Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2247
Peer-review started: October 21, 2020
First decision: December 3, 2020
Revised: December 14, 2020
Accepted: January 27, 2021
Article in press: January 27, 2021
Published online: April 6, 2021
Processing time: 160 Days and 1.7 Hours
Suspension training (SET) is a method of neuromuscular training that enables the body to carry out active training under unstable support through a suspension therapy system. However, there have been few reports in the literature on the application of SET to anterior cruciate ligament reconstruction (ACLR) patients. It is not clear what aspects of the patient's function are improved after SET.
To investigate the effect of SET on the neuromuscular function, postural control, and knee kinematics of patients after ACLR surgery.
Forty participants were randomized to an SET group or a control group. The SET group subjects participated in a SET protocol over 6 wk. The control group subjects participated in a traditional training protocol over 6 wk. Isokinetic muscle strength of the quadriceps and hamstrings, static and dynamic posture stability test, and relative translation of the injured knee were assessed before and after training.
The relative peak torque of the quadriceps and hamstrings in both groups increased significantly (P < 0.001), and the SET group increased by a higher percentage than those in the control group (quadriceps: P = 0.004; hamstrings: P = 0.011). After training, both groups showed significant improvements in static and dynamic posture stability (P < 0.01), and the SET group had a greater change than the control group (P < 0.05). No significant improvement on the relative translation of the injured knee was observed after training in either group (P > 0.05).
Our findings show that SET promotes great responses in quadriceps and hamstring muscle strength and balance function in ACLR patients.
Core Tip: In our study, suspension training (SET) was applied to anterior cruciate ligament reconstruction (ACLR) post-rehabilitation as a new sports training method. First, this study provides the first evidence for the feasibility of SET in ACLR rehabilitation. Second, this study presents a detailed and ACLR-targeted SET program. Further, we demonstrated the effect of the SET on neuromuscular function, postural control, and knee kinematics in ACLR patients.
- Citation: Huang DD, Chen LH, Yu Z, Chen QJ, Lai JN, Li HH, Liu G. Effect of suspension training on neuromuscular function, postural control, and knee kinematics in anterior cruciate ligament reconstruction patients. World J Clin Cases 2021; 9(10): 2247-2258
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2247.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2247
Anterior cruciate ligament (ACL) rupture is common during sports and activities[1]. ACL reconstruction (ACLR) is a frequent surgical procedure to restore functional joint stability after an ACL injury[1,2]. After ACLR surgery, the strength of the patient's injured limb is significantly reduced due to muscular atrophy and articular muscle inhibition[3,4], which increases the risk of re-injury of the knee joint and accelerates the degeneration of articular cartilage, leading to the development of osteoarthritis[5-8]. Common physical therapy for ACLR patients includes instruction, bracing, cryotherapy, joint mobility training, muscle strength training, gait reeducation, and neuromuscular training[9,10]. Neuromuscular training is an important part of current ACLR rehabilitation[9]. Studies have shown that neuromuscular training can improve muscle strength, correct abnormal biomechanics, and enhance lower limb neuromuscular control, thus reducing the incidence of re-injury in ACLR patients[11-13]. Myer et al[14] showed that a progressive, end-stage regressive neuromuscular training program could improve lower limb muscle strength and correct the abnormal distribution of plantar pressure in ACLR athletes. Kibele et al[15] reported that neuromuscular training resulted in a significantly greater increase in knee stability by using a balance ball. However, Cooper et al[16] found that neuromuscular training with a balance board/Swiss ball did not significantly improve the muscle strength and balance function of ACLR patients. Therefore, different neuromuscular training techniques or different design schemes may lead to different rehabilitation effects.
Suspension training (SET) is a method of neuromuscular training that enables the body to carry out active training under unstable support through a suspension therapy system[17]. The training mode includes muscle relaxation training, joint motion training, traction, joint stability training, sensory and motor coordination training, and muscle potential energy training[18]. The personalized schemes of SET could be designed according to the different functional levels and functional requirements[19]. Moreover, this method has been widely used in the field of sports and rehabilitation because of its simpler operation and cheaper training equipment[19,20]. Studies have shown that adding SET to the rehabilitation program of healthy athletes can significantly improve quadriceps muscle strength[21]. In the field of rehabilitation, SET is mainly applied to bone and joint diseases, sports injuries, nerve injuries, etc.[20,22]. However, there have been few reports in the literature on the application of SET to the postoperative rehabilitation of ACLR patients.
Therefore, the primary purpose of the study was to determine the effect of SET on neuromuscular function, postural control, and knee kinematics in ACLR patients.
A total of 40 patients were initially included in this study, and all underwent unilateral ACLR for the first time with a healthy opposite leg and volunteered to participate in a 6-wk intervention program after finishing 6-mo standard early rehabilitation. The inclusion criteria were: (1) Age 18 to 45 years; (2) ACL injuries diagnosed by arthroscopy or magnetic resonance examination; and (3) ACLR operation performed by the same experienced joint surgeon using a semitendinosus or gracilis tendon graft. The exclusion criteria were: (1) Previous injury or operation on the injured knee; (2) Joint injury that might influence the rehabilitation; (3) History of central or peripheral neurological impairment; and (4) Concomitant with any cardiac, pulmonary, or metabolic conditions. All admitted subjects provided informed consent in accordance with the Declaration of Helsinki[23]. All protocols were approved by the institutional review board.
All the patients were mainly recruited from the rehabilitation clinic and sports medicine clinic of the hospital. The rehabilitation treatment of the patients was completed in the rehabilitation center, and the evaluation was performed in the motor function assessment center.
This is a single-center, prospective, randomized, controlled clinical trial that followed the CONSORT guidelines. The sample size was based on the expected number of ACLR patients in the facility and previous pilot studies. Patients who met the criteria were randomized to an SET group or a control group according to a computer-generated form that was kept in a sealed, opaque envelope. A designated physician outside the team administered randomization. The primary investigators in charge of outpatient service were responsible for the recruitment, qualification, and allocation of patients. All data were analyzed by an experienced therapist who was blinded to the group information.
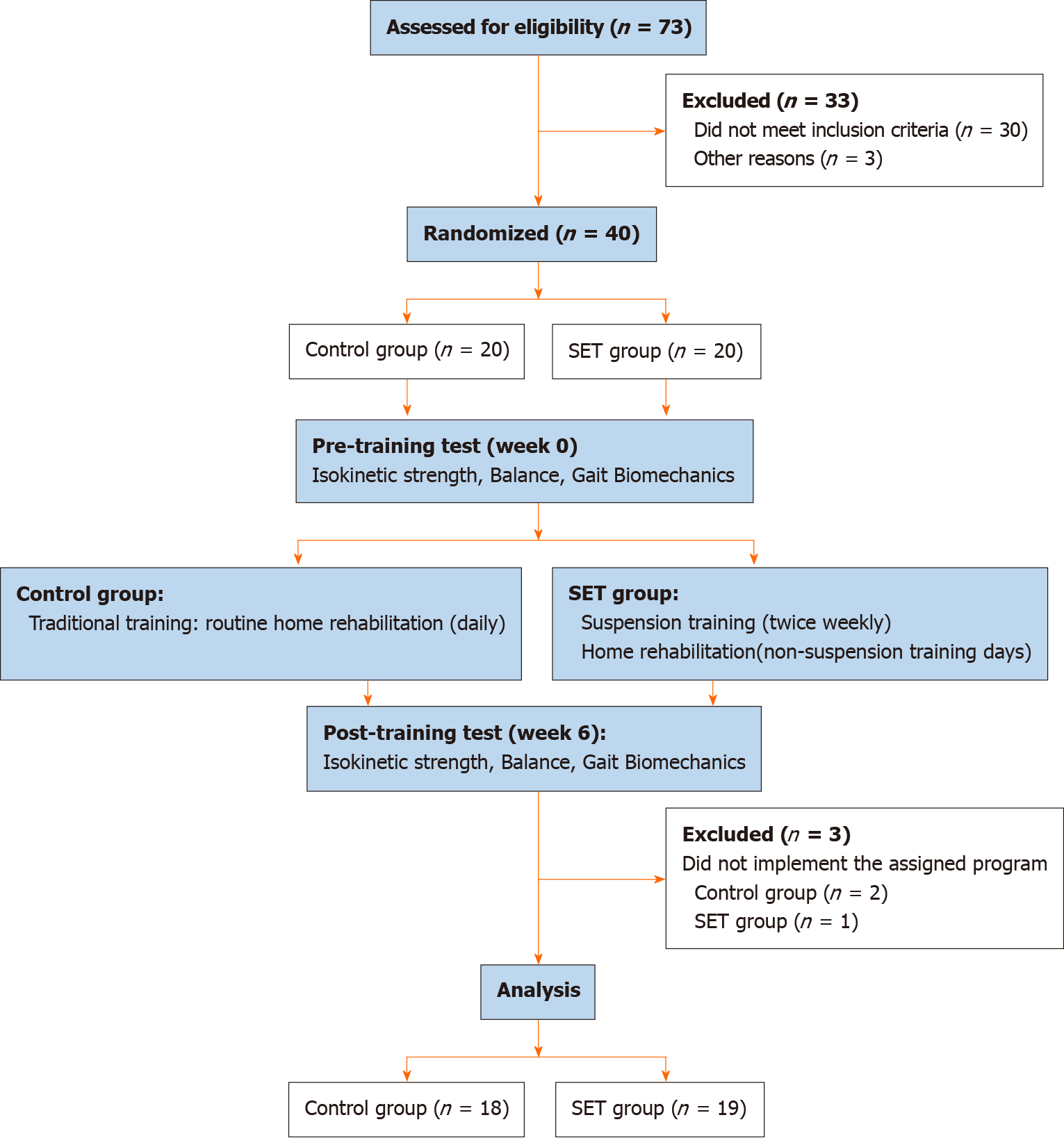
The SET group subjects participated in a SET training protocol over 6 wk, which included SET (twice weekly) and routine home rehabilitation (non-SET days). The control group subjects participated in a traditional training protocol over 6 wk, which included daily routine home rehabilitation (the supplement included detailed home rehabilitation program; Supplementary Table 1). Three patients later were excluded from the study for not complying with the course of rehabilitation. Consequently, 37 patients completed all protocol and testing sessions and were included in the data analysis (Figure 1).
SET
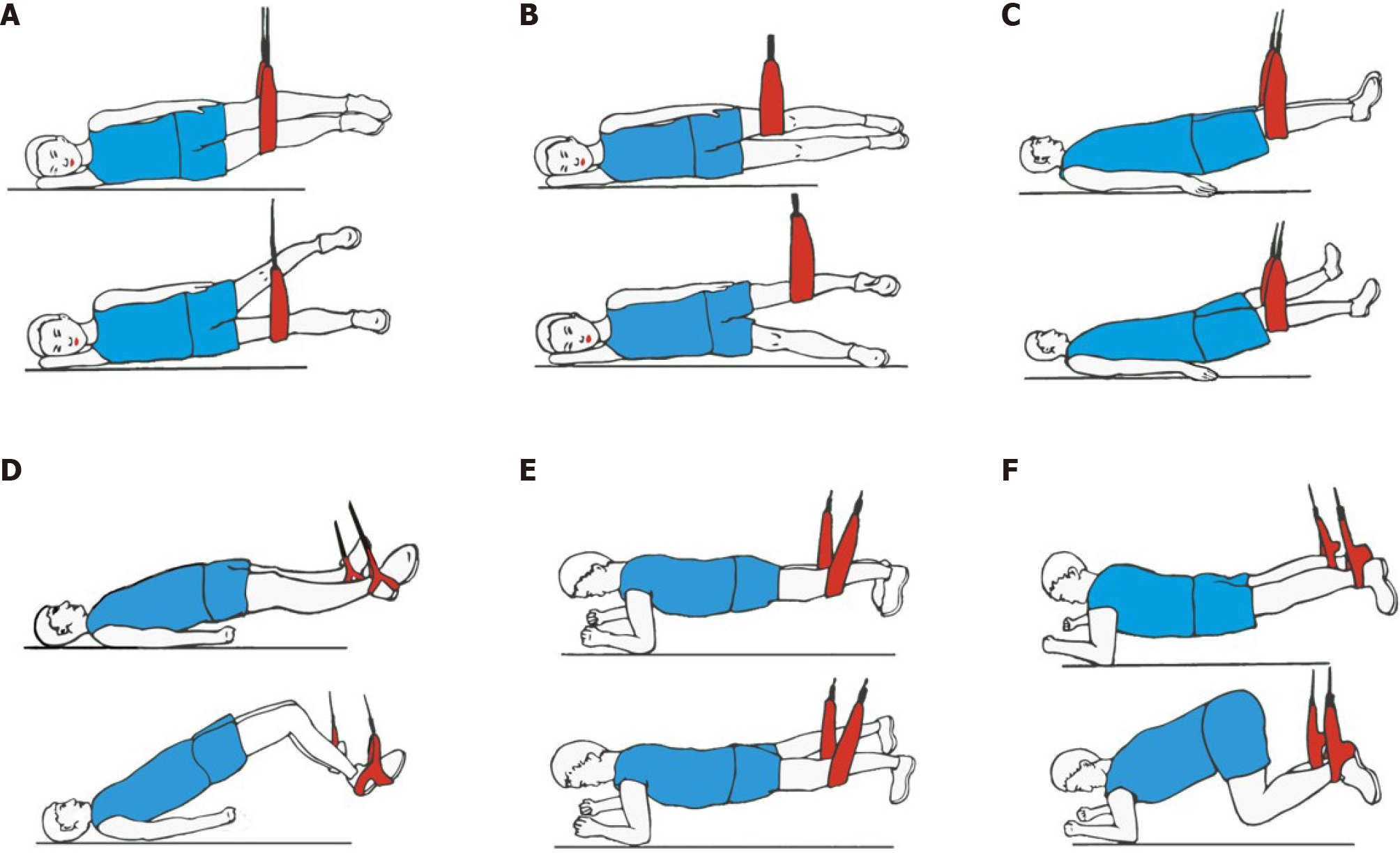
The SET group performed the SET program twice a week for 6 consecutive weeks. Four sets of 10-repetition maximum were performed for each exercise, with 1-2 min of rest between sets. A dedicated system of adjustable slings was used throughout the study with inelastic ropes (Figure 2). All treatments were performed by three designated therapists who strictly followed the designed program when implementing the patients' training program.
Affected side position: The patient was placed in the lateral position on the affected side with leaning on one elbow. With the anchor point of the suspension rope located on the superior border of the affected patella, the patient was supposed to place the affected leg on the adjusted suspension rope and press hard on the rope until the shoulder, hip, and leg were in line. The healthy leg was abducted to maximal joint angle and held for 2 s before returning to the starting position without being in contact with the sling ropes.
Healthy side position: The patient was placed in the lateral position on the healthy side with leaning on one elbow. With the anchor point of the suspension rope located on the superior border of the affected patella, the patient was supposed to place the affected leg on the adjusted suspension rope and press hard on the rope until the shoulder, hip, and leg were in line. The healthy leg was abducted to maximal joint angle and held for 2 s before returning to the starting position.
Supine position: The patient was placed in the supine position. (1) He/she was supposed to keep his/her hands across the chest and place the affected leg on the rope with the anchor point of the suspension rope located on the popliteal fossa of the leg. And then, the affected leg was pressed hard down on the rope and the healthy leg was abducted to 45° joint angle and held for 2 s before returning to the starting position; and (2) The patient was supposed to hang both legs on the two ropes and place arms in contact with the floor. And then, he/she contracted the trunk and both knees and held the position for 2 s before returning to the starting position.
Prone position: The patient was placed in the prone position with leaning on their elbows. (1) He/she was supposed to place the affected leg on the rope with the anchor point of the suspension rope located on the superior border of the affected patella. And then, the affected leg was pressed hard down on the rope to lift the upper body, hips, and knees. The healthy leg was abducted to 45° joint angle and held the position for 2 s before returning to the starting position; and (2) The patient was supposed to place both legs on the two ropes. And then, they contracted their trunk and both knees and held the position for 2 s before returning to the starting position.
The patients should perform regular warm-up exercises (10 min) on a bicycle dynamometer before the test. Muscle strength was evaluated using the concentric protocol module of IsoMed 2000 (D&R Ferstl). Before the formal test, the patients performed five repetitions of leg flexion and extension exercises to adjust to the test pattern. After a 2-min rest, the patients were asked to perform 10 repetitions with maximum effort at an angular velocity of 60°/s between 10° and 90° of knee flexion for both legs separately. The test of the uninjured leg was performed first and a rest for 5 min was given before another test mode. The symmetry index refers to the ratio index of the scaled peak moment on the injured side and the non-injured side.
The balance was assessed by using a stabilometer platform (Tecnobody, PK 254, Italy). Two different test modes were performed, static posture stability test (level 12, stable platform) and dynamic posture stability test (level 4, unstable platform). The measurement of static postural stability involves the swing area of the center of gravity (Area). The higher score the Area index, the worse the static posture stability[24,25]. The measurement of dynamic stability includes the multi-axis mean trajectory difference (average trace error, ATE). The smaller the mean trajectory error, the better the proprioceptive sensitivity of the subjects[26,27]. Each participant was given three successful tests for each test mode.
Kinematic data of both knees were recorded and analyzed with a portable infrared optoelectronic motion capture system (Opti-Knee; Shanghai Innomotion Inc.). Before the test, each subject was required to walk on a test treadmill at a speed of 3 km/h to adjust to the test pattern. The gait cycle and the movement of the knee joint were tracked and recorded with a double-ended stereoscopic infrared camera and high-speed camera. Each participant was given three successful tests for each limb.
All data were statistically analyzed using IBM SPSS Statistics Version 24.0 (IBM Corp, Chicago, IL, United States). The data are expressed as the mean ± SD with 95% confidence intervals. Independent-samples t-test and Fisher’s exact test were used to compare the baseline characteristics between the SET and control groups. The normal distribution of data was assessed using the Shapiro-Wilks test (P > 0.05), and homogeneity of variance (where appropriate) was tested by Levene’s test (P > 0.05). Differences between and within groups were performed. An independent-samples t-test was used to compare isokinetic muscle strength, balance function data, and gait biomechanics data between groups. A paired-samples t-test was used to compare isokinetic muscle strength, balance function data, and gait biomechanics data before and after rehabilitation.
For reasons unrelated to the study, three participants did not complete the study protocol, and only 37 patients completed the full rehabilitation program (SET group: n = 19, Control group: n = 18). There was no significant difference in any of the anthropometric variables between the two groups (Table 1). No adverse events occurred.
| Group | |||
| Control (n = 18) | SET (n = 19) | P value | |
| Mean age | 28.0 ± 6.9 | 28.5 ± 5.8 | 0.82 |
| Gender (male/female) | 14/4 | 16/3 | 0.69 |
| Body mass index (kg/m2) | 22.07 ± 2.59 | 23.78 ± 3.34 | 0.15 |
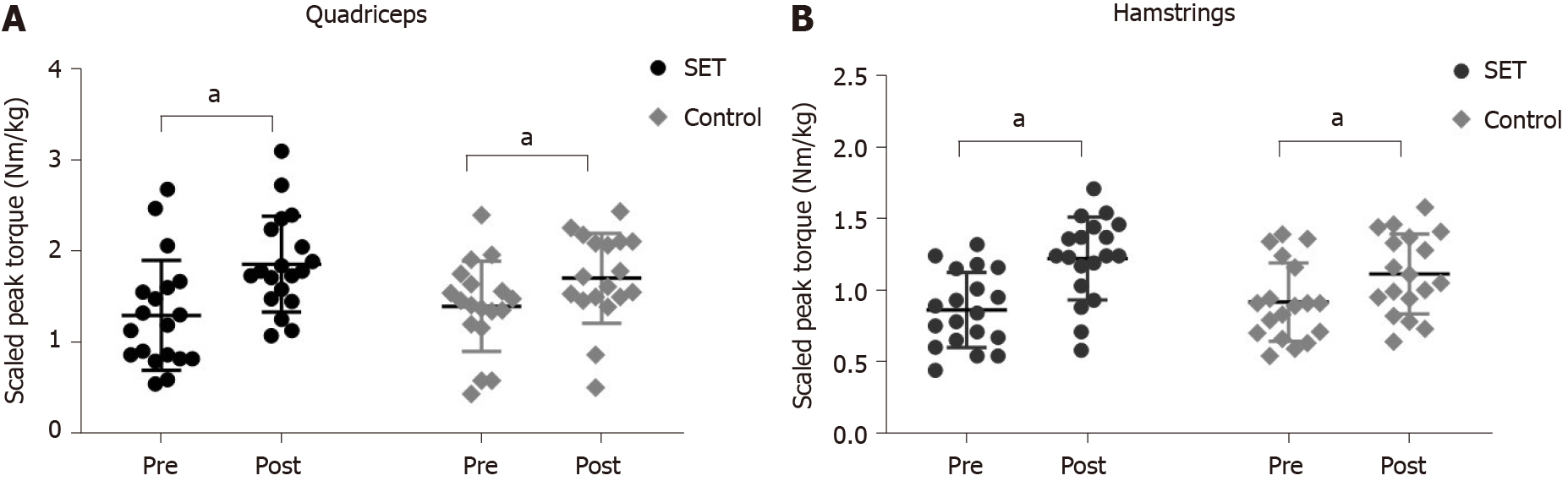
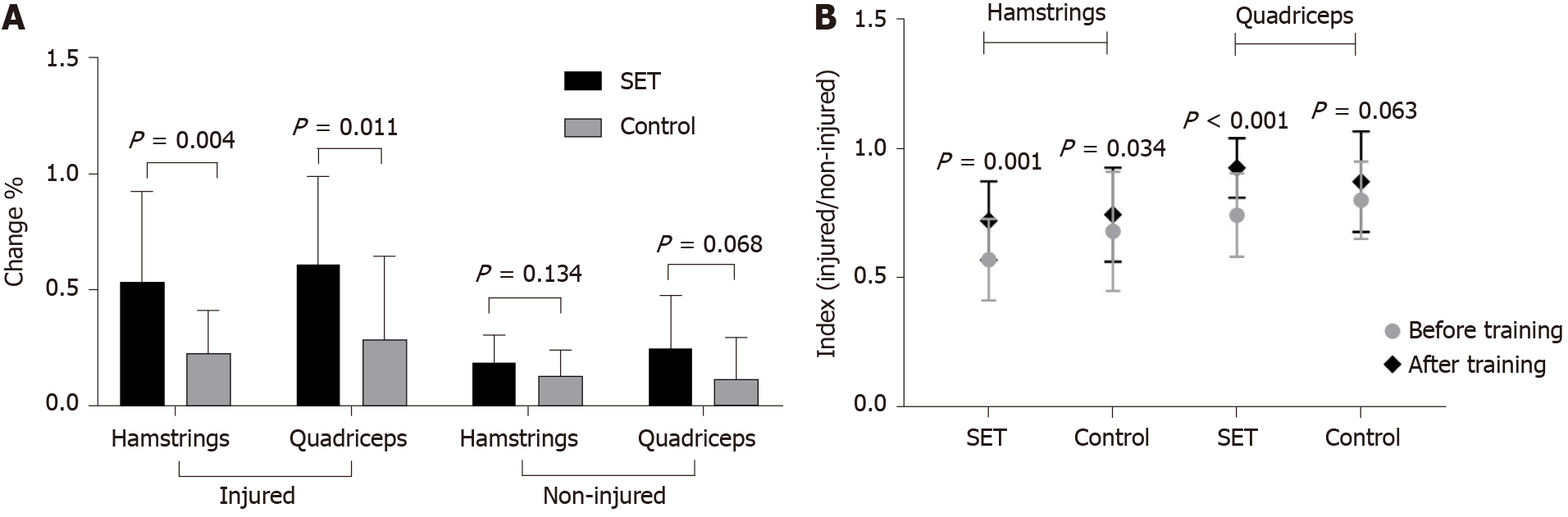
In terms of isometric muscle strength test, after 6 wk of training, the relative peak torque of the quadriceps and hamstrings in the injured leg of both groups increased significantly (P < 0.001) (Figure 3), and the relative peak torque of the quadriceps and hamstrings in the injured leg of the SET group increased by a higher percentage than those in the control group (P = 0.004 and P = 0.011). There was no significant difference between the SET group and the control group in the increased percentage of the relative peak torque of the uninjured leg (Figure 4A). The symmetry index of the quadriceps femoris in both groups was significantly higher than that before training (SET: P = 0.001, Control: P = 0.034). In the SET group, the hamstring symmetry index of the operative leg increased significantly (P < 0.001), while the hamstring symmetry index of the control group did not change significantly (P = 0.063) (Figure 4B).
In the balance stability test, significant decline of Area and ATE were observed in both groups (P < 0.001), and the SET group had a significantly greater decrease than the control group (P < 0.05) (Table 2). In the gait biomechanics test, there was no significant difference in relative translation of the injured knee in either group after training (P > 0.05) (Table 3).
| Measurement | Control | SET | ||||
| Pre | Post | P value | Pre | Post | P value | |
| Swing area (mm2) | 313.56 ± 74.26 (276.63 to 350.49) | 293.22 ± 69.31 (258.75 to 327.69) | < 0.01 | 375.63 ± 188.58 (284.74 to 466.52) | 318.05 ± 154.29a (243.69 to 392.42) | < 0.01 |
| ATE-injured (%) | 36.56 ± 7.85(32.65 to 40.46) | 30.56 ± 7.24 (26.96 to 34.15) | < 0.01 | 39.11 ± 12.81 (32.93 to 45.28) | 26.42 ± 6.20c (23.43 to 29.41) | < 0.01 |
| ATE-uninjured (%) | 30.72 ± 7.49(27.0 to 34.45) | 26.44 ± 6.28 (23.32 to 29.57) | < 0.01 | 33.05 ± 8.64 (28.89 to 37.22) | 24.79 ± 4.88b (22.44 to 27.14) | < 0.01 |
| Measurement | Control | SET | ||||
| Pre | Post | P value | Pre | Post | P value | |
| Relative translation (mm) | ||||||
| Anterior-posterior | 1.21 ± 0.44 (0.99 to 1.43) | 1.09 ± 0.28 (0.95 to 1.23) | 0.32 | 1.30 ± 0.51 (1.05 to 1.55) | 1.38 ± 0.43 (1.17 to 1.59) | 0.55 |
| Internal-external | 1.23 ± 0.48 (0.99 to 1.47) | 1.17 ± 0.4 (0.97 to 1.37) | 0.58 | 1.28 ± 0.49 (1.04 to 1.52) | 1.44 ± 0.6 (1.15 to 1.73) | 0.29 |
| Proximal-distal | 0.81 ± 0.38 (0.62 to 1.0) | 0.82 ± 0.31 (0.67 to 0.97) | 0.75 | 0.74 ± 0.23 (0.63 to 0.85) | 0.72 ± 0.23 (0.61 to 0.83) | 0.75 |
This study is the first to examine the effect of SET in the ACLR rehabilitation program. The main findings of this clinical study are as follows: (1) SET resulted in a significant increase in quadriceps and hamstring muscle strength and strength symmetry; (2) SET resulted in greater improvements in the balance stability of the lower limbs; and (3) SET had a limited effect on the injured knee kinematics.
The functioning of quadriceps and hamstring muscles is a critical factor in the patients' ability to prevent reinjury after ACLR surgery[1,28]. Consequently, it is of great importance to regain quadriceps and hamstring strength after surgery. Similar to previous studies, we found that our patients did not fully regain the muscle strength of their reconstructed leg despite a 6-mo intensive rehabilitation program[29]. The main causes of muscle weakness include poor neuromuscular control and substantial muscle atrophy, which are also major risk factors for the postoperative reinjury of the knee joint[28].
SET is a special kind of neuromuscular training, and previous studies have shown that neuromuscular training can improve strength[21]. Therefore, adding SET to an athletes' rehabilitation program can significantly enhance the power of the quadriceps[30]. Furthermore, the application of SET to patients after knee arthroplasty can achieve a better rehabilitation effect[22]. In this study, SET was applied to the postoperative rehabilitation of ACLR patients. After SET, the relative peak torque of the quadriceps and hamstrings in the injured leg of the SET group showed greater improvements than before. The SET group demonstrated a more significant percentage of change in isokinetic torques of the injured leg than the control group. It can be speculated that the use of SET training resulted in a significant improvement in quadriceps and hamstring strength. Meanwhile, compared with conventional training, SET can more quickly improve muscle strength and shorten the development period of rehabilitation.
In this study, SET obtained reliable results in improving the symmetry of the lower limb strength in ACLR patients. Since the training program focuses on the rehabilitation of the injured leg, there was no difference in the increased percentage of the uninjured knee strength between the two groups. In the design of the SET program, open kinetic chain exercises and closed kinetic chain exercises were combined. The movements (A, B, C, and E) follow the same pattern as the open chain movement of the healthy leg and the closed chain movement of the injured limb. Previous studies have confirmed that the rehabilitation program for ACLR patients can obtain a greater improvement of the rehabilitation effect after the combination of the open kinetic chain and closed kinetic chain[31]. The strength of the quadriceps muscle is a critical factor for the stability of knee joints in patients after ACLR surgery[4,28]. SET could be targeted to activate the weak chain of the muscle of the lower limb[32,33]. A report has confirmed that both close-chain and open chain movements under SET can greatly activate the quadriceps femoris[21]. Due to severe muscle atrophy after ACLR surgery, muscle asymmetry is considered a risk factor for secondary knee injury[3]. The quadriceps index and hamstring index can well reflect the symmetry of the strength between the injured side and the contralateral side. A larger index is associated with a better symmetry of bilateral strength[28]. In our study, we found that the quadriceps and hamstrings peak torque of the injured side recovered to “75%” and “57%” of the contralateral side before training in the SET group. After training, the injured side's quadriceps and hamstring indexes were “93%” and “72%”, respectively, which were significantly improved compared with the control group. It can be speculated that SET has a more significant effect on the improvement of the double lower limb strength symmetry. This finding suggests that adding SET to the rehabilitation process could effectively improve the muscle strength and symmetry of the lower limbs, which helps to reduce the risk of re-injury of the reconstructed ACL in ACLR patients.
After 6 wk of training, static balance and dynamic balance were improved in both groups, and the SET group had a greater improvement than the control group. This result was expected given that the balance stability of the lower limbs is significantly related to the ability of neuromuscular control. What's more, dynamic balance stability is not only related to the local stabilizing muscles around the joint but is also affected by the stability and coordination of the other muscles of the body[34].
Studies have proven that training with an unstable plane results in the high internal contraction of muscles and overloading if the instability difficulty of this plane is moderate, providing an effective training environment for muscles[14,15,35]. However, most of the recommended core training modes only work in one or two motion planes[12]. The key of SET is motion control. By providing a three-dimensional unstable training environment, the subjects were required to perceive the position of the body in three-dimensional space to maintain the stability of the position. The instability of the training plane is higher, and the core muscles of the patient can bear more exercise load during the training[32]. SET can promote the coordinated contraction of the trunk, hip, and knee, recruit more muscle groups, and activate local stable muscle groups during the coordinated contraction of the overall muscles, which is helpful to improve the dynamic balance function of the lower limbs[33]. It can be inferred that the application of SET to ACLR patients can not only effectively activate the strong contraction of the trunk and lower limb muscles and improve the neuromuscular control ability but also promote the strength growth of local muscles around the knee joint[36], thus enhancing the postural control of ACLR patients.
In the present study, we discuss the injured knee kinematics by performing a calculation of the relative motion of the tibial femur joint. However, there was no significant improvement in both groups after training. The relative displacement of the knee joint on the coronal plane mainly reflects the varus and valgus of the joint. Moderate rotation of the tibia occurs during a normal gait cycle, while anterior-posterior and proximal-distal relative translation reflects the track of the tibial femur joint in the sagittal plane[37]. The relative motion of the tibial femur joint was affected by soft tissue and muscle around the knee. In this study, muscle strength around the knee joint was increased equably after training, which avoided the significant kinematic changes of the knee joint due to the imbalance of the strength. It is known that factors affecting the motor function of the lower limbs include the coordinated movement of multiple joints and muscles, and changes in the hip and ankle joints will also affect the walking pattern[38]. In addition, ACLR patients experienced a long period of knee braking in the early postoperative period, resulting in error motor adaptation[39]. It can be speculated that short-term training has a very limited impact on unilateral joint movement. Future studies will be needed to design a long-term, systematic SET program and explore its impact on the biomechanical changes of the hip and ankle joints of ACLR patients.
In conclusion, SET promotes great responses in quadriceps and hamstring muscle strength and balance control in ACLR patients. More importantly, the SET program designed for ACLR patients is worthy of clinical promotion, and it also has reference value for the design of SET programs for other orthopedic postoperative patients.
Suspension training (SET), a method of neuromuscular training that enables the body to carry out active training under unstable support through a suspension therapy system, has been widely used in the field of sports and rehabilitation. However, there have been few reports in the literature on the application of SET to the postoperative rehabilitation of anterior cruciate ligament reconstruction (ACLR) patients.
We hope to explore the effect of SET on neuromuscular function, postural control, and knee kinematics in ACLR patients.
To compare the clinical efficacy between SET protocol and traditional training protocol in ACLR patients.
Forty participants were randomized to an SET group or a control group. The SET group subjects participated in a SET protocol over 6 wk. The control group subjects participated in a traditional training protocol over 6 wk. Isokinetic muscle strength of the quadriceps and hamstrings, static and dynamic posture stability test, and relative translation of injured knee were assessed before and after training.
A total of 37 patients were included in the final analysis (SET group, n = 19; control group, n = 18). The relative peak torque of the quadriceps and hamstrings in both groups increased significantly (P < 0.001), and the SET group increased by a higher percentage than those in the control group (quadriceps: P = 0.004, hamstrings: P = 0.011). After training, both groups showed significant improvements in static and dynamic posture stability (P < 0.01), and the SET group had a greater change than the control group (P < 0.05). No significant improvement on the relative translation of injured knee was observed after training in both groups (P > 0.05).
SET can improve the postoperative rehabilitation effect of ACLR patients and is worthy of clinical promotion.
We only focused on the effect of SET on the injured knee. Thus, further studies should be performed to explore its biomechanical impact on the hip and ankle joints of ACLR patients and provide more evidence for the clinical application of SET.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Association of Rehabilitation Medicine.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Biondi A, Hashimoto N S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 271] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 2. | Musahl V, Becker R, Fu FH, Karlsson J. New trends in ACL research. Knee Surg Sports Traumatol Arthrosc. 2011;19 Suppl 1:S1-S3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Thomas AC, Wojtys EM, Brandon C, Palmieri-Smith RM. Muscle atrophy contributes to quadriceps weakness after anterior cruciate ligament reconstruction. J Sci Med Sport. 2016;19:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 136] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 4. | Perraton L, Clark R, Crossley K, Pua YH, Whitehead T, Morris H, Telianidis S, Bryant A. Impaired voluntary quadriceps force control following anterior cruciate ligament reconstruction: relationship with knee function. Knee Surg Sports Traumatol Arthrosc. 2017;25:1424-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 272] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 783] [Cited by in RCA: 925] [Article Influence: 61.7] [Reference Citation Analysis (0)] |
| 7. | Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 282] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 8. | Legnani C, Peretti GM, Del Re M, Borgo E, Ventura A. Return to sports and re-rupture rate following anterior cruciate ligament reconstruction in amateur sportsman: long-term outcomes. J Sports Med Phys Fitness. 2019;59:1902-1907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 257] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 10. | Przybylak K, Sibiński M, Domżalski M, Kwapisz A, Momaya AM, Zielińska M. Supervised physiotherapy leads to a better return to physical activity after anterior cruciate ligament reconstruction. J Sports Med Phys Fitness. 2019;59:1551-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Liu-Ambrose T, Taunton JE, MacIntyre D, McConkey P, Khan KM. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scand J Med Sci Sports. 2003;13:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Junker D, Stöggl T. The Training Effects of Foam Rolling on Core Strength Endurance, Balance, Muscle Performance and Range of Motion: A Randomized Controlled Trial. J Sports Sci Med. 2019;18:229-238. [PubMed] |
| 13. | Nagelli C, Wordeman S, Di Stasi S, Hoffman J, Marulli T, Hewett TE. Biomechanical Deficits at the Hip in Athletes With ACL Reconstruction Are Ameliorated With Neuromuscular Training. Am J Sports Med. 2018;46:2772-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22:987-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Kibele A, Behm DG. Seven weeks of instability and traditional resistance training effects on strength, balance and functional performance. J Strength Cond Res. 2009;23:2443-2450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Cooper RL, Taylor NF, Feller JA. A randomised controlled trial of proprioceptive and balance training after surgical reconstruction of the anterior cruciate ligament. Res Sports Med. 2005;13:217-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Fontana TL, Richardson CA, Stanton WR. The effect of weight-bearing exercise with low frequency, whole body vibration on lumbosacral proprioception: a pilot study on normal subjects. Aust J Physiother. 2005;51:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Liu G. Foundation and clinical application of suspension therapy. Guangzhou: Sun Yat-Sen University Press; 2014: 19-36. |
| 19. | Linek P, Saulicz E, Myśliwiec A, Wójtowicz M, Wolny T. The Effect of Specific Sling Exercises on the Functional Movement Screen Score in Adolescent Volleyball Players: A Preliminary Study. J Hum Kinet. 2016;54:83-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Kim JH, Kim YE, Bae SH, Kim KY. The effect of the neurac sling exercise on postural balance adjustment and muscular response patterns in chronic low back pain patients. J Phys Ther Sci. 2013;25:1015-1019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Chang WD, Huang WS, Lee CL, Lin HY, Lai PT. Effects of open and closed kinetic chains of sling exercise therapy on the muscle activity of the vastus medialis oblique and vastus lateralis. J Phys Ther Sci. 2014;26:1363-1366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Mau-Moeller A, Behrens M, Finze S, Bruhn S, Bader R, Mittelmeier W. The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: a randomized active-controlled clinical study. Health Qual Life Outcomes. 2014;12:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | World Medical Association Inc. . Declaration of Helsinki. Ethical principles for medical research involving human subjects. J Indian Med Assoc. 2009;107:403-405. [PubMed] |
| 24. | Tjernström F, Björklund M, Malmström EM. Romberg ratio in quiet stance posturography--Test to retest reliability. Gait Posture. 2015;42:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 25. | Paillard T, Noé F. Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. Biomed Res Int. 2015;2015:891390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 300] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 26. | Pinsault N, Vuillerme N. Test-retest reliability of centre of foot pressure measures to assess postural control during unperturbed stance. Med Eng Phys. 2009;31:276-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 27. | Taglietti M, Dela Bela LF, Dias JM, Pelegrinelli ARM, Nogueira JF, Batista Júnior JP, Carvalho RGDS, McVeigh JG, Facci LM, Moura FA, Cardoso JR. Postural Sway, Balance Confidence, and Fear of Falling in Women With Knee Osteoarthritis in Comparison to Matched Controls. PM R. 2017;9:774-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Shi H, Huang H, Ren S, Yu Y, Liang Z, Wang Q, Hu X, Ao Y. The relationship between quadriceps strength asymmetry and knee biomechanics asymmetry during walking in individuals with anterior cruciate ligament reconstruction. Gait Posture. 2019;73:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Machado F, Debieux P, Kaleka CC, Astur D, Peccin MS, Cohen M. Knee isokinetic performance following anterior cruciate ligament reconstruction: patellar tendon versus hamstrings graft. Phys Sportsmed. 2018;46:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Saeterbakken AH, van den Tillaar R, Seiler S. Effect of core stability training on throwing velocity in female handball players. J Strength Cond Res. 2011;25:712-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 31. | Tagesson S, Oberg B, Good L, Kvist J. A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med. 2008;36:298-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 32. | Li X, Liu H, Lin KY, Miao P, Zhang BF, Lu SW, Li L, Wang CH. Effects of Different Sling Settings on Electromyographic Activities of Selected Trunk Muscles: A Preliminary Research. Biomed Res Int. 2020;2020:2945952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Kim JJ. An analysis on muscle tone and stiffness during sling exercise on static prone position. J Phys Ther Sci. 2016;28:3440-3443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Palmer TB, Farrow AC, Palmer BM. Relationships between hamstring morphological characteristics and postural balance in elderly men. J Musculoskelet Neuronal Interact. 2020;20:88-93. [PubMed] |
| 35. | Vitale JA, La Torre A, Banfi G, Bonato M. Effects of an 8-Week Body-Weight Neuromuscular Training on Dynamic Balance and Vertical Jump Performances in Elite Junior Skiing Athletes: A Randomized Controlled Trial. J Strength Cond Res. 2018;32:911-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Kim GY, Kin SH. Effects of Push-ups Plus Sling Exercise on Muscle Activation and Cross-sectional Area of the Multifidus Muscle in Patients with Low Back Pain. J Phys Ther Sci. 2013;25:1575-1578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Yao ZL, Wang SB, Zhang Y, Huang WH, Shen HY, Ma LM, Huang HY, Xia H. Clinical Significance of a Novel Knee Joint Stability Assessment System for Evaluating Anterior Cruciate Ligament Deficient Knees. Orthop Surg. 2016;8:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Davis K, Williams JL, Sanford BA, Zucker-Levin A. Assessing lower extremity coordination and coordination variability in individuals with anterior cruciate ligament reconstruction during walking. Gait Posture. 2019;67:154-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 39. | Webster KE, Wittwer JE, O'Brien J, Feller JA. Gait patterns after anterior cruciate ligament reconstruction are related to graft type. Am J Sports Med. 2005;33:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (1)] |