Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.245
Peer-review started: August 24, 2020
First decision: September 23, 2020
Revised: October 7, 2020
Accepted: November 2, 2020
Article in press: November 2, 2020
Published online: January 6, 2021
Processing time: 130 Days and 9.5 Hours
Appendectomy is the procedure of choice for the treatment of acute appendicitis. However, surgery may not be appropriate for patients with coexisting severe illness or comorbidities such as acute pancreatitis (AP). Endoscopic retrograde appendicitis treatment (ERAT) may be a novel alternative to surgery for treating such patients where existing medical therapies have failed.
We report 2 cases of moderately severe AP who developed acute uncomplicated appendicitis during their hospital stay and did not respond to traditional medical therapy. One patient had moderately severe AP due to hyperlipidemia, while the other patient had a gallstone induced by moderately severe AP. Neither patient was fit to undergo an appendectomy procedure because of the concurrent AP. Therefore, the alternative and minimally invasive ERAT was considered. After written informed consent was collected from the patients, the ERAT procedure was performed. Both patients exhibited fast postoperative recovery after ERAT with minimal surgical trauma.
ERAT is a safe and effective minimally invasive endoscopic procedure for acute appendicitis in patients with coexistent AP.
Core Tip: Endoscopic retrograde appendicitis treatment (ERAT) is a minimally invasive technique for the treatment of acute appendicitis. We performed ERAT in 2 patients with moderately severe acute appendicitis with uncomplicated acute pancreatitis after the failure of traditional medical therapy. Both patients exhibited fast recovery without the need to perform an appendectomy procedure and retained the potential physi-ological function of the appendix. There were no postprocedure complications. We believe that ERAT can be a suitable alternative to appendectomy in high-risk patients of acute appendicitis with coexisting severe illnesses.
- Citation: Du ZQ, Ding WJ, Wang F, Zhou XR, Chen TM. Endoscopic treatment for acute appendicitis with coexistent acute pancreatitis: Two case reports. World J Clin Cases 2021; 9(1): 245-251
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/245.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.245
Acute pancreatitis (severe acute pancreatitis) (AP) is mainly caused by biliary diseases and alcoholism. The incidence of AP is increasing[1], and severe AP is associated with multiorgan dysfunction including cardiorespiratory failure, resulting in a higher rate of mortality[2]. The treatment of choice for acute appendicitis is laparoscopic or open appendectomy[3], however, endoscopic retrograde appendicitis therapy (ERAT) is an emerging technique for the treatment of acute appendicitis. Inspired by endoscopic retrograde cholangiopancreatography for acute suppurative cholangitis, Liu et al[4] proposed the feasibility of endoscopic treatment of acute appendicitis in 2012 and subsequently conducted a multicenter study in China[5]. ERAT is a minimally invasive procedure that can be performed in uncomplicated cases of acute appendicitis. We report 2 cases of moderately severe AP where the patients also developed acute uncomplicated appendicitis and did not respond to medical therapy during the hospital stay. However, both laparoscopic and open appendectomies require anesthesia, which is associated with its own morbidity and risk of mortality in critically ill patients. Therefore, the 2 patients were treated by ERAT with minimal surgical trauma and fast postoperative recovery. Both patients were successfully treated.
Case 1: A 28-year-old male presented with abdominal pain and dyspnea for 1 d.
Case 2: A 44-year-old female presented with abdominal pain for more than 2 d with worsening nausea and vomiting for 4 h.
Case 1: The patient developed severe persistent pain in the upper abdomen for 1 d. He also had difficulty breathing, which was progressive in nature.
Case 2: The patient experienced intermittent colicky pain in the upper abdomen for more than 2 d with gradually worsening intensity. Abdominal pain was associated with nausea and vomiting.
Case 1: He had previous history of hyperlipidemia.
Case 2: No significant past history or any illness or surgery.
Case 1: On admission, the patient was afebrile, had tachycardia and tachypnea. An abdominal examination revealed epigastric tenderness.
Case 2: Clinical examination revealed epigastric tenderness.
Case 1: Laboratory test results upon admission were as follows: White blood cell count 18.14 × 109/L (3.5-9.5 × 109/L); hematocrit 50% (40%-50%); C-reactive protein 180 mg/L (0-8 mg/L); serum amylase 676 U/L (25-125 U/L); serum lipase 258 U/L (20-180 U/L); serum calcium 1.98 mmol/L (2.25-2.75 mmol/L); alanine aminotransferase 212 U/L (0-40 U/L); aspartate aminotransferase 74 U/L (0-40 U/L); and serum triglycerides 25.3 mmol/L (0.56-1.7 mmol/L). Arterial blood gas analysis showed lactic acidosis [pH: 7.254 (7.35-7.45), lactate: 5.96 mmol/L (0.5-1.7 mmol/L)].
Case 2: Blood test results were as follows: White blood cell count 17.15 × 109/L (3.5-9.5 × 109/L); alanine aminotransferase 246 U/L (0-40 U/L); aspartate aminotransferase 139 U/L (0-40 U/L); serum lipase 1835 U/L (20-180 U/L); and serum amylase 862 U/L (25-125 U/L).
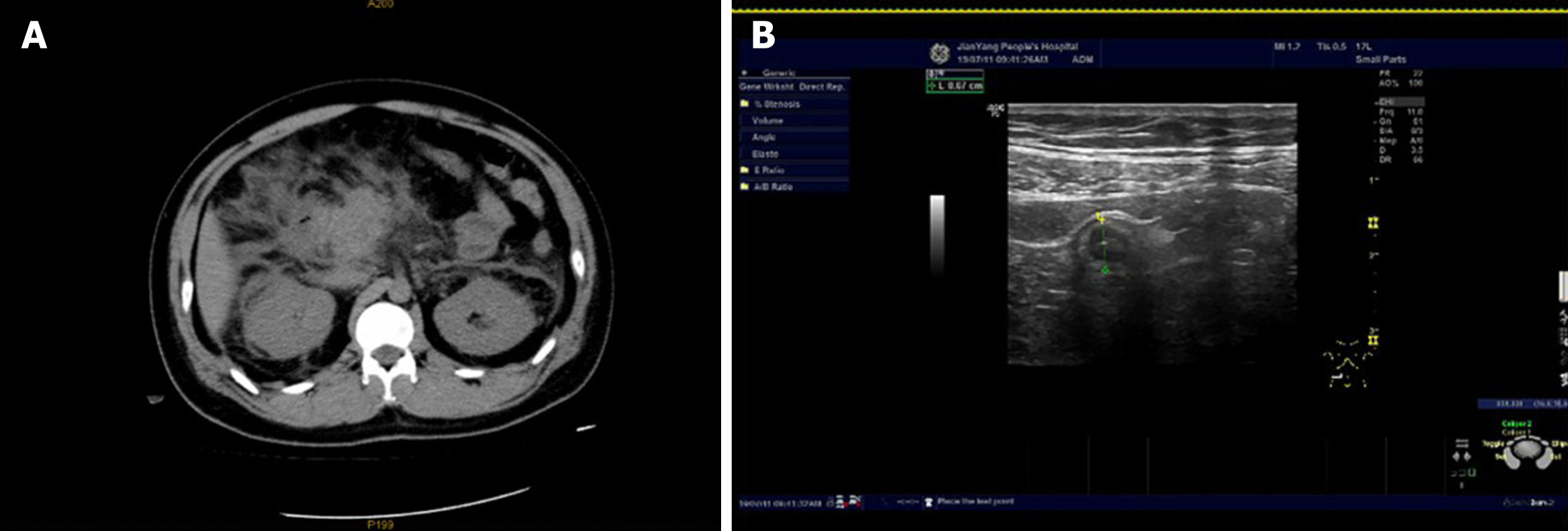
Case 1: Computed tomography of the chest revealed bilateral lower lobe partial consolidation with mild pleural effusion. Computed tomography of the upper abdomen showed features suggestive of AP (Figure 1A).
Case 2: Abdominal color Doppler ultrasound revealed gallstones with a thickened gallbladder wall and no common bile duct stones or intrahepatic biliary tract dilatation. Abdominal computed tomography features were suggestive of AP.
Case 1: A diagnosis of moderately severe AP secondary to hyperlipidemia was made.
Case 2: The diagnosis of gallstone-induced moderately severe AP was made.
Case 1: The patient was administered the medical treatment for AP, which included intravenous analgesia, active fluid resuscitation, nasal oxygen therapy, anti-inflammatory drugs, gastric acid suppression and nasogastric decompression, Somatostatin to reduce pancreatic secretions, anti-hyperlipidemic and anticoagulation medications, external application of Chinese medicine, catharsis and other treatments were also administered.
Case 2: After admission, the patient was treated with intravenous analgesia, active fluid resuscitation, antibiotics, electrolyte supplementation, gastric acid suppression, nasogastric decompression, medication to reduce pancreatic secretions and enzyme activity, external application of Chinese medicine, catharsis and other treatments.
Case 1: The patient’s upper abdominal bloating and pain improved, urine output increased, and bowel functions were restored within 1-2 d of admission. However, after 48 h of admission, the patient developed a high-grade fever and severe pain in the right lower abdomen. On clinical examination, there was rebound tenderness at the McBurney’s point in the right lower abdomen. Emergency abdominal color Doppler ultrasound revealed a thickened dilated appendix with a strip of hypoechoic fluid in the lower right abdomen suggestive of acute appendicitis (Figure 1B).
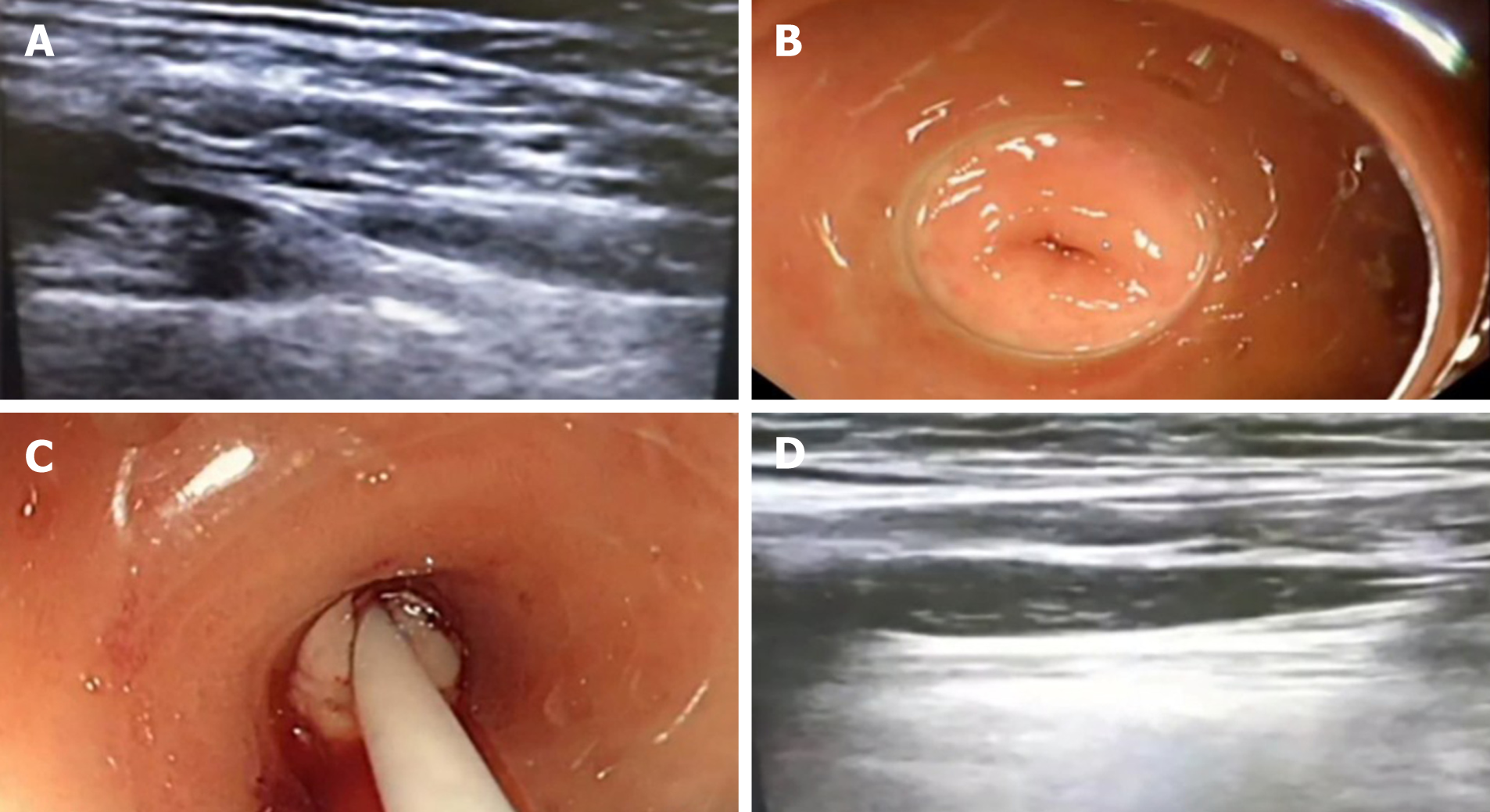
Case 2: With the medical therapy, the patient had relief regarding the upper abdominal pain and abdominal distension with restoration of bowel functions. However, 72 h later, the patient felt continuous pain in the right lower abdomen radiating to the right lower back. On examination, the upper abdominal tenderness was alleviated, and rebound tenderness was present at the McBurney’s point. Abdominal ultrasound revealed a dilated and thickened appendix with cord-like material in its lumen, suggestive of acute appendicitis (Figure 2).
Acute appendicitis with coexistent AP.
The patient started empirical intravenous antibiotics. Despite 2 d of antibiotic treatment, the patient had no significant improvement. Hence, the patient was considered for appendectomy, but the presence of moderately severe AP indicated a risk of respiratory and other complications associated with anesthesia for a laparoscopic or open appendectomy. On the other hand, there was no evidence of appendicular abscess or perforation. Therefore, an alternative minimally invasive ERAT was considered and was explained to the patient and his relatives.
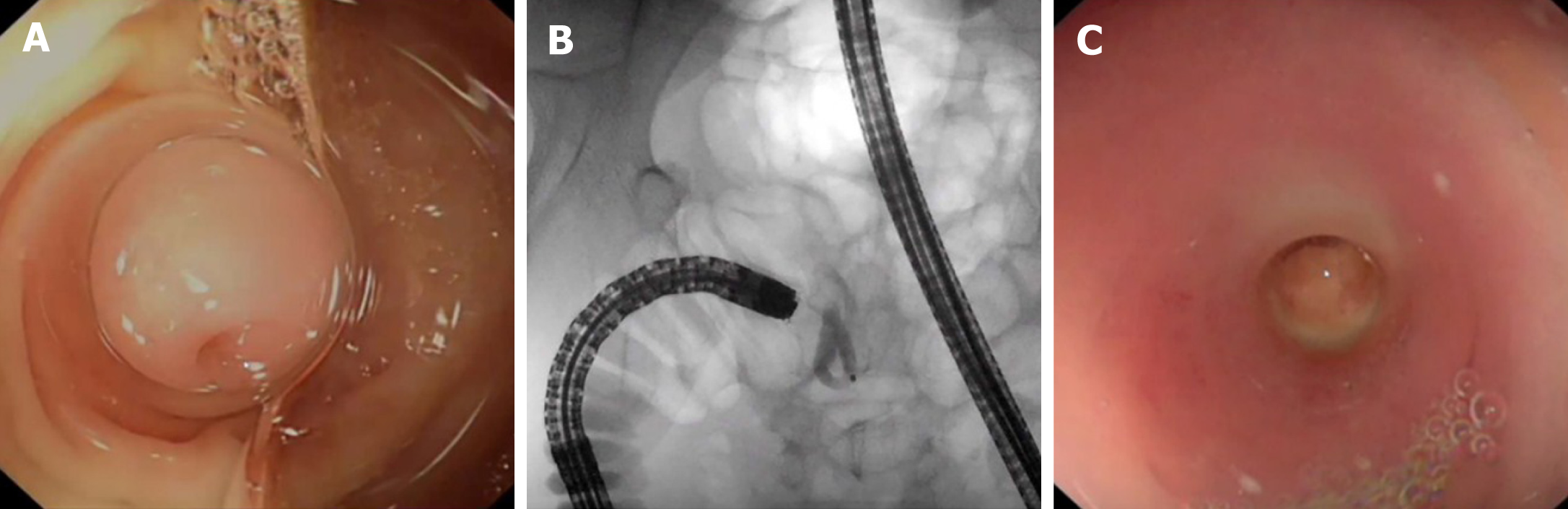
ERAT does not require anesthesia. Therefore, after obtaining written informed consent, the ERAT procedure was performed. Before the procedure, the patient was given a low-pressure clean soap water enema (200-300 mL) 2-3 times. A conical transparent cap (Olympus Medical Corporation of Japan) was fixed to the tip of the enteroscope (Fujineng 4450, Japan) and then introduced into the large intestine. For the colonic insufflation, carbon dioxide gas was used. On reaching the ileocecal region, the opening of the appendix and Gerlach’s valve was identified and the colonoscope was fixed near the appendix. The transparent cap was used to push the Gerlach’s valve to the side to expose the appendix (Figure 3A). The tip of the transparent cap was then aligned with the opening of the appendix. A loach guide wire was built into the enteroscope forceps. Under the guidance of the loach, the catheter was inserted into the appendiceal cavity for a length of about 2 cm. After the insertion of the catheter into the appendiceal cavity, the contrast agent ioversol (Jiangsu Hengrui Medicine Co., Ltd) was injected in a 1:1 ratio under fluoroscopic guidance (Figure 3B). The appendiceal cavity was retrospectively visualized to reveal luminal stenosis and fecal impaction. The appendiceal cavity was irrigated with normal saline (100 mL) and tinidazole (200 mL) (Sichuan Kelun Pharmaceutical Co., Ltd.) using a 5 mL syringe, endoscopic forceps and pressure perfusion. This liquified the feces and facilitated its discharge into the cecum (Figure 3C). After repeated flushing until the flushing liquid was clear, we observed that the appendiceal cavity had cleared. The procedure time was 40 min.
ERAT was considered and explained to the patient and her relatives. After providing written informed consent, the ERAT procedure was performed. Before the procedure, the patient was given a low-pressure clean soap water enema (200-300 mL) 2-3 times.
The transparent cap was fixed to the enteroscope and advanced into the cecum (Figure 4A and 4B). The opening of the appendix was seen with pus flowing out, and the mucosa at the opening of the appendix was markedly congested and edematous (Figure 4C). Using catheter-guide wire technology, a catheter was inserted into the appendiceal cavity along with the guide wire, and the pus was suctioned to reduce the pressure in the appendiceal cavity. Under the guidance of bedside ultrasound, the appendiceal lumen was irrigated with saline (150 mL) and tinidazole (200 mL) (Figure 4D). There was obstruction in the cavity due to fecal stones. After repeated flushing, the sediment-like fecal stones and pus were flushed out. Repeated flushing was performed until the irrigation fluid became clear. On bedside ultrasound, the cord-like material seen in the appendiceal cavity had disappeared. The procedure time was 60 min. The medical management of AP including antibiotics were continued.
After 2 h of observation, the pain in the right lower quadrant gradually eased. The medical management of AP including antibiotics were continued. The fever and right lower quadrant pain resolved by the 3rd d. Postoperative review of the appendix B-ultrasound showed that the swelling of the appendix was significantly reduced, no fecal stones were seen in the appendix cavity, and the exudation around the appendix was significantly reduced. The patient recovered and was discharged after 4 d of hospital stay. At the last follow-up at 6 mo after discharge, the patient was symptom free.
The pain in the right lower abdomen disappeared on the 3rd d. Postoperative review of the appendix B-ultrasound showed that the swelling of the appendix was significantly reduced, no fecal stones were seen in the appendix cavity, the exudation around the appendix was significantly reduced, and the cord-shaped material disappeared. The patient recovered and was discharged after 5 d of hospital stay. At the last follow-up at 6 mo after discharge, the patient was symptom free.
For more than a century, an appendectomy has been the standard method for the treatment of acute appendicitis[6]. However, this procedure requires anesthesia, which has its own morbidity and risk of mortality in critically ill patients, similar to the 2 cases of moderately severe AP seen in this case series. In recent years, there is a consensus that surgical removal of the appendix increases the incidence of digestive tract tumors. Various studies have shown that the incidence of colonic tumors in patients after appendectomy is 14%, which is higher than those who have not had their appendix removed[7]. The appendix secretes digestive enzymes and hormones that promote intestinal motility[8]. In addition, recent experimental evidence suggests that the appendix may play an important role in the immune system[9] and may retain the normal microbial community of the individual[10]. Therefore, the appendix and its function must be preserved as much as possible.
In 2012, Liu et al[4] was the first to report the use of a novel ERAT for the treatment of acute uncomplicated appendicitis. ERAT is a new type of minimally invasive endoscopic treatment with less damage, higher safety and lower cost than general surgery. The main principle is to find the opening of the appendix using an enteroscope. The appendiceal lumen is then cannulated and repeated irrigation with antibiotics is performed to relieve the luminal obstruction and reduce the inflammatory edema of the appendix. For those with severe appendicitis and suppuration, a guide tube can be inserted into the irrigation tube to insert into the appendix after purging the internal pus. The fecal stones in the cavity can be removed by washing, mesh basket or balloon. If required, a stent can be placed to relieve the stenosis, drain the cavity and then flush the lumen with antibiotics. The procedure can be guided by ultrasound, which provides real-time intra-abdominal images to make the procedure safer. Later, several further studies confirmed that ERAT is effective for the direct diagnosis and treatment of acute appendicitis without excision of the appendix[11].
In the 2 patients presented here, we used a soapy water low-pressure clean enema because soapy water can reduce the surface tension of water. This allows water to enter the stools quickly and facilitate the dilution and softening of the stools. Also, soapy water stimulates bowel motility, promotes defecation and facilitates bowel preparation. We used an enteroscope and carbon dioxide for insufflation as it is easily absorbed and thereby reduces the possibility of abdominal distension and aggravation of AP[12]. We successfully treated both patients with ERAT without any complications. ERAT also helped to retain the potential physiological function of the appendix. To the best of our knowledge, there is no previous study on the use of ERAT for patients with coexistent AP and appendicitis.
Recent systematic reviews and meta-analyses of random control trials have concluded that the majority of patients with uncomplicated acute appendicitis can be treated with an antibiotic-first approach[13-15]. But the 5-year follow-up results of the APPAC trial reported that among patients who were initially treated with antibiotics, the likelihood of late recurrence was 39.1%[16]. If antibiotics are combined with ERAT, we believe that better efficacy and lower recurrence rates can be achieved.
In conclusion, ERAT is a safe and effective minimally invasive endoscopic procedure for the treatment of acute uncomplicated appendicitis in patients who are not responding to intravenous antibiotics and not willing or unfit for appendectomy. Although there is a possibility of recurrence of acute appendicitis after ERAT, it is advantageous over surgery for critically ill patients with severe pancreatitis. Future prospective large sample size studies are required to confirm the safety and effectiveness of ERAT as seen in this case series.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sikiric P, Wilcox CM S-Editor: Zhang L L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Fagenholz PJ, Castillo CF, Harris NS, Pelletier AJ, Camargo CA Jr. Increasing United States hospital admissions for acute pancreatitis, 1988-2003. Ann Epidemiol. 2007;17:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 212] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 2. | Mann DV, Hershman MJ, Hittinger R, Glazer G. Multicentre audit of death from acute pancreatitis. Br J Surg. 1994;81:890-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 128] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Traverso LW, Kozarek RA. Pancreatic necrosectomy: definitions and technique. J Gastrointest Surg. 2005;9:436-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Liu BR, Song JT, Han FY, Li H, Yin JB. Endoscopic retrograde appendicitis therapy: a pilot minimally invasive technique (with videos). Gastrointest Endosc. 2012;76:862-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Liu BR, Ma X, Feng J, Yang Z, Qu B, Feng ZT, Ma SR, Yin JB, Sun R, Guo LL, Liu WG. Endoscopic retrograde appendicitis therapy (ERAT): a multicenter retrospective study in China. Surg Endosc. 2015;29:905-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | McBurney C. IV. The Incision Made in the Abdominal Wall in Cases of Appendicitis, with a Description of a New Method of Operating. Ann Surg. 1894;20:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 203] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Wu SC, Chen WT, Muo CH, Ke TW, Fang CW, Sung FC. Association between appendectomy and subsequent colorectal cancer development: an Asian population study. PLoS One. 2015;10:e0118411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, Cornwell EE 3rd, Chang DC, Siram SM. Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg. 2011;201:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 9. | Andreu-Ballester JC, Pérez-Griera J, Ballester F, Colomer-Rubio E, Ortiz-Tarín I, Peñarroja Otero C. Secretory immunoglobulin A (sIgA) deficiency in serum of patients with GALTectomy (appendectomy and tonsillectomy). Clin Immunol. 2007;123:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol. 2007;249:826-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 222] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 11. | Li Y, Mi C, Li W, She J. Diagnosis of Acute Appendicitis by Endoscopic Retrograde Appendicitis Therapy (ERAT): Combination of Colonoscopy and Endoscopic Retrograde Appendicography. Dig Dis Sci. 2016;61:3285-3291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Du Z, Luo S, Wang F. Feasibility and outcomes of colonoscopy with combining carbon dioxide insufflation and water-infusion for resection of colonic polyps. Int J Clin Exp Med. 2018;11:7408-7414. |
| 13. | Podda M, Gerardi C, Cillara N, Fearnhead N, Gomes CA, Birindelli A, Mulliri A, Davies RJ, Di Saverio S. Antibiotic Treatment and Appendectomy for Uncomplicated Acute Appendicitis in Adults and Children: A Systematic Review and Meta-analysis. Ann Surg. 2019;270:1028-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 173] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 14. | Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, Agoritsas T, Heels-Ansdell D, Guyatt GH, Tikkinen KA. Meta-analysis of antibiotics vs appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103:656-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 185] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 15. | Huston JM, Kao LS, Chang PK, Sanders JM, Buckman S, Adams CA, Cocanour CS, Parli SE, Grabowski J, Diaz J, Tessier JM, Duane TM. Antibiotics vs. Appendectomy for Acute Uncomplicated Appendicitis in Adults: Review of the Evidence and Future Directions. Surg Infect (Larchmt). 2017;18:527-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Mecklin JP, Sand J, Virtanen J, Jartti A, Grönroos JM. Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018;320:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 315] [Article Influence: 45.0] [Reference Citation Analysis (2)] |