Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.81
Peer-review started: September 28, 2020
First decision: November 3, 2020
Revised: November 10, 2020
Accepted: November 14, 2020
Article in press: November 14, 2020
Published online: January 6, 2021
Processing time: 94 Days and 21 Hours
Computed tomography (CT) has become a routine preoperative examination for tibial plateau fractures (TPFs). Assessing the location of the fragment and intercondylar eminence fracture can provide clinicians with valuable information; however, the evaluation of traumatic meniscal lesion (TML) and arthroscopic management are controversial.
To predict TML by three-dimensional skeletal anatomy changes in unilateral TPF and bilateral TPF on preoperative thin layer CT.
Acute fracture of tibial plateau patients undergoing arthroscopic surgery between December 2017 and December 2019 were included in this retrospective study. The type, zone, and location of TMLs were diagnosed based on the operation records and/or arthroscopic videos. Measurement of three-dimensional fracture morphology included the following: Frontal fragment width of plateau, sagittal fragment subsiding distance (FSD), sagittal fracture line distance, sagittal posterior tibial slope, and transversal area ratio of fragment area) on preoperative CT three-dimensional plane. The correlation of TML with skeletal values was calculated according to unicondylar TPFs and bicondylar TPFs.
A total of 67 patients were enrolled in this study, among which 30 patients had TMLs, lateral/medial (23/7). FSD was a particularly positive factor to predict TML, with odds ratio of 2.31 (1.26-5.63). On sagittal view of CT, FSD degree of 8 mm and posterior tibial slope exceeding 11.74° implied enhanced risk of TML in bicondylar TPFs. On coronal view, once fragment width of plateau surpassed 3 cm, incidence of TML reached 100%. On transverse view, area ratio of fragment as enhanced risk of 5.5% and FSD > 4.3 mm for predicting TML were observed in unicondylar TPFs.
TML can be predicted by different parameters on preoperative CT views according to unicondylar fractures and bicondylar TPFs.
Core Tip: On sagittal view of computerized tomography, fragment subsiding distance degree of 8 mm and posterior tibial slope exceeding 11.74° implied enhanced risk of traumatic meniscal lesion (TML) in bicondylar tibial plateau fractures. On coronal view, once fragment width of plateau surpassed 3 cm, incidence of TML reached 100%. On transverse view, area ratio of fragment area as enhanced risk of 5.5% and fragment subsiding distance > 4.3 mm for predicting TML was observed in unicondylar tibial plateau fractures.
- Citation: Chen YD, Chen SX, Liu HG, Zhao XS, Ou WH, Li HX, Huang HX. Is traumatic meniscal lesion associated with acute fracture morphology changes of tibia plateau? A series of arthroscopic analysis of 67 patients. World J Clin Cases 2021; 9(1): 81-90
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/81.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.81
It is now commonly accepted that traumatic meniscal lesion (TML) is one of the most common inter-articular soft-injuries in acute TPFs[1-3], as confirmed through arthroscopic findings[4]. Computed tomography (CT) can offer precise diagnosis for anterior and posterior osseous avulsions, but subtle meniscus information obtained from CT may be less than magnetic resonance imaging[5], which is not a conventional preoperative scan in many states, unfortunately. Minimally invasive surgery and accelerated enhanced recovery after surgery lead to an increasing number of arthroscopic managements for TPFs[6]. There is medical literature that suggests CT shows a relationship between the occurrence of lateral meniscal lesions and the state of fracture depression in the lateral TPFs (85 cases)[7,8]. Recently, it has been reported that arthroscopic meniscal lesions contain degenerative tears with partial fracture parameters on CT, according to the degree of fracture severity[9]. To our knowledge, the true value of three-dimensional CT is not clear for evaluating the type, zone, and location of TMLs in unicondylar fractures and bicondylar fractures.
A total of 67 consecutive acute TPF patients were enrolled in the sports trauma medicine center from December 2017 to December 2019. Three-dimensional CT scan should be primarily performed preoperatively, and further arthroscopic management included meniscal debride/stitching and minimally invasive internal fixation surgery of TPFs. Fractures according to Schatzker type and the Association for Osteosynthesis/ Orthopedic Trauma Association were recorded (Table 1). Ipsilateral femoral fractures and isolated tibial avulsion fractures were excluded; meanwhile, in cases where 64-slice three-dimensional CT scans (sagittal plane, frontal plane, and axial plane) were not performed preoperatively, or surgery was delayed for more than 21 d, the patients were excluded from this study. The same applied to fracture revisions of tibial plateau.
| Fracture type | Characteristics | Number |
| Side, left /right | 33/34 | |
| Sex, male/female | 30/37 | |
| Unicondylar fracture | Lateral split fracture | 3 |
| Lateral split and depression fracture | 16 | |
| Lateral depression fracture | 12 | |
| Medial plateau fracture | 11 | |
| Bicondylar fracture | bicondylar split fracture | 13 |
| bicondylar with diaphyseal fracture | 12 | |
| AO/OTA | B1 | 5 |
| B2 | 18 | |
| B3 | 11 | |
| C1 | 8 | |
| C2 | 12 | |
| C3 | 13 |
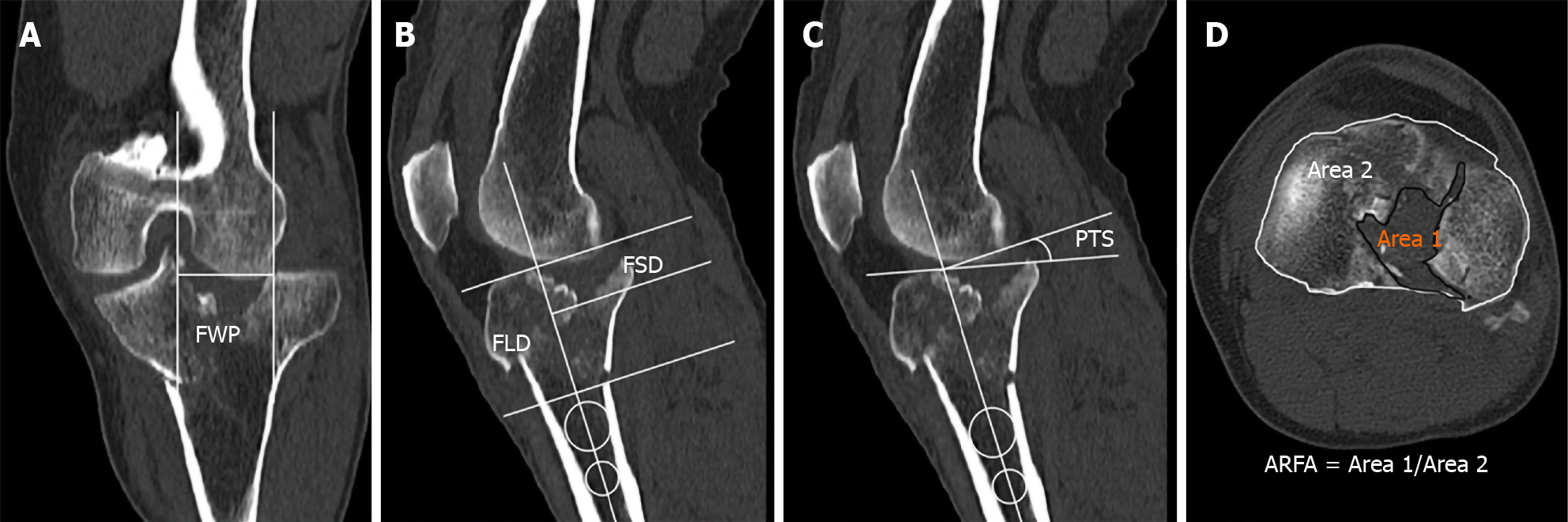
Fracture classification (Association for Osteosynthesis/Orthopedic Trauma Association and Schatzker) was performed by two authors (Radiologist, Trauma surgeon), and measurement of fracture displacement was completed by the other three authors. Condition of scanning: Gem CT (Discovery CT 750 HD, GE Company, Boston, MA, United States), bone joint scanning mode, voltage 120 KVP, current 630 mA. The matrix was 512 × 512, the scanning time was 1 s, the bed moving speed was 1-5 s, the layer thickness was 1.25 mm, the three-dimensional reconstruction distance was 1 mm, the lower limit of CT threshold was 140-300, the upper limit was 2000-2048, and the interval was 0.5-2.0; window width: 1500 HU; window level: 500 HU. The sample was demonstrated as below: Figure 1A-D male, 60-years-old, unicondylar fracture, motorcycle injury.
Fragment width of plateau: The largest width between fracture lines on coronal plane. We took the widest distance at the standard plateau line among multiple fracture lines (Figure 1A).
Fragment subsiding distance: The distance from the articular surface to the distal end of the largest fragment depression by using the intramedullary alignment line as a reference line on sagittal plane. We chose the highest anterior-posterior cartilage surface if there was not a true plateau line in bicondylar fracture (Figure 1B).
Fracture line distance: The distance from the articular surface to the distal end of the largest fracture line was determined by using the intramedullary alignment line as a reference line on sagittal plane. We chose the highest anterior-posterior cartilage surface if there was not a true plateau line in bicondylar fracture (Figure 1B).
Posterior tibial slope: The angle between the articular surface and a line perpendicular to the proximal anatomic axis of the tibia on the sagittal plane. If it was a negative number, we took the absolute value (Figure 1C).
Area ratio of fracture area: Ratio of area1/area2, the range of fracture blocks involved and total plateau area by using the polygon measurement tool at the fibular head on the axial plane (Figure 1D).
TML diagnostic criteria: Access to surgical arthroscopic video Records (Smith & Nephew Company, London, United Kingdom) and/or operation records with or without TML: Side (left/right), zone (white-white, red-white, red-red), location (anterior horner, midbody, posterior horner), patterns of TMLs were widely applicated[10], and covered before reduction and stitching via medial and lateral compartment arthroscopy. Diagnosis of TMLs was all performed by the two senior professionals with over 20 years’ experience in sports medicine. Ordinary supine position and tourniquet pressured 300 mmHg pre-surgery were conventional for patients suffering lower limb fracture. Standard anterior-lateral portal and anterior-medial portal were settled up before any tractive fracture reduction to prevent re-injury. Patients with TMLs were observed but not treated. Next, closed reduction and internal fixation were carried out. Once approving reduction was up to anatomic reduction standard, TMLs were performed by debridement, partial meniscectomy, or suture repair.
A software package PASW 25.0 (SPSS Inc., IBM Corp., Armonk, NY, United States) was carried out for predicting risk of TMLs. The location, zone, and pattern of TMLs were primarily calculated and then divided by unicondylar fractures and bicondylar fractures. Dividing a fracture into unicompartment and bicompartment is the most reliable method[11]. The pathophysiological parameters of the TML were first weighted by the single frequency, followed by the chi-square test of the cross table in the descriptive statistical analysis. All measured values of fragment width of plateau (FWP), fragment subsiding distance (FSD), fracture line distance (FLD), posterior tibial slop (PTS), and area ratio of fracture area (ARFA) were shown as a result of mean ± standard deviation (SD) and odds ratio (OR) value [95% confidence interval(CI)]. Association of each potential predictor was employed by one-way analysis of variance and binary regression analysis in TML group and normal group after verifying homogeneity of variance. Receiver operating characteristic (ROC) analysis was applied to resolve the degree and threshold of each latent parameter for cast TMLs. Descriptive statistics were expressed as percentage or mean ± SD, OR value (95%CI). All tests were significant with P < 0.05, bilaterally.
A total of 30 patients of TMLs (44.8%, 30/67) (Table 2) were confirmed by arthroscopic examination. Incidence of male TMLs was 16/25 (64%), and that of female TMLs was 14/42 (33.3%), among which 16 cases were left TMLs and 14 were right.
| Meniscus physiopathology | Unicondylar TPF, n = 42, incidence | Bicondylar TPF, n = 25, incidence | P value |
| Lateral | 16 (38.9%) | 7 (28.0%) | 0.4 |
| Medial | 1 (2.4%) | 2 (8.0%) | 0.28 |
| Combined | 3 (7.1%) | 1 (4.0%) | 0.57 |
| Location | |||
| Anterior horner | 4 (9.5%) | 2 (8.0%) | 0.83 |
| Mid body | 11 (26.2%) | 7 (28.0%) | 0.87 |
| Posterior horner | 8 (19.0%) | 2 (8.0%) | 0.22 |
| Zone | |||
| White-white | 16 (38.9%) | 5 (20.0%) | 0.12 |
| Red-white | 7 (16.7%) | 1 (4.0%) | 0.12 |
| Red-red | 0 | 5 (20.0%) | 0.01 |
| Tear pattern | |||
| Oblique tear, parrot beak | 13(31.0%) | 5 (20.0%) | 0.32 |
| Longitude tear, bucket handle | 0 | 4 (16.0%) | 0.01 |
| Radical tear, transverse | 1 (2.4%) | 0 | 0.44 |
| Complex tear | 5 (11.9%) | 1 (4.0%) | 0.27 |
On frontal plane of CT, the mean FWP was (3.05 ± 1.31) cm and (2.54 ± 1.19) cm in total TPF group with and without TMLs and had no significant difference. Respectively, FWP demonstrated significant difference between groups (4.25 ± 0.99); contrast to (3.05 ± 1.39) in bicondylar TPFs (OR = 2.30, 95%CI: 1.02-5.65) but not in unicondylar TPFs.
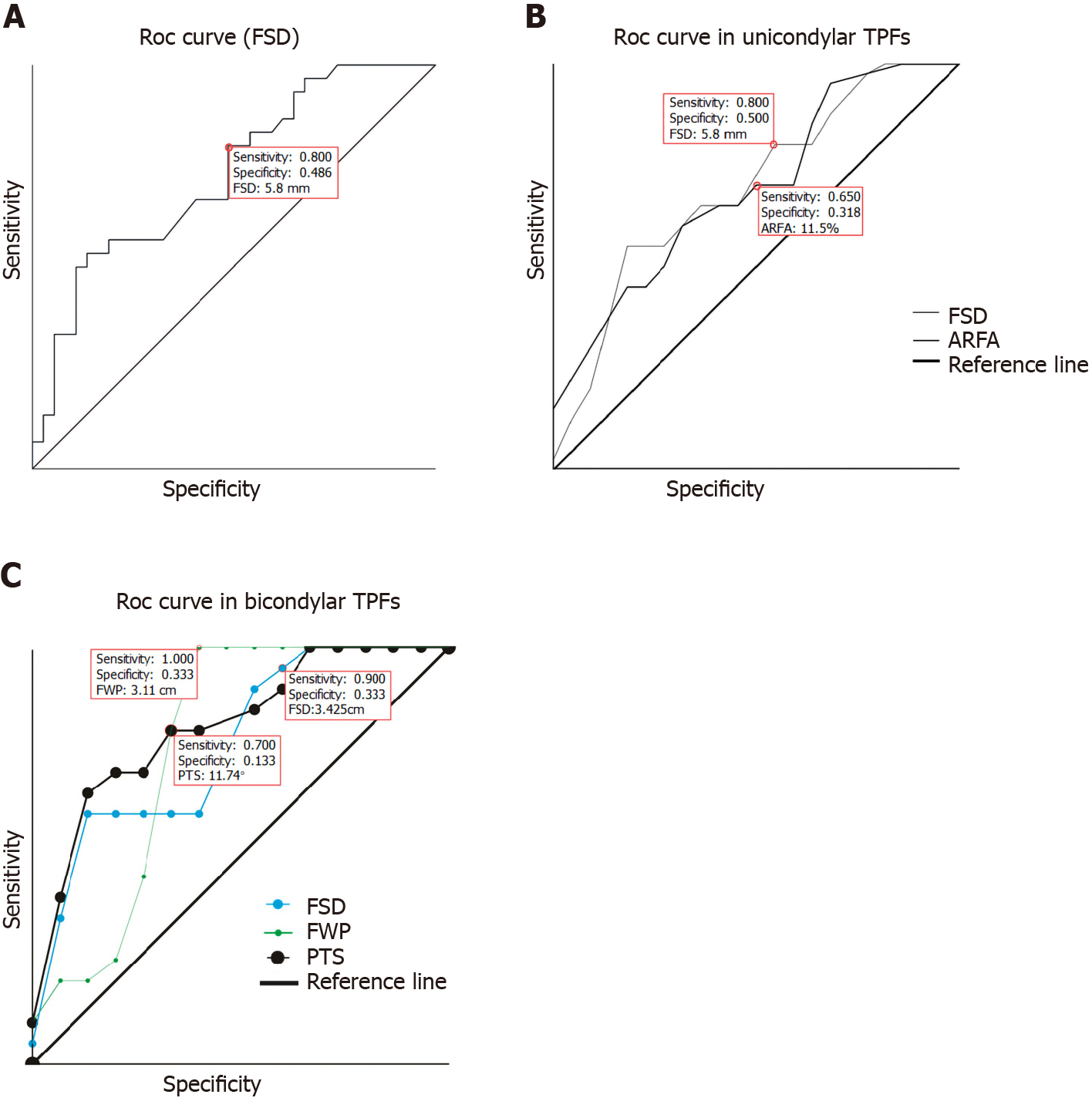
On sagittal view of CT, the FSD range with and without TMLs in total TPFs was (1.63 ± 1.31) cm and (0.78 ± 0.76) cm, respectively, OR = 2.31 (1.26-5.63), with significant mean difference between groups (P = 0.001). A similar effect was manifested in unicondylar fractures (OR = 2.53, P = 0.03) and bicondylar fractures (OR = 2.95, P = 0.03). ROC curve (Figure 2A) showed that once FSD > 5.8 mm, sensitivity of predicting TMLs reached 80%. However, there was no apparent statistical significance in FWP, PLS, and ARFA in total TPF group (Table 3).
| Fracture group | Variable | OR | 95%CI | ROC area | P value |
| Unicondylar TPF | FWP | 0.95 | 0.68 -2.54 | 0.58 | 0.36 |
| FSD | 2.53 | 1.02-6.28 | 0.69 | 0.03 | |
| FLD | 0.42 | 0.65-1.14 | 0.44 | 0.52 | |
| PTS | 1.10 | 0.73-1.27 | 0.49 | 0.95 | |
| ARFA | 0.07 | 0.00-0.19 | 0.71 | 0.02 | |
| Bicondylar TPF | FWP | 2.30 | 1.02-5.65 | 0.77 | 0.03 |
| FSD | 2.95 | 1.07-6.66 | 0.76 | 0.03 | |
| FLD | 1.15 | 0.79-1.32 | 0.52 | 0.86 | |
| PTS | 1.40 | 0.96-3.66 | 0.81 | 0.01 | |
| ARFA | 0.13 | 0.00-0.27 | 0.51 | 0.93 | |
| Total TPF | FWP | 1.51 | 0.69-1.84 | 0.63 | 0.07 |
| FSD | 2.31 | 1.26-5.63 | 0.73 | 0.00 | |
| FLD | 0.62 | 0.59-1.01 | 0.47 | 0.73 | |
| PTS | 1.18 | 0.90-1.42 | 0.59 | 0.18 | |
| ARFA | 0.11 | 0.01-0.22 | 0.62 | 0.09 |
The mean FLD in unicondylar TPFs with TMLs was (3.79 ± 2.61) cm, and it was similar in the group without TMLs, which averaged (3.21 ± 3.29) cm, OR = 0.62 (95%CI: 0.59-1.01). This did not demonstrate statistical significance in bicondylar TPFs and in total TPFs (P > 0.05).
The PTS was (11.26 ± 2.86) degrees and (8.38 ± 2.61) degrees in bicondylar fractures with and without TMLs, which was significantly different (OR = 1.40, 95%CI: 0.96-3.66). The area under the ROC curve (0.81, P = 0.01) is shown in Figure 2C.
On transversal view of CT, the AFRA was (0.14 ± 0.08), contrast to (0.08 ± 0.05) in unicondylar TPF with and without TMLs, and it demonstrated apparent significance (F = 7.39, OR = 0.07, 95%CI: 0.00-0.19, P = 0.02). ROC curve (Figure 2B and C) shows that PTS, FWP, and FSD serve as prediction models for TMLs in bicondylar fracture.
Meniscus tear can be divided into structural and unstructural tears. The latter includes contusion and degenerative lesion, which are not reckoned as similar results for surgery management and physical exercises[12]. Although management of structural meniscal tear is still controversial, TMLs usually need repair. We calculated the lower incidence of TMLs that required surgical intervention and contrasted it to 92.2%-99% in the previous study of Schatzker II fracture of tibial plateau and the recent research (71 Lateral, 15 medial/132 cases) in acute TPFs[7,13]. There are no statistically different results according to the severity of fracture, including Schatzker IV, which is consistent with previous literature[14,15]. Our further study, however, shows that red-red zone, longitude tear (bucket handle) pattern of TMLs demonstrated different results in different condylar number groups. Thus arthroscopy has a better indication for bicondylar TPFs that are associated with meniscal longitude tear (bucket handle) in minimally invasive reduction of articular surface fragment.
Tibial plateau is divided into medial and lateral plateau by intercondylar eminence anatomically. TPFs commonly contain medial and lateral unicondylar fractures and bicondylar fractures, combined eminence fracture, intra-articular ligament, cartilage, and meniscus injuries[16-19]. Such a classification is feasible[11,20]. This classification is more conducive to predicting pure meniscus injury preoperatively for radiologists and managing TMLs intraoperatively for surgeons, and it may be appropriate and accessible for multidisciplinary studies (radiologists, etiologists, orthopedic surgeons, sports medicine surgeons, anatomists, and trauma surgeons). It is necessary to conduct in-depth research on the mechanism and management for certain special fractures, such as segon fracture, avulsion fracture, and Schatzker IV fracture, which are commonly combined with cruciate ligament injuries.
It has been suggested by a recent study that lateral TPFs with articular impaction ≥ 4.3 mm on CT mean inevitably meniscus tear, as the risk of meniscus injury increased by 21% when articular displacement increased 1 mm, especially in the anterior region by four zone methods[8]. The result was also confirmed by other researches[7,13,21,22]. In Borrelli’s retrospective study, 83% of meniscus lesions happened when articular surface compression increased more than 5 mm, and when it was greater than 8 mm at the lateral compartment, the instance of meniscus lesion was 53%[23]. Although such methods as X-ray, CT, and magnetic resonance imaging were employed, arthroscopy remains the golden standard for the diagnosis of meniscus injury. FSD can be implicated independently with TMLs, OR = 2.31 (1.26-5.63). Therefore, in frontal images, FSD should be a predictor of meniscus damage, relevant to acute unicondylar and bicondylar TPFs, in sharp contrast to FLD. The study also demonstrates that the fracture width was a significant predictor of incidence of meniscal injury, and if its width was more than 8 mm, the proportion of meniscus injuries was as high as 78%[23]. On X-ray when it surpassed 7.4 mm, the incidence of TMLs increased[24].
Our study has found that once FWP surpasses 3 cm, the incidence of TMLs reaches 100% in bicondylar TPFs (Figure 2C). This is inconsistent with previous reports, which may be due to different measurement methods adopted and different samples included. The former, definition of the width of the fracture based on distance from lateral femoral condyle, may differ from our research, which used the largest fragment width in line of articular surface. Even so, we have found that FSD, the slope of the sagittal plane, and FWP of the frontal plane are related to the occurrence of meniscal trauma in bicondylar fracture, which can be further improved to explain the tibial fracture mechanism of plateau and direction of the violence associated with it.
Is PTS a risk factor associated with TMLs? There are few studies on posterior slope with TPFs. A recent total knee arthroplasty study by Williams et al[25] has shown that PTS may be a crucial factor during step-up and step-down activities, especially for cruciate ligament tears[26]. Similar to the high tibial osteotomy research of medial open-wedge type, which considered that increase in PTS would lead to amendment loss in coronal images[27], our research is the first to suggest that greater risk of TMLs is observed when PTS reach 11.74° in bicondylar fractures. Recent research has shown that the PTS measurements obtained by lateral anatomical axis on full-length or proximal tibia radiographs are different from mechanical axial measurements[28]. The Chinese cadaveric study revealed that the PTS was 11.5° in the intramedullary way and 14.7 degrees in the extramedullary way. The PTS has a certain positive correlation appearance with age[29]. Our results had no difference in age baseline and when PTS adopted intramedullary measurement and reached 11.74° of great risk.
In a recent study, the predictive risk of ACL injury in volumetric lateral joint depressions was ≤ 209.5 mm2 but not meniscal injury[9]. In contrast to our study, there was no significant mean difference and 95%CI in bicondylar fracture with and without TMLs. When ARFA achieved 11.5%, sensitivity and specificity (0.65 and 0.32) were at the ideal range (Table 3 and Figure 2C). We speculate that the volume and depression of the fragment may be helpful in predicting the TMLs in unicondylar fractures, the mechanism, force direction, and size of which are different from those of bicondylar TPFs.
There are some limitations in our research: (1) Delayed and comminuted fractures combined with neurovascular injuries, external fixation, or compartment syndrome were not included in this research, which may result in selectivity bias; and (2) The inclusion criteria and exclusion criteria for cases were strict, incomplete meniscus data records were not included, and clinical cases were relatively not many, which requires a multi-center and larger sample for in-depth study.
Plateau subsiding distance measured on sagittal CT images portends a higher stake of meniscus tear associated with unicondylar TPFs and bicondylar TPFs. ARFA measured on axial views might predict TMLs for unicondylar TPFs; PTS and FMP measured on sagittal plane might predict TMLs for bicondylar TPFs, respectively.
Few studies have shown the correlation of traumatic meniscal lesion (TML) diagnosed via arthroscopy and acute tibial plateau fracture according to well-accepted single and bilateral classification.
How to predict TML by three-dimensional skeletal anatomy changes in unilateral tibial plateau fractures (TPFs) and bilateral TPFs without magnetic resonance imaging or arthroscopy? Should surgery be done by optimal, open reduction, minimally invasive incision or via arthroscope?
We performed a retrospective study of patients diagnosed with acute fracture of tibial plateau who underwent arthroscopic surgery.
In this retrospective case series, the type, zone, and location of TMLs were diagnosed based on the operation records and/or arthroscopic videos. Measurement of three-dimensional fracture morphology was performed on preoperative computed tomography (CT) three-dimensional plane. The correlation of TML with skeletal values was calculated according to unicondylar TPFs and bicondylar TPFs.
In this study, a total of 30 patients had TMLs, lateral/medial (23/7). The incidence of TMLs was not related to TPF type. Fragment subsiding distance (FSD) was a particularly positive factor to predict TML, OR = 2.31 (1.26-5.63) for each TPF type. On coronal view, once fragment width of plateau surpassed 3 cm, incidence of TML reached 100%; on sagittal view of CT, FSD degree of 8 mm, and posterior tibial slope exceeding 11.74° implied enhanced risk of TML in bicondylar TPFs. On transverse view, ARFA as enhanced risk of 5.5% and FSD > 4.3 mm for predicting TML were observed in unicondylar TPFs.
TML can be predicted by different parameters on preoperative three dimensional CT views (frontal, sagittal, and axial planes) according to unicondylar TPFs and bicondylar TPFs. Plateau subsiding distance measured on sagittal CT images portends a higher stake of meniscus tear associated with each group TPFs.
Arthroscopy is still the gold standard for diagnosing meniscus injuries and is suitable for all types of TPFs. According to the research, further in-depth research requires a multi-center study with larger sample for each type of TPF.
Manuscript source: Unsolicited manuscript
Specialty type: Pathology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Uz Zaman M S-Editor: Zhang H L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Krause M, Preiss A, Meenen NM, Madert J, Frosch KH. "Fracturoscopy" is Superior to Fluoroscopy in the Articular Reconstruction of Complex Tibial Plateau Fractures-An Arthroscopy Assisted Fracture Reduction Technique. J Orthop Trauma. 2016;30:437-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | Warner SJ, Garner MR, Schottel PC, Fabricant PD, Thacher RR, Loftus ML, Helfet DL, Lorich DG. The Effect of Soft Tissue Injuries on Clinical Outcomes After Tibial Plateau Fracture Fixation. J Orthop Trauma. 2018;32:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84:1541-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 154] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Abdel-Hamid MZ, Chang CH, Chan YS, Lo YP, Huang JW, Hsu KY, Wang CJ. Arthroscopic evaluation of soft tissue injuries in tibial plateau fractures: retrospective analysis of 98 cases. Arthroscopy. 2006;22:669-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Mui LW, Engelsohn E, Umans H. Comparison of CT and MRI in patients with tibial plateau fracture: can CT findings predict ligament tear or meniscal injury? Skeletal Radiol. 2007;36:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Zawam SHM, Gad AM. Arthroscopic Assisted Reduction and Internal Fixation of Tibial Plateau Fractures. Open Access Maced J Med Sci. 2019;7:1133-1137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Ringus VM, Lemley FR, Hubbard DF, Wearden S, Jones DL. Lateral tibial plateau fracture depression as a predictor of lateral meniscus pathology. Orthopedics. 2010;33:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Salari P, Busel G, Watson JT. A radiographic zone-based approach to predict meniscus injury in lateral tibial plateau fracture. Injury. 2020;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Chang H, Zheng Z, Shao D, Yu Y, Hou Z, Zhang Y. Incidence and Radiological Predictors of Concomitant Meniscal and Cruciate Ligament Injuries in Operative Tibial Plateau Fractures: A Prospective Diagnostic Study. Sci Rep. 2018;8:13317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Fox AJ, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28:269-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 11. | Lee AK, Cooper SA, Collinge C. Bicondylar Tibial Plateau Fractures: A Critical Analysis Review. JBJS Rev. 2018;6:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | van de Graaf VA, Noorduyn JCA, Willigenburg NW, Butter IK, de Gast A, Mol BW, Saris DBF, Twisk JWR, Poolman RW; ESCAPE Research Group. Effect of Early Surgery vs Physical Therapy on Knee Function Among Patients With Nonobstructive Meniscal Tears: The ESCAPE Randomized Clinical Trial. JAMA. 2018;320:1328-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 120] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 13. | Tang HC, Chen IJ, Yeh YC, Weng CJ, Chang SS, Chen AC, Chan YS. Correlation of parameters on preoperative CT images with intra-articular soft-tissue injuries in acute tibial plateau fractures: A review of 132 patients receiving ARIF. Injury. 2017;48:745-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Sweigart MA, Athanasiou KA. Toward tissue engineering of the knee meniscus. Tissue Eng. 2001;7:111-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 150] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Yan B, Sun J, Yin W. The prevalence of soft tissue injuries in operative Schatzker type IV tibial plateau fractures. Arch Orthop Trauma Surg. 2020;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Molenaars RJ, Mellema JJ, Doornberg JN, Kloen P. Tibial Plateau Fracture Characteristics: Computed Tomography Mapping of Lateral, Medial, and Bicondylar Fractures. J Bone Joint Surg Am. 2015;97:1512-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 116] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 17. | Krupp RJ, Malkani AL, Roberts CS, Seligson D, Crawford CH 3rd, Smith L. Treatment of bicondylar tibia plateau fractures using locked plating versus external fixation. Orthopedics. 2009;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Markhardt BK, Gross JM, Monu JU. Schatzker classification of tibial plateau fractures: use of CT and MR imaging improves assessment. Radiographics. 2009;29:585-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Kfuri M, Schatzker J. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 2018;49:2252-2263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 157] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 20. | Charalambous CP, Tryfonidis M, Alvi F, Moran M, Fang C, Samarji R, Hirst P. Inter- and intra-observer variation of the Schatzker and AO/OTA classifications of tibial plateau fractures and a proposal of a new classification system. Ann R Coll Surg Engl. 2007;89:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Wang J, Wei J, Wang M. The distinct prediction standards for radiological assessments associated with soft tissue injuries in the acute tibial plateau fracture. Eur J Orthop Surg Traumatol. 2015;25:913-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Spiro AS, Regier M, Novo de Oliveira A, Vettorazzi E, Hoffmann M, Petersen JP, Henes FO, Demuth T, Rueger JM, Lehmann W. The degree of articular depression as a predictor of soft-tissue injuries in tibial plateau fracture. Knee Surg Sports Traumatol Arthrosc. 2013;21:564-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Borrelli J Jr. Management of soft tissue injuries associated with tibial plateau fractures. J Knee Surg. 2014;27:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Stahl D, Serrano-Riera R, Collin K, Griffing R, Defenbaugh B, Sagi HC. Operatively Treated Meniscal Tears Associated With Tibial Plateau Fractures: A Report on 661 Patients. J Orthop Trauma. 2015;29:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Williams D, Metcalfe A, Madete J, Whatling G, Kempshall P, Forster M, Lyons K, Holt C. The relationship between alignment, function and loading in total knee replacement: In-vivo analysis of a unique patient population. J Biomech. 2020;112:110042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Winkler PW, Hughes JD, Musahl V. Editorial Commentary: Respect the Posterior Tibial Slope and Make Slope-Reducing Osteotomies an Integral Part of the Surgical Repertoire. Arthroscopy. 2020;36:2728-2730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Asada S, Akagi M, Mori S, Matsushita T, Hashimoto K, Hamanishi C. Increase in posterior tibial slope would result in correction loss in frontal plane after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2012;20:571-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Dean RS, DePhillipo NN, Chahla J, Larson CM, LaPrade RF. Posterior Tibial Slope Measurements Using the Anatomic Axis Are Significantly Increased Compared to Those That Use the Mechanical Axis. Arthroscopy. 2020;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 29. | Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15:224-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 111] [Article Influence: 4.4] [Reference Citation Analysis (0)] |