Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2205
Peer-review started: September 22, 2020
First decision: December 13, 2020
Revised: January 15, 2021
Accepted: February 11, 2021
Article in press: February 11, 2021
Published online: April 6, 2021
Processing time: 182 Days and 5.2 Hours
Coronavirus disease 2019 (COVID-19) has spread rapidly to multiple countries through its infectious agent severe acute respiratory syndrome coronavirus 2. The severity, atypical clinical presentation, and lack of specific anti-viral treatments have posed a challenge for the diagnosis and treatment of COVID-19. Understanding the epidemiological and clinical characteristics of COVID-19 cases in different geographical areas is essential to improve the prognosis of COVID-19 patients and slow the spread of the disease.
To investigate the epidemiological and clinical characteristics and main therapeutic strategy for confirmed COVID-19 patients hospitalized in Liaoning Province, China.
Adult patients (n = 65) with confirmed COVID-19 were enrolled in this retrospective study from January 20 to February 29, 2020 in Liaoning Province, China. Pharyngeal swabs and sputum specimens were collected from the patients for the detection of severe acute respiratory syndrome coronavirus 2 nucleic acid. Patient demographic information and clinical data were collected from the medical records. Based on the severity of COVID-19, the patients were divided into nonsevere and severe groups. All patients were followed until March 20, 2020.
The mean age of 65 COVID-19 patients was 45.5 ± 14.4 years, 56.9% were men, and 24.6% were severe cases. During the 14 d before symptom onset, 25 (38.5%) patients lived or stayed in Wuhan, whereas 8 (12.3%) had no clear history of exposure. Twenty-nine (44.6%) patients had at least one comorbidity; hypertension and diabetes were the most common comorbidities. Compared with nonsevere patients, severe patients had significantly lower lymphocyte counts [median value 1.3 × 109/L (interquartile range 0.9-1.95) vs 0.82 × 109/L (0.44-1.08), P < 0.001], elevated levels of lactate dehydrogenase [450 U/L (386-476) vs 707 U/L (592-980), P < 0.001] and C-reactive protein [6.1 mg/L (1.5-7.2) vs 52 mg/L (12.7-100.8), P < 0.001], and a prolonged median duration of viral shedding [19.5 d (16-21) vs 23.5 d (19.6-30.3), P = 0.001]. The overall median viral shedding time was 19.5 d, and the longest was 53 d. Severe patients were more frequently treated with lopinavir/ritonavir, antibiotics, glucocorticoid therapy, immunoglobulin, thymosin, and oxygen support. All patients were discharged following treatment in quarantine.
Our findings may facilitate the identification of severe cases and inform clinical treatment and quarantine decisions regarding COVID-19.
Core Tip: This study describes the clinical and laboratory characteristics of 65 adult coronavirus disease 2019 (COVID-19) patients who were diagnosed and treated in Liaoning Province. The prevalence of afebrile patients was significantly higher in nonsevere COVID-19 patients than in severe patients, whereas severe COVID-19 patients were more likely to have lymphopenia and elevated levels of lactate dehydrogenase and C-reactive protein. The longer median duration of viral shedding in severe patients should be noted to improve transmission control measures.
- Citation: Zhang W, Ban Y, Wu YH, Liu JY, Li XH, Wu H, Li H, Chen R, Yu XX, Zheng R. Epidemiological and clinical characteristics of 65 hospitalized patients with COVID-19 in Liaoning, China. World J Clin Cases 2021; 9(10): 2205-2217
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2205.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2205
The ongoing spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; previously 2019-nCoV), the virus that causes coronavirus disease 2019 (COVID-19), continues worldwide[1] and poses a constant threat to global public health[2]. On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic, and more than 88 million infections and almost 1.9 million deaths from more than 200 countries, areas, or territories as of January 10, 2021[1]. The most-affected regions as of January 10, 2021 are the Americas and Europe, which are not only responsible for 77% of cumulative cases and 80% of cumulative deaths globally but also for the majority of new cases and deaths[1]. According to the Centers for Disease Control and Prevention, as of January 13, 2021, over 22 million COVID-19 cases have been confirmed in the United States, and 379255 patients have died due to the disease[3]. Many countries have imposed restrictions on the movement[4-6] of people to limit the spread of SARS-CoV-2 and reduce the burden on health systems, but these measures have brought a heavy economic cost and global economic decline[6].
In the early stage of the coronavirus outbreak in China, the government employed two strategies-containment and suppression-in an attempt to prevent and control COVID-19 spread. Thereafter, the number of new cases of COVID-19 in China declined, and internationally imported cases or second-generation cases from importations accounted for the majority of new COVID-19 cases[7]. In December 2020, there were 104 new confirmed cases of COVID-19 in China, representing an increase of 76.3% over November. During the New Year's Day and Spring Festival there was an increase in the number of overseas returnees; high mobility of domestic personnel; more gathering activities, especially indoor activities; and a rise in imported cold-chain food and cargo logistics. All of these factors are believed to have contributed to an increased transmission risk of SARS-CoV-2[8]. Therefore, the epidemic situation in China remains severe and complicated. As of January 13, 2021, SARS-CoV-2 has caused 4635 deaths out of 87844 confirmed cases in mainland China[9], of which 68149 (77.6%) cases occurred in Hubei Province[10], and 396 (0.045‰) occurred in Liaoning Province[11]. Several recent studies have indicated that COVID-19 case frequency and/or mortality vary according to population characteristics, socioeconomic status, climate, and social distancing interventions[12-15]. Previous studies in China have mainly documented the epidemiological and clinical characteristics of COVID-19 cases in Hubei Province[16-19]; however, descriptions of confirmed cases in Liaoning Province have remained limited to date[20].
This study aimed to analyze the epidemiological, clinical, and laboratory characteristics as well as the main therapeutic strategy for hospitalized COVID-19 patients in Liaoning Province, China.
This retrospective observational study included 65 COVID-19 patients (≥ 18 years old) on whom the principle investigator of this study participated in the clinical guidance, as a member of the Liaoning Province COVID-19 medical treatment expert team from January 20 to February 29, 2020 in Liaoning Province, China. Throat swabs and sputum samples from suspected SARS-CoV-2 infected patients were obtained to detect viral nucleic acid using real-time reverse transcription-polymerase chain reaction. The patients were divided into two groups: Nonsevere group and severe group based on the level of COVID-19 severity.
This case series was approved by the Medical Ethics Committee of Shengjing Hospital of China Medical University (reference number 2020PS065K).
Demographics and clinical data of patients, including age, sex, medical history, exposure history, comorbidities, signs and symptoms, laboratory findings, chest computed tomographic (CT) findings, and treatment measures, were retrospectively collected. Patients were discharged when deemed clinically recovered, including afebrile for at least 3 d, resolution of symptoms, radiologic improvement, and two negative results of consecutive nucleic acid tests taken at least 24 h apart. Clinical outcomes were followed until March 20, 2020.
The date of disease onset was defined as the day when the first symptoms were noticed. Fever was considered as an increase in body temperature above 37.2 °C. The level of COVID-19 severity was defined according to the New Coronavirus Pneumonia Diagnosis and Treatment Protocol (Trial Version 8) released by China’s National Health Commission[21]. Adult COVID-19 cases meeting at least one of the following criteria were considered to have severe COVID-19: (1) Shortness of breath with a respiratory rate > 30 breaths/min; (2) Oxygen saturation level using a pulse oximeter ≤ 93% at rest; (3) Oxygenation index (partial pressure of artery oxygen/fraction of inspired oxygen, PaO2/FiO2) ≤ 300 mmHg; or (4) Progressively worsening clinical symptoms with pulmonary imaging showing significant progression of lesions within 24-48 h > 50%.
Categorical variables are reported as frequencies and percentages, and continuous variables are described using the mean and standard deviation, or median and interquartile range (IQR) according to the normality of distribution. Missing values of the variables were filled with median or mean imputation. Differences between groups were compared using the Student’s t-test or the Mann-Whitney U test for quantitative variables according to their distribution, and the χ2 test or Fisher exact test when appropriate for categorical variables. Statistical significance was represented by a P value < 0.05. All statistical analyses were performed with Statistic Package for Social Science (IBM Statistic Package for Social Science Statistics 21.0).
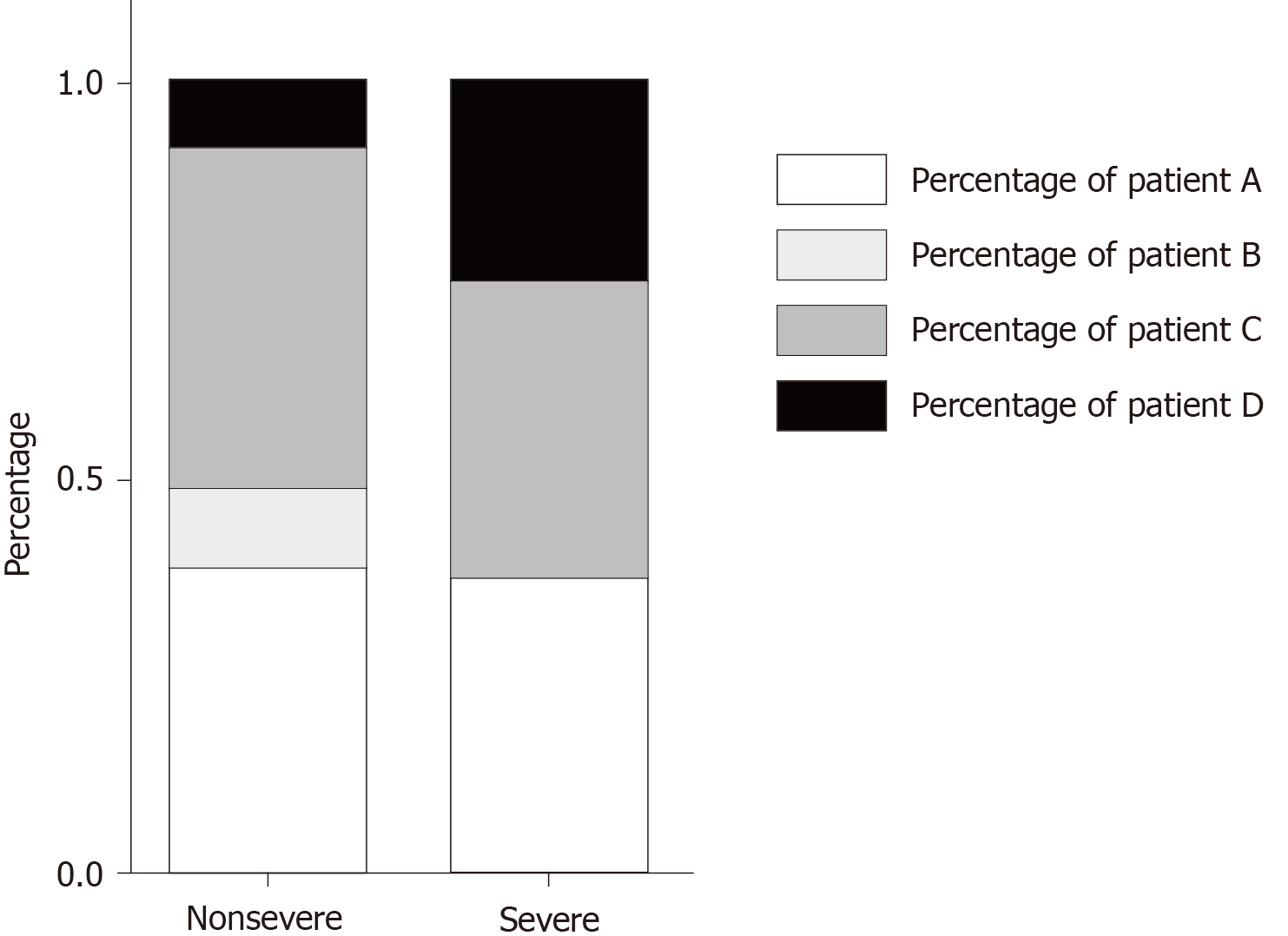
This study involved 65 SARS-CoV-2 infected patients with pneumonia, all of whom were confirmed and treated in Liaoning Province. Among them, 25 (38.5%) patients lived or stayed in Wuhan within 14 d after confirmation of COVID-19, 5 (7.7%) lived or stayed in Hubei Province except Wuhan, 27 (41.5%) who were residents of Liaoning Province had an exposure to confirmed cases, and 8 (12.3%) who were residents of Liaoning Province had no clear exposure history. There were no significant differences between the nonsevere and severe groups in the percentages of potential exposure to the source of infection within 14 d after confirmation of COVID-19 (Figure 1). The 65 patients were neither hospital workers nor did they have a direct exposure history to the Huanan Seafood Wholesale Market or wildlife animals in Wuhan.
Of the 65 patients, 49 (75.4%) and 16 (24.6%) were classified into the nonsevere and severe groups, respectively (Table 1). The mean age was 45.5 ± 14.4 years, and 37 (56.9%) were men. The mean time from illness onset to first hospital admission was 4.7 ± 3.5 d. Twenty-nine (44.6%) patients had at least one underlying comorbidity; hypertension (15.4%), diabetes (13.8%), cardiovascular disease (6.2%), and chronic liver disease (6.2%) were the most frequent comorbidities. The most commonly experienced symptoms were fever (70.8%) and dry cough (60%), followed by expectoration (29.2%), fatigue (24.6%), dyspnea (17.2%), and pharyngalgia (12.3%). Other less common symptoms included myalgia, runny or stuffy nose, headache, diarrhea, nausea or vomiting, chest pain, and hemoptysis. In addition, eight nonsevere patients showed no clinical symptoms since the onset of illness. As expected, the prevalence of dyspnea was higher in severe patients than in nonsevere patients (40% vs 10.2%, P = 0.022). Furthermore, compared with severe patients, afebrile was more frequent in nonsevere patients (38.8% vs 0%, P = 0.008).
| Characteristic | Total (n = 65) | Nonsevere (n = 49) | Severe (n = 16) | P value |
| Age, yr | 45.5 ± 14.4 | 43.6 ± 14.2 | 51.2 ± 14.1 | 0.067 |
| Male sex | 37 (56.9) | 26 (53.1) | 11 (68.8) | 0.271 |
| Current and former smokers | 7 (10.8) | 3 (6.1) | 4 (25) | 0.099 |
| Comorbidities | 29 (44.6) | 20 (40.8) | 9 (56.3) | 0.281 |
| Diabetes mellitus | 9 (13.8) | 8 (16.3) | 1 (6.3) | 0.551 |
| Hypertension | 10 (15.4) | 9 (18.4) | 1 (6.3) | 0.443 |
| Cardiovascular disease | 4 (6.2) | 3 (6.1) | 1 (6.3) | 1 |
| Cerebrovascular disease | 1 (1.5) | 1 (2) | 0 (0) | 1 |
| Chronic bronchitis | 2 (3.1) | 1 (2) | 1 (6.3) | 0.435 |
| Chronic liver disease | 4 (6.2) | 4 (8.2) | 0 (0) | 0.565 |
| Signs and symptoms | ||||
| Fever | 46 (70.8) | 30 (61.2) | 16 (100) | 0.008 |
| Highest temperature, °C | 37.9 ± 0.9 | 37.7 ± 0.9 | 38.5 ± 0.6 | < 0.001 |
| < 37.3 | 17 (26.2) | 17 (34.7) | 0 | NA |
| 37.3-38.5 | 30 (46.2) | 21 (42.9) | 9 (56.3) | NA |
| > 38.5 | 18 9 (7.7%) | 11 (22.4) | 7 (43.8) | NA |
| Dry cough | 39 (60) | 27 (55.1) | 12 (75) | 0.158 |
| Expectoration | 19 (29.2) | 14 (28.6) | 5 (31.3) | 1 |
| Dyspnea | 11 (17.2) | 5 (10.2) | 6 (40) | 0.022 |
| Fatigue | 16 (24.6) | 12 (24.5) | 4 (25) | 1 |
| Myalgia | 4 (6.2) | 2 (4.1) | 2 (12.5) | 0.252 |
| Pharyngalgia | 8 (12.3) | 6 (12.2) | 2 (12.5) | 1 |
| Stuffy and runny nose | 3 (4.6) | 1 (2) | 2 (12.5) | 0.147 |
| Hemoptysis | 2 (3.1) | 1 (2) | 1 (6.3) | 0.435 |
| Chest pain | 2 (3.1) | 1 (2) | 1 (6.3) | 0.435 |
| Headache | 3 (4.6) | 2 (4.1) | 1 (6.3) | 1 |
| Nausea | 3 (4.6) | 2 (4.1) | 1 (6.3) | 1 |
| Vomiting | 2 (3.1) | 2 (4.1) | 0 (0) | 1 |
| Diarrhea | 3 (4.6) | 2 (4.1) | 1 (6.3) | 1 |
| Days from illness onset to first hospital admission | 4.7 ± 3.5 | 4.4 ± 3.4 | 5.6 ± 3.9 | 0.218 |
| Heart rate, bpm1 | 82.6 ± 9 | 82.8 ± 9 | 82.1 ± 9.2 | 0.81 |
| Respiratory rate, bpm2 | 19 (18-20) | 18 (18-20) | 20 (18.3-20) | 0.084 |
| Mean arterial pressure, mm Hg | 98.2 ± 12 | 98 ± 12.9 | 98.8 ± 9.1 | 0.819 |
Based on chest CT scans, 53 (81.5%) patients showed bilateral lung involvement, and a small amount of pleural effusion was found in 3 (4.6%) patients (Table 2). No lung cavitation was observed. Additionally, pure ground-glass opacity (GGO) occurred in 24 (36.9%) patients, and GGO and consolidation were observed in 41 (63.1%) patients. The chest CT images of nonsevere patients were more likely to show pure GGO compared to severe patients (46.9% vs 6.3%, P = 0.003). In contrast, GGO and consolidation were more frequently observed in severe patients than in nonsevere patients (53.1% vs 93.8%, P = 0.003). A peripheral distribution of pulmonary infiltrates was demonstrated in all patients; however, there were no statistical differences between the two groups in the proportion of peripheral and central pulmonary lesions.
| Normal range | Total (n = 65) | Nonsevere (n = 49) | Severe (n = 16) | P value | |
| Chest CT findings, n (%) | |||||
| Bilateral distribution | NA | 53 (81.5) | 37 (75.5) | 16 (100) | 0.069 |
| Pure ground-glass opacity | NA | 24 (36.9) | 23 (46.9) | 1 (6.3) | 0.003 |
| Ground-glass opacity and Consolidation | NA | 41 (63.1) | 26 (53.1) | 15 (93.8) | 0.003 |
| Peripheral distribution | NA | 65 (100) | 49 (100) | 16 (100) | NA |
| Peripheral and central distribution | NA | 26 (40) | 17 (34.7) | 9 (56.3) | 0.126 |
| Laboratory findings | |||||
| White blood cell count, × 109/L | 3.5-9.5 | 5 (3.47-6.75) | 5 (3.47-6.8) | 5.01 (3.59-5.51) | 0.976 |
| Neutrophil count, × 109/L | 1.8-6.3 | 3.71 ± 2.58 | 3.26 ± 1.59 | 5.1 ± 4.2 | 0.104 |
| Lymphocyte count, × 109/L | 1.1-3.2 | 1.15 (0.83-1.78) | 1.3 (0.9-1.95) | 0.82 (0.44-1.08) | < 0.001 |
| < 1.0, n (%) | NA | 26 (40) | 15 (30.6) | 11 (68.8) | 0.007 |
| Monocyte count, × 109/L | 0.1-0.6 | 0.41 (0.3-0.41) | 0.4 (0.35-0.47) | 0.4 (0.3-0.4) | 0.253 |
| Platelet count, × 109/L | 125-350 | 200 ± 72 | 204 ± 79 | 188 ± 47 | 0.445 |
| Prothrombin time, s | 11-14 | 11.58 (10.5-12) | 11.5 (10.5-11.6) | 11.5 (10.4-12.2) | 0.788 |
| D-dimer, mg/L | 0-0.55 | 0.27 (0.18-0.44) | 0.27 (0.16-0.27) | 0.51 (0.27-0.81) | < 0.001 |
| Albumin, g/L | 35-50 | 35.6 ± 5.5 | 36.2 ± 5.2 | 33.6 ± 6.1 | 0.099 |
| Alanine aminotransferase, U/L | 0-40 | 29 (19.5-48.5) | 29 (17-40) | 41.5 (21.8-69.3) | 0.068 |
| Aspartate aminotransferase, U/L | 0-40 | 25 (20-31) | 25 (17-29) | 27.5 (22.3-43.5) | 0.105 |
| Total bilirubin, mmol/L | 3-22 | 18.5 ± 6.6 | 17.7 ± 6.1 | 21.1 ± 7.7 | 0.08 |
| Creatinine, μmol/L | 58-110 | 56.8 ± 13.8 | 56.6 ± 14.4 | 57.4 ± 12.2 | 0.843 |
| Blood urea nitrogen, mmol/L | 2.5-6.1 | 3.7 ± 1.1 | 3.6 ± 0.9 | 4.2 ± 1.3 | 0.046 |
| Creatine kinase, U/L | 55-170 | 50 (35-79) | 50 (32.5-62.5) | 74 (48.3-130) | 0.03 |
| Creatine kinase-MB, U/L | 0-16 | 2 (1-6.5) | 2 (1-4) | 5.5 (2-12.1) | 0.015 |
| Lactate dehydrogenase, U/L | 313-618 | 461 (407-614) | 450 (386-479) | 707 (592-980) | < 0.001 |
| > 618, n (%) | NA | 16 (24.6) | 4 (8.2) | 12 (75) | < 0.001 |
| Potassium, mmol/L | 3.5-5.1 | 4.1 ± 0.5 | 4.3 ± 0.5 | 3.8 ± 0.5 | 0.001 |
| Sodium, mmol/L | 137-145 | 134 ± 3.5 | 135 ± 3.1 | 132 ± 3.8 | 0.002 |
| C-reactive protein, mg/L | 0-8 | 6.2 (2.9-28.7) | 6.1 (1.5-7.2) | 52 (12.7-100.8) | < 0.001 |
| > 8, n (%) | NA | 21 (32.3) | 9 (18.4) | 12 (75) | < 0.001 |
| Procalcitonin, ng/mL | 0-0.25 | 0.04 (0.04-0.05) | 0.04 (0.04-0.05) | 0.043 (0.04-0.08) | 0.084 |
| Duration of viral shedding after COVID-19 onset | NA | 19.5 (17-24) | 19.5 (16-21) | 23.5 (19.6-30.3) | 0.001 |
Overall, blood cell counts in the majority of patients were within normal limits, excluding the lymphocyte count that was notably lower in severe cases than in nonsevere cases [1.3 × 109/L (IQR: 0.9-1.95) vs 0.82 × 109/L (IQR: 0.44-1.08), P < 0.001]. Moreover, severe patients showed higher levels of D-dimer, blood urea nitrogen, creatine kinase, and creatine kinase-MB, despite the median values of these laboratory tests for the two groups being within their corresponding normal range. Markedly elevated levels of C-reactive protein (CRP) [6.1 mg/L (IQR: 1.5-7.2) vs 52 (IQR: 12.7-100.8), P < 0.001] and lactate dehydrogenase (LDH) [450 U/L (IQR: 386-476) vs 707 (IQR: 592-980), P < 0.001] were observed in severe patients than in nonsevere patients.
The duration of viral shedding from illness onset ranged from 4 to 53 d, and the median duration of viral shedding was 19.5 d (IQR: 17-24). Notably, severe patients showed a longer median duration of viral shedding from illness onset than nonsevere patients [19.5 d (IQR: 16-21) vs 23.5 (IQR: 19.6-30.3), P = 0.001]. The severity of illness scores for hospitalized patients with COVID-19 is shown in Table 3.
| Total (n = 65) | Nonsevere (n = 49) | Severe (n = 16) | P value | |
| APACHE II | 4.8 ± 3.6 | 3.9 ± 2.9 | 7.4 ± 4.4 | 0.009 |
| SOFA | 1 (0-2) | 0 (0-1) | 3 (2-4) | < 0.001 |
| PSI | 49.5 ± 21.7 | 43.2 ± 18.5 | 68.7 ± 19.7 | < 0.001 |
| MuLBSTA | 5 (5-8) | 5 (4.5-7) | 9 (5-11) | < 0.001 |
As of March 20, 2020, all patients had been discharged after undergoing treatment in isolation. Except for four nonsevere cases, the remaining 61 (93.8%) patients were administered antiviral treatment (Table 4). Overall, 36 (55.4%) patients were given empirical antibiotic treatment, including moxifloxacin (46.1%), levofloxacin (4.6%), cefoperazone sodium and sulbactam sodium (4.6%), carbopenems (9.2%), linezolid (4.6%), and caspofungin (1.5%). Expectedly, severe patients were more likely to receive lopinavir/ritonavir (LPV/r), antibiotics, glucocorticoid therapy, immunoglobulin, thymosin, and oxygen support than nonsevere patients. The prone position was intermittently used to improve oxygenation in six patients with severe hypoxemia, four of whom received oxygen via high-flow nasal cannula and the other two received oxygen via regular nasal cannulas. Consequently, oxygenation was significantly improved in five patients after being placed in the prone position. Only one of the six patients, whose hypoxemia did not improve rapidly, received subsequent noninvasive ventilation, invasive mechanical ventilation, extracorporeal membrane oxygenation, and pulmonary rehabilitation. Finally, this 41-year-old male patient recovered following antiviral, glucocorticoid, and antibiotic therapies.
| Total (n = 65) | Nonsevere (n = 49) | Severe (n = 16) | P value | |
| Antiviral therapy | ||||
| Oseltamivir | 12 (18.5) | 8 (16.3) | 4 (25) | 0.685 |
| Arbidol | 40 (61.5) | 32 (65.3) | 8 (50) | 0.275 |
| Ribavirin | 3 (4.6) | 3 (6.1) | 0 | 0.569 |
| Lopinavir/Ritonavir | 35 (53.8) | 22 (44.9) | 13 (81.3) | 0.011 |
| Interferon | 21 (32.3) | 16 (32.7) | 5 (31.3) | 0.917 |
| Chloroquine | 1 (1.5) | 0 | 1 (6.3) | 0.246 |
| Antibiotic therapy | 36 (55.4) | 21 (42.9) | 15 (93.8) | < 0.001 |
| Antifungal therapy | 1 (1.5) | 0 | 1 (6.3) | 0.246 |
| Glucocorticoid therapy | 12 (18.5) | 2 (4.1) | 10 (62.5) | < 0.001 |
| Immunoglobulin | 3 (4.6) | 0 | 3 (18.8) | 0.013 |
| Thymosin | 11 (16.9) | 4 (8.2) | 7 (43.8) | 0.004 |
| Traditional Chinese medicine | 51 (78.5) | 38 (77.6) | 13 (81.3) | 1 |
| Oxygen support | 20 (30.8) | 4 (8.2) | 16 (100) | < 0.001 |
| Nasal cannulas | 20 (30.8) | 4 (8.2) | 16 (100) | < 0.001 |
| HFNC | 6 (9.2) | 0 | 6 (37.5) | < 0.001 |
| NIV | 1 (1.5) | 0 | 1 (6.3) | 0.246 |
| IMV | 1 (1.5) | 0 | 1 (6.3) | 0.246 |
| ECMO | 1 (1.5) | 0 | 1 (6.3) | 0.246 |
| Prone position | 6 (9.2) | 0 | 6 (37.5) | < 0.001 |
Owing to the high infectivity and high pathogenicity of SARS-CoV-2, the rising number of COVID-19 cases has caused global public health concerns. Here, we report the results of a comparative analysis of 49 nonsevere and 16 severe cases with pneumonia diagnosed and treated as COVID-19 in Liaoning Province. Nearly 12.3% of the patients did neither live in nor visit Hubei Province; they also had no exposure history of direct contact with confirmed COVID-19 cases. Thus, we speculate that in these COVID-19 cases, transmission was likely linked to asymptomatic COVID-19 patients[22,23] mainly through inhalation of respiratory droplets or contact with contaminated surfaces[24]. In contrast to our data, Guan et al[25] reported in their study of patients from 552 hospitals in China, the percentage reporting no direct contact with confirmed COVID-19 cases reached a higher rate, at nearly 25.9%. In another study of 94 COVID-19 patients in China, the proportion of presymptomatic transmission was reported to be approximately 44%[26]. These findings suggested that as potential sources of SARS-CoV-2 infection, the identification and management of asymptomatic cases or presymptomatic COVID-19 patients should be strengthened.
The median age of COVID-19 patients was previously reported to range from 49 to 57 years in Wuhan[16-19,27]. The mean age of patients in our study was slightly lower (45.5 years), but similar to recent data from Beijing (median age 47.5 years)[28] and another selected cohort of patients throughout China (median age 47 years)[25]. Despite people of any age being susceptible to SARS-CoV-2[29], older age has been associated with higher mortality[18,30] and more frequent severe COVID-19 cases than younger age[16,17], as observed in the present study.
In agreement with recent findings[17,18], our data showed hypertension and diabetes as the most frequent underlying diseases in infected people. Nevertheless, our study failed to find a significantly larger proportion of underlying diseases in severe patients than in nonsevere patients, as reported in recent studies[16,17]. The main reason for this discrepancy may be the younger mean age and/or a smaller sample size in our study. The most common clinical symptoms of COVID-19 in the present study included fever, cough, fatigue, dyspnea, and pharyngalgia, consistent with other recent reports[16]. Interestingly, our results showed that 17 (34.7%) patients with nonsevere COVID-19 had no febrile response and the occurrence of fever and dyspnea was remarkably higher than that in severe patients (0%). This suggests that COVID-19 patients with stable vital signs, who lack fever or dyspnea, may be relatively mild cases, excluding those with impaired immune function.
Regarding radiological findings, in this study bilateral involvement (81.5%), peripheral distribution (100%), and GGO (100%) were the most common chest CT manifestations of COVID-19, and pleural effusions (4.6%) were rare. Notably, our results showed that critically ill patients had a higher incidence of GGO with consolidation (93.8%) than nonsevere patients (53.1%). Similarly, in other studies, it has been observed that as the illness progressed, GGO in chest CT images of COVID-19 patients increased, enlarged, and consolidated[31]. These findings may help clinicians recognize the time-course and severity of COVID-19.
As expected, compared to nonsevere COVID-19 patients, we observed notable increased levels of D-dimer, creatine kinase-MB, LDH, and blood urea nitrogen in severe patients, suggesting that coagulation derangements, myocardial injury, and decreased renal function were more common in severe COVID-19 cases[32]. Recent studies showed the association of lymphopenia with the severity and poor prognosis of COVID-19[18,33]. It has been demonstrated that SARS-CoV-2 infection leads to the functional exhaustion of cytotoxic lymphocytes and the breakdown of antiviral immunity in the early stage of infection[34]. We did not find significantly elevated serum procalcitonin levels in our patients, which may indicate that increased concentrations of other inflammatory markers, such as CRP and LDH, are due to a SARS-CoV-2 infection rather than a bacterial infection. CRP has been extensively used as a marker of inflammation in clinical practice. In the host innate immune response, CRP is involved in recognition of viral infection[35], activation of complement, and promoting the inflammatory response in severe influenza infection[36]. Previous studies found that high levels of CRP and LDH in COVID-19 patients were correlated with more severe COVID-19 illness[18,37]. In the present study, 43.1% of COVID-19 patients had lymphopenia, and severe patients with COVID-19 had significantly lower absolute lymphocyte counts and abnormally higher levels of CRP and LDH than nonsevere patients. These results are similar to previously reported data[16,17,38]. This suggests that the maladjusted immune response and excessive activation of the inflammatory response are more likely to occur in critically ill patients with COVID-19, and thus contribute to pulmonary tissue damage, functional impairment, and deterioration of severe COVID-19 patients.
Previous reports of COVID-19 cases found that the viral load from the respiratory tract declined after the first week of symptom onset[39,40]. The results of the present study show that the median viral shedding time for COVID-19 from throat swabs or sputum samples was 19.5 d, which was close to the finding of 20.0 d reported by Zhou et al[18], but longer than 12.0 d reported by Qian et al[41]. We found that the longest viral shedding time for COVID-19 persisted for 53 d, in contrast to 37 d and 34 d in other reports[18,41]. The 53-d viral shedding time was found in the nonsevere COVID-19 case of a 66-year-old man with a history of diabetes, hypertension, and intracerebral hemorrhage; he was treated with arbidol. However, the reason for the prolonged shedding time in this case remains unclear, and host factors may have contributed. Zhou et al[18] recently reported that SARS-CoV-2 ribonucleic acid from respiratory tract samples was present until death in non-survivors. Similarly, ours results showed that the median duration of viral shedding in the severe COVID-19 group was 4 d longer than that of the nonsevere group. Understanding the duration and pattern of viral shedding in individuals infected with SARS-CoV-2 could help reduce exposure to and transmission of SARS-CoV-2 and improve infection control.
To date, no antiviral drug has been fully proven effective for COVID-19, and some potential vaccine candidates against COVID-19 have already reached phase 3 clinical trials[42]. Encouragingly, several COVID-19 vaccines, including Pfizer-BioNTech COVID-19 vaccine and Sinopharm vaccine, have been approved for conditional or emergency use in some countries, and these are expected to prevent SARS-CoV-2 infection and reduce the severity of the illness.
A recent in vitro study demonstrated that remdesivir and chloroquine were highly effective against SARS-CoV-2 infection[43]. Grein et al[44] observed clinical improvement in 68% of 53 COVID-19 patients treated with compassionate-use remdesivir. In addition, remdesivir was demonstrated to significantly shorten the time to recovery compared to a placebo[45,46]. Despite the proven efficacy, in a trial with 1062 hospitalized patients with COVID-19[45], grade 3 or 4 adverse events with remdesivir therapy were reported in 51.3% of patients in the remdesivir group, while serious adverse events observed in 24.6% of patients. The WHO suggests against remdesivir except treating patients hospitalised with COVID-19 regardless of disease severity[47]. A retrospective cohort study reported that arbidol combined with LPV/r delayed the progression of lung injury and reduced viral load in COVID-19 patients[48], whereas a recent randomized controlled clinical trial in severe COVID-19 cases did not show any obvious benefit of LPV/r in clinical improvement, mortality, or throat viral ribonucleic acid detectability[49]. In the present study, according to Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment[21], antiviral drugs were empirically used in most patients, especially LPV/r in severe patients. As mentioned above, the patients in the present study did not show significantly high procalcitonin levels; thus, antibiotics were considered as compassionate use in 55.4% of the patients, including the application of linezolid and caspofungin in severe patients.
The evidence for corticosteroid therapy for COVID-19 is controversial and inconclusive, and systemic corticosteroids are recommended for the treatment of severe and critical COVID-19 patients according to the WHO living guidance[47]. Thus, corticosteroids were prescribed depending on disease severity and clinical experience in this study. Of 16 severe COVID-19 patients in the present study, 81.3% received LPV/r, 62.5% received corticosteroids, 50% received arbidol, and 43.8% received thymosin. These drugs may have been helpful in clinical improvement of these COVID-19 patients. In our study, in addition to medication, a 41-year-old male patient with severe COVID-19 received mechanical ventilation and extracorporeal membrane oxygenation in the early phase of acute respiratory distress syndrome, and he subsequently underwent an early pulmonary rehabilitation program after weaning, including prone position, respiratory training, physical exercises, psychological intervention, and sleep promotion. Early identification and mechanical ventilation of hypoxemia, prone position ventilation, and early pulmonary rehabilitation may contribute to improved oxygenation and survival among COVID-19 patients with acute respiratory distress syndrome[20,50].
Our study has several limitations. First, this observational study was subject to the limitations of a retrospective cohort design. Second, this study was limited by a relatively small sample size. Third, the estimated duration of viral shedding was limited by the frequency of respiratory specimen collection. Furthermore, the present study lacks information on COVID-19 patients who did not recover and survive.
In summary, our study findings and therapeutic regimens may provide useful information for the identification and treatment of severe cases, and inform quarantine practices for COVID-19 patients.
Coronavirus disease 2019 (COVID-19) has spread rapidly to multiple countries, and the illness severity, the atypical clinical presentation, and lack of specific anti-viral treatment have posed a challenge for the diagnosis and treatment of COVID-19.
Understanding the epidemiological and clinical characteristics of COVID-19 cases in different geographical areas are essential to improve the prognosis of COVID-19 patients.
This study aimed to investigate the epidemiological and clinical characteristics and main therapeutic strategy for confirmed COVID-19 patients hospitalized in Liaoning Province, China.
A total of 65 adult patients with confirmed COVID-19 were enrolled in this retrospective study from January 20 to February 29, 2020 in Liaoning Province, China. Based on the severity of COVID-19, the patients were divided into nonsevere and severe groups.
Compared with nonsevere patients (75.4%), severe patients (24.6%) had significantly lower lymphocyte counts, elevated levels of lactate dehydrogenase and C-reactive protein, and a longer median duration of viral shedding. The overall median viral shedding time was 19.5 d, and the longest was 53 d. Severe patients were more frequently treated with lopinavir/ritonavir, antibiotics, glucocorticoid therapy, immunoglobulin, thymosin, and oxygen support.
Our findings may facilitate the identification of severe cases and inform clinical treatment and quarantine decisions regarding COVID-19 patients.
The identification of severe cases with COVID-19 may help prevent poor outcomes, while the estimated duration of viral shedding may help inform quarantine decisions and prevent acute respiratory syndrome coronavirus 2 spread.
The authors thank Dr. Li-Qiang Zheng for his helpful advice on statistical analysis.
Manuscript source: Unsolicited manuscript
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ampollini L, Jurman G, Saha S S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Wang LL
| 1. | World Health Organization. COVID-19 Weekly Epidemiological Update. [cited 12 January 2021]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update---12-january-2021. |
| 2. | Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the Uncharted. N Engl J Med. 2020;382:1268-1269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1124] [Cited by in RCA: 1046] [Article Influence: 209.2] [Reference Citation Analysis (0)] |
| 3. | Centers for Disease Control and Prevention. CDC COVID Data Tracker. [cited 14 January 2021]. Available from: https://covid.cdc.gov/covid-data-tracker/?eType=EmailBlastContent&eId=898fa3f2-6696-41d2-aa8d-d16239fbf0cc#cases_casesper100klast7days. |
| 4. | Salje H, Tran Kiem C, Lefrancq N, Courtejoie N, Bosetti P, Paireau J, Andronico A, Hozé N, Richet J, Dubost CL, Le Strat Y, Lessler J, Levy-Bruhl D, Fontanet A, Opatowski L, Boelle PY, Cauchemez S. Estimating the burden of SARS-CoV-2 in France. Science. 2020;369:208-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 762] [Cited by in RCA: 681] [Article Influence: 136.2] [Reference Citation Analysis (0)] |
| 5. | Kraemer MUG, Yang CH, Gutierrez B, Wu CH, Klein B, Pigott DM; Open COVID-19 Data Working Group; du Plessis L; Faria NR; Li R; Hanage WP; Brownstein JS; Layan M; Vespignani A; Tian H; Dye C; Pybus OG; Scarpino SV. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2015] [Cited by in RCA: 1474] [Article Influence: 294.8] [Reference Citation Analysis (0)] |
| 6. | Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, Asgari N, Oh J, García-Basteiro AL, Hanefeld J, Cook AR, Hsu LY, Teo YY, Heymann D, Clark H, McKee M, Legido-Quigley H. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525-1534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 457] [Cited by in RCA: 455] [Article Influence: 91.0] [Reference Citation Analysis (0)] |
| 7. | Li Z, Chen Q, Feng L, Rodewald L, Xia Y, Yu H, Zhang R, An Z, Yin W, Chen W, Qin Y, Peng Z, Zhang T, Ni D, Cui J, Wang Q, Yang X, Zhang M, Ren X, Wu D, Sun X, Li Y, Zhou L, Qi X, Song T, Gao GF, Feng Z; China CDC COVID-19 Emergency Response Strategy Team. Active case finding with case management: the key to tackling the COVID-19 pandemic. Lancet. 2020;396:63-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 221] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 8. | National health commission of the People’s Republic of China. Transcript of the press conference of the Joint Prevention and Control Mechanism of the State Council on December 30, 2020. [cited 30 December 2020]. Available from: http://www.nhc.gov.cn/xcs/fkdt/202012/4b72af6ad0ca4973a3880f322dd6b4c2.shtml. |
| 9. | National health commission of the People’s Republic of China. Updates on the epidemic situation of COVID-19 in China on January 13, 2021. [cited 14 January 2021]. Available from: http://www.nhc.gov.cn/xcs/yqtb/202101/1cd117e46f2640a29d00d5e9323ca2e5.shtml. |
| 10. | Health commission of Hubei province. Updates on the epidemic situation of COVID-19 in Hubei province at 24:00 on January 13, 2021. [cited 14 January 2021]. Available from: http://wjw.hubei.gov.cn/bmdt/dtyw/202101/t20210114_3241501.shtml. |
| 11. | Health commission of Liaoning province. Updates on the epidemic situation of COVID-19 in Liaoning province at 24:00 on January 13, 2021. [cited 14 January 2021]. Available from: http://wsjk.ln.gov.cn/wst_wsjskx/202012/t20201230_4062371.html. |
| 12. | Sobral MFF, Duarte GB, da Penha Sobral AIG, Marinho MLM, de Souza Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci Total Environ. 2020;729:138997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 174] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 13. | Matrajt L, Leung T. Evaluating the Effectiveness of Social Distancing Interventions to Delay or Flatten the Epidemic Curve of Coronavirus Disease. Emerg Infect Dis. 2020;26:1740-1748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 215] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 14. | Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs. JAMA. 2020;323:2192-2195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 508] [Article Influence: 101.6] [Reference Citation Analysis (0)] |
| 15. | Loomba RS, Aggarwal G, Aggarwal S, Flores S, Villarreal EG, Farias JS, Lavie CJ. Disparities in case frequency and mortality of coronavirus disease 2019 (COVID-19) among various states in the United States. Ann Med. 2021;53:151-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14751] [Article Influence: 2950.2] [Reference Citation Analysis (0)] |
| 17. | Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2139] [Cited by in RCA: 2340] [Article Influence: 468.0] [Reference Citation Analysis (0)] |
| 18. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18175] [Article Influence: 3635.0] [Reference Citation Analysis (0)] |
| 19. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30057] [Article Influence: 6011.4] [Reference Citation Analysis (3)] |
| 20. | Zhu C, Wu Y, Liu H, Ban Y, Ma X, Zhang Z. Early pulmonary rehabilitation for SARS-CoV-2 pneumonia: Experience from an intensive care unit outside of the Hubei province in China. Heart Lung. 2020;49:449-450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | National Health Commission of the People’s Republic of China. New Coronavirus Pneumonia Diagnosis and Treatment Protocol (Trial Version 8). [cited 19 December 2020]. Available from: http://www.gov.cn/zhengce/zhengceku/2020-08/19/content_5535757.htm. |
| 22. | Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, Seilmaier M, Drosten C, Vollmar P, Zwirglmaier K, Zange S, Wölfel R, Hoelscher M. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020;382:970-971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2799] [Cited by in RCA: 2489] [Article Influence: 497.8] [Reference Citation Analysis (0)] |
| 23. | Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020;368:489-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2338] [Cited by in RCA: 2091] [Article Influence: 418.2] [Reference Citation Analysis (0)] |
| 24. | Lancet COVID-19 Commissioners, Task Force Chairs, and Commission Secretariat. Lancet COVID-19 Commission Statement on the occasion of the 75th session of the UN General Assembly. Lancet. 2020;396:1102-1124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 25. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18844] [Article Influence: 3768.8] [Reference Citation Analysis (7)] |
| 26. | He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, Lau YC, Wong JY, Guan Y, Tan X, Mo X, Chen Y, Liao B, Chen W, Hu F, Zhang Q, Zhong M, Wu Y, Zhao L, Zhang F, Cowling BJ, Li F, Leung GM. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2588] [Cited by in RCA: 2854] [Article Influence: 570.8] [Reference Citation Analysis (0)] |
| 27. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12962] [Article Influence: 2592.4] [Reference Citation Analysis (1)] |
| 28. | Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, Chen H, Wang D, Liu N, Liu D, Chen G, Zhang Y, Li D, Li J, Lian H, Niu S, Zhang L, Zhang J. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80:401-406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 711] [Cited by in RCA: 685] [Article Influence: 137.0] [Reference Citation Analysis (0)] |
| 29. | Singhal T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J Pediatr. 2020;87:281-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2006] [Cited by in RCA: 1567] [Article Influence: 313.4] [Reference Citation Analysis (0)] |
| 30. | O'Driscoll M, Ribeiro Dos Santos G, Wang L, Cummings DAT, Azman AS, Paireau J, Fontanet A, Cauchemez S, Salje H. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 749] [Article Influence: 149.8] [Reference Citation Analysis (0)] |
| 31. | Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, Hu Q, Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30:3306-3309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 564] [Cited by in RCA: 632] [Article Influence: 126.4] [Reference Citation Analysis (0)] |
| 32. | Tjendra Y, Al Mana AF, Espejo AP, Akgun Y, Millan NC, Gomez-Fernandez C, Cray C. Predicting Disease Severity and Outcome in COVID-19 Patients: A Review of Multiple Biomarkers. Arch Pathol Lab Med. 2020;144:1465-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 33. | Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang YQ, Wang Q, Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 759] [Cited by in RCA: 1045] [Article Influence: 209.0] [Reference Citation Analysis (0)] |
| 34. | Zheng M, Gao Y, Wang G, Song G, Liu S, Sun D, Xu Y, Tian Z. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020;17:533-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1043] [Cited by in RCA: 1283] [Article Influence: 256.6] [Reference Citation Analysis (0)] |
| 35. | Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, Pan P, Wang W, Hu D, Liu X, Zhang Q, Wu J. Coronavirus infections and immune responses. J Med Virol. 2020;92:424-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1056] [Cited by in RCA: 1167] [Article Influence: 233.4] [Reference Citation Analysis (0)] |
| 36. | Gao R, Wang L, Bai T, Zhang Y, Bo H, Shu Y. C-Reactive Protein Mediating Immunopathological Lesions: A Potential Treatment Option for Severe Influenza A Diseases. EBioMedicine. 2017;22:133-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, Wang Z, Li J, Li J, Feng C, Zhang Z, Wang L, Peng L, Chen L, Qin Y, Zhao D, Tan S, Yin L, Xu J, Zhou C, Jiang C, Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1522] [Cited by in RCA: 1363] [Article Influence: 272.6] [Reference Citation Analysis (0)] |
| 38. | Leisman DE, Ronner L, Pinotti R, Taylor MD, Sinha P, Calfee CS, Hirayama AV, Mastroiani F, Turtle CJ, Harhay MO, Legrand M, Deutschman CS. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med. 2020;8:1233-1244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 660] [Cited by in RCA: 633] [Article Influence: 126.6] [Reference Citation Analysis (0)] |
| 39. | Kim ES, Chin BS, Kang CK, Kim NJ, Kang YM, Choi JP, Oh DH, Kim JH, Koh B, Kim SE, Yun NR, Lee JH, Kim JY, Kim Y, Bang JH, Song KH, Kim HB, Chung KH, Oh MD; Korea National Committee for Clinical Management of COVID-19. Clinical Course and Outcomes of Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Infection: a Preliminary Report of the First 28 Patients from the Korean Cohort Study on COVID-19. J Korean Med Sci. 2020;35:e142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 230] [Cited by in RCA: 268] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 40. | Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M, Bleicker T, Brünink S, Schneider J, Ehmann R, Zwirglmaier K, Drosten C, Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4682] [Cited by in RCA: 4801] [Article Influence: 960.2] [Reference Citation Analysis (0)] |
| 41. | Qian GQ, Chen XQ, Lv DF, Ma AHY, Wang LP, Yang NB, Chen XM. Duration of SARS-CoV-2 viral shedding during COVID-19 infection. Infect Dis (Lond). 2020;52:511-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 42. | Singh JA, Upshur REG. The granting of emergency use designation to COVID-19 candidate vaccines: implications for COVID-19 vaccine trials. Lancet Infect Dis. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 43. | Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4289] [Cited by in RCA: 4558] [Article Influence: 911.6] [Reference Citation Analysis (0)] |
| 44. | Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, Feldt T, Green G, Green ML, Lescure FX, Nicastri E, Oda R, Yo K, Quiros-Roldan E, Studemeister A, Redinski J, Ahmed S, Bernett J, Chelliah D, Chen D, Chihara S, Cohen SH, Cunningham J, D'Arminio Monforte A, Ismail S, Kato H, Lapadula G, L'Her E, Maeno T, Majumder S, Massari M, Mora-Rillo M, Mutoh Y, Nguyen D, Verweij E, Zoufaly A, Osinusi AO, DeZure A, Zhao Y, Zhong L, Chokkalingam A, Elboudwarej E, Telep L, Timbs L, Henne I, Sellers S, Cao H, Tan SK, Winterbourne L, Desai P, Mera R, Gaggar A, Myers RP, Brainard DM, Childs R, Flanigan T. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N Engl J Med. 2020;382:2327-2336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1926] [Cited by in RCA: 1884] [Article Influence: 376.8] [Reference Citation Analysis (0)] |
| 45. | Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fätkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG, Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC; ACTT-1 Study Group Members. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 2020;383:1813-1826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5711] [Cited by in RCA: 5099] [Article Influence: 1019.8] [Reference Citation Analysis (0)] |
| 46. | Beigel JH, Tomashek KM, Dodd LE. Remdesivir for the Treatment of Covid-19 - Preliminary Report. Reply. N Engl J Med. 2020;383:994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 346] [Article Influence: 69.2] [Reference Citation Analysis (0)] |
| 47. | Siemieniuk R, Rochwerg B, Agoritsas T, Lamontagne F, Leo YS, Macdonald H, Agarwal A, Zeng L, Lytvyn L, Appiah JA, Amin W, Arabi Y, Blumberg L, Burhan E, Bausch FJ, Calfee CS, Cao B, Cecconi M, Chanda D, Cooke G, Du B, Dunning J, Geduld H, Gee P, Hashimi M, Hui DS, Kabra S, Kanda S, Kawano-Dourado L, Kim YJ, Kissoon N, Kwizera A, Laake JH, Machado FR, Mahaka I, Manai H, Mino G, Nsutedu E, Pshenichnaya N, Qadir N, Sabzwari S, Sarin R, Sharland M, Shen Y, Sri Ranganathan S, Souza J, Ugarte S, Venkatapuram S, Quoc Dat V, Vuyiseka D, Stegemann M, Wijewickrama A, Maguire B, Zeraatkar D, Bartoszko J, Ge L, Brignardello-Petersen R, Owen A, Guyatt G, Diaz J, Jacobs M, Vandvik PO. A living WHO guideline on drugs for covid-19. BMJ. 2020;370:m3379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 550] [Article Influence: 110.0] [Reference Citation Analysis (0)] |
| 48. | Deng L, Li C, Zeng Q, Liu X, Li X, Zhang H, Hong Z, Xia J. Arbidol combined with LPV/r vs LPV/r alone against Corona Virus Disease 2019: A retrospective cohort study. J Infect. 2020;81:e1-e5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 306] [Cited by in RCA: 334] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 49. | Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, Ruan L, Song B, Cai Y, Wei M, Li X, Xia J, Chen N, Xiang J, Yu T, Bai T, Xie X, Zhang L, Li C, Yuan Y, Chen H, Li H, Huang H, Tu S, Gong F, Liu Y, Wei Y, Dong C, Zhou F, Gu X, Xu J, Liu Z, Zhang Y, Li H, Shang L, Wang K, Li K, Zhou X, Dong X, Qu Z, Lu S, Hu X, Ruan S, Luo S, Wu J, Peng L, Cheng F, Pan L, Zou J, Jia C, Wang J, Liu X, Wang S, Wu X, Ge Q, He J, Zhan H, Qiu F, Guo L, Huang C, Jaki T, Hayden FG, Horby PW, Zhang D, Wang C. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382:1787-1799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3386] [Cited by in RCA: 3625] [Article Influence: 725.0] [Reference Citation Analysis (0)] |
| 50. | Bein T, Grasso S, Moerer O, Quintel M, Guerin C, Deja M, Brondani A, Mehta S. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Med. 2016;42:699-711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 147] [Article Influence: 16.3] [Reference Citation Analysis (0)] |