Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.61
Peer-review started: April 24, 2020
First decision: September 14, 2020
Revised: October 14, 2020
Accepted: November 9, 2020
Article in press: November 9, 2020
Published online: January 6, 2021
Processing time: 248 Days and 7.4 Hours
Surgery is often indicated for patients with massively prolapsed intervertebral disc herniation. The interlaminar endoscopic spine system (iLESSYS) Delta 6-mm working channel endoscope has advantages over other systems. The aim of this study was to explore the benefits and complications of using the iLESSYS Delta for the treatment of massively prolapsed intervertebral disc herniation.
To explore the clinical benefits of treating massively prolapsed lumbar intervertebral disc herniation with the iLESSYS Delta endoscope.
In this study, the data of 37 patients who underwent surgery with the iLESSYS Delta endoscope at The Affiliated Hospital of Qingdao University were retrospectively analyzed. Intraoperative blood loss, operation time, and complications were collected. The visual analog scale (VAS), oswestry disability index (ODI), and modified MacNab criteria were determined before and at 1 d, 3 mo, and 6 mo after surgery.
The mean intraoperative blood loss was 20.4 ± 1.2 mL. The mean operation time was 97.3 ± 12.4 min. The VAS scores for leg and back pain decreased from 68.0 ± 7.3, 34.4 ± 8.5 before operation to 2.5 ± 1.7, 5.5 ± 1.9 at 6 mo after surgery, respectively. The ODI also decreased from 60.2 ± 7.3 to 17.9 ± 3.4 at 6 mo after surgery. The improvement rate of the MacNab score was 86.4%, which was considered excellent. No spinal dural injury, nerve root injury, secondary protrusion of intervertebral disc, or myeloid hypertension was found during follow-up.
The iLESSYS Delta 6-mm working channel endoscope has several advantages in terms of clinical and functional benefits, complications, and low risk of residual vertebral pulp in treating patients with massively prolapsed intervertebral disc herniation.
Core Tip: Surgery is often indicated for patients with massively prolapsed intervertebral disc herniation. The interlaminar endoscopic spine system (iLESSYS) Delta 6-mm working channel endoscope has advantages over other systems but there are still few studies about it. The results suggest that the iLESSYS Delta 6-mm working channel endoscope has several advantages in terms of clinical and functional benefits, complications, and low risk of residual vertebral pulp in treating patients with massively prolapsed lumbar intervertebral disc herniation.
- Citation: Meng SW, Peng C, Zhou CL, Tao H, Wang C, Zhu K, Song MX, Ma XX. Massively prolapsed intervertebral disc herniation with interlaminar endoscopic spine system Delta endoscope: A case series. World J Clin Cases 2021; 9(1): 61-70
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/61.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.61
Lumbar disk herniation is the protrusion, extrusion, or sequestration of the intervertebral disk from its usual anatomic location. It may be asymptomatic or may result in radiculopathy or non-radicular pain[1]. It can result from normal aging or a recent trauma and cause mechanical compression of the nerve root by herniated material or sensitization of the nerve root[1]. Lumbar disk herniation is found incidentally in 20%-36% of patients undergoing computed tomography (CT) or magnetic resonance imaging (MRI)[2]. The incidence of hospitalization due to lumbar disk herniation is 7.8 per 1000 among active adults in Europe[3]. The risk factors include obesity, a history of lower back pain, long periods of standing and bending forward, smoking, physical activity, and genetic factors[1,2]. In most patients, conservative treatments alone will be sufficient to manage the condition, but surgery is indicated in cases of cauda equine syndrome, severe and progressive neurologic deficits, and no improvement after conservative treatments[1,2,4,5].
Massively prolapsed intervertebral disc herniation (i.e. the disc occupying > 50% of the spinal canal on MRI)[6] mainly occurs in middle-aged or young patients who have a history of trauma or lumbar hypermobility. The disease has acute onset and severe radicular pain, and is generally accompanied by cauda equina syndrome and decreased muscle strength in dorsal stretching. Strict conservative treatments including bed rest, dehydration, and anti-inflammatory drugs can improve the condition in many patients[7,8], but symptoms or fear of dural compression and cauda equina syndrome lead to surgery[9-12]. Surgical treatments such as conventional fenestration, transforaminal lumbar interbody fusion (TLIF), and minimally invasive TLIF have definite treatment efficacies and decompression effects and therefore are commonly selected by spine surgeons[6,13,14].
With the advancements of minimally invasive spinal surgery, endoscopic discectomy has been widely applied for the treatment of degenerative spinal diseases such as protrusion of intervertebral disc, spinal canal stenosis, and degenerative spondylolisthesis, and have achieved a new breakthrough in patient outcomes[15,16]. Endoscopic discectomy through both interlaminal and transforaminal approaches can be used for the treatment of massively prolapsed intervertebral disc herniation. The interlaminar endoscopic spine system (iLESSYS) Delta 6-mm working channel endoscope has the advantages of large exploration range and sufficient decompression and therefore has been widely applied in the treatment of lumbar spinal stenosis[17-21]. To date, very few studies have used the iLESSYS Delta 6-mm working channel endoscope for the treatment of prolapsed intervertebral disc herniation.
Therefore, the aim of this study was to explore the benefits and complications of using the iLESSYS Delta 6-mm working channel endoscope for the treatment of massively prolapsed intervertebral disc herniation.
In this case series, patients who underwent surgery with the iLESSYS Delta 6-mm working channel endoscope for the treatment of massively prolapsed intervertebral disc herniation at The Spinal Surgery Department of The Affiliated Hospital of Qingdao University (Shandong, China) from September 2016 to September 2018 were retrospectively analyzed. The patients with infectious spinal diseases, severe spinal canal stenosis, lumbar vertebral instability, or primary or metastatic lumbar vertebra tumors were excluded. The study was approved by the Ethics Committee of The Affiliated Hospital of Qingdao University.
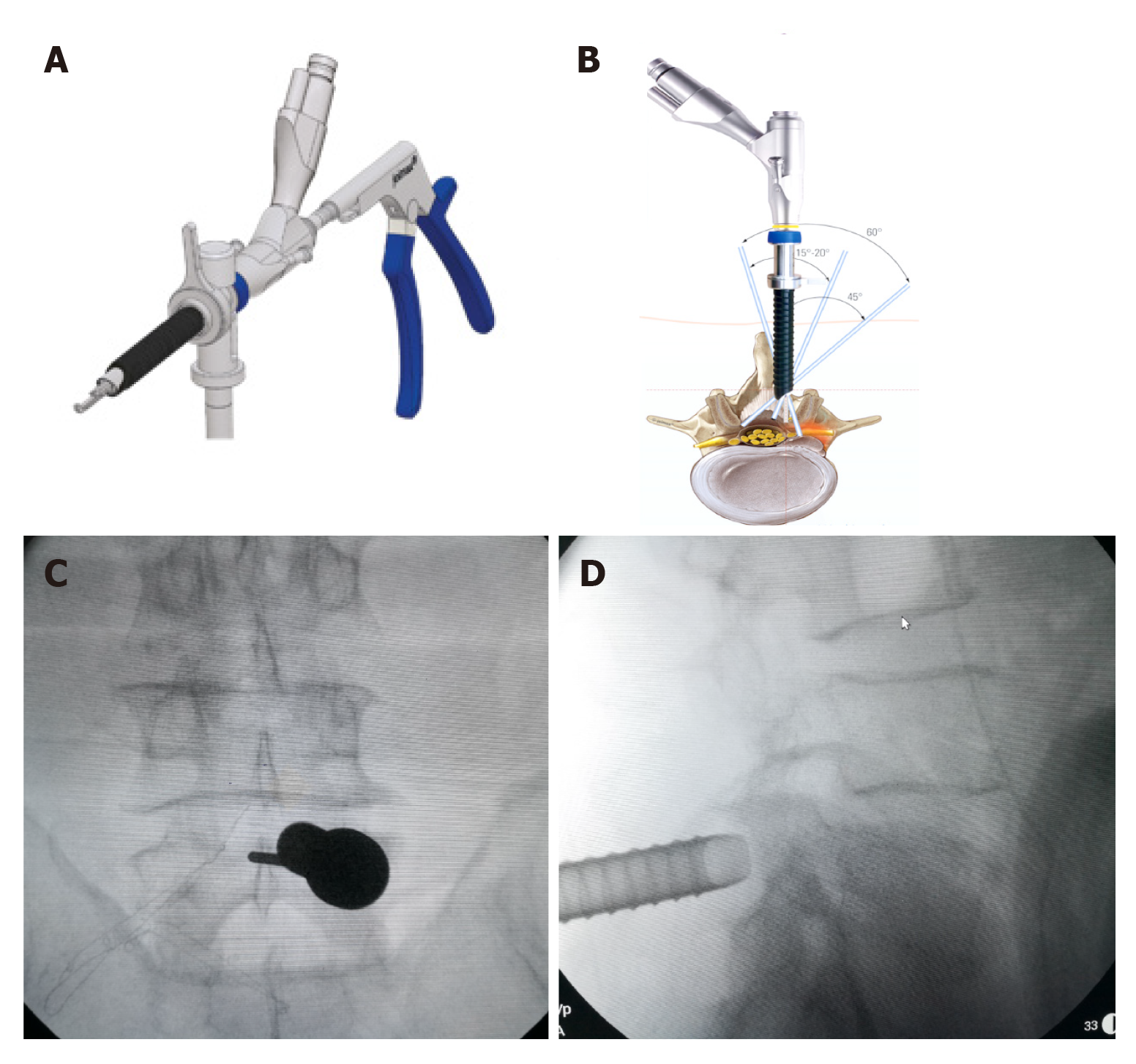
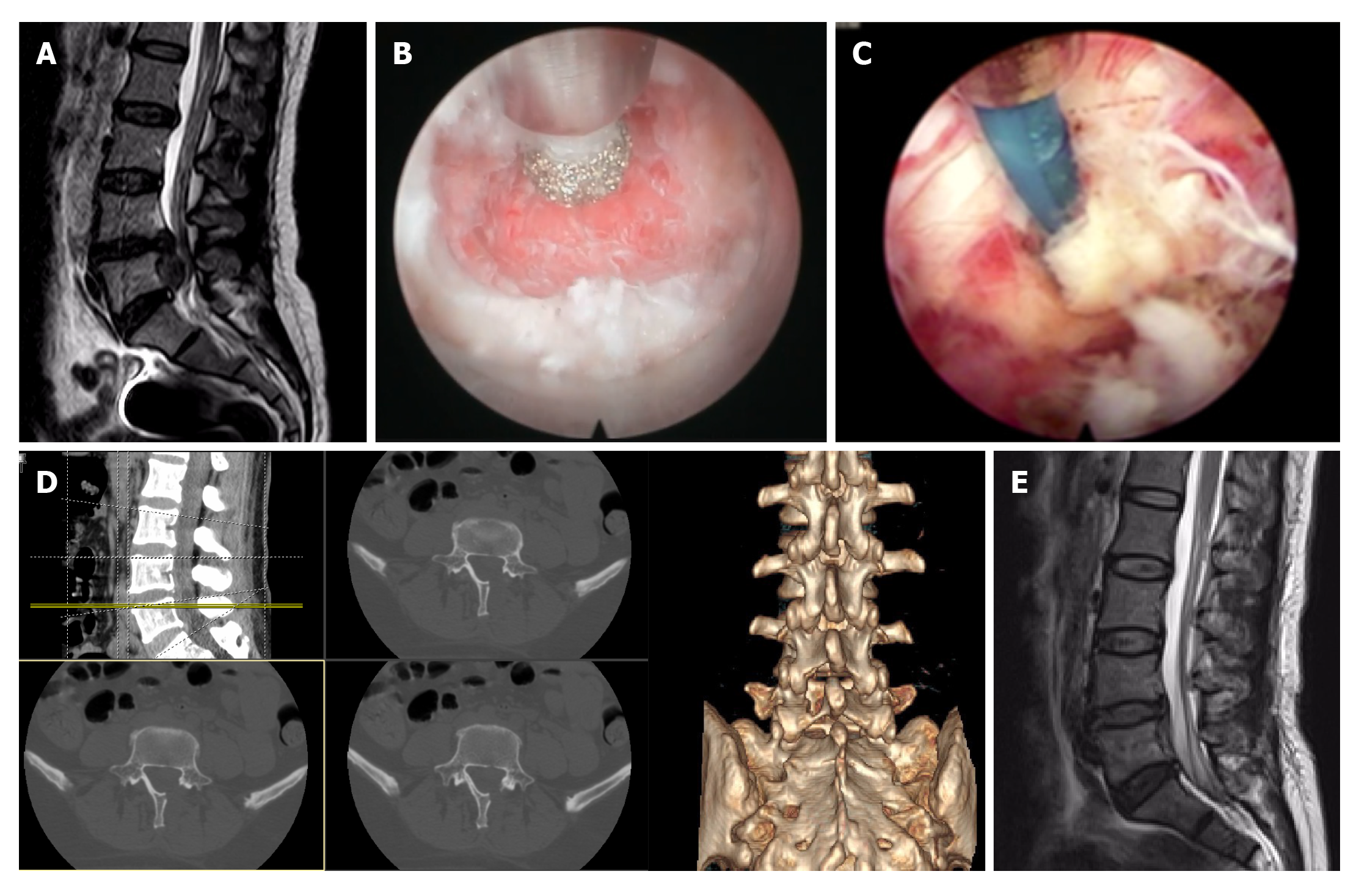
After tracheal intubation and general anesthesia, the patients were placed in the prone position on the operating table. The chest and iliac bone were elevated using cushions, and the operating table was adjusted to expose the laminae interval space. Skin positioning was conducted under the imaging guidance, and the skin and deep fascia were cut using a scalpel. The paraspinal muscle was dilated using a trocar until reaching the vertebral plate, and then the working channel was placed along the trocar channel. The iLESSYS Delta 6-mm working channel endoscope (Figure 1) was inserted after withdrawing the trocar, and the muscles attached to the vertebral plate were separated. An endoscopic bur and bone ribbing rongeur for vertebral plate was used to remove a part of the vertebral plate and increase the laminae interval space, while the zygopophysis was protected (Figure 2). The ligamenta flava was gradually broken through along the medial vertebral plate to expose the spinal canal, and the structures were separated and identified under endoscopy. An endoscopic plectrum could be used to separate the intervertebral disc and surrounding tissues, explore the spinal cord, nerve roots, and vertebral pulp. The vertebral pulp was removed, and further exploration was conducted to make sure there was no residual vertebral pulp. Then the working channel and endoscope were removed, and the incision was sutured. No antibiotics or glucocorticoids were used during the operation.
Methylprednisolone (80 mg) and mannitol (25 g) were intravenously administered to reduce the edema of the nerve roots after surgery. The patients could move by themselves with the assistance of a waist strap at 2 d after surgery and were discharged. Three-dimensional CT scanning and MRI examinations were conducted at 1 d, 3 mo, and 6 mo after surgery to assess the decompression effectiveness, as well as the presence of residual or secondary intervertebral disc herniation.
Data including intraoperative blood loss, operation time, hospital stay, and complications were collected. In addition, the 100-point visual analog scale (VAS), oswestry disability index (ODI) before and at 1 d, 3 mo and 6 mo after surgery were used to assess the clinical outcomes. Modified MacNab criteria after surgery were also used to assess the clinical outcomes at 1 year after surgery, of which the improvement rate of 75%-100% was considered excellent, 50%-74% was considered good, 25%-49% was considered fair, and < 25% was considered poor.
SPSS 17.0 software (SPSS Inc., Chicago, IL, United States) was used for statistical analysis. Continuous data were described as mean ± standard deviation and analyzed using the paired t-test or repeated measure analysis of variance with Tukey’s post hoc test. Categorical data are presented as n (%). Two-sided P values < 0.05 were considered statistically significant.
Among the 37 included patients, there were 21 (56.8%) males and 16 (43.2%) females. The massively prolapsed intervertebral disc herniation was at the L3/4, L4/5, and L5/S1 segment in 2 (5.4%), 21 (56.8%), and 14 (37.8%) patients, respectively. All patients were with radicular pain in unilateral leg and local skin hyperalgesia. Some also had decreased muscle strength of the thigh and ankle in dorsal stretching. In all those patients, conservative treatments resulted in poor efficacy.
All patients were followed up, with a follow-up time ranging from 7 to 13 mo. The mean intraoperative blood loss was 20.4 ± 1.2 mL. The mean operation time was 97.3 ± 12.4 min (range: 80-110 min). The VAS scores for leg pain and back pain decreased from 68.0 ± 7.3 and 34.4 ± 8.5 before operation to 2.5 ± 1.7 and 5.5 ± 1.9 at 6 mo after surgery, respectively (Table 1). The ODI also decreased from 60.2 ± 7.3 before operation to 17.9 ± 3.4 after surgery (Table 1). The improvement rate of the MacNab score was 86.4% (32/37), which was considered excellent.
| Variables | Before | 1 d after | 3 mo after | 6 mo after | P value |
| VAS for back pain | 34.4 ± 8.5 | 10.3 ± 5.3 | 7.7 ± 1.2 | 5.5 ± 1.9 | < 0.01 |
| VAS for leg pain | 68.0 ± 7.3 | 7.6 ± 3.1 | 3.5 ± 1.9 | 2.5 ± 1.7 | < 0.01 |
| ODI | 60.2 ± 7.3 | 22.3 ± 3.4 | 18.8 ± 0.2 | 17.9 ± 3.4 | < 0.01 |
No spinal dural injury or nerve root injury, secondary protrusion of intervertebral disc, or myeloid hypertension was found during follow-up.
Surgery is often indicated for patients with massively prolapsed intervertebral disc herniation[9-12]. The iLESSYS Delta 6-mm working channel endoscope has advantages over other systems[17-21], but there are still few studies about it. Therefore, the aim of this study was to explore the benefits and complications of using the iLESSYS Delta 6-mm working channel endoscope for the treatment of massively prolapsed intervertebral disc herniation. The results suggest that the iLESSYS Delta 6-mm working channel endoscope has several advantages in terms of clinical and functional benefits, complications, and low risk of residual vertebral pulp in treating patients with massively prolapsed intervertebral disc herniation.
Massively prolapsed intervertebral disc herniation is a special type of intervertebral disc herniation that can be detected by MRI but not necessarily by CT since regular CT scanning could only scan the layers of laminae interval space[22]. According to the regional positioning method on the sagittal plane of layers I, II, and III for lumbar disc herniation reported by Hu et al[23], when the CT is restricted to the scanning of layer I, the protruding vertebral pulps at layers II and III cannot be displayed. Therefore, thin-layer CT scanning should be conducted. If the vertebral pulp is calcified, mass shadows can be found on the images. For MR scanning, most patients have acute onset of the massively prolapsed intervertebral disc herniation, and even strict conservative treatments still result in suboptimal outcomes. Some patients have cauda equina syndrome due to mechanical compression, nerve root edema, and blood flow obstruction[24], and thus require an operation. The protruding vertebral pulps are mainly inferior-migrated, but some protruding vertebral pulps can also be superiorly migrated. Severe prolapse is diagnosed when the distance from the lowest margin of the protruding vertebral pulps to the upper border of the vertebral body is > 1 cm[22]. In this study, the margin of the protruding vertebral pulps was prolapsed to the level of the lower border of the lower vertebral body in the most severe cases, and the patients were accompanied with evidently decreased muscle strength of the thighs in dorsal stretching.
Several conventional surgeries, including simple fenestration discectomy, posterior lumbar interbody fusion (PLIF), and TLIF, are available for the treatment of massively prolapsed intervertebral disc herniation[6,13,14]. The operating field is relatively poor in simple fenestration discectomy, which could influence the stability of the zygopophysis and induce iatrogenic instability. On the other hand, TLIF reduces the traction of dura and nerve roots comparing to PLIF but still has several disadvantages, including large area muscle detachment, high volume blood loss, and long hospital stay[25-27]. In addition, open surgery can also lead to epidural scar, lumbar vertebrae instability, postoperative infection, and consequently increase the risk of the failed back surgery syndrome[28], which has attracted more and more attention from surgeons. Therefore, many surgeons are now exploring new surgical methods. With the advancements of minimally invasive spinal surgeries and minimally invasive techniques, minimally invasive spine surgery is becoming accepted. Spinal endoscopy was first introduced in Europe and America but is being developed in China and Korea. Currently, spinal endoscopy has gradually advanced from the Yeung endoscopic spine system (YESS) to the transforaminal endoscopic spine system (TESSYS), and therefore achieved the transformation from “inside-out” to “outside-in”[29,30].
The TESSYS technique can achieve “precise puncture” according to the positions of the protrusion of the intervertebral disc. TESSYS uses cannulated trephines for foraminoplasty to widen the foramen and, therefore, could treat the more distantly prolapsed vertebral pulps than the YESS[31]. As a massively prolapsed intervertebral disc occupies a large area in the spinal canal, the treatments on the protruding vertebral pulp could result in nerve root compression by the working channel and therefore induce nerve root injuries[32]. When trying to achieve a higher head-tilting angle, the increased range for foraminoplasty could potentially induce iatrogenic instability. A sequestration-type disc involves discontinuity between the vertebral body and vertebral pulp. For such cases, intraoperative exploration should be conducted carefully to avoid missing vertebral fractures[33]. PELD generally requires local anesthesia, and feedback from the patients can be obtained during the operation. For patients with massively prolapsed intervertebral disc herniation, inflammation can lead to drastic pain when the vertebral pulp is clamped outward, which could influence the surgery or even lead to surgery termination. In addition, TESSYS has relatively high requirements for beginners. For instance, the operators have to have sufficient anatomic knowledge and 3-dimensional concepts, which have steep learning curves[34].
Comparing with PELD, surgeries through the interlaminal approach could reduce the times of imaging, and the anatomic structures are relatively simple[35]. Therefore, such surgeries are suitable for prolapsed intervertebral disc herniation with certain features such as L5/S1, relatively high iliac crest, and relatively small intervertebral foramen. Incising the ligamenta flava could allow access to the vertebral canal, which is highly safe[36]. In addition, the zygopophysis is not resected, which further reduces the risk of iatrogenic lumbar vertebrae instability. As the lumbar laminae interval space increases gradually from upper to lower[37], surgery through the interlaminar approach is suitable for L5/S1 intervertebral disc herniation. Nevertheless, a small laminae interval space is generally found in clinical practice, or the prolapse is at L3/4 or L4/5; therefore, the position of the channel is unsatisfactory, or the decompression area is relatively small. The diameter of the regular PTED endoscope is 7 mm, and the swinging ability within the channel is relatively poor; therefore, the exploration can be incomplete, and residual distal prolapsed vertebral pulp can be found.
The diameter of the iLESSYS Delta 6-mm working channel endoscope is 10 mm, which allows the use of apparatus with even larger diameters and endoscopic power to increase the working efficiency and visual field further. The swinging range of the endoscope is large, which favors the discrimination of endoscopic structures. Therefore, the iLESSYS Delta 6-mm working channel endoscope has innate advantages for the treatment of massively prolapsed intervertebral disc herniation. The assistant application of an endoscopic bur to thin the vertebral plate could help increase the laminae interval space, and therefore is especially useful for massively prolapsed intervertebral disc herniation with a relatively small laminae interval space, such as such diseases at L3/4, L4/5, and L5/S1. According to preoperative imaging data, the upper or lower vertebral plate is ground downward or upward until reaching the distal end of the prolapsed intervertebral disc. A bone ribbing rongeur is used to open the spinal canal, which could expose the protruding vertebral pulp below. The distal part of the vertebral pulp can be directly reached, and the risk of residual vertebral pulp is very low. Therefore, the operation time is greatly reduced. Intervertebral disc herniation can be at the axillary, shoulder, or both, of the nerve roots. The iLESSYS Delta 6-mm working channel endoscope can offer wide visual fields, which could expose the axilla and shoulder of the nerve root at the same time, and reduce the traction and oppression on the nerve root[38]. With the assistant application of an inner cannula, a breach of the annulus fibrosus can be further identified, and the spongy intervertebral disc tissues in the laminae interval space can be managed, which could further reduce the recurrence rate while ensuring safety. In the present study, the longest follow-up of a patient was 13 mo, and no recurrence was found. Due to the positions of the iLESSYS Delta channel, there are still debates on the treatment efficacy of this method on massively central intervertebral disc herniation[17-21]. Therefore, no such patients were included in this study. The resection of the ligamenta flava can directly expose the spinal dura, while any improper operations can increase the risk of the rupture of the spinal dura. There are still debates on the use of the iLESSYS Delta 6-mm working channel endoscope for the treatment of the cauda equina syndrome, and safety is still undefined.
In addition to the methods described in this study, several other methods have also been used for the endoscopic treatment of massively prolapsed intervertebral disc herniation. Kim et al[39] have reported treating high-grade prolapsed lumbar disc herniations with endoscopic transforaminal suprapedicular approach. Some other studies have also reported using two-channel approaches to treat such diseases[23,40]. Nevertheless, these methods still have several disadvantages, such as fixed channel positions, high skill requirements, and high risks of nerve damages.
This study had some limitations. This was a retrospective study of a small number of patients all treated by the same surgeons at the same hospital. The data were limited to those available from the medical charts. Additional studies, especially randomized controlled trials, are still necessary to determine the exact benefits of the iLESSYS Delta 6-mm working channel endoscope for a wide variety of patients.
As a minimal invasive spinal surgery system for the treatment of lumbar canal stenosis, the iLESSYS Delta 6-mm working channel endoscope has distinct advantages in treating patients with massively prolapsed intervertebral sic herniation in addition to special types of lumbar intervertebral disc herniations such as severe distal prolapsed lumbar disc herniations at L4/5, severe proximal prolapsed lumbar disc herniations at L5/S1, severe distal prolapsed lumbar disc herniations at L5/S1, and distal prolapsed lumbar disc herniations at L5/S1 with too small laminae interval space, as described in the literature[17-21]. Using this system could favor the complete removal of the sequestrated lumbar disc tissues, the surgical effectiveness is high, and the incidence of complications is low. Therefore, this technique has good application prospects.
Lumbar disk herniation is caused by protrusion, extrusion, or sequestration of the intervertebral disk from its usual anatomic location, and may be asymptomatic or result in radiculopathy or non-radicular pain. Conservative treatments are sufficient to manage the condition in most patients, but surgery is indicated in cases of cauda equine syndrome, severe and progressive neurologic deficits, and no improvement after conservative treatments.
Massively prolapsed lumbar intervertebral disc (IVD) herniation has an acute onset and with severe radicular pain and these symptoms or fear of dural compression and cauda equina syndrome can require surgery. Conventional fenestration, transforaminal lumbar interbody fusion (TLIF), and minimally invasive TLIF have definite treatment efficacies and decompression effects and therefore are often used. However, endoscopic discectomy through the interlaminar endoscopic spine system (iLESSYS) Delta 6-mm working channel endoscope, which has been widely applied in the treatment of lumbar spinal stenosis, is possible. But very few studies have used this method for the treatment of prolapsed intervertebral disc herniation.
This retrospective study explored the clinical benefits of treating massively prolapsed IVD herniation with the iLESSYS Delta endoscope.
The clinical data of 37 patients that underwent surgery with the iLESSYS Delta endoscope at The Affiliated Hospital of Qingdao University were retrospectively analyzed. Intraoperative blood loss, operation time, and complications were collected. The visual analog scale (VAS), oswestry disability index (ODI), and modified MacNab criteria were determined before and at 1 d, 3 mo and 6 mo after surgery.
The mean intraoperative blood loss for the 37 patients was 20.4 ± 1.2 mL. The mean operation time was 97.3 ± 12.4 min. The VAS scores for leg decreased from 68.0 ± 7.3 to 2.5 ± 1.7 and back pain decreased from 34.4 ± 8.5 to 5.5 ± 1.9 from the measurements before operation to 6 mo after surgery. The ODI also decreased from 60.2 ± 7.3 to 17.9 ± 3.4 at 6 mo after surgery. The improvement rate of the MacNab score was 86.4%, which was considered excellent. No spinal dural injury, nerve root injury, secondary protrusion of intervertebral disc, or myeloid hypertension was found during follow-up.
We demonstrated that the iLESSYS Delta 6-mm working channel endoscope has several advantages in terms of clinical and functional benefits, complications, and low risk of residual vertebral pulp in treating patients with massively prolapsed IVD herniation.
We consider that further randomized controlled trials are necessary to determine the exact benefits of the iLESSYS Delta 6-mm working channel endoscope for a wide variety of patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chiu KW S-Editor: Huang P L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Deyo RA, Mirza SK. CLINICAL PRACTICE. Herniated Lumbar Intervertebral Disk. N Engl J Med. 2016;374:1763-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 222] [Article Influence: 24.7] [Reference Citation Analysis (1)] |
| 2. | Van Boxem K, Cheng J, Patijn J, van Kleef M, Lataster A, Mekhail N, Van Zundert J. 11. Lumbosacral radicular pain. Pain Pract. 2010;10:339-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 3. | Mattila VM, Sillanpää P, Visuri T, Pihlajamäki H. Incidence and trends of low back pain hospitalisation during military service--an analysis of 387,070 Finnish young males. BMC Musculoskelet Disord. 2009;10:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Gregory DS, Seto CK, Wortley GC, Shugart CM. Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician. 2008;78:835-842. [PubMed] |
| 5. | Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007;25:387-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 200] [Article Influence: 11.1] [Reference Citation Analysis (1)] |
| 6. | Jeon CH, Chung NS, Son KH, Lee HS. Massive lumbar disc herniation with complete dural sac stenosis. Indian J Orthop. 2013;47:244-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007;89:782-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Postacchini F. Management of herniation of the lumbar disc. J Bone Joint Surg Br. 1999;81:567-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Shapiro S. Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery. 1993;32:743-746; discussion 746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 113] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976). 2000;25:1515-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 249] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Louison R, Barber JB. Massive herniation of lumbar discs with compression of the cauda equina--a surgical emergency; report of two cases. J Natl Med Assoc. 1968;60:188-190. [PubMed] |
| 13. | Postacchini F. Results of surgery compared with conservative management for lumbar disc herniations. Spine (Phila Pa 1976). 1996;21:1383-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Satoh I, Yonenobu K, Hosono N, Ohwada T, Fuji T, Yoshikawa H. Indication of posterior lumbar interbody fusion for lumbar disc herniation. J Spinal Disord Tech. 2006;19:104-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Kim M, Kim HS, Oh SW, Adsul NM, Singh R, Kashlan ON, Noh JH, Jang IT, Oh SH. Evolution of Spinal Endoscopic Surgery. Neurospine. 2019;16:6-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 99] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 16. | Kim JH, Kim HS, Kapoor A, Adsul N, Kim KJ, Choi SH, Jang JS, Jang IT, Oh SH. Feasibility of Full Endoscopic Spine Surgery in Patients Over the Age of 70 Years With Degenerative Lumbar Spine Disease. Neurospine. 2018;15:131-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Middleton SD, Wagner R, Gibson JNA. Multi-level spine endoscopy: A review of available evidence and case report. EFORT Open Rev. 2017;2:317-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Lee CH, Choi M, Ryu DS, Choi I, Kim CH, Kim HS, Sohn MJ. Efficacy and Safety of Full-endoscopic Decompression via Interlaminar Approach for Central or Lateral Recess Spinal Stenosis of the Lumbar Spine: A Meta-analysis. Spine (Phila Pa 1976). 2018;43:1756-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 19. | Wagner R, Telfeian AE, Krzok G, Iprenburg M. Fully-endoscopic lumbar laminectomy for central and lateral recess stenosis: Technical note. Interdisciplinary Neurosurg. 2018;13:6-9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Kim HS, Paudel B, Jang JS, Oh SH, Lee S, Park JE, Jang IT. Percutaneous Full Endoscopic Bilateral Lumbar Decompression of Spinal Stenosis Through Uniportal-Contralateral Approach: Techniques and Preliminary Results. World Neurosurg. 2017;103:201-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 100] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 21. | Shen J. Fully Endoscopic Lumbar Laminectomy for Treatment of Large Dorsal Ligamentum Flavum Cyst and Severe Spinal Stenosis: A Technical note on a Case Report. J Spine. 2018;S7:11. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | U ECY, Shetty A, Craig PRS, Chitgopkar SD. An observation of massive lumbar disc prolapse. J Spine Surg. 2018;4:583-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Hu QF, Pan H, Fang YY, Jia GY. Percutaneous endoscopic lumbar discectomy for high-grade down-migrated disc using a trans-facet process and pedicle-complex approach: a technical case series. Eur Spine J. 2018;27:393-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Ammar A, Zarnegar R, Yassari R, Kinon M. Large central lumbar disc herniation causing acute cauda equina syndrome with loss of evoked potentials during prone positioning for surgery. Surg Neurol Int. 2018;9:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Tan JH, Liu G, Ng R, Kumar N, Wong HK, Liu G. Is MIS-TLIF superior to open TLIF in obese patients? Eur Spine J. 2018;27:1877-1886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 26. | Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019;14:229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 27. | Buccholz AL, Quinn JC, Buell TJ, Yen CP, Haid RW, Shaffrey CI, Smith JS. TLIF - A Review of Techniques and Advances. Contemp Neurosurg. 2019;41:1-8. |
| 28. | Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 134] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 29. | Wu XD, Chen Y, Yu WC, Liu Y, Cao P, Tian Y, Wang XW, Chen HJ, Ye XJ, Yuan W, Yeung A. Effectiveness of Bi-Needle Technique (Hybrid Yeung Endoscopic Spine System/Transforaminal Endoscopic Spine System) for Percutaneous Endoscopic Lumbar Discectomy. World Neurosurg. 2018;119:e53-e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Chen Z, Zhang L, Dong J, Xie P, Liu B, Wang Q, Chen R, Feng F, Yang B, Shu T, Li S, Yang Y, He L, Pang M, Rong L. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine. 2018;28:300-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 31. | Ba Z, Li Z, Liu Z, Li H, Wu D, Zhu J. Eccentric technique for foraminoplasty in percutaneous endoscopic transforaminal procedure: A technical note. Int J Surg. 2017;46:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58:ONS59-68; discussion ONS59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, Shin SW, Kang HY. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 cases. Spine (Phila Pa 1976). 2006;31:E285-E290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Sun B, Shi C, Xu Z, Wu H, Zhang Y, Chen Y, Wu XD, Yuan W. Learning Curve for Percutaneous Endoscopic Lumbar Diskectomy in Bi-needle Technique Using Cumulative Summation Test for Learning Curve. World Neurosurg. 2019;129:e586-e593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 35. | Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976). 2013;38:617-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 123] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 36. | Kong W, Liao W, Ao J, Cao G, Qin J, Cai Y. The Strategy and Early Clinical Outcome of Percutaneous Full-Endoscopic Interlaminar or Extraforaminal Approach for Treatment of Lumbar Disc Herniation. Biomed Res Int. 2016;2016:4702946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Ebraheim NA, Miller RM, Xu R, Yeasting RA. The location of the intervertebral lumbar disc on the posterior aspect of the spine. Surg Neurol. 1997;48:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Liu C, Chu L, Yong HC, Chen L, Deng ZL. Percutaneous Endoscopic Lumbar Discectomy for Highly Migrated Lumbar Disc Herniation. Pain Physician. 2017;20:E75-E84. [PubMed] |
| 39. | Kim HS, Ju CI, Kim SW, Kim JG. Endoscopic transforaminal suprapedicular approach in high grade inferior migrated lumbar disc herniation. J Korean Neurosurg Soc. 2009;45:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 40. | Wu X, Fan G, Gu X, Guan X, He S. Surgical Outcome of Two-Level Transforaminal Percutaneous Endoscopic Lumbar Discectomy for Far-Migrated Disc Herniation. Biomed Res Int. 2016;2016:4924013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |