do HM. Increased risk for complications following diagnostic cerebral angiography in older patients: Trends from the Nationwide Inpatient Sample (1999-2009). J Clin Neurosci. 2016;32:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Cho DY, Choi JH, Kim BS, Shin YS. Comparison of Clinical and Radiologic Outcomes of Diverse Endovascular Treatments in Vertebral Artery Dissecting Aneurysm Involving the Origin of PICA. World Neurosurg. 2019;121:e22-e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Kim MJ, Chung J, Kim SL, Roh HG, Kwon BJ, Kim BS, Kim TH, Kim BM, Shin YS. Stenting from the vertebral artery to the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2012;33:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Altenbernd J, Kuhnt O, Hennigs S, Hilker R, Loehr C. Frontline ADAPT therapy to treat patients with symptomatic M2 and M3 occlusions in acute ischemic stroke: initial experience with the Penumbra ACE and 3MAX reperfusion system. J Neurointerv Surg. 2018;10:434-439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |