Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.170
Peer-review started: March 30, 2020
First decision: September 24, 2020
Revised: October 2, 2020
Accepted: November 21, 2020
Article in press: November 21, 2020
Published online: January 6, 2021
Processing time: 277 Days and 10 Hours
At the end of 2019, a new epidemic of viral pneumonia emerged in China and was determined to be caused by a novel coronavirus, which was named coronavirus disease 2019 (COVID-19) by the World Health Organization. The epidemic quickly spread, causing a worldwide pandemic. Scientists and clinicians across the globe have shifted their research efforts towards understanding the virus itself and its epidemiology.
In mid-January 2020, a Chinese family made a visit to a local city, and within the next 2 wk one after another fell ill with COVID-19. At the beginning of their first illness onset, the family had eaten in a restaurant, which led to the subsequent illness onset in another two families. All cases were diagnosed as COVID-19 by real-time fluorescent reverse transcription-polymerase chain reaction. Epidemiological investigation showed that the transmission chain was complete.
This chain of social exposure highlights the danger of group aggregative behavior for spread of COVID-19.
Core Tip: Since its first emergence at the end of 2019, we have gained limited knowledge about the coronavirus disease 2019 and its epidemiology. We investigated a group of aggregated cases, diagnosed by viral genetic testing (real-time fluorescent reverse transcription-polymerase chain reaction), and characterized the epidemic characteristics of spread for such. The findings provide strong evidence for controlling human social behaviors to help mitigate the virus’s threat to human health.
- Citation: Zuo H, Hu ZB, Zhu F. Risk of group aggregative behavior during COVID-19 outbreak: A case report. World J Clin Cases 2021; 9(1): 170-174
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/170.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.170
Since the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began to appear at the end of 2019[1], causing the sometimes life-threatening coronavirus disease 2019 (COVID-19), it has spread globally and been responsible for over 1 million deaths to date. In order to combat the virus’s spread in the early days of the pandemic, the World Health Organization (WHO) published an interim guidance (dated January 29, 2020) that included actionable guidance to protect public health. Although the optimal epidemiological measures (i.e., screening) and methods (i.e., contract tracing) remain to be definitely established[2], it is clear that human social behaviors affect the epidemic event.
Here, we report a typical spread of COVID-19 due to congregational behavior. This experience should prompt both individuals and communities to pay attention to the risk of such social behavior during the ongoing COVID-19 outbreak.
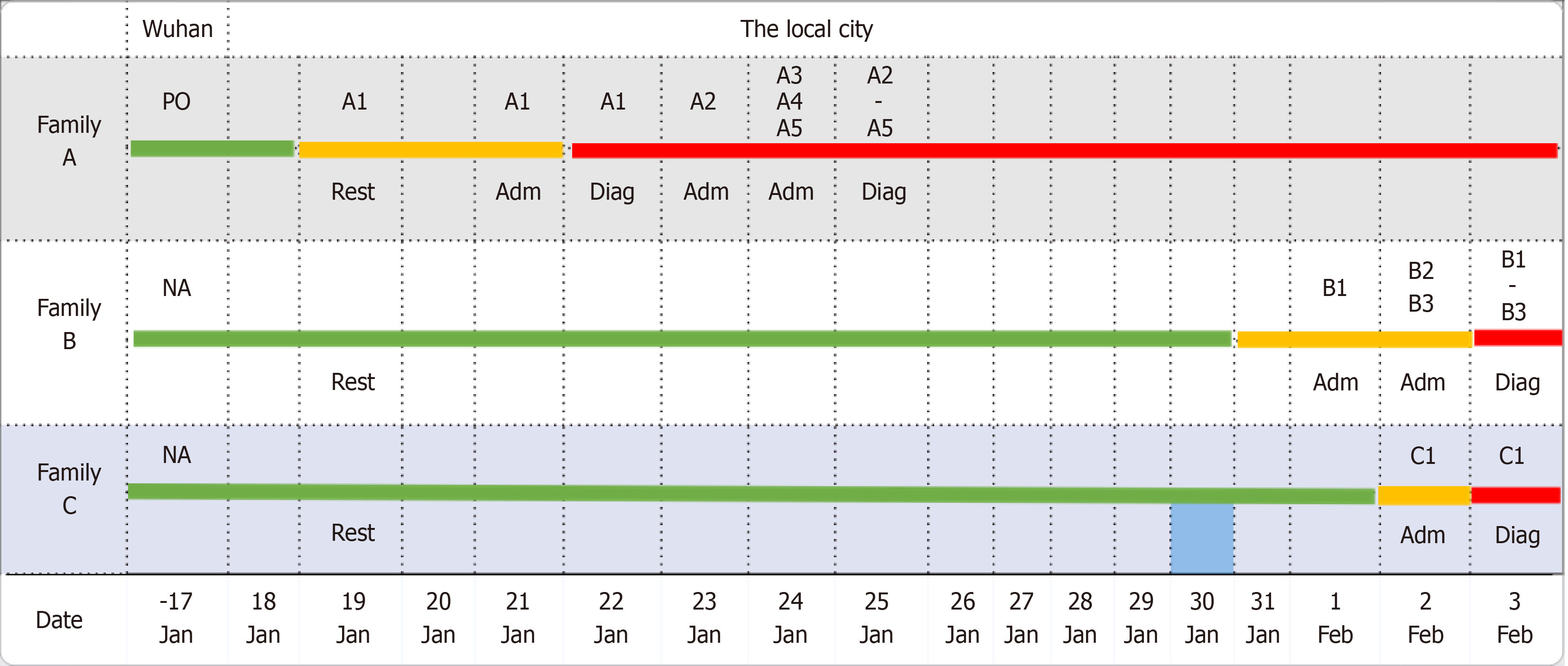
On January 18, 2020, ten members of family A from Wuhan, China traveled to a local city. An elderly female experienced COVID-19 illness onset first, during their travel. In response, local healthcare authorities (on government mandate) concentrated the other nine family members in an isolated place for medical observation. Within the next week, four of those nine experienced illness onset.
At the beginning of February, another family (Family B) in the local city had three members fall ill with COVID-19 in a short (2 d) period. These three members included the hostess from a restaurant visited by Family A, who was the first of the three to fall ill (on February 2, 2020); the other two members fell ill on February 3, 2020.
Almost at the same time, another hostess (from family C) from the restaurant visited by family A experienced illness onset.
Every individual from the three families who fell ill presented to the appointed COVID-19 hospital.
In all cases, the patients’ symptoms (from all three families) were similar to a common cold but led to concern of COVID-19 due to the epidemic outbreak.
In all cases, the personal medical history was unremarkable.
The members from family A and family B presented, subsequently, with the same illness onset within 1 wk or 2 wk of the index case.
In all cases, the physical examination (conducted at the appointed COVID-19 hospital) showed similar symptomatic profile, including cough, asthenia, anorexia, and body temperature > 37.5 ºC.
In all cases, total white blood cell count and neutrophil count were within normal range.
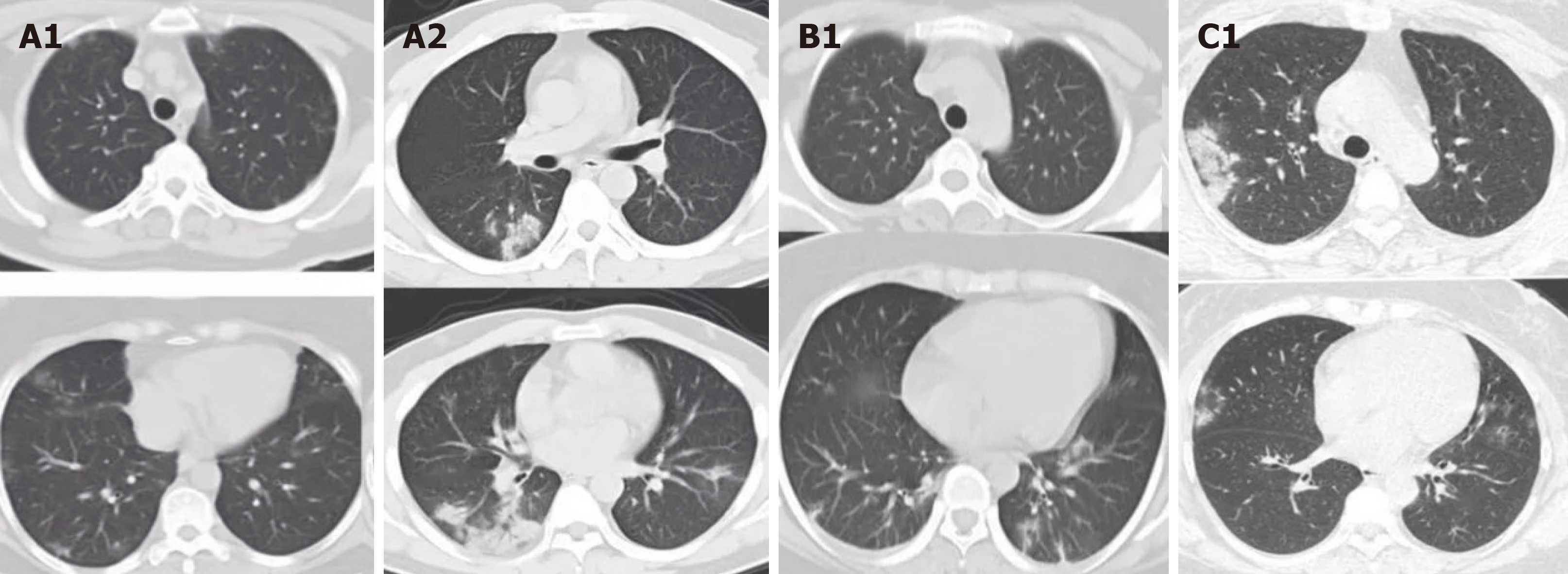
For all cases, chest computed tomography scans showed multiple ground glass shadows in one or both lungs (Figure 1).
Epidemiologic investigation was carried out by interview (via a questionnaire). Each suspected case was asked for information regarding their familial relatives, exposure histories during the 2 wk period of suspected exposure (including the dates, times, frequency, and patterns of exposures to any unknown person), especially those in Wuhan or exposures to any relevant environments, such as specific markets (e.g., live animal ‘wet’ markets)[3].
Family A came from Wuhan, which was the first place to report cases of the COVID-19 epidemic in China. The family reported having gone to a restaurant in a local city for dinner on the evening on January 19, 2020, at which time an elderly female member was experiencing illness symptoms during their travel. None of the members from family B and family C had a history of living or travel in the epidemic area of the city nor of contact with any related individuals; for both families, the exception was dining at a restaurant on the evening of January 19, 2020.
Thus, family B and family C, who were not familiar with each other, were present and eating in the same place, at the same time. This raised the question of whether the two families were exposed to any infectious sources accordingly? Follow-up with the restaurant itself afforded surveillance video of that day, which showed that family A was seated at a table between the tables occupied by family B and family C, respectively. Without warning, the three families who were unknown to each other formed a congregation, with family A from the epidemic area seated in the middle, and family B to the left and family C to the right. Family A had one member who had already begun to experience illness during that day; the timing of consecutive illness onset in family A and family B matched the incubation time of COVID-19 (Figure 2).
All COVID-19 diagnoses were made by real-time fluorescent reverse transcription-polymerase chain reaction detection of respiratory specimens, according to the “Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia” (6th Trial Version; http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf). The kit used was specific to the COVID-19 virus gene sequence and was designed based on the previous WHO recommendation (Laboratory Diagnostics for Novel Coronavirus. WHO 2020). All tests were conducted by KingMed Diagnostics Group Co., Ltd (Guangzhou, China), under supervision of the Centre for Disease Control and Prevention of the local city in China.
Based on the local government’s policy, all COVID-19 cases from the three families were admitted as in-patients to COVID-19 appointed hospitals (representing two of such). The other family members were concentrated for a 14 d medical observation in an isolated place. Relevant clinical treatment was carried out for the COVID patients, following guidance from the “Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia” (6th Trial Version).
About 3 wk after the first case (family A) was discovered, all those with illness from the three families recovered from the pneumonia that had developed from the virus infection. All were allowed to leave the hospital after achieving a negative laboratory test result for the SARS-CoV-2-virus. Other members of the three families underwent four rounds of testing to confirm no SARS-CoV-2-infection during the 14 d period of medical observation.
As of mid-March, the epidemic situation in China was considered to be under control, although substantial difficulties and challenges were met, which are largely unknown abroad. A large number of lessons are worth learning for the Western countries, who are still under a COVID-19 storm. We report this case series, including consecutive persons infected by the SARS-CoV-2 virus through an exposure of group aggregative dining behavior, to highlight that the virus spreads directly through the air.
This report draws our attention to the importance of personal prevention and control during a COVID-19 storm. Due to the characteristics of SARS-CoV-2 virus transmission[3], respiratory droplet transmission is more likely to occur in a narrow space[4]. Considering the swift spread among social congregations (and families) that is occurring continuously, populations need to minimize outings, reduce group aggregative behaviors, and practice effective isolation of any suspected cases. In addition, sufficient personal protection should be practiced, including the wearing of face masks and keeping a reasonable distance from other persons.
Infection with the COVID-19 virus can be life-threatening at worst and produce a negative impact on human health at best. The virus shows no regard for geographic region and all nations’ populations are at risk. It is thus necessary for us to check our behaviors, particularly group aggregative behaviors, to help curb the ongoing pandemic and the damage to individual lives threatened by COVID-19.
We would like to acknowledge KingMed Diagnostics Group Co., Ltd (Guangzhou, China) for the laboratory testing of case specimens and the Centre for Disease Control and Prevention of Guangzhou, China for supervising all epidemiologic investigations.
Manuscript source: Unsolicited manuscript
Specialty type: Public, environmental and occupational health
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papazafiropoulou A S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9319] [Article Influence: 1863.8] [Reference Citation Analysis (0)] |
| 2. | Leung CC, Lam TH, Cheng KK. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020;395:945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 216] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 3. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17647] [Article Influence: 3529.4] [Reference Citation Analysis (0)] |
| 4. | Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Lo SK, Chan KH, Poon VK, Chan WM, Ip JD, Cai JP, Cheng VC, Chen H, Hui CK, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514-523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6483] [Cited by in RCA: 5423] [Article Influence: 1084.6] [Reference Citation Analysis (0)] |