Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.284
Peer-review started: October 9, 2020
First decision: November 20, 2020
Revised: November 21, 2020
Accepted: December 6, 2020
Article in press: December 6, 2020
Published online: January 6, 2021
Processing time: 84 Days and 10.2 Hours
Acromial and scapular spine fractures after reverse total shoulder arthroplasty (RTSA) are a well-known complication that may negatively impact the effects of long-term outcomes. However, to the best of our knowledge, there has been no report of simultaneous bilateral fractures of the acromion or scapular spine that occurred following staged RTSA.
A 79-year-old right-handed male visited our outpatient clinic with a chief complaint of pain and limited motion of both shoulder joints for a one-year duration. Based on plain radiographs and magnetic resonance images, the preoperative diagnosis was bilateral cuff tear arthropathy with failed rotator cuff repair. This patient was treated with staged bilateral RTSA at a two-month interval. At 5 and 3 mo after right and left side surgery, the patient returned to the outpatient clinic with severe pain and limited motion of both shoulder joints for 2 wk without a traumatic event. A computed tomography scan revealed non-displaced acromial base fractures of both shoulders. Considering bilateral involvement, fracture location, and patient’s demand, open reduction and internal fixation (ORIF) using plate for bilateral acromial base fractures were performed. At 2 years after ORIF, the fracture was completely healed, and the patient was satisfied with shoulder status.
This report describes an extremely rare case of simultaneous bilateral acromial base fractures after staged RTSA managed successfully by ORIF with a pre-contoured plate designed for distal clavicle fractures. Although acromial fracture after RTSA can be treated conservatively, simultaneous bilateral fractures may warrant surgical intervention as a means of addressing difficulties in activities of daily living.
Core Tip: Acromial and scapular spine fractures are a well-known complication that can occur by deltoid tension with increased arm length after reverse total shoulder arthroplasty (RTSA). The reported incidences range from 0.6% to 15.8%. However, simultaneous bilateral fractures of the acromion or scapular spine following staged RTSA are extremely rare. Furthermore, its management has not been established. Although acromial fracture after RTSA can be treated conservatively, simultaneous bilateral fractures may warrant surgical intervention as a means of addressing difficulties in activities of daily livings.
- Citation: Kim DH, Kim BS, Cho CH. Simultaneous bilateral acromial base fractures after staged reverse total shoulder arthroplasty: A case report. World J Clin Cases 2021; 9(1): 284-290
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/284.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.284
Bilateral reverse total shoulder arthroplasty (RTSA) is a proven treatment option for in cuff tear arthropathy (CTA), requiring bilateral arthroplasty[1-3]. Acromial and scapular spine fractures after RTSA are a well-known complication that may negatively impact long-term outcomes[4-6]. In patients undergoing bilateral RTSA, bilateral fractures of the acromion or scapular spine are very rare. In fact, a review of the literature reveals that only 2 cases with sequential bilateral fractures of the acromion or scapular spine have been reported[7,8]. However, to the best of our knowledge, there has been no report of simultaneous bilateral fractures of the acromion or scapular spine following staged RTSA. Furthermore, its management has not been established.
This report describes an extremely rare case of simultaneous bilateral acromial base fractures after staged RTSA managed successfully by open reduction and internal fixation (ORIF) with a pre-contoured plate designed for distal clavicle fractures.
A 79-year-old right-handed male visited our outpatient clinic with severe pain and limited range of motion (ROM) of both shoulder joints.
The patient’s symptoms started 2 wk ago without a traumatic event.
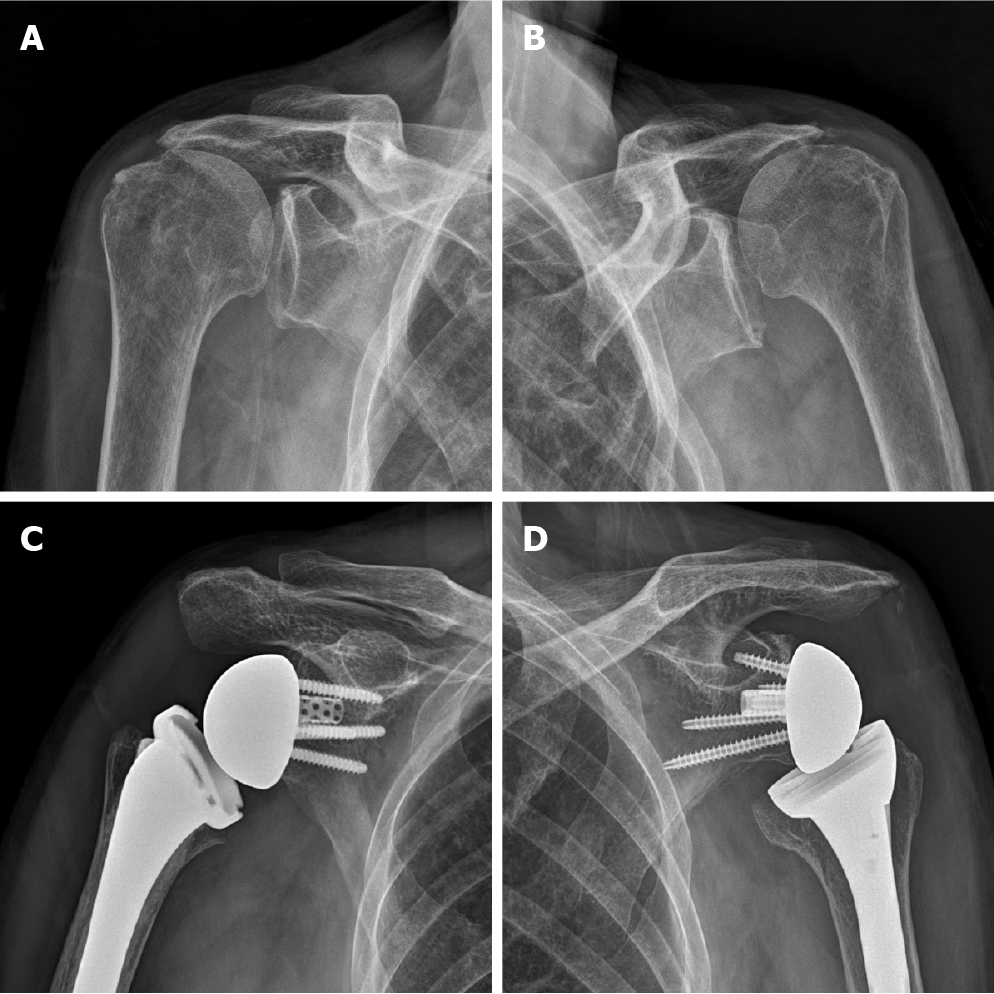
Six years ago, this patient underwent bilateral repair for a massive rotator cuff tear at a one-year interval in a local clinic. The patient visited our hospital complaining of worsening both shoulder pain 6 mo ago; an active ROM of the right shoulder was 20° of forward flexion, 30° of abduction, 45° of external rotation, and the 4th lumbar vertebra level of internal rotation on physical examination. Active ROM of the left shoulder was 20° of forward flexion, 20° of abduction, 60° of external rotation, and the 4th lumbar vertebra level of internal rotation. Based on plain radiographs and magnetic resonance images, the preoperative diagnosis was bilateral CTA with failed rotator cuff repair. No preoperative acromial pathology was observed. This patient was treated with staged bilateral RTSA [right shoulder: Equinoxe (Exactech, Gainesville, FL, United States), left shoulder: Delta Xtend (DePuy, Warsaw, IN, United States)] at a two-month interval (Figure 1).
The patient reported being satisfied with significant pain relief and functional restoration after RTSA. At 3 mo after right RTSA, active ROM increased to 140° of forward flexion, 100° of abduction, 50° of external rotation, and the 5th lumbar vertebra level of internal rotation. At 6 wk after left RTSA, active ROM increased to 100° of forward flexion, 80° of abduction, 50° of external rotation, and the 5th lumbar vertebra level of internal rotation.
The patient underwent RTSA on the right shoulder 5 mo ago and left shoulder 3 mo ago.
Physical examination revealed tenderness on the posterolateral area of both shoulders without soft tissue swelling or redness. Active ROM was not able to be assessed due to severe pain. Visual Analogue Scale for pain, American Shoulder and Elbow Surgeons score, and Subjective Shoulder Value of both shoulders were 8%, 15%, and 15%, respectively.
The results of preoperative laboratory tests were normal.
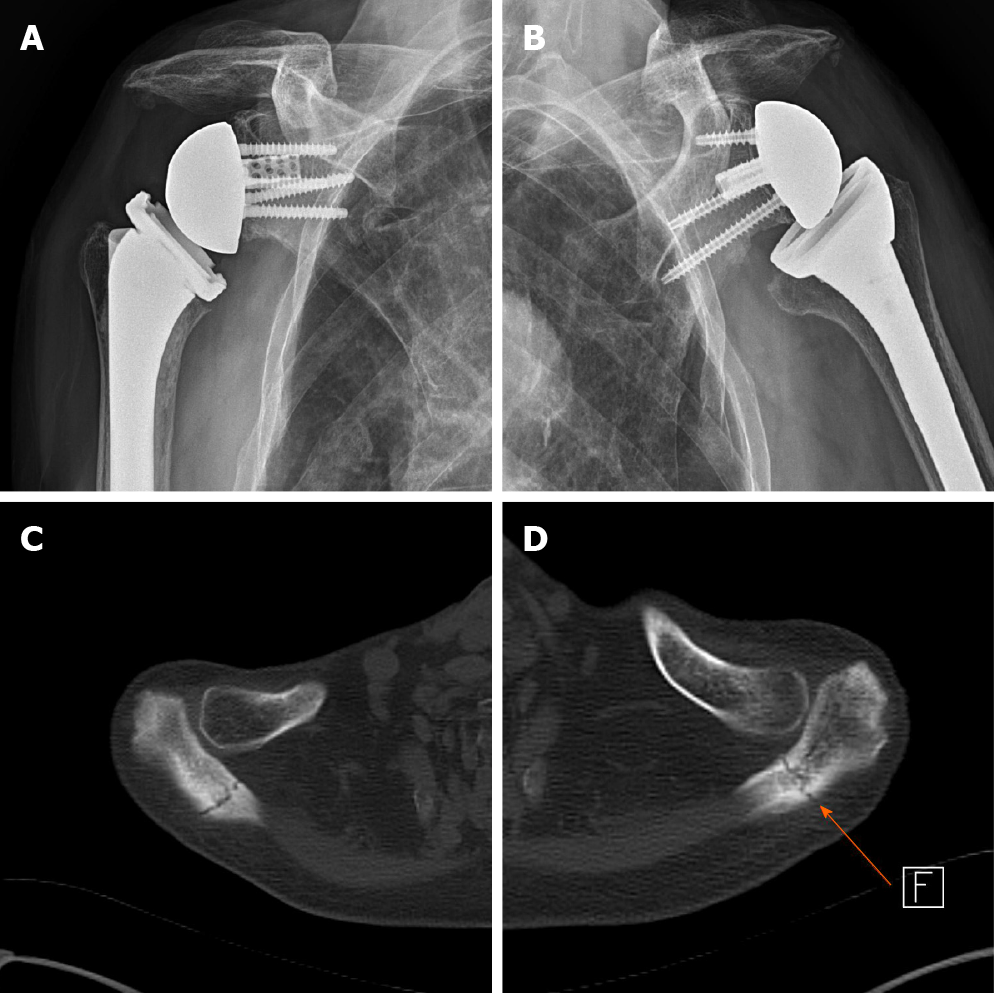
Plain radiographs revealed no definite fractures or bony abnormalities compared to previous plain radiographs. Computed tomography (CT) scan revealed non-displaced acromial base fractures of both shoulders (Figure 2). The t score of bone mineral density for lumbar spine was -2.9.
The final diagnosis of the presented case was bilateral acromial base fractures after staged RTSA.
Despite immobilization and opioid medication, the patient complained of significant difficulties with activities of daily living (ADL) without pain relief. Considering bilateral involvement, fracture location, and importance of performing ADLs, and patient’s demand, ORIF for bilateral acromial base fractures was selected.
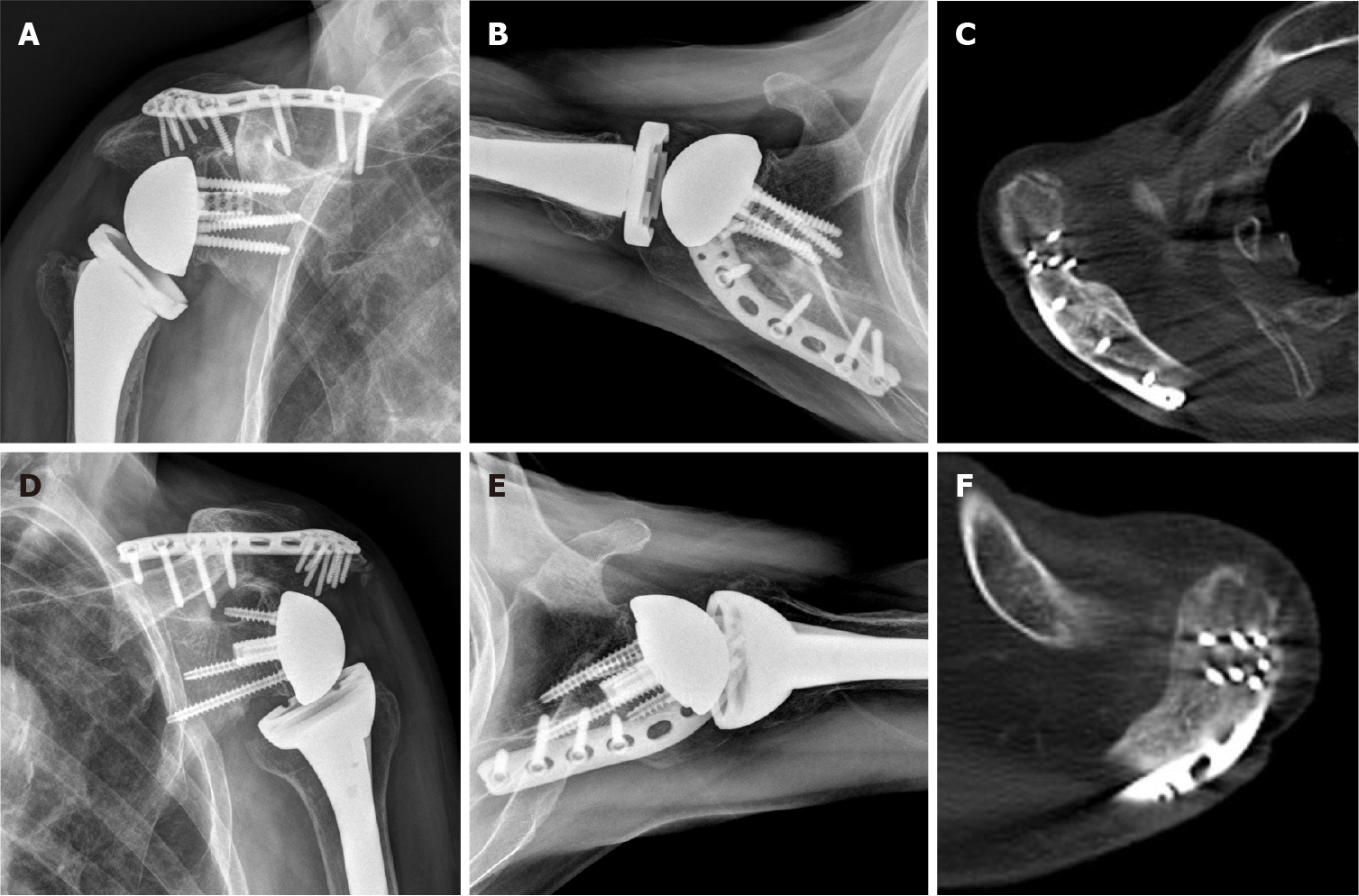
After general anesthesia, the patient was placed in the beach chair position. Skin incision was made along the lateral margin of the acromion and scapular spine. After a fasciocutaneous flap was raised medially along the incision line, the fracture site was exposed. A pre-contoured plate (Acumed, Hillsboro, OR, United States) designed for distal clavicle fractures was bent along the acromial bony contour. After temporary Kirschner-wires fixation of the fracture site, plate fixation was completed (Figure 3). Postoperatively, both shoulders were immobilized with an arm sling. Active and passive ROM exercises commenced 3 d after surgery.
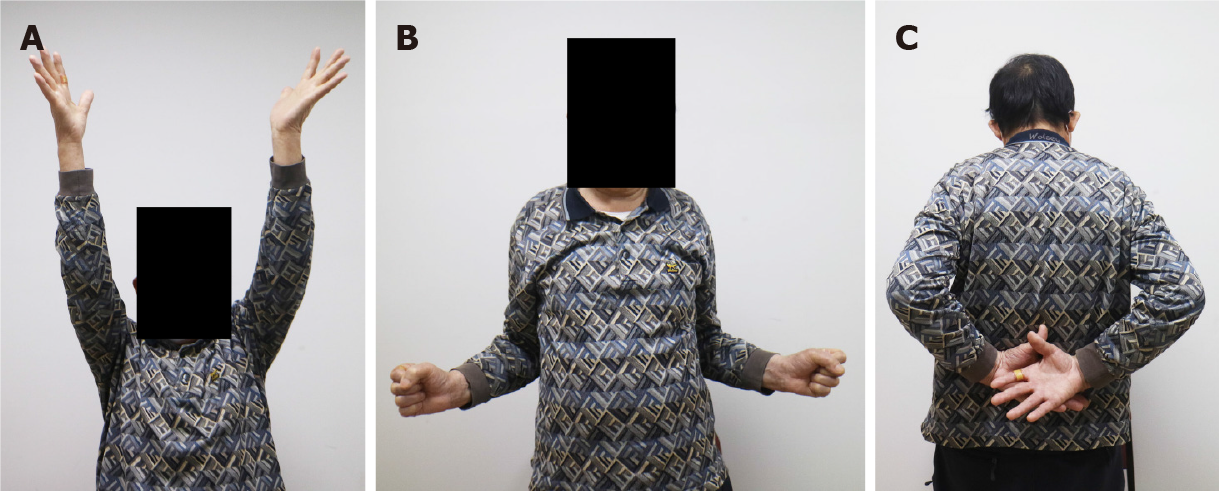
At 2 years after ORIF, the fracture was completely healed, and the patient was satisfied with shoulder status. The patient was capable of 140° of forward flexion, 120° of abduction, 50° of external rotation, and the 3rd lumbar vertebra level of internal rotation for both shoulders (Figure 4). Visual Analogue Scale for pain, American Shoulder and Elbow Surgeons score, and Subjective Shoulder Value of both shoulders were 3%, 75%, and 70%, respectively.
RTSA has been shown to have efficacy for the treatment of debilitating shoulder diseases with rotator cuff deficiency[4,9]. As the indications for RTSA have expanded, there has been a dramatic growth in the frequency of RTSA worldwide over the past decade[3,10]. In the past, bilateral RTSA was considered inadvisable because patients may struggle with ADLs following treatment[2]. Recently, with the advance of implant design, bilateral RTSA has proven to be a successful option for the treatment of bilateral CTA[1,2]. Levy et al[1] reported that bilateral RTSA results in marked and predictable improvement in all movements, pain relief, and functional outcomes (e.g., ADLs, hygiene, leisure activities).
Acromial and scapular spine fractures are a well-known complication that can occur by deltoid tension with increased arm length after RTSA. The reported incidences range from 0.6% to 15.8%[4,6]. Patients with acromial or scapular spine fracture have inferior clinical outcomes and may be at increased risk for revision surgery compared to patients without acromial or scapular spine fracture[5,7,8]. This complication may lead to functional deterioration at long-term follow-up. Nonetheless, there is no consensus as to the appropriate treatment.
Levy et al[1] reported that two out of 19 patients treated with bilateral RTSA staged at an average interval of 18-mo had a traumatic scapular spine fracture after a fall. One had moderate recovery after ORIF for scapular spine fracture occurred 2 mo postoperatively (final Constant score, 40.6). The second had a scapular spine fracture that occurred 8 years postoperatively and declined any further surgery because of comorbidities (final Constant score, 24.0). Mellano et al[2] reported that 10% of patients (5/50) with bilateral RTSA staged at an average interval of 15-mo experienced acromial fractures.
A literature review revealed that 2 cases with sequential bilateral fractures of the acromion or scapular spine in patients underwent bilateral RTSA have been reported[7,8]. Nicolay et al[7] reported an 89-year-old woman with bilateral atraumatic scapular spine fracture after bilateral RTSA staged at an interval of 16-mo. At 1 mo after right RTSA (second surgery), the patient experienced a left scapular spine fracture 17 mo after left RTSA (initial surgery). Four months later, a similar scapular spine fracture was detected in the right shoulder. Considering patient’s age, conservative treatment was chosen and her shoulder function was never completely regained in both shoulders, with the patient struggling to maintain ADLs[7]. Stevens et al[8] reported a 63-year-old woman with bilateral acromial base fractures after bilateral RTSA staged at an interval of 27-mo. The patient had right acromial base fracture at 10.5 mo after right RTSA (initial surgery). Left acromial base fracture was detected at 3.5 years after left RTSA (second surgery). Because her right shoulder had poor clinical outcome after conservative treatment, ORIF for left fracture was strongly recommended. However, this patient declined ORIF and had poor shoulder function at final follow-up.
In the present study, the patient experienced simultaneous bilateral acromial base fractures at 5 and 3 mo after right and left RTSA, respectively. Considering bilateral involvement, fracture location, and patient’s demand for ADLs (e.g., perineal care, hygiene), ORIF was performed in spite of non-displaced fractures. During ORIF, a lateral clavicle pre-contoured plate bent along bony contour of the acromion was used. This is an advantage of applying many locking screws with different screw direction on acromion compared to other plates. Finally, the patient had satisfactory clinical and radiological outcomes at 2 years after ORIF.
To the best of our knowledge, this is the first report of simultaneous bilateral acromial base fractures after staged RTSA managed successfully by ORIF using a pre-contoured plate designed for distal clavicle fractures. Although acromial fracture after RTSA can be treated conservatively, simultaneous bilateral fractures may warrant surgical intervention as a means of addressing difficulties in ALDs. Further studies are needed to determine whether ORIF for acromial or scapular spine fractures is a reasonable option in patients treated with bilateral RTSA.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu F S-Editor: Huang P L-Editor: A P-Editor: Wu YXJ
| 1. | Levy O, Walecka J, Arealis G, Tsvieli O, Della Rotonda G, Abraham R, Polyzois I, Jurkowski Z, Atoun E. Bilateral reverse total shoulder arthroplasty-functional outcome and activities of daily living. J Shoulder Elbow Surg. 2017;26:e85-e96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Mellano CR, Kupfer N, Thorsness R, Chalmers PN, Feldheim TF, O'Donnell P, Cole BJ, Verma NN, Romeo AA, Nicholson GP. Functional results of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:990-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Walters JD, Denard PJ, Brockmeier SF, Werner BC. The relationship of bilateral shoulder arthroplasty timing and postoperative complications. J Shoulder Elbow Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Cho CH, Jung JW, Na SS, Bae KC, Lee KJ, Kim DH. Is Acromial Fracture after Reverse Total Shoulder Arthroplasty a Negligible Complication? Clin Orthop Surg. 2019;11:427-435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Hess F, Zettl R, Smolen D, Knoth C. Anatomical reconstruction to treat acromion fractures following reverse shoulder arthroplasty. Int Orthop. 2018;42:875-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Patterson DC, Chi D, Parsons BO, Cagle PJ Jr. Acromial spine fracture after reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019;28:792-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 7. | Nicolay S, De Beuckeleer L, Stoffelen D, Vanhoenacker F, Pouillon M. Atraumatic bilateral scapular spine fracture several months after bilateral reverse total shoulder arthroplasty. Skeletal Radiol. 2014;43:699-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Stevens CG, Murphy MR, Stevens TD, Bryant TL, Wright TW. Bilateral scapular fractures after reverse shoulder arthroplasties. J Shoulder Elbow Surg. 2015;24:e50-e55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Jeong JY, Cha HE. Reverse Total Shoulder Arthroplasty in the Massive Rotator Cuff Tear. Clin Shoulder Elbow. 2014;17:145-150. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Sperling JW. Pearls and Tips in Shoulder Arthroplasty. Clin Orthop Surg. 2019;11:258-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |