Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.274
Peer-review started: October 12, 2020
First decision: October 27, 2020
Revised: November 2, 2020
Accepted: November 13, 2020
Article in press: November 13, 2020
Published online: January 6, 2021
Processing time: 81 Days and 3 Hours
This study reports the clinical presentation of intraparenchymal hemorrhage as a rare complication after surgical decompression of an intracranial epencephalon arachnoid cyst (IEAC) at the posterior cranial fossa.
The clinical information of a patient with an IEAC was reported, and the related literature was reviewed. A female patient with nausea presented to our hospital. Computed tomography demonstrated an IEAC located at the posterior cranial fossa, which was large and required surgical intervention. After operation, postoperative intraparenchymal hemorrhage was detected. She had a good recovery with conservative treatment 1 mo later.
Though postoperative intraparenchymal hemorrhage is rare after surgical decompression of an IEAC, more attention should be paid to such a complication.
Core Tip: Although intracranial epencephalon arachnoid cysts (IEACs) are rare, patients may become symptomatic due to cyst enlargement. In these patients, surgical intervention is required. I here report a case of intraparenchymal hemorrhage as a rare complication after the surgical decompression of an IEAC. This case indicated that patient’s condition should be carefully reviewed after operation in case of fatal complications.
- Citation: Wang XJ. Intraparenchymal hemorrhage after surgical decompression of an epencephalon arachnoid cyst: A case report. World J Clin Cases 2021; 9(1): 274-277
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/274.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.274
Intracranial epencephalon arachnoid cysts (IEACs) represent a relatively rare disease, accounting for less than 1% of all brain mass lesions[1]. IEACs are usually benign collections of cerebrospinal fluid (CSF), partly accompanied by a placeholder effect. Most patients with IEACs are asymptomatic and found incidentally. However, some of them may become symptomatic due to cyst enlargement. I here report a case of intraparenchymal hemorrhage as a rare complication after surgical decompression of an IEAC.
A previously healthy female (28 years old, right-handed) was admitted to our hospital with intractable nausea.
Medical treatment for nausea failed.
This patient had no history of past illness.
This patient had no other previous medical history.
No neurological deficit or papilledema was observed in her neurological examination.
Laboratory tests were in the normal range.
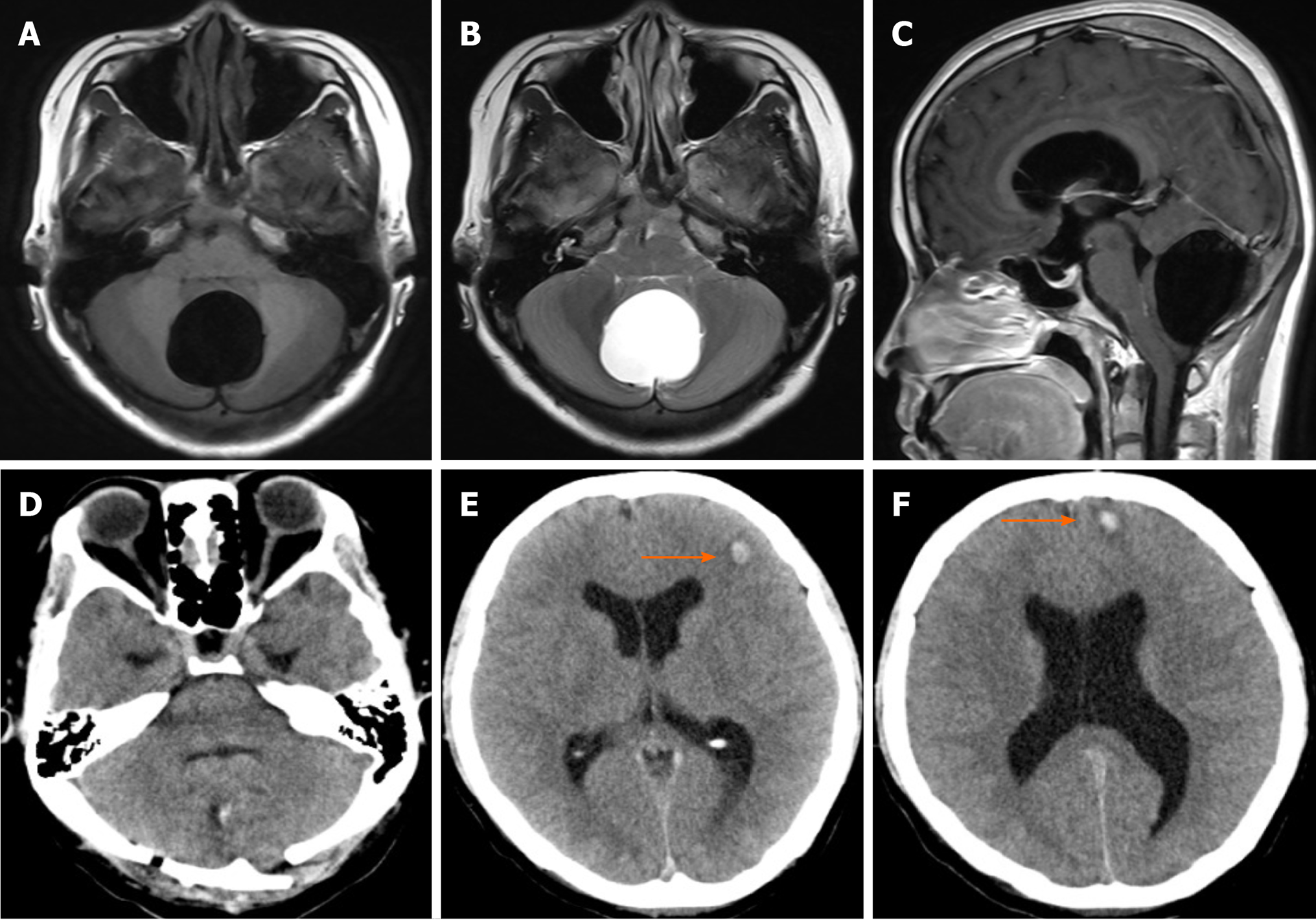
In her brain magnetic resonance imaging scan, a large fluid collection could be found at the posterior cranial fossa with a size of 6 cm × 7 cm (Figure 1A-C).
A large IEAC.
Considering the mass effect and intractable nausea, the patient was admitted to the hospital for surgical decompression. During the operation, after occipital craniotomy, cerebellum dura was opened, and the wall of the cyst was resected and fully separated. Indirect surgical approaches with conservative procedures were used to gradually decompress this arachnoid cyst. Arachnoid cyst was opened and decompressed to the cisterna magna to avoid recurrence.
From the postoperative routine review of computed tomography (CT), a good decompression was achieved (Figure 1D), while two focuses of intraparenchymal hemorrhage were found in the frontal lobe (Figure 1E and F). She had slight vomiting and headache. The neurological examination was normal. She achieved an excellent recovery 1 mo later with conservative treatment.
IEACs are collections of intro-arachnoidal CSF, which account for less than 1% of all non-traumatic brain mass lesions and are often asymptomatic[1,2]. Nevertheless, the patients can be symptomatic due to cyst enlargement. Early diagnosis is critical as cysts cause the mass effect, which may require surgical intervention. The therapeutic schemes of IEACs remain controversial because of their variable manifestation patterns. Therapeutic options for larger cysts include CSF shunting, endoscopic fenestration, or craniotomy and open fenestration[3].
IEACs are frequently found in the middle cranial fossa in 50% of cases, with a slight predilection for the left side and the male gender[1]. Symptoms include headache, behavioral problems, ataxia, cerebellar signs, nausea, vomiting, visual disturbance, and seizures. De et al[4,5] have reported that the most common symptom is a headache, followed by behavioral problems. For example, a change in personality and impaired mental function are the second most frequently reported symptoms and sometimes may be the only presenting features. Its origin remains unknown. The diagnosis is always apparent in CT. The most effective treatment for IEACs is surgical decompression of the cyst[6,7]. In clinical practice, if there is a space-occupying lesion or apparent clinical symptoms, it is considered that there is an operative indicator.
There are several complications after the surgical decompression of arachnoid cysts, including recurrence, hydrocephalus, subdural hematomas, cerebral edema, infection, and seizures[3,8-10]. However, intraparenchymal hemorrhage in the brain parenchyma is a rare complication after the decompression of IEACs[11,12]. Few studies have reported the hemorrhage after surgical decompression of IEACs[11-13]. To the best of our knowledge, the first description of intraparenchymal hemorrhage after surgical decompression of IEACs was reported by Borges et al[14] in 1995. They reported a case of brainstem hemorrhage after surgical removal of IEAC of the lateral fissure[14]. Until now, the pathogenesis of such complication remains largely unexplored, which may be attributed to reperfusion injury[11]. It is well known that intracerebral hemorrhage may occur after rapid decompression of chronic subdural hematomas, and hypoperfusion of brain parenchyma after surgical decompression for cerebral tumor has also been reported[11,15,16]. It is believed that hemorrhage could be mainly attributed to the rapid decompression of the cyst, although the risk of rapid decompression was considered, and a gradual decompression of IEAC, in this case, was given to avoid rapid decompression and decrease the incidence of such rare complications.
Collectively, hemorrhage in a postoperative arachnoid cyst is a rare complication. However, it is critical to establish a timely and accurate diagnosis after a routine postoperative CT scan. Symptoms and signs are usually non-specific, and the diagnosis relies on a precise history, imageological examination, and careful observations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Strainiene S S-Editor: Chen XF L-Editor: MedE-Ma JY P-Editor: Wang LL
| 1. | Parsch CS, Krauss J, Hofmann E, Meixensberger J, Roosen K. Arachnoid cysts associated with subdural hematomas and hygromas: analysis of 16 cases, long-term follow-up, and review of the literature. Neurosurgery. 1997;40:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 70] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | de Longpre J. Large Arachnoid Cyst. N Engl J Med. 2017;376:2265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Auschwitz T, DeCuypere M, Khan N, Einhaus S. Hemorrhagic infarction following open fenestration of a large intracranial arachnoid cyst in a pediatric patient. J Neurosurg Pediatr. 2015;15:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | De K, Berry K, Denniston S. Haemorrhage into an arachnoid cyst: a serious complication of minor head trauma. Emerg Med J. 2002;19:365-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Igarashi Y, Murai Y, Yamada O, Shirokane K, Hironaka K, Sato S, Sugiyama M, Tachizawa T, Morita A. Cerebral Aneurysm Associated with an Arachnoid Cyst: 3 Case Reports and a Systematic Review of the Literature. World Neurosurg. 2018;109:e203-e209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Sener RN. Arachnoid cysts associated with post-traumatic and spontaneous rupture into the subdural space. Comput Med Imaging Graph. 1997;21:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Clifton W, Rahmathulla G, Tavanaiepour K, Alcindor D, Jakubek G, Tavanaiepour D. Surgically Treated de Novo Cervicomedullary Arachnoid Cyst in Symptomatic Adult Patient. World Neurosurg. 2018;116:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Shettar M, Karkal R, Misra R, Kakunje A, Mohan Chandran VV, Mendonsa RD. Arachnoid Cyst Causing Depression and Neuropsychiatric Symptoms: a Case Report. East Asian Arch Psychiatry. 2018;28:64-67. [PubMed] |
| 9. | Corona-Ruiz JM, De Jesus O. Enlarging Temporal Arachnoid Cyst Extending Inside the Sphenoid Sinus. World Neurosurg. 2018;115:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Hanrahan J, Frantzias J, Lavrador JP, Bodi I, Zebian B. Posterior fossa arachnoid cyst causing torticollis and gastro-oesophageal reflux in an infant. Childs Nerv Syst. 2018;34:2519-2523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Esmaeeli B, Eftekhar B. Intraparenchymal hemorrhage after surgical decompression of a Sylvian fissure arachnoid cyst. Neurol India. 2006;54:320-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Mori H, Terabayashi T, Kitazawa T, Sugiyama Y. [Multiple intracerebral hemorrhages immediately after surgical excision of middle fossa arachnoid cysts and evacuation of chronic subdural hygroma. Case report]. Neurol Med Chir. 29:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Ramachandran GM, Nair RP, Kongwad LI, Shanthakumar G. Rapid Brain Shift with Remote-Site Haemorrhage after Arachnoid Cyst Excision: Treatment Dilemmas. Pediatr Neurosurg. 2017;52:98-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Borges G, Fernandes YB, Gallani NR. [Brainstem hemorrhage after surgical removal of arachnoid cyst of the Sylvian fissure: a case report]. Arq Neuropsiquiatr. 1995;53:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Modesti LM, Hodge CJ, Barnwell ML. Intracerebral hematoma after evacuation of chronic extracerebral fluid collections. Neurosurgery. 1982;10:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Ovül I, Oner K. Intracerebral hematoma after evacuation of chronic subdural hematoma. Neurochirurgia. 31:160-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |